Abstract
Background
Natural killer (NK) cells are the main effective component of the innate immune system that responds to chronic hepatitis B (CHB) infection. Although numerous studies have reported the immune profiles of NK cells in CHB patients, they are limited by inconsistent results. Thus, we performed a meta-analysis to characterize reliably the immune profiles of NK cells after CHB infection, specifically frequency, phenotype, and function.
Methods
A literature search of the computer databases MEDLINE, PUBMED, EMBASE, and Cochrane Center Register of Controlled Trails was performed and 19 studies were selected. The standard mean difference (SMD) and 95% confidence interval (CI) of each continuous variable was estimated with a fixed effects model when I2 < 50% for the test for heterogeneity, or the random effects model otherwise. Publication bias was evaluated using Begg’s and Egger’s tests.
Results
The meta-analysis of publications that reported frequency of peripheral NK cells showed that NK cell levels in CHB patients were significantly lower compared with that of healthy controls. A higher frequency of CD56bright NK subsets was found in CHB patients, but the CD56dim NK subsets of CHB patients and healthy controls were similar. CHB patients before and after antiviral therapy with nucleotide analogues (NUCs) showed no statistical difference in NK frequency. The activating receptors were upregulated, whereas inhibitory receptors were comparable in the peripheral NK cells of CHB individuals and healthy controls. NK cells of CHB patients displayed higher cytotoxic potency as evidenced by CD107a protein levels and conserved potency to produce interferon-gamma (IFNγ), compared with their healthy counterparts.
Conclusion
Our results revealed that CHB patients had a lower frequency of NK cells compared with healthy individuals not treatable with antiviral NUC therapy. With an activating phenotype, NK cells in CHB patients showed better cytotoxic potency and conserved IFNγ production.
Introduction
Hepatitis B virus (HBV) infection is an important health problem worldwide. About 2 billion people have been infected with this virus as reported by the World Health Organization. Over 400 million patients infected with HBV eventually develop chronic hepatitis [1]. Most CHB patients also suffer severe liver disease such as liver cirrhosis and hepatocellular carcinoma [2, 3]. The mechanism by which some HBV patients progress to chronic hepatitis has not yet been fully elucidated [4–6]. The host immune response is considered an important factor for determining whether HBV infection is cleared or persists [7, 8].
NK cells are the main effective population of the innate immune system that responds to viral infection (e.g., HBV) via cytotoxic effectors and cytokine production [9, 10]. NK cells constitute approximately 40% to 60% of liver lymphocytes and 5–15% of total lymphocytes [11, 12]. Derived from hematopoietic progenitor cells in the bone marrow, these large granular lymphocytes have been identified by flow cytometry from CD56 levels and lack of the T-cell marker CD3 (that is, CD3−CD56+ NK cell status) [13]. CD3−CD56+ NK cells can be further subdivided into CD56dim NK cells, which express CD16 (Fcγ-receptor) and KIR (killer-cell immunoglobulin-like receptor), and CD56bright NK cells, which lack expression of the two above markers [10, 13]. Although CD56dim NK cells are the largest population and CD56bright NK cells are in the minority in the blood, this subdivision can be significantly changed by persistent viral infection [14].
NK cells display at least two major effector functions to control viral infection: they can directly attack infected cells through cell-to-cell contact, but they also secret a variety of antiviral cytokines such as interferon-gamma (IFNγ) [10, 13, 15]. An increasing number of studies have shown that during HBV infection, effective immune responses by NK cells may lead to the initial control of the acute infection in the early phase and allow the efficient development of an adaptive immune response [16, 17]. Since NK function is closely regulated by activating receptors (NKP30, NKp44, NKp46, NKG2D, NKG2C) and inhibitory receptors (NKG2A, CD158a, CD158b), interactions between NK cell receptors and their corresponding ligands determine the fate of NK cells [15, 18]. Interestingly, in chronic viral infection such as with HBV, NK cell function is impaired through changes in their receptors [15, 19].
The current therapy for CHB is based on the application of pegylated interferon-alpha (Peg-IFNα) or NUCs [20, 21]. Recent studies have reported the effects of anti-viral therapy on innate effectors such as NK cells [22–26]. It has been shown that inhibition of HBV replication by antiviral therapeutic medicine such as NUCs helped to restore partially the function of NK cells in the peripheral blood [22, 23]. However, little is known about the influence of antiviral therapy on the proportion of NK cells.
A large number of studies have addressed the immune profiles of NK cells in CHB patients. Nonetheless, these documented studies are limited by small sample size, differences in patient ethnicities and geographical locations, and, especially, inconsistent results. Therefore, we performed a systematic review and meta-analysis of the currently relevant literature to investigate the frequency, phenotypes, and functions of NK cells in CHB patients.
Materials and Methods
Literature search strategy
The study was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses criteria (PRISMA) (S1 PRISMA Checklist). A search of the MEDLINE, PUBMED, EMBASE, and Cochrane Center Register of Controlled Trails computer databases (from 1980 to December 2015) was performed of manuscripts. The search strategy involved selecting Medical Subject Headings (MeSH) and text words used in combination or alone: “HBV”, “NK cell”, “hepatitis B virus”, “natural killer cells”. The scope of the search was restricted to “human” and “English”. Emails were sent to corresponding authors of related articles in which enough data was not provided. We excluded the non-informative studies if the authors did not reply. Independent searches were conducted by QFZ and JYS.
Selection criteria
Published studies in English were included when they met the following criteria: randomized control, case-control, or cohort studies; reports of NK cell frequency, phenotypes, receptors, or functions, in peripheral blood or liver tissue; treatment-naïve patients with chronic mono-HBV infection (i.e., no patients taking antiviral therapy or immunosuppressive drugs within 6 months before the sampling); investigating the effect on NK cells of treatment with NUCs or Peg-IFNα. Papers were excluded if they contained unclear or confusing data; or reports of NK cells immune profiles of patients co-infected with hepatitis C virus, hepatitis D virus, or human immunodeficiency virus. The names of the authors or journals of the articles did not influence our selection decisions.
Data extraction
Two reviewers (QFZ and JYS) independently applied the inclusion criteria, selected the studies, and extracted the data. The following data were extracted from each paper: number of patients in the study; details of the study design; characteristics of patients; treatment regimen; and results measured by flow cytometry. Studies were selected in a 2-stage process. Firstly, the titles and the abstracts from the electronic searches were scrutinized by two reviewers independently (QFZ and JYS) and the full manuscripts of all citations that were likely to meet the predefined selection criteria were obtained. Secondly, final inclusion or exclusion decisions were made upon examination of the full manuscripts. In case of duplicates, the most recent or the most comprehensive publication with all the results was used.
Study quality
The methodological quality of the articles was assessed using the Newcastle-Ottawa Scale (Wells et al. 2000) [27]. The quality score was calculated on the basis of 3 major components of case-control studies: selection of study groups (0–4 stars), comparability of study groups (0–2 stars), and ascertainment of the outcome of interest (0–3 stars; S1 Table). The quality assessment tool for the cohort study consisted of three domains, including selection of the exposed and unexposed cohort (maximum: 4 stars), comparability of the two cohorts (maximum: 2 stars), and outcome assessment (maximum: 3 stars; S1 Table). A higher score indicated better methodology. The quality of each study was independently assessed by the same two reviewers (QFZ and JYS). In case of disagreement between the 2 reviewers, a third party (DZZ) was consulted.
