Abstract
Background
HIV infection is clinically managed with antiretroviral therapy (ART), but only with sustained adherence. Cost-efficient interventions to improve and sustain ART adherence remain a pressing priority for populations challenged by non-adherence.
Purpose
To test the independent and interactive effects of (a) brief phone-delivered self-regulation counseling and (b) daily phone-delivered text message medication reminders on HIV adherence and HIV viral suppression.
Method
A randomized 2 (5-sessions of phone-delivered adherence support counseling vs. contact-matched control) × 2 (daily ART text reminders vs. no reminders) trial with primary endpoints of monthly phone-based unannounced pill count-determined ART adherence and HIV viral suppression monitored over 12-months.
Results
Self-regulation adherence counseling demonstrated significant improvements in achieving 90% ART adherence relative to the control group over the first 6-months of follow-up. Effects remained significant in sensitivity analyses conducted at 85% and 95% adherence. Counseling also demonstrated modest but significant effects on HIV suppression. There were no main effects or interactions for daily text message reminders, with some evidence for adverse effects on adherence self-efficacy.
Conclusions
Brief adherence support counseling delivered by phone demonstrates clinically meaningful improvements in ART adherence and HIV suppression, although these benefits were not evidenced in all patients or in the long-term. Advancing adherence interventions along with an effective means for sustaining gains in adherence remain priorities if ART is to achieve its potential clinical and public health benefits.
Keywords: HIV Treatment, Adherence, Self-regulation counseling, Adherence support, Counseling, mHealth, Behavioral intervention
Introduction
Antiretroviral therapy (ART) has the potential to transform HIV infection into a manageable chronic illness and to slow HIV epidemics. But many people with HIV are not reaping the full benefits of ART (1). People living with HIV in the US often remain untreated and a significant number of those treated have unsuppressed virus (2, 3). Among the reasons for these missed opportunities is the challenge of achieving and sustaining HIV suppression through optimal ART adherence. Many people living with HIV require more frequent monitoring and greater support than is possible with routine clinic visits. In addition, there is evidence that patients who live in poverty are in even greater need of adherence assistance with fewer available resources (4).
Few interventions result in significant impacts on ART adherence, and even fewer demonstrate effects on HIV suppression (5). One exception has been supportive behavioral adherence counseling (6). Brief phone-delivered adherence counseling offers an approach to delivering low-cost and effective medication adherence interventions (7), with positive outcomes reported in managing multiple chronic conditions (8-12). Adherence counseling focuses on patient education, self-monitoring, direct patient feedback, and individualized problem solving (13).
Behavioral counseling grounded in Self-Regulation Theory and delivered by phone has shown particular promise for improving ART adherence (14-16). Although phone-delivered self-regulation counseling may improve adherence, studies repeatedly find patients faced with challenges to maintaining adherence over the long-term. A solution to sustained adherence may be short message service (SMS) text message reminders (17, 18), although the evidence is mixed for the effectiveness of various models (19, 20). Interventions designed to capitalize on low-cost mobile text message reminders to support adherence are promising (21), but have not been tested as a means of sustaining improvements in medication adherence following behavioral counseling.
In the current study, people living with HIV who demonstrated poor ART adherence were randomized in a 2 × 2 factorial design to test two independent interventions: (a) 5-sessions of brief bi-weekly adherence self-regulation counseling compared to a contact-matched control condition and (b) daily reminder text messages compared to no reminders. We hypothesized that the main effect for counseling as well as the counseling × text message reminder interaction would significantly improve ART adherence and HIV suppression relative to the control conditions. We also hypothesized that self-regulation processes of adherence self-efficacy and use of adherence strategies would mediate the counseling effects.
Methods
Participants and setting
Participants were 600 men and women recruited from infectious disease clinics throughout Atlanta, GA. Enrollment occurred between August 2011 and February 2014, and follow-ups were completed March 2015. Potential participants were screened for inclusion in an adherence-determining run-in period using the entry criteria: age 18 or older, receiving ART and self-reported less than 95% adherent in the past month as per a validated visual analogue adherence scale (22). Participants in the run-in period completed one-month of phone-based unannounced pill counts to determine trial eligibility, < 95% ART adherence. All study protocols were approved by the Connecticut Institutional Review Board and was registered in the clinical trials registry clinicaltrials.gov (NCT01359280).