Statistical analysis
Statistical analyses for continuous variables were conducted. Heterogeneity was measured using the I2 test [28]. In these tests, I2 > 50% indicated significant heterogeneity; P < 0.05 was also considered to indicate significant heterogeneity. In cases where significant heterogeneity existed, a random effects model was used to quantify heterogeneity across studies. A fixed effects model was used in the other cases [29]. Outcomes were expressed as SMD, with 95%CI. If the value 0 was not included in the 95% CI, the point estimate of the SMD was considered to have reached statistical significance (P < 0.05).
To explain heterogeneity among different studies, stratified analyses were performed of alanine transaminase (ALT) levels, HBV-DNA, study location, patient ages, case sample size, and publication year [30]. The ALT levels, immunity status, and NK subsets were further examined in subgroup analyses. Publication bias was evaluated with Begg’s and Egger’s tests [31]. All analyses were performed with STATA version 12.0 (Stata, College Station, TX) in accordance with the recommendations of the manufacturer. P < 0.05 was considered significant.
Results
Search results and study characteristics
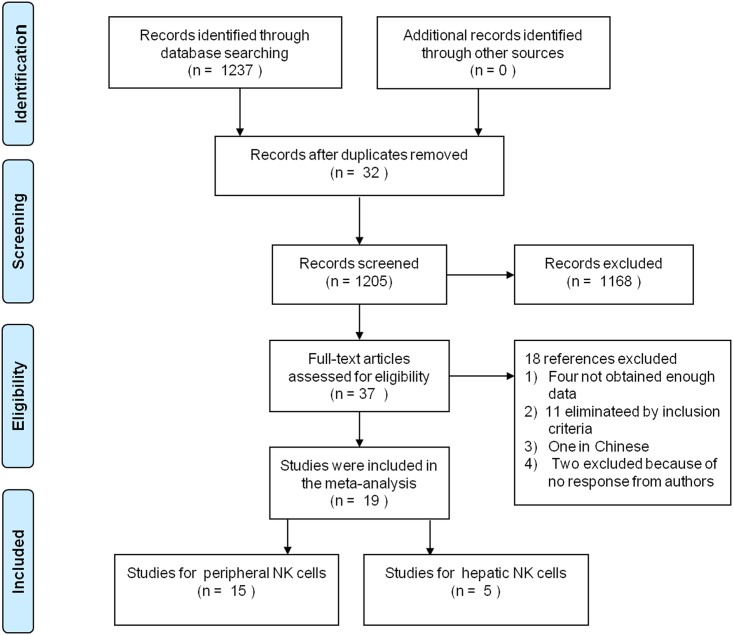
Using the strategy described above, 1237 studies were initially identified and screened for retrieval (Fig 1). After reviewing the title or the abstract, 1205 studies were excluded and 37 were retrieved and subjected to detailed evaluation after removing duplicates and scanning titles and abstracts. Of the 37 studies, one study was excluded because of language. By applying the inclusion and exclusion criteria of the present study, 11 studies were eliminated. Due to lack of data, four studies were excluded, and another two studies were excluded because the author did not respond to requests for information. Finally, 19 studies [14, 22–24, 32–46] (S1 File) comprising 993 patients were included in the meta-analysis.
Fig 1. The selection process for eligible studies.
Of the 1237 studies initially identified from our electronic search, 19 met the inclusion criteria.
Of the 19 studies, three were cohort studies and 16 were case control studies. All these studies were published between 2006 and 2015. The basic characteristics of each study are listed in Tables 1 and 2. Eleven of the studies were from China, three from the Netherlands, the one each from Italy, United Kingdom, Ireland, Germany, and France. The sample size of each of the studies ranged from 18 to 154 people. The mean ages ranged from 24.2 to 47.0 years. The male-to-female ratios ranged from 0.7 to 8.0.
Table 1. Characteristics of the 18 studies included in the analysis.
| First author, Year | Location | Study type | Immune State | Age, y a | Gender, M/F | ||
|---|---|---|---|---|---|---|---|
| HBV | HC | HBV | HC | ||||
| Bonorino, 2009 | French | Case-control | NA | 38 (17–63) b | NA | 1.11 | NA |
| Conroy, 2014 | Irish | Case-control | NA | 34.3 (18–60) b | NA | 1 | NA |
| Gu, 2009 | Chinese | Case-control | IA | 35.50 ± 6.21 | 35.18 ± 7.01 | 2.57 | 2.75 |
| Li, 2012 | Chinese | Case-control | NA | 34 c | 29 c | 2.32 | 1.33 |
| Li, 2014 | Chinese | Case-control | IT | 28.27 ± 34.59 | 25.35 ± 40.94 | 0.88 | 0.80 |
| Chinese | Case-control | IA | 30.82 ± 68.57 | 25.35 ± 40.94 | 4.25 | 0.80 | |
| Li, 2015 | Chinese | Case-control | IT | 32.8 ± 8.9 | 42.1 ± 10.9 | 2.0 | 1.9 |
| Chinese | Case-control | IA | 38.1± 11.6 | 42.1 ± 10.9 | 2.1 | 1.9 | |
| Chinese | Case-control | IN | 32.2 ± 7.4 | 42.1 ± 10.9 | 6.3 | 1.9 | |
| Lunemann, 2014 | German | Case-control | NA | 41 (22–59) b | 48 (21–65) b | 0.70 | 1.00 |
| Lv, 2012 | Chinese | Cohort | IA | 34.4 ± 20.9 | 35.9 ± 35.0 | 2.43 | 5.00 |
| Oliviero, 2009 | Italian | Case-control | NA | 48 (20–72) b | NA | 1.44 | NA |
| Peppa, 2010 | English | Case-control | NA | 37.2±11.9 | 30.0 ± 8.5 | 1.13 | 1.12 |
| Sprengers, 2006 | Dutch | Case-control | NA | 36.29±9.84 | NA | 2.36 | NA |
| Sun, 2012 | Chinese | Case-control | NA | 33.4± 2.6 | 34.1 ± 1.8 | 1.23 | 1.06 |
| Tjwa, 2011 | Dutch | Case-control | NA | 38.1 ± 10.1 | 36.9 ± 8.0 | 2.08 | 1.27 |
| Dutch | Cohort | IA | 43.1 ± 12.78 | 36.9 ± 8.0 | 2.81 | 1.27 | |
| Tjwa, 2014 | Dutch | Case-control | NA | 37.15 ± 7.43 | 0 | 1.24 | NA |
| Yan, 2006 | Chinese | Case control | NA | 39.23 ± 18.92 | 38.17 ± 15.77 | 1.16 | 1.80 |
| Zhang, 2011 | Chinese | Case-control | IT | 24 (16–44) b | 27 (20–35) b | 1.70 | 1.89 |
| Chinese | Case-control | IA | 27 (16–46) b | 27 (20–35) b | 2.79 | 1.89 | |
| Zhao J, 2012 | Chinese | Case-control | IA | 38 (22–65) b | 30 (25–45) b | 3.75 | 3.00 |
| Zhao P, 2012 | Chinese | Cohort | NA | 27.5 (19–43) b | 29 (23–50) b | 8.00 | 3.67 |
| Zheng, 2015 | Chinese | Case-control | IT | 34 (20–55) b | 30 (25–38) b | 2.60 | 1.50 |
| Chinese | Case-control | IA | 31 (17–46) b | 30 (25–38) b | 1.83 | 1.50 | |
a Median ± SD, unless noted otherwise;
b median (range);
c median
Abbreviations: ALT, alanine transaminase; IA, immune active; IN, immune inactive; IT, immune tolerant; NA, not available
Table 2. Characteristics of the 18 studies included in the analysis.