Sample size
Sample size was determined by effect sizes observed from pilot study effects (15), previous research (14), and meta-analyses (16, 23). Moderate effect sizes were estimated for ART adherence and viral load, d = 59, d = .45, respectively. We assumed 80% retention and estimated 150 participants in each study arm (N = 600) to achieve 90% chance of detecting differences in main effects of counseling and text reminders, as well as 80% for the counseling × text reminders interaction.
Recruitment and enrollment
We notified AIDS service providers and infectious disease clinics in Atlanta about the research opportunity and placed study brochures in waiting rooms. Interested persons phoned the research site to schedule an intake appointment. Individuals with adherence below 95% of ART confirmed during a one month run-in period measured by unannounced phone-based pill counts were recruited for participation in the trial. We selected 95% adherence as the cut-off to screen out individuals with optimal ART adherence while limiting false negatives. The only additional study entry criteria was age 18 or older.
Randomization and blinding
Participants were randomly assigned to conditions following informed consent, baseline assessments, training in phone operations and pill counting procedures. Allocation was accomplished by a project manager using a computer generated simple randomization scheme. Two participants living together and sharing adherence tools were assigned as a couple to avoid contamination. Recruitment, screening, and office-based assessment staff remained blinded to condition throughout the study and adherence counselors never conducted outcome assessments.
Intervention Conditions
Adherence support counseling
The experimental adherence counseling in this study was based on Self-Regulation Theory (24, 25) and was pilot tested (15). Self-Regulation Theory posits that adherence is directly influenced by illness experiences (e.g., symptoms, medication side effects), social interactions, sources of information, and cognitive/affective processes. The phone delivered intervention was framed around corrective feedback and was delivered by an adherence counselor using techniques commonly employed in motivational interviewing (26). The initial session was conducted in a 45-minute face-to-face office visit and included information on how HIV impacts the immune system, how ART slows the progression of HIV disease, and developing a personalized adherence plan that included overcoming barriers to taking medications and creating a profile of times and dosing. The four subsequent biweekly counseling sessions occurred by phone. Each session began with a pill count followed by the counselor calculating adherence while on the phone and delivering immediate corrective feedback. Participants who were greater than or equal to 95% ART adherent according to the counseling-session pill count were reinforced and established a plan for remaining adherent. The counselor probed the participant regarding challenges he/she faced and decisions made about their medications over the previous two weeks.
Participants who were less than 95% adherent systematically worked through missed doses and problem solved barriers encountered. The counselor provided participants with feedback on their adherence and asked about the circumstances of their most recent missed medication. Challenges identified by the participant were subjected to a problem solving scheme that entailed an action plan for maintaining adherence under similar circumstances in the future. The adherence counselor specifically revisited past challenges and action plans at subsequent sessions. The final session ended with a detailed plan for participants to self-monitor and sustain their adherence.
Contact matched counseling control condition
The counseling control arm was a contact-matched non-contaminating health improvement intervention. This condition concentrated on improving general health and well-being in relation to living with HIV/AIDS. The structure and frequency of the control counseling mirrored the self-regulation adherence counseling.
Daily text message reminders
Upon completion of the adherence support and control phone counseling sessions, half of participants in each of these conditions were randomized to receive text message reminders for up to two daily medication times and half did not receive any additional intervention. The content of the text message was generated by the participant. Text messages were delivered to participants' personal and/or study phone by an automated system and signaled a light flashing, sound, and vibration upon delivery. Participants were trained in phone operations, including silencing all alert functions.
Measures
During the run-in period, all participants completed informed consent and audio-computer assisted structured interviews (ACASI) for demographic and health characteristics (27). All follow-up assessments were conducted using phone interviews.