| First author, Year | Immue state | ALT, IU/L a | HBV-DNA a, b | Blood, n | Liver, n | ||
|---|---|---|---|---|---|---|---|
| HBV | HBV | HBV | HC | HBV | HC | ||
| Bonorino, 2009 | NA | 42.7 ± 27.8 | 45 ± 1.9 c | 19 | 18 | 6 | 0 |
| Conroy, 2014 | NA | 33.8 (8–143) d | 2.92 (0.85–8.65) d | 66 | 62 | 0 | 0 |
| Gu, 2009 | IA | 403.72 ± 258.06 | 5.85 ± 1.08 | 100 | 30 | 0 | 0 |
| Li, 2012 | NA | 81 e | 5.27 (3–8.48) d | 73 | 35 | 0 | 0 |
| Li, 2014 | IT | 22.22 ± 27.58 | 7.58 ± 0.81 | 15 | 18 | 0 | 0 |
| IA | 199.85 ± 1250 | 6.62 ± 1.17 | 42 | 18 | 0 | 0 | |
| Li, 2015 | IT | <50 | 7.0 ± 1.8 | 24 | 20 | 0 | 0 |
| IA | 198.8 ± 113.4 | 6.2 ± 1.9 | 40 | 20 | 0 | 0 | |
| IN | <50 | <3 | 22 | 20 | 0 | 0 | |
| Lunemann, 2014 | NA | 30 (14–166) d | 3.47 (2.53–7.52) c,d | 17 | 30 | 0 | 0 |
| Lv, 2012 | IA | 124.5±211.4 | 7.6 ± 3.2 c | 24 | 12 | 0 | 0 |
| Oliviero, 2009 | NA | 50.5 (13–291) d | 5.17 (2.23–8.14) c,d | 22 | 30 | 0 | 0 |
| Peppa, 2010 | NA | 69.3 ± 99.4 | 4.4 ± 2.2 c | 64 | 31 | 8 | 0 |
| Sprengers, 2006 | NA | 153.85 ± 189.84 | 5.67 ± 1.66 | 47 | 0 | 47 | 0 |
| Sun, 2012 | NA | 98 ± 117 | >3.30 c | 154 | 95 | 0 | 0 |
| Tjwa, 2011 | NA | 60 ± 82.22 | 6.5 ± 1.9 | 40 | 25 | 0 | 0 |
| IA | 75 ± 13 | 7.7 ± 2.3 | 15 | 25 | 0 | 0 | |
| Tjwa, 2014 | NA | 85.05 ± 64.86 | 6.0 ± 2.2 c | 56 | 0 | 56 | 0 |
| Yan, 2006 | NA | 369.26 ± 238.87 | NA | 54 | 14 | 0 | 0 |
| Zhang, 2011 | IT | 23 (12–26) d | 8.43 (7.15–8.81) c,d | 27 | 26 | 15 | 12 |
| IA | 196 (41–1298) d | 8.29 (4.40–9.29) c,d | 51 | 26 | 29 | 12 | |
| Zhao J, 2012 | IA | 242 (42–1298) d | 7.2 (2.7–8.6) c,d | 19 | 16 | 0 | 0 |
| Zhao P, 2012 | NA | 165 (12–914) d | 4.3 (1.86–9.3) d | 18 | 14 | 0 | 0 |
| Zheng, 2015 | IT | 28 (14–46) d | 5.32 (3.00–7.88) d | 36 | 10 | 0 | 0 |
| IA | 149 (52–1733) d | 5.61 (4.10–8.58) c,d | 34 | 10 | 24 | 0 | |
a Median ± SD, unless noted otherwise;
b log10 copies/mL, unless noted otherwise;
c log10 IU/mL;
d median (range);
e median
Abbreviations: ALT, alanine transaminase; IA, Immune active; IN, Immune inactive; IT, Immune tolerant; NA, not available
Peripheral NK cells in CHB patients compared with healthy controls
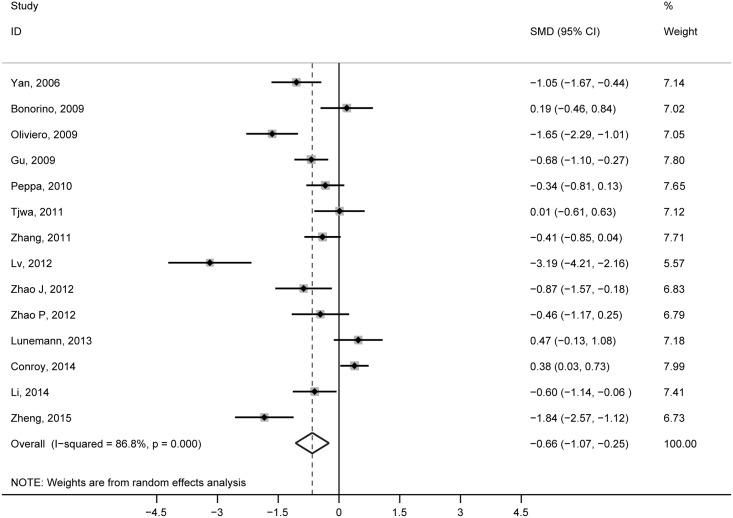
The meta-analysis of the 14 studies showed that peripheral NK cell levels in CHB patients were significantly higher than in the healthy controls (SMD = –0.66, 95% CI: –1.07 to –0.25, P = 0.002; Fig 2). There was evidence of high statistical heterogeneity among the studies (I2 = 86.8%), and the randomized-effects model was applied. A meta-regression analysis was conducted to examine the source of heterogeneity (S2 Table), and ALT levels had a potency effect on NK percentage (P = 0.037).
Fig 2. Pooled comparison of peripheral NK cells in CHB patients and healthy controls.
Based on results from the meta-regression analysis, we subsequently performed a subgroup analysis based on ALT levels (Table 3). Our findings diverged significantly due to the ALT levels. In the subgroup with CHB patients (<80 IU/L), the frequency of NK cells did not change significantly compared to healthy counterparts (SMD = 0.15, 95% CI: –0.16 to 0.46, P = 0.355, I2 = 44.2%). In the other two subgroups, lower levels of NK cells were found for CHB patients compared with the healthy controls (80–300 IU/L: SMD = –1.46, 95% CI: –2.30 to –0.62, P = 0.001, I2 = 88.7%) and (>300 IU/L: SMD = –0.76, 95% CI: –1.04 to –0.47, P = 0.000, I2 = 0.0%). Additionally, the I2 statistic (I2 = 88.7%) only showed high heterogeneity in the subgroup that consisted of CHB patients with ALT levels 80–300 IU/L.
Table 3. Results of subgroup analysis evaluating the difference in NK cells between CHB patients and healthy controls.
| NK cells in PBMC, % | Subsgroup | CHB/HC, n | Study no. | SMD | I2 | 95% CI | P |
|---|---|---|---|---|---|---|---|
| Total | 616/328 | 14 | –0.66 | 86.8% | –1.07 to –0.25 | 0.002 | |
| ALT, IU/L | <80 | 174/158 | 5 | 0.15 | 44.2% | –0.16 to 0.46 | 0.355 |
| 80–300 | 298/143 | 5 | –1.46 | 88.7% | –2.30 to –0.62 | 0.001 | |
| >300 | 191/74 | 4 | –0.76 | 0.0% | –1.04 to –0.47 | 0.000 | |
| Immune state | Immune tolerant | 76/54 | 3 | –0.53 | 72.4% | –1.25 to 0.20 | 0.153 |
| Immune active | 253/96 | 5 | –0.97 | 85.5% | –1.23 to –0.72 | 0.000 | |
| NK subsets | CD56 dim | 117/130 | 4 | 0.08 | 0.0% | –0.17 to 0.33 | 0.534 |
| CD56 bright | 119/95 | 4 | 0.33 | 48.4% | 0.05 to 0.61 | 0.021 |
After further exclusion of studies that contained no relevant information, we performed two subgroup analyses of immunity status (immune tolerant and immune active) and NK subsets (CD56dim NK and CD56bright NK; Table 3). Interestingly, the analysis of studies of immune tolerant patients was non-significant (SMD = –0.53, 95% CI: –1.25 to 0.20, P = 0.153) whereas patients in immune active phase showed significantly decreased NK frequency compared to healthy controls (SMD = –0.97, 95% CI: –1.23 to –0.72, P = 0.000). Regarding the NK subsets, the frequency of CD56dim NK cells were similar between the CHB patients and healthy controls (SMD = 0.08, 95% CI: –0.17 to 0.33, P = 0.534), whereas CD56bright NK subsets displayed a higher frequency in CHB patients compared to healthy controls (SMD = 0.33, 95% CI: 0.05 to 0.61, P = 0.021).
A meta-analysis was conducted of four studies that evaluated the NK frequency of CHB patients in liver and peripheral blood (S1A Fig). In the liver, the NK cell populations were larger compared with that in the peripheral blood. When a meta-analysis was performed that excluded these two studies as sources of heterogeneity (S1B Fig) identified by Galbraith’s plots [33, 45], the heterogeneity disappeared (S1C Fig). We also analyzed the role of treatment with NUCs on the frequency of peripheral NK cells (S2 Fig). No significant difference was found in CHB patients before and after treatment.
NK cell receptors between CHB patients and healthy controls
We also analyzed NK cell receptor expression between CHB patients and healthy controls, including the activating receptors NKp44, NKp46, NKp30, NKG2D and NKG2C, and the inhibitory receptors NKG2A, CD158a, and CD158b (Table 4). Activating receptors NKp46, NKp30, NKG2D and NKG2C were increased, whereas inhibitory receptors NKG2A, CD158a, and CD158b were comparable in the peripheral blood of CHB patients, compared with that of healthy controls. Thus, NK cells displayed an activating phenotype during CHB infection.
Table 4. Results of meta-analyses of studies evaluating the difference in NK receptors between CHB patients and healthy controls.
| NKR in NK cells, % | CHB/HC, n | Study no. | SMD | I2 | 95% CI | P |
|---|---|---|---|---|---|---|
| NKp44 | 288/139 | 5 | 0.137 | 89.80% | -0.58 to 0.85 | 0.707 |
| NKp46 | 288/139 | 5 | 0.386 | 79.90% | 0.18 to 0.60 | 0.000 |
| NKp30 | 365/169 | 7 | 0.585 | 79.70% | 0.13 to 1.04 | 0.011 |
| NKG2D | 172/95 | 5 | 0.465 | 59.70% | 0.03 to 0.90 | 0.035 |
| NKG2C | 267/133 | 6 | 0.522 | 94.90% | 0.29 to 0.76 | 0.000 |
| NKG2A | 376/174 | 8 | 0.002 | 12.90% | –0.20 to 0.21 | 0.985 |
| CD158a | 208/103 | 5 | -0.072 | 68.70% | –0.53 to 0.38 | 0.756 |
| CD158b | 235/106 | 6 | -0.079 | 40.50% | –0.40 to 0.24 | 0.626 |
Production of CD107a and IFNγ in CHB patients compared with healthy controls
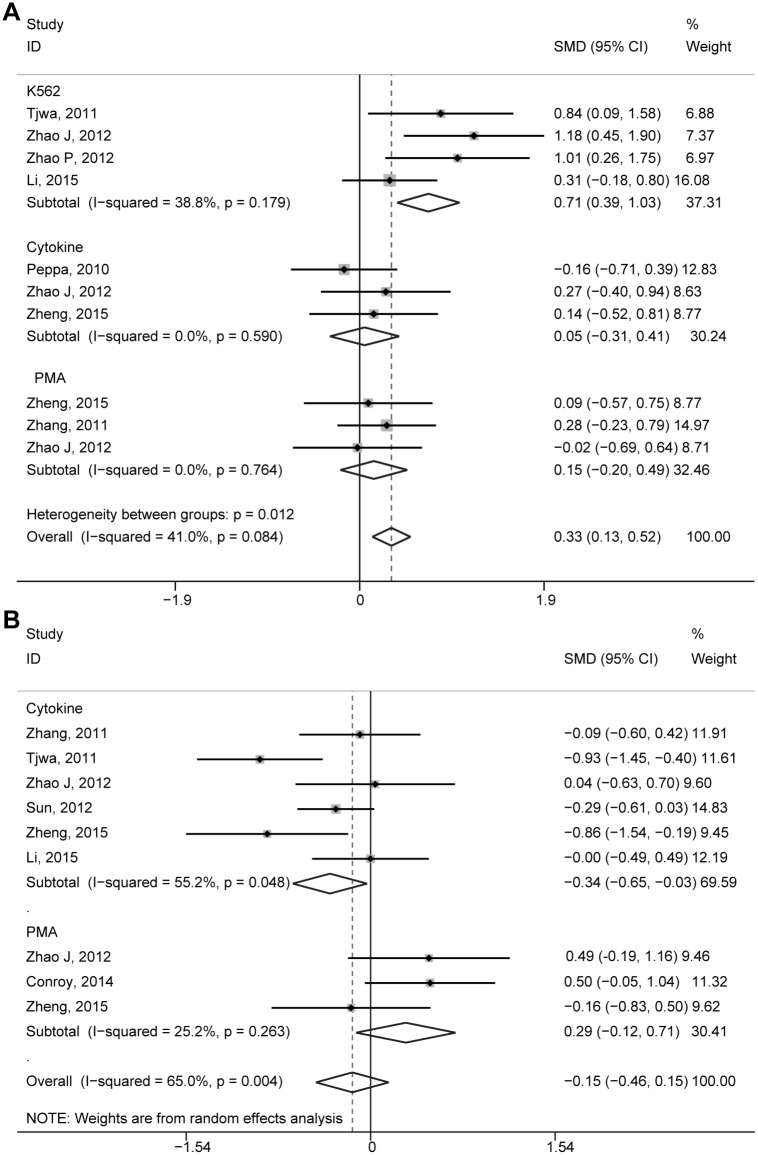
We evaluated the cytotoxicity of NK cells and IFNγ production to evaluate the function of NK cells in CHB patients relative to that of the healthy controls. A CD107a degranulation assay was performed as an indirect reflection of cytotoxicity, because it is now widely used to assess the cytotoxic potency of CD8 T-cells and NK cells [47, 48]. Seven studies reported CD107a degranulation of peripheral NK cells stimulated by major histocompatibility complex-devoid K562 target cells, cytokines, or mitogenic phorbol myristate acetate (PMA)/ionomycin. These studies included 400 CHB patients and 159 healthy controls. The total degranulation ability of NK cells was higher in CHB patients compared with the healthy controls (SMD = 0.33, 95% CI: 0.13 to 0.52, P = 0.001, I2 = 41.0%) and the fixed-effects model was applied (Fig 3A). This difference was more pronounced for peripheral NK cells stimulated by K562 cells (SMD = 0.71, 95% CI: 0.39 to 1.03, P = 0.000, I2 = 38.8%). However, the differences with healthy controls were not significant when NK cells were stimulated either with cytokines (SMD = 0.05, 95% CI: –0.31 to 0.41, P = 0.781, I2 = 0.0%) or PMA/ionomycin (SMD = 0.15, 95% CI: –0.20 to 0.49, P = 0.406, I2 = 0.0%). Seven studies, which included 480 CHB patients and 204 healthy controls, reported IFNγ production of peripheral NK cells stimulated by cytokines or PMA/ionomycin. Our data revealed that IFNγ production of NK cells was comparable in CHB patients compared with that in healthy controls (SMD = –0.15, 95% CI: –0.46 to 0.15, P = 0.323, I2 = 65.0%; Fig 3B). In the subgroup in which NK cells produced IFNγ in response to cytokines, NK cells in the CHB patients produced less IFNγ compared with the healthy controls (SMD = –0.34, 95% CI: –0.65 to -0.03, P = 0.032, I2 = 55.2%). Between these groups, IFNγ production was similar after simulation with PMA/ionomycin (SMD = –0.15, 95% CI: –0.12 to 0.71, P = 0.166, I2 = 25.2%). Taken together, our meta-analysis showed a functional dichotomy in CHB patients as their cytotoxic potency appeared to be elevated, whereas IFNγ secretion, an important non-cytolytic mechanism of virus control, was conserved.