Primary Outcomes
ART adherence
HIV treatment adherence was monitored with monthly unannounced phone-based pill counts. Note that these assessments were conducted independent of counseling which included its own intervention adherence monitoring. The counselors and assessors never discussed participant adherence. Unannounced pill counts are reliable and valid when conducted in participants' homes and on the phone (28, 29). Participants were provided with a phone that restricted service for project contacts and emergency use and were called at unscheduled times to count their pills during baseline and for 12 consecutive months. These procedures have been validated in previous research (29). Pharmacy information from pill bottles was collected to verify number of pills dispensed between calls. Adherence was calculated as the ratio of pills counted relative to pills prescribed taking into account the number dispensed.
HIV RNA viral load
We used a participant assisted method for collecting baseline chart abstracted viral load and CD4 cell counts from medical records. Participants were given a form that requested their doctor's office to provide results and dates of their most recent viral load and CD4 cell counts that included the provider's office stamp or signature to assure authenticity.
To determine HIV RNA concentrations at the 12-month follow-up, participants provided blood specimens to test for HIV (RNA) viral load. Blood samples were drawn at the project office using standard phlebotomy and couriered to a university lab for processing. Whole blood specimens in EDTA tube (Becton Dickinson) were centrifuged at 500 g for 10 min within 4 hours of collection. The plasma was recovered and aliquoted into 1 ml samples and stored at -70°C. For consistency across assays and baseline chart values, we defined viral suppression as < 100 copies/ml.
Secondary outcomes
Medication adherence self-efficacy
Based on theories of health behavior change (30) we used a measure of self-efficacy that allowed participants to judge how confident they were that they could take their medications in various situations (31). The scale consists of eight circumstances that potentially challenge adherence. The items varied in social relationships, affective states, and settings and were responded to using an 11-point ascending confidence scale, with responses 0 = “Not at all certain” to 10 = “Very certain”, alpha = .88.
Behavioral adherence strategies
Participants indicated whether they had used 14 common strategies for improving medication adherence. We asked about monthly use of a broad array of adherence strategies identified from previous research (32, 33), alpha = .70.
Counselor training
Interventionists were female Bachelors-level counselors with experience working in AIDS services. Counselors represented the skills and professional background that are common in clinics such as adherence nurses and case managers. The counselors were trained in the protocols and supervised weekly.
Statistical analyses
We first examined differences between conditions on demographic and health characteristics using analyses of variance (ANOVA) for continuous measures and contingency table chi-square tests for categorical variables. We also used procedures suggested by Jurs and Glass (34) to test baseline equivalence between conditions and effects of attrition on dependent measures.
Primary and secondary outcome analyses used an intent-to-treat approach where all available follow-up data from participants was included in the analyses regardless of their exposure to intervention sessions. Primary outcome analyses for adherence used generalized estimating equations (GEE) with unstructured working correlation matrixes. All outcome analyses controlled for baseline values (35). Counseling condition, text message condition, time of assessment, and all interactions were entered as model effects. Adherence outcomes represent over-dispersed count data and therefore used Poisson distribution. Adherence values were also dichotomized as below and above 90% ART taken over the course of the month at each assessment point. We also examined adherence using 85% and 95% cut-offs for sensitivity analyses. For viral load outcomes, we performed logistic regressions coding viral load as detectable (≥ 100 copies) = 1 / undetectable (< 100 copies) = 0. We tested all conditions in an omnibus model to initially determine proportional differences followed by subsequent models for main effects and interactions. Secondary outcomes for adherence self-efficacy and adherence strategies assessed at alternating post-intervention phone assessments (post-counseling months 2, 4, 6, 8 and 10) were analyzed in the full factorial model using repeated measures generalized linear models (GLM) with continuous linear distributions controlling for baseline scores.
To test whether ART adherence self-efficacy and adherence strategies mediated the intervention effects, we conducted multiple mediation models for time points that demonstrated intervention effects on adherence. We used methods described by Baron and Kenny (36) and the Process Macro designed by Preacher and Hayes (37). We computed 95% confidence intervals (CI) for the indirect effects of counseling on ART adherence self-efficacy and strategies estimated from 5,000 bootstrap resamples. All analyses controlled for baselines and defined statistical significance as p < .05.