Fig 3. Comparison of CD107a and IFNγ production of peripheral NK cells of CHB patients and healthy controls.
(A) Comparison of CD107a production of peripheral NK cells of CHB patients and healthy controls. (B) Comparison of IFNγ production of peripheral NK cells of CHB patients and healthy controls.
Publication bias
Begg’s and Egger’s tests were performed to assess the publication bias of the literature, and no evidence of publication bias was found (S3 Table).
Discussion
Our present work is the first attempt to review the literature and provide a comprehensive and extensive estimate of abnormal immune profiles of NK cells in CHB patients. We demonstrated that NK cells in CHB patients with a lower frequency displayed an active phenotype and exhibited a functional dichotomy featured by an increased cytotoxicity and a conserved cytokine production.
Concomitant with data reported in previous studies [36, 43], our meta-analysis suggests that, among CHB patients, there is a higher proportion of NK cells in the liver than in the peripheral blood. Zhang et al. [36] reported that decreased frequency of hepatic NK cells of CHB patients in immune active phase displayed an activated phenotype, and skewed toward cytolytic activity, but without a concomitant increase in IFNγ production, compared with healthy subjects. Since there is little information in the literature regarding hepatic NK cells, the differences in intrahepatic NK cells between CHB patients and healthy individuals has not been established. Despite the differences in the proportion and functional characteristics of NK cells in the liver and peripheral blood, persistent HBV infection can significantly influence peripheral NK cells, which can mirror alterations in intrahepatic NK cells [49]. Thus, most publications have assessed circulating NK cells, as these are more accessible and also easy to evaluate.
Our meta-analysis revealed that the frequency of circulating NK cells was lower in CHB patients compared with the healthy controls. Noticeably, the NK cell frequency in patients with minimal or no inflammation (ALT < 80 IU/L) or in immune-tolerant phase was comparable to that in healthy controls. This phenomenon might be a reflection of the time required to develop an effective and accurate immune response, from innate to adaptive immunity. In the early stage of HBV infection, the innate immune response is relatively strong. However, HBV-specific immune response is inefficient with anergy, deletion, and altered maturation of HBV-specific effector cells [50]. As a major component of the innate immune system, NK cells dominate the immune effector cell population in this phase and the distribution of NK cells resembles that seen in the normal liver [51]. With the development of adaptive immunity, the innate immune response is reduced [42].
The number of intrahepatic NK cells in immune tolerant phase is putatively higher than that during the immune active phase [33], further supporting the hypothesis above. Our data also confirm a significant reduction in the NK cells of CHB patients in the immune active phase, even though many of the eligible studies lacked the absolute number of NK cells required to perform a meta-analysis. The main reasons for the reduction in NK cells may be because, firstly, in HBV infections under proinflammatory conditions, NK cells are more susceptible to apoptosis [52]. In addition, the clear differences in NK cell frequencies strongly support that HBV itself, like the hepatitis C virus, may be able to significantly suppress the proliferation of NK cells [53–55]. Moreover, the reduced frequency of NK cells may result from the expansion of other cells, such as an increased number of dendritic cells, regulatory T-cells, and T helper 17 (Th17) cells [56–59].
As for NK subsets, increased frequency of CD56bright NK cells in CHB patients but no significant difference was found in CD56dim NK subsets. It is tempting to speculate that persistent HBV infection not only influences the frequency of peripheral NK cells but also modulates these subsets.
The present guidelines support both NUCs and Peg-IFN-α as first-line treatment options [20]. However, a satisfactory antiviral response has been achieved only in a minor population of patients treated with Peg-IFN-α, and the off-treatment durability of response to NUCs is generally low [20, 25, 26]. Since the immune response to CHB infection acts as a determinant of disease prognosis, a better understanding of the immune effect of anti-viral therapy is urgently needed. Despite the influence on the adaptive immune system, the effects of anti-viral therapy on innate effectors such as NK cells remain a strong concern [22–26]. Our results revealed that frequency of NK cells could not be adequately reversed by treatment with nucleotide inhibitors, although some studies have reported functional changes in NK cells [8, 9, 22, 38]. It has been previously shown that Peg-IFN-α therapy could drive the proliferation and expansion, in absolute numbers, of CD56bright NK cell numbers [26]. Tan et al. [25] reported that combined treatment of Peg-IFN-α and oral NUCs has a synergistic effect on innate parameters, such as NK cells, in CHB patients. To improve the therapeutic options for HBV, we need to explore further the immune basis by which HBV impairs anti-viral immune responses.
NK cells are essential effectors of the antiviral response in innate immunity, via the direct killing of infected cells, and produce a variety of antiviral and immunoregulatory cytokines. IFNγ is one of the main cytokines [10, 13, 15]. Furthermore, the functions of NK cells depend on a fine balance between activator and inhibitory receptors [15, 18, 60, 61]. Studies exploring the role of NK cells in persistent HBV infection in recent years have reported inconsistent results. Our results show CHB patients with a predominantly activating phenotype, featuring a higher percentage of NK cells expressing the activating receptors and a similar percentage of NK cells expressing the inhibitory receptors, compared with healthy controls. Because functional changes do not necessarily reflect altered function [62, 63], we subsequently analyzed the cytolytic potency of NK cells and cytokine production in CHB patients. Unexpectedly, in the present study NK activation did not induce all the effector cytotoxic functions of NK cells to an equal degree. NK function was characterized by enhanced cytolytic potency and conserved cytokine production. The results differed according to the stimulation applied to the NK cells. K562 was associated with increased levels, whereas cytokine or PMA/ionomycin resulted in CD107a levels in CHB patients similar to that of the healthy controls. NK cells produced less IFNγ after stimulation with cytokines compared with healthy controls. However, these results did not reach statistical significance when NK cells were stimulated with PMA/ionomycin.
In summary, our results suggest the existence of a selective defect in NK function. It is likely that the elevated NK cytolytic activity could contribute to liver injury, whereas concomitant inefficient IFNγ production may favor viral persistence, further promoting the progression of HBV infection. Such divergence of NK function is in accord with the recent finding that cytokines are trafficked and secreted by completely different pathways to cytotoxic granules in NK cells [64, 65]. And interleukin-10 (IL-10) and transforming growth factor-β (TGF-β) might participate in the pathways [22].
Nonetheless, one should be cautious when explaining these results due to the limitations of the included studies. A limitation in this meta-analysis is the failure to collect enough data regarding hepatic NK cells. We were unable to estimate the alteration of hepatic NK cells in CHB patients relative to healthy individuals. In addition, the optimal way to evaluate the immune profiles of NK cells in CHB patients is to compare CHB patients in each immune phase with healthy controls. Unfortunately, many of the eligible studies in this meta-analysis lacked the necessary information to perform these types of subgroup investigations. Thus, further high-quality studies are still needed to confirm these results.
Conclusions
The present meta-analysis revealed a lower frequency of NK cells with an activating phenotype in CHB patients. The functional dichotomy of NK cells was characterized by an enhanced cytotoxic potency and a conserved cytokine production, which may be an important mechanism contributing to liver injury and HBV persistence. Our meta-analysis draws a more precise estimation of the altered immune profiles of NK cells during CHB infection. This may further understanding of the mechanism of HBV persistence, and provide an insight into the challenge of our battle against hepatitis B infection for the future.
Supporting Information
(A) Comparison of hepatic NK cells VS peripheral NK cells in CHB patients with high heterogeneity; (B) Galbraith´s plots for publication heterogeneity for NK cells in liver VS in blood of CHB patients; (C) Comparison of hepatic NK cells VS peripheral NK cells in CHB patients without significant heterogeneity.
(DOC)
(DOC)
(DOCX)
(DOC)
(DOC)
(DOC)
(A) Quantitative Data of pooled frequency of peripheral NK cells on Bias. (B) Quantitative Data of pooled frequency of CD107a degranulation of NK cells on Bias. (C) Quantitative Data of pooled frequency of IFNγ production of NK cells on Bias.
(DOC)
Acknowledgments
We thank Medjaden for their useful language editing to improve the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by the National Natural Science Foundation of China (81171560, 309 30082, 81171561, 30972584), the National Science and Technology Major Project of China (200 8ZX10002-006, 2012ZX1002007001, 2011ZX09302005, 2012ZX09303001-001, 2012ZX100020 03), the National High Technology Research and Development Program of China (2011AA0 201 11), the Key Project of Chongqing Science and Technology Commission (cstc2012ggyyjsB10007), the Chongqing Natural Science Foundation (cstc2011jjA10025), and the Medical Research Fund by Chongqing Municipal Health Bureau (2009-1-71). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.McMahon BJ. Chronic hepatitis B virus infection. The Medical clinics of North America. 2014;98(1):39–54. Epub 2013/11/26. 10.1016/j.mcna.2013.08.004 . [DOI] [PubMed] [Google Scholar]
- 2.Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48(2):335–52. Epub 2007/12/22. 10.1016/j.jhep.2007.11.011 . [DOI] [PubMed] [Google Scholar]
- 3.Peng CY, Chien RN, Liaw YF. Hepatitis B virus-related decompensated liver cirrhosis: benefits of antiviral therapy. J Hepatol. 2012;57(2):442–50. Epub 2012/04/17. 10.1016/j.jhep.2012.02.033 . [DOI] [PubMed] [Google Scholar]
- 4.Matthews GV, Nelson MR. The management of chronic hepatitis B infection. International journal of STD & AIDS. 2001;12(6):353–7. Epub 2001/05/23. . [DOI] [PubMed] [Google Scholar]
- 5.Guidotti LG, Chisari FV. Immunobiology and pathogenesis of viral hepatitis. Annual review of pathology. 2006;1:23–61. Epub 2007/11/28. 10.1146/annurev.pathol.1.110304.100230 . [DOI] [PubMed] [Google Scholar]
- 6.Brechot C. Pathogenesis of hepatitis B virus-related hepatocellular carcinoma: old and new paradigms. Gastroenterology. 2004;127(5 Suppl 1):S56–61. Epub 2004/10/28. . [DOI] [PubMed] [Google Scholar]
- 7.Schwartz RH. T cell anergy. Annual review of immunology. 2003;21:305–34. Epub 2002/12/10. 10.1146/annurev.immunol.21.120601.141110 . [DOI] [PubMed] [Google Scholar]
- 8.Chen M, Sallberg M, Hughes J, Jones J, Guidotti LG, Chisari FV, et al. Immune tolerance split between hepatitis B virus precore and core proteins. J Virol. 2005;79(5):3016–27. Epub 2005/02/15. 10.1128/JVI.79.5.3016-3027.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. Functions of natural killer cells. Nature immunology. 2008;9(5):503–10. Epub 2008/04/22. 10.1038/ni1582 . [DOI] [PubMed] [Google Scholar]
- 10.Caligiuri MA. Human natural killer cells. Blood. 2008;112(3):461–9. Epub 2008/07/25. 10.1182/blood-2007-09-077438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doherty DG, O'Farrelly C. Innate and adaptive lymphoid cells in the human liver. Immunological reviews. 2000;174:5–20. Epub 2000/05/12. . [DOI] [PubMed] [Google Scholar]
- 12.Gregoire C, Chasson L, Luci C, Tomasello E, Geissmann F, Vivier E, et al. The trafficking of natural killer cells. Immunological reviews. 2007;220:169–82. Epub 2007/11/06. 10.1111/j.1600-065X.2007.00563.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper MA, Fehniger TA, Caligiuri MA. The biology of human natural killer-cell subsets. Trends in immunology. 2001;22(11):633–40. Epub 2001/11/08. . [DOI] [PubMed] [Google Scholar]
- 14.Oliviero B, Varchetta S, Paudice E, Michelone G, Zaramella M, Mavilio D, et al. Natural killer cell functional dichotomy in chronic hepatitis B and chronic hepatitis C virus infections. Gastroenterology. 2009;137(3):1151–60, 60, e1–7. Epub 2009/05/28. 10.1053/j.gastro.2009.05.047 . [DOI] [PubMed] [Google Scholar]
- 15.Mondelli MU, Varchetta S, Oliviero B. Natural killer cells in viral hepatitis: facts and controversies. European journal of clinical investigation. 2010;40(9):851–63. Epub 2010/07/06. 10.1111/j.1365-2362.2010.02332.x . [DOI] [PubMed] [Google Scholar]
- 16.Fisicaro P, Valdatta C, Boni C, Massari M, Mori C, Zerbini A, et al. Early kinetics of innate and adaptive immune responses during hepatitis B virus infection. Gut. 2009;58(7):974–82. Epub 2009/02/10. 10.1136/gut.2008.163600 . [DOI] [PubMed] [Google Scholar]
- 17.Webster GJ, Reignat S, Maini MK, Whalley SA, Ogg GS, King A, et al. Incubation phase of acute hepatitis B in man: dynamic of cellular immune mechanisms. Hepatology. 2000;32(5):1117–24. Epub 2000/10/26. 10.1053/jhep.2000.19324 . [DOI] [PubMed] [Google Scholar]
- 18.Rehermann B. Pathogenesis of chronic viral hepatitis: differential roles of T cells and NK cells. Nature medicine. 2013;19(7):859–68. Epub 2013/07/10. 10.1038/nm.3251 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maini MK, Peppa D. NK cells: a double-edged sword in chronic hepatitis B virus infection. Front Immunol. 2013;4:57 Epub 2013/03/06. 10.3389/fimmu.2013.00057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rehermann B, Bertoletti A. Immunological aspects of antiviral therapy of chronic hepatitis B virus and hepatitis C virus infections. Hepatology. 2014. Epub 2014/07/23. 10.1002/hep.27323 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rijckborst V, Sonneveld MJ, Janssen HL. Review article: chronic hepatitis B—anti-viral or immunomodulatory therapy? Alimentary pharmacology & therapeutics. 2011;33(5):501–13. Epub 2011/01/05. 10.1111/j.1365-2036.2010.04555.x . [DOI] [PubMed] [Google Scholar]
- 22.Peppa D, Micco L, Javaid A, Kennedy PT, Schurich A, Dunn C, et al. Blockade of immunosuppressive cytokines restores NK cell antiviral function in chronic hepatitis B virus infection. PLoS Pathog. 2010;6(12):e1001227 10.1371/journal.ppat.1001227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lv J, Jin Q, Sun H, Chi X, Hu X, Yan H, et al. Antiviral treatment alters the frequency of activating and inhibitory receptor-expressing natural killer cells in chronic hepatitis B virus infected patients. Mediators Inflamm. 2012;2012:804043 Epub 2013/01/11. 10.1155/2012/804043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao PW, Jia FY, Shan YX, Ji HF, Feng JY, Niu JQ, et al. Downregulation and altered function of natural killer cells in hepatitis B virus patients treated with entecavir. Clinical and experimental pharmacology & physiology. 2013;40(3):190–6. Epub 2013/01/03. 10.1111/1440-1681.12048 . [DOI] [PubMed] [Google Scholar]
- 25.Tan AT, Hoang LT, Chin D, Rasmussen E, Lopatin U, Hart S, et al. Reduction of HBV replication prolongs the early immunological response to IFNalpha therapy. J Hepatol. 2014;60(1):54–61. Epub 2013/09/03. 10.1016/j.jhep.2013.08.020 . [DOI] [PubMed] [Google Scholar]
- 26.Micco L, Peppa D, Loggi E, Schurich A, Jefferson L, Cursaro C, et al. Differential boosting of innate and adaptive antiviral responses during pegylated-interferon-alpha therapy of chronic hepatitis B. J Hepatol. 2013;58(2):225–33. Epub 2012/10/11. 10.1016/j.jhep.2012.09.029 . [DOI] [PubMed] [Google Scholar]
- 27.Wells G, Shea B, O’connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000.