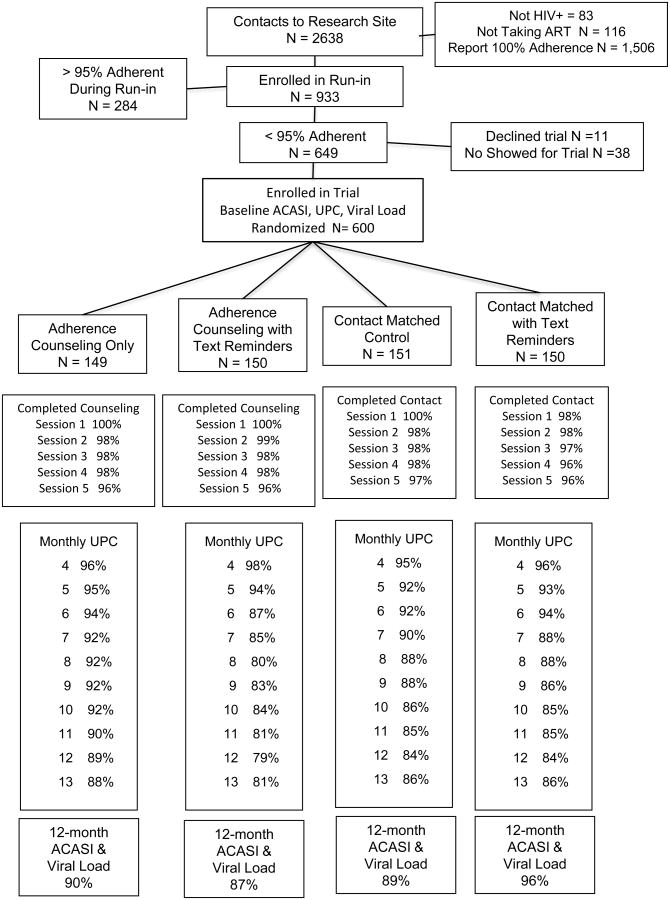
Results
Figure 1 shows the complete study retention rates and Table 1 shows the demographic and health characteristics of participants allocated to each of the four conditions. All participants met the entry criteria of < 95% ART adherent on unannounced phone-based pill counts in the run-in period; 82% were < 90% and 61% were less than 85% adherent at baseline. One in four (24%) participants had unsuppressed HIV RNA (≥100 copies/ml) at baseline. Baseline comparisons demonstrated that there were no significant differences between intervention conditions on any demographic/health characteristics or outcome variables. Retention at 12-months follow-up was 90% and was evenly distributed across conditions. The randomization and retention procedures therefore resulted in balanced conditions without observed biases. There were no intervention-associated adverse events.
Figure 1.
Flow chart of participants in the randomized trial of self-regulation counseling and daily text reminders to improve ART adherence and HIV suppression.
Table 1.
Baseline demographic and health characteristics of clinical trial participants across four conditions.
| Characteristic | Adherence Counseling (N = 149) | Adherence Counseling + Reminders (N = 150) | Contact Matched Control (N = 151) | Contact Matched + Reminders (N = 150) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| M | SD | M | SD | M | SD | M | SD | |
| Age | 47.8 | 9.9 | 47.0 | 9.1 | 46.8 | 10.0 | 46.8 | 9.0 |
| Years of education | 12.6 | 1.7 | 12.7 | 1.7 | 12.5 | 1.8 | 12.5 | 1.8 |
| Years since testing HIV+ | 15.2 | 7.3 | 15.2 | 7.3 | 15.1 | 8.1 | 15.8 | 8.1 |
| HIV symptoms | 3.9 | 3.5 | 3.8 | 3.3 | 3.9 | 3.4 | 4.1 | 3.4 |
| ART Side effects | 5.3 | 4.9 | 5.0 | 5.4 | 5.3 | 4.8 | 5.7 | 4.8 |
| CD4 cell count | 487.2 | 322.0 | 437.1 | 252.3 | 434.2 | 262.2 | 471.8 | 470.3 |
| Adherence self-efficacy | 7.6 | 2.1 | 7.5 | 1.8 | 7.7 | 1.8 | 7.7 | 1.8 |
| Adherence Strategies | 5.7 | 2.9 | 5.9 | 2.8 | 5.7 | 3.0 | 5.9 | 2.8 |
|
|
||||||||
| N | % | N | % | N | % | N | % | |
|
|
||||||||
| Men | 114 | 76 | 112 | 75 | 97 | 64 | 105 | 70 |
| Women | 35 | 24 | 38 | 25 | 54 | 36 | 45 | 30 |
| Transgender identity | 11 | 7 | 7 | 5 | 14 | 9 | 9 | 6 |
| African-American | 140 | 94 | 144 | 96 | 141 | 93 | 142 | 95 |
| Receives disability | 93 | 62 | 89 | 59 | 83 | 55 | 82 | 55 |
| Income < $10,000 year | 94 | 63 | 101 | 67 | 109 | 72 | 89 | 60 |
| CD4 count < 200 cell/cc | 30 | 20 | 27 | 18 | 26 | 17 | 35 | 23 |
| Lacks transportation | 80 | 53 | 77 | 51 | 79 | 52 | 90 | 60 |
| Alcohol use in past month | 79 | 53 | 82 | 55 | 82 | 54 | 99 | 66 |
| CESD Score > 16 | 72 | 48 | 70 | 46 | 71 | 47 | 74 | 49 |
| ART adherence < 85% | 81 | 54 | 96 | 54 | 100 | 66 | 87 | 58 |
| ART adherence < 90% | 115 | 77 | 125 | 84 | 127 | 85 | 123 | 82 |