- 28.Petitti DB. Approaches to heterogeneity in meta-analysis. Statistics in medicine. 2001;20(23):3625–33. Epub 2001/12/18. . [DOI] [PubMed] [Google Scholar]
- 29.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled clinical trials. 1986;7(3):177–88. Epub 1986/09/01. . [DOI] [PubMed] [Google Scholar]
- 30.Thompson SG, Higgins JP. How should meta-regression analyses be undertaken and interpreted? Statistics in medicine. 2002;21(11):1559–73. Epub 2002/07/12. 10.1002/sim.1187 . [DOI] [PubMed] [Google Scholar]
- 31.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. Epub 1997/10/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yan MX, Mao HT, Liu Q, Wang WQ, Li YQ. Elevated levels of serum soluble E-selectin in patients with chronic hepatitis B: Correlation with T lymphocyte subsets, NK cells and liver inflammation. Hepatol Res. 2006;35(2):111–7. Epub 2006/05/03. 10.1016/j.hepres.2006.03.006 . [DOI] [PubMed] [Google Scholar]
- 33.Sprengers D, van der Molen RG, Kusters JG, Hansen B, Niesters HG, Schalm SW, et al. Different composition of intrahepatic lymphocytes in the immune-tolerance and immune-clearance phase of chronic hepatitis B. Journal of medical virology. 2006;78(5):561–8. Epub 2006/03/24. 10.1002/jmv.20576 . [DOI] [PubMed] [Google Scholar]
- 34.Gu XB, Yang XJ, Wang D, Hua Z, Xu YQ, Lu ZH. Relationship between serum HBV DNA level and HBV-specific, nonspecific cytotoxic T lymphocytes and natural killer cells in patients with chronic hepatitis B. Chinese medical journal. 2009;122(18):2129–32. Epub 2009/09/29. . [PubMed] [Google Scholar]
- 35.Bonorino P, Ramzan M, Camous X, Dufeu-Duchesne T, Thelu MA, Sturm N, et al. Fine characterization of intrahepatic NK cells expressing natural killer receptors in chronic hepatitis B and C. J Hepatol. 2009;51(3):458–67. Epub 2009/07/15. 10.1016/j.jhep.2009.05.030 . [DOI] [PubMed] [Google Scholar]
- 36.Zhang Z, Zhang S, Zou Z, Shi J, Zhao J, Fan R, et al. Hypercytolytic activity of hepatic natural killer cells correlates with liver injury in chronic hepatitis B patients. Hepatology. 2011;53(1):73–85. Epub 2011/01/22. 10.1002/hep.23977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tjwa ET, van Oord GW, Hegmans JP, Janssen HL, Woltman AM. Viral load reduction improves activation and function of natural killer cells in patients with chronic hepatitis B. J Hepatol. 2011;54(2):209–18. 10.1016/j.jhep.2010.07.009 . [DOI] [PubMed] [Google Scholar]
- 38.Zhao J, Li Y, Jin L, Zhang S, Fan R, Sun Y, et al. Natural killer cells are characterized by the concomitantly increased interferon-gamma and cytotoxicity in acute resolved hepatitis B patients. PLoS One. 2012;7(11):e49135 Epub 2012/11/08. 10.1371/journal.pone.0049135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li F, Wei H, Wei H, Gao Y, Xu L, Yin W, et al. Blocking the natural killer cell inhibitory receptor NKG2A increases activity of human natural killer cells and clears hepatitis B virus infection in mice. Gastroenterology. 2013;144(2):392–401. 10.1053/j.gastro.2012.10.039 . [DOI] [PubMed] [Google Scholar]
- 40.Sun C, Fu B, Gao Y, Liao X, Sun R, Tian Z, et al. TGF-beta1 down-regulation of NKG2D/DAP10 and 2B4/SAP expression on human NK cells contributes to HBV persistence. PLoS Pathog. 2012;8(3):e1002594 10.1371/journal.ppat.1002594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lunemann S, Malone DF, Hengst J, Port K, Grabowski J, Deterding K, et al. Compromised function of natural killer cells in acute and chronic viral hepatitis. The Journal of infectious diseases. 2014;209(9):1362–73. 10.1093/infdis/jit561 . [DOI] [PubMed] [Google Scholar]
- 42.Li Y, Wang JJ, Gao S, Liu Q, Bai J, Zhao XQ, et al. Decreased peripheral natural killer cells activity in the immune activated stage of chronic hepatitis B. PLoS One. 2014;9(2):e86927 Epub 2014/02/13. 10.1371/journal.pone.0086927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tjwa ET, Zoutendijk R, van Oord GW, Biesta PJ, Verheij J, Janssen HL, et al. Intrahepatic natural killer cell activation, but not function, is associated with HBsAg levels in patients with HBeAg-negative chronic hepatitis B. Liver Int. 2014;34(3):396–404. 10.1111/liv.12272 . [DOI] [PubMed] [Google Scholar]
- 44.Conroy MJ, Mac Nicholas R, Grealy R, Taylor M, Otegbayo JA, O'Dea S, et al. Circulating CD56dim natural killer cells and CD56+ T cells that produce interferon-gamma or interleukin-10 are expanded in asymptomatic, E antigen-negative patients with persistent hepatitis B virus infection. Journal of viral hepatitis. 2015;22(3):335–45. 10.1111/jvh.12299 . [DOI] [PubMed] [Google Scholar]
- 45.Zheng Q, Zhu YY, Chen J, Ye YB, Li JY, Liu YR, et al. Activated natural killer cells accelerate liver damage in patients with chronic hepatitis B virus infection. Clin Exp Immunol. 2015;180(3):499–508. 10.1111/cei.12597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li W, Jiang Y, Wang X, Jin J, Qi Y, Chi X, et al. Natural Killer p46 Controls Hepatitis B Virus Replication and Modulates Liver Inflammation. PLoS One. 2015;10(8):e0135874 Epub 2015/08/21. 10.1371/journal.pone.0135874 ; PubMed Central PMCID: PMCPmc4546267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rehermann B, Naoumov NV. Immunological techniques in viral hepatitis. J Hepatol. 2007;46(3):508–20. Epub 2007/01/24. 10.1016/j.jhep.2007.01.002 . [DOI] [PubMed] [Google Scholar]
- 48.Betts MR, Brenchley JM, Price DA, De Rosa SC, Douek DC, Roederer M, et al. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J Immunol Methods. 2003;281(1–2):65–78. Epub 2003/10/29. . [DOI] [PubMed] [Google Scholar]
- 49.Guidotti LG, Rochford R, Chung J, Shapiro M, Purcell R, Chisari FV. Viral clearance without destruction of infected cells during acute HBV infection. Science. 1999;284(5415):825–9. Epub 1999/04/30. . [DOI] [PubMed] [Google Scholar]
- 50.Carey I, D'Antiga L, Bansal S, Longhi MS, Ma Y, Mesa IR, et al. Immune and viral profile from tolerance to hepatitis B surface antigen clearance: a longitudinal study of vertically hepatitis B virus-infected children on combined therapy. J Virol. 2011;85(5):2416–28. Epub 2010/12/15. 10.1128/jvi.01449-10 ; PubMed Central PMCID: PMCPmc3067801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Norris S, Collins C, Doherty DG, Smith F, McEntee G, Traynor O, et al. Resident human hepatic lymphocytes are phenotypically different from circulating lymphocytes. J Hepatol. 1998;28(1):84–90. Epub 1998/04/16. . [DOI] [PubMed] [Google Scholar]
- 52.Schierloh P, Yokobori N, Aleman M, Musella RM, Beigier-Bompadre M, Saab MA, et al. Increased susceptibility to apoptosis of CD56dimCD16+ NK cells induces the enrichment of IFN-gamma-producing CD56bright cells in tuberculous pleurisy. Journal of immunology. 2005;175(10):6852–60. Epub 2005/11/08. . [DOI] [PubMed] [Google Scholar]
- 53.Crotta S, Stilla A, Wack A, D'Andrea A, Nuti S, D'Oro U, et al. Inhibition of natural killer cells through engagement of CD81 by the major hepatitis C virus envelope protein. J Exp Med. 2002;195(1):35–41. Epub 2002/01/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tseng CT, Klimpel GR. Binding of the hepatitis C virus envelope protein E2 to CD81 inhibits natural killer cell functions. J Exp Med. 2002;195(1):43–9. Epub 2002/01/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pileri P, Uematsu Y, Campagnoli S, Galli G, Falugi F, Petracca R, et al. Binding of hepatitis C virus to CD81. Science. 1998;282(5390):938–41. Epub 1998/10/30. . [DOI] [PubMed] [Google Scholar]
- 56.Zhang Z, Chen D, Yao J, Zhang H, Jin L, Shi M, et al. Increased infiltration of intrahepatic DC subsets closely correlate with viral control and liver injury in immune active pediatric patients with chronic hepatitis B. Clin Immunol. 2007;122(2):173–80. Epub 2006/10/21. 10.1016/j.clim.2006.09.006 . [DOI] [PubMed] [Google Scholar]
- 57.Zhang Z, Zou ZS, Fu JL, Cai L, Jin L, Liu YJ, et al. Severe dendritic cell perturbation is actively involved in the pathogenesis of acute-on-chronic hepatitis B liver failure. J Hepatol. 2008;49(3):396–406. Epub 2008/07/23. 10.1016/j.jhep.2008.05.017 . [DOI] [PubMed] [Google Scholar]
- 58.Xu D, Fu J, Jin L, Zhang H, Zhou C, Zou Z, et al. Circulating and liver resident CD4+CD25+ regulatory T cells actively influence the antiviral immune response and disease progression in patients with hepatitis B. Journal of immunology. 2006;177(1):739–47. Epub 2006/06/21. . [DOI] [PubMed] [Google Scholar]
- 59.Zhang JY, Zhang Z, Lin F, Zou ZS, Xu RN, Jin L, et al. Interleukin-17-producing CD4(+) T cells increase with severity of liver damage in patients with chronic hepatitis B. Hepatology. 2010;51(1):81–91. Epub 2009/10/21. 10.1002/hep.23273 . [DOI] [PubMed] [Google Scholar]
- 60.Raulet DH. Roles of the NKG2D immunoreceptor and its ligands. Nature reviews Immunology. 2003;3(10):781–90. Epub 2003/10/03. 10.1038/nri1199 . [DOI] [PubMed] [Google Scholar]
- 61.Mandelboim O, Lieberman N, Lev M, Paul L, Arnon TI, Bushkin Y, et al. Recognition of haemagglutinins on virus-infected cells by NKp46 activates lysis by human NK cells. Nature. 2001;409(6823):1055–60. Epub 2001/03/10. 10.1038/35059110 . [DOI] [PubMed] [Google Scholar]
- 62.Morishima C, Paschal DM, Wang CC, Yoshihara CS, Wood BL, Yeo AE, et al. Decreased NK cell frequency in chronic hepatitis C does not affect ex vivo cytolytic killing. Hepatology. 2006;43(3):573–80. [DOI] [PubMed] [Google Scholar]
- 63.Golden-Mason L, Madrigal-Estebas L, McGrath E, Conroy MJ, Ryan EJ, Hegarty JE, et al. Altered natural killer cell subset distributions in resolved and persistent hepatitis C virus infection following single source exposure. Gut. 2008;57(8):1121–8. Epub 2008/03/29. 10.1136/gut.2007.130963 . [DOI] [PubMed] [Google Scholar]
- 64.Reefman E, Kay JG, Wood SM, Offenhauser C, Brown DL, Roy S, et al. Cytokine secretion is distinct from secretion of cytotoxic granules in NK cells. Journal of immunology. 2010;184(9):4852–62. Epub 2010/04/07. 10.4049/jimmunol.0803954 . [DOI] [PubMed] [Google Scholar]
- 65.Kim N, Saudemont A, Webb L, Camps M, Ruckle T, Hirsch E, et al. The p110delta catalytic isoform of PI3K is a key player in NK-cell development and cytokine secretion. Blood. 2007;110(9):3202–8. Epub 2007/07/24. 10.1182/blood-2007-02-075366 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Comparison of hepatic NK cells VS peripheral NK cells in CHB patients with high heterogeneity; (B) Galbraith´s plots for publication heterogeneity for NK cells in liver VS in blood of CHB patients; (C) Comparison of hepatic NK cells VS peripheral NK cells in CHB patients without significant heterogeneity.
(DOC)
(DOC)
(DOCX)
(DOC)
(DOC)
(DOC)
(A) Quantitative Data of pooled frequency of peripheral NK cells on Bias. (B) Quantitative Data of pooled frequency of CD107a degranulation of NK cells on Bias. (C) Quantitative Data of pooled frequency of IFNγ production of NK cells on Bias.
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.