| HIV RNA < 100 copies/mL | 116 | 78 | 109 | 73 | 120 | 79 | 113 | 75 |
Note: No significant differences between conditions were detected across groups on any baseline characteristics.
Primary Outcomes: ART Adherence
Results of the 2 × 2 factorial GEE model using the continuous adherence values with repeated monthly assessments and controlling for baseline, indicated a significant effect of counseling condition over time, Wald X2 = 26.83, p < .01. There was no effect of text messaging and the counseling × text messaging interaction was not significant. Table 2 shows the number and percent of participants achieving 90% adherence at each of the post-counseling phone-based unannounced pill counts (baseline shown in Table 1). GEE modeling was consistent with the analysis of continuous adherence values demonstrating significant effects of counseling over time, controlling for baseline, Wald X2 = 17.78, p < .05. Post hoc tests showed that more participants in the adherence counseling condition had achieved 90% adherence at 1, 2, 3, and 6-months post counseling. Again, both the text messaging main effect and the counseling × text messaging interaction were not significant. In sensitivity tests, at the upper bound of 95% adherence, the effect of counseling remained significant, Wald X2 = 26.41, p < .01. Differences between counseling conditions were significant at the 1, 2, 3, and 6-month follow-ups, with no effects for text messaging and no counseling × text messaging interaction. The lower bound of 85% adherence showed the same pattern, with only an effect for counseling condition, Wald X2 = 15.29, p < .08, with significant differences at 1, 2 and 6-months.
Table 2.
Proportion of participants achieving 90% adherence at baseline and follow-up unannounced pill counts for the four intervention conditions.
| Time Post Counseling | Adherence Counseling | Adherence Counseling + Reminders | Contact Matched Control | Contact Matched + Reminders | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| (N = 149) | (N = 150) | (N = 151) | (N = 150) | |||||
| N | % | N | % | N | % | N | % | |
| 1-month | 79 | 54 | 80 | 54 | 61 | 42 | 60 | 41 |
| 2-months | 77 | 54 | 80 | 57 | 59 | 42 | 56 | 40 |
| 3-months | 69 | 49 | 60 | 45 | 47 | 33 | 57 | 40 |
| 4-months | 73 | 53 | 53 | 41 | 57 | 41 | 54 | 40 |
| 5-months | 63 | 46 | 58 | 48 | 58 | 43 | 63 | 48 |
| 6-months | 63 | 45 | 62 | 50 | 54 | 41 | 49 | 36 |
| 7-months | 59 | 42 | 55 | 43 | 53 | 40 | 55 | 43 |
| 8-months | 63 | 46 | 53 | 43 | 49 | 38 | 55 | 43 |
| 9-months | 56 | 41 | 49 | 41 | 53 | 41 | 52 | 41 |
| 10 months | 57 | 43 | 52 | 43 | 55 | 42 | 44 | 34 |
| HIV RNA < 100 copies/ml | ||||||||
| 10-months | 108 | 79 | 104 | 79 | 98 | 73 | 110 | 76 |
Note: Counseling occurred over two months. The 10 month post counseling reflects 12-months from baseline.
HIV Suppression
Logistic regression models conducted on detectable/undetectable blood plasma viral load as the dependent measure with the four intervention conditions entered as the omnibus predictor variable and controlling for baseline indicated a significant effect for counseling, OR = 1.24, 95% CI(1.01-1.52), p < .05 (see Table 2, baseline shown in Table 1). Adherence counseling demonstrated significantly greater viral suppression at the follow-up than control participants, OR = 1.23, CI(1.01-1.51), p < .05. The text messaging effect and counseling × text messaging interaction were not significant.
Secondary Outcomes: Adherence Self-Efficacy and Strategies
Table 3 shows the means for adherence self-efficacy scores (upper panel) and adherence strategies (lower panel). For self-efficacy, results indicated a significant main effect of counseling, Wilks' λ = 0.98, F(4, 471) = 2.41, p <.05; participants receiving counseling demonstrated significantly greater adherence self-efficacy over time. Post hoc tests indicated the differences between conditions were significant at 2, 4, and 6-month follow-ups, but not at 8 and 10-months. There was also a main effect for text messaging on adherence self-efficacy, Wilks' λ = 0.97, F(4, 471) = 2.51, p <.05; counter to intended outcomes participants who received daily text message reminders demonstrated poorer self-efficacy for ART adherence over time. Post hoc tests showed differences at the 6 and 8-month assessments. The interaction of counseling and text messages was not significant.
Table 3.
Adherence self-efficacy and strategies at baseline and follow-up assessments for the four intervention conditions.
| Self-efficacy scale | Adherence Counseling (N = 149) | Adherence Counseling + Reminders (N = 150) | Contact Matched Control (N = 151) | Contact Matched + Reminders (N = 150) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| M | SD | M | SD | M | SD | M | SD | |
| Baseline | 7.6 | 2.1 | 7.5 | 1.8 | 7.7 | 1.8 | 7.7 | 1.8 |
| 2-months | 8.7 | 1.4 | 8.6 | 1.2 | 8.3 | 1.5 | 8.3 | 1.4 |
| 4-months | 8.7 | 1.2 | 8.5 | 1.3 | 8.4 | 1.7 | 8.2 | 1.5 |
| 6-months | 8.6 | 1.4 | 8.4 | 1.5 | 8.3 | 1.6 | 8.1 | 1.5 |
| 8-months | 8.6 | 1.3 | 8.3 | 1.7 | 8.3 | 1.6 | 8.2 | 1.4 |
| 10-months | 8.5 | 1.4 | 8.5 | 1.3 | 8.4 | 1.4 | 8.3 | 1.4 |
| Adherence Strategies | ||||||||
| Baseline | 5.7 | 2.9 | 5.9 | 2.8 | 5.7 | 2.9 | 5.9 | 2.8 |
| 2-months | 6.8 | 2.8 | 7.2 | 3.1 | 5.0 | 2.5 | 5.9 | 2.7 |
| 4-months | 6.5 | 3.0 | 6.4 | 3.0 | 5.1 | 2.8 | 5.5 | 2.6 |
| 6-months | 6.2 | 3.0 | 5.9 | 3.1 | 5.0 | 2.8 | 5.4 | 2.8 |
| 8-months | 6.0 | 3.1 | 5.9 | 3.4 | 4.6 | 2.8 | 5.1 | 2.8 |
| 10-months | 5.7 | 3.0 | 5.4 | 3.4 | 4.8 | 3.0 | 4.9 | 2.9 |
Note: Counseling occurred over two months. The 10 month post counseling reflects 12-months from baseline.
For adherence strategies, the main effect for counseling conditions was also significant, Wilks' λ = 0.97, F(4, 471) = 2.89, p <.05; participants receiving adherence counseling reported more use of adherence strategies than the control condition. Subsequent tests showed significant differences at 2, 4, 6, and 8-months post counseling. There were no effects of text message reminders and the counseling by text message interaction was not significant.
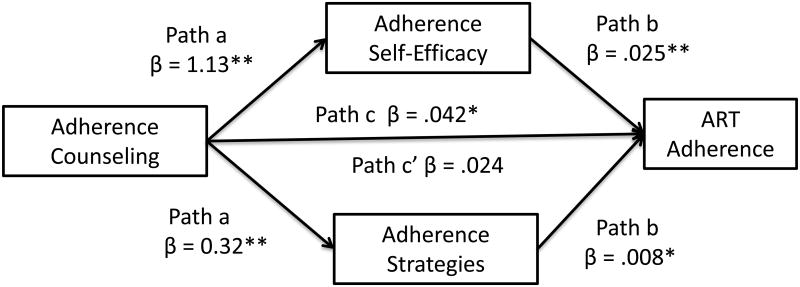
Self-Regulation Adherence Processes Mediation Models
We tested whether self-regulation processes, adherence self-efficacy and strategies, mediated the intervention effects at 2-months and 4-months after counseling. Models for 2 and 4 months after counseling were significant in predicting ART adherence, F(df = 6, 547) = 18.5, p < .01, accounting for 15.9%, and, F(df = 6, 535) = 19.67, p < .01, accounting for 17.1% of the adjusted variance, respectively. Results of the more distal 4-month follow-up model testing self-regulation mediators of counseling on adherence are shown in Figure 2. Results showed that counseling significantly predicted self-efficacy and strategies (a paths), self-efficacy and strategies significantly predicted ART adherence (b paths), and the total effects of counseling on adherence were significant (c path). Accounting for self-efficacy and strategies resulted in a non-significant association between counseling and ART adherence (c' path). Based on 5,000 bootstrap resamples, the test of indirect effects of counseling on adherence through self-efficacy at 4 months post counseling was significant, 95%CI: 0.002 to 0.018, and the indirect effect of counseling on adherence through strategies was significant, 95%CI: 0.001 to 0.021. Combined, the total indirect effect was significant, 95%CI: 0.007 to 0.034. These same effects were observed at the two-month follow-up.
Figure 2.
Mediation model for counseling effects on adherence self-efficacy, adherence strategies, and ART adherence. Note, * p <.05, ** p <.01
Discussion
Adherence support counseling for people living with HIV demonstrated significant improvements in ART adherence. In the first few months after counseling the number of participants who achieved 90% ART adherence was as much as 25% to 30% greater than participants in the control condition. The same pattern of effects was observed in sensitivity tests at the upper bound 95% and lower bound 85% adherence. In addition, self-regulation counseling was associated with viral suppression. Participants receiving adherence counseling were less likely than the contact-matched control group to revert from being viral suppressed to unsuppressed (20% vs. 25%), and more likely to improve from viral unsuppressed to suppressed (13% vs. 9%). These modest but significant differences in viral suppression occurred ten months after counseling, despite the relatively short-term impacts on ART adherence. Further supporting the effects of the counseling intervention, we observed strengthened adherence self-efficacy and increased use of adherence strategies relative to the control condition.
Our study design allowed for a test of the independent and interactive effects of daily medication text message reminders. Results failed to demonstrate any added benefit of daily text message reminders, neither as a stand-alone intervention nor as a means of sustaining adherence following counseling. The one significant finding for daily reminders was an adverse effect on adherence self-efficacy. We speculate that participants may habituate to daily adherence reminders, which may even demotivate adherence by cuing participants to their non-adherence. In contrast, other studies have shown weekly intermittent text message reminders are effective in increasing ART adherence and sustaining HIV suppression (19, 38). For example, in a head-to-head comparison, weekly text messages increased adherence while daily messages did not (39). In addition, our sample represented patients living with HIV for an extended time, and text message interventions may be more effective earlier in treatment (40).
The outcomes of the trial should be considered in light of its limitations. Adherence greater than 95% was not achieved for more than half of participants receiving counseling and more than one-third of participants receiving counseling did not even reach the lower-bound of 85% adherence. And for those who did improve their adherence the gains were not sustained in the long-term. Our study design was limited by only assessing HIV RNA at baseline and 12-months later. Because adherence improvements were not sustained beyond six months from counseling, we may have missed the opportunity to observe shorter-term effects on viral suppression. In addition, our participants had variable experience with text messaging which may have accounted for the lack of effects observed with the text message reminder intervention. With these limitations in mind, we conclude that brief adherence counseling delivered by phone to patients facing significant challenges to ART adherence demonstrates clinically meaningful outcomes, but further refinements are needed to optimize and sustain the effects of adherence support counseling.
One factor that may have limited the impact of counseling on adherence and viral suppression was the limited number of sessions. We set the number of intervention sessions at five based on past ART adherence trials. For example, Reynolds et al. (14) tested 14 sessions of brief phone ART adherence counseling, but with only 70% session attendance. Examining the number of sessions needed to achieve 95% adherence in our trial, we found that 34% of participants had achieved success by the second session, and 48% achieved this criteria by the fifth session. Given the decision to limit counseling to five sessions was not grounded in any empirical findings, it is unknown whether additional sessions would have brought a majority of individuals to achieve 95% adherence. Alternatively, adherence counseling may be more efficiently delivered on an as-needed basis. For example, real-time electronic medication monitoring can be paired with phone counseling to offer in-the-moment adherence problem solving (41). Future research is needed to determine the number of sessions and optimal timing needed to achieve clinically meaningful outcomes for all patients and at what cost.
Acknowledgments
The authors thank Cindy Merely, Brandi Welles, Christina Amaral, Denise White, Christopher Conway-Washington, Ginger Hoyt, Tamar Grebler, and Christopher Kegler for the contributions to the execution of this trial.
This project was supported by National Institute of Nursing Research Grant R01-NR012962, Kalichman, PI. Schinazi was supported by the Center for AIDS Research, Emory University School of Medicine, National Institutes of Health (NIH) grant P30-AI050409 and the Department of Veterans Affairs.
Footnotes
Conflicts: The authors declare no conflicts of interest.
References
- 1.Lima VD, Bangsberg DR, Harrigan PR, Deeks SG, Yip B, Hogg RS, et al. Risk of Viral Failure Declines With Duration of Suppression on Highly Active Antiretroviral Therapy Irrespective of Adherence Level. J Acquir Immune Defic Syndr. doi: 10.1097/QAI.0b013e3181f2ac87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley H, Hall HI, Wolitski RJ, Van Handel MM, Stone AE, LaFlam M, et al. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV--United States, 2011. MMWR Morbidity and mortality weekly report. 2014;63(47):1113–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. Am Psychol. 2013;68(4):197–209. doi: 10.1037/a0032694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathes T, Pieper D, Antoine SL, Eikermann M. Adherence-enhancing interventions for highly active antiretroviral therapy in HIV-infected patients - a systematic review. HIV Med. 2013;14(10):583–95. doi: 10.1111/hiv.12051. [DOI] [PubMed] [Google Scholar]
- 6.Hill S, Kavookjian J. Motivational interviewing as a behavioral intervention to increase HAART adherence in patients who are HIV-positive: a systematic review of the literature. AIDS Care. 2012;24(5):583–92. doi: 10.1080/09540121.2011.630354. [DOI] [PubMed] [Google Scholar]
- 7.Teeter BS, Kavookjian J. Telephone-based motivational interviewing for medication adherence: a systematic review. Translational behavioral medicine. 2014;4(4):372–81. doi: 10.1007/s13142-014-0270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobs M, Sherry PS, Taylor LM, Amato M, Tataronis GR, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc (2003) 2012;52(5):613–21. doi: 10.1331/JAPhA.2012.10183. [DOI] [PubMed] [Google Scholar]
- 9.Janssen V, De Gucht V, van Exel H, Maes S. Beyond resolutions? A randomized controlled trial of a self-regulation lifestyle programme for post-cardiac rehabilitation patients. European journal of preventive cardiology. 2013;20(3):431–41. doi: 10.1177/2047487312441728. [DOI] [PubMed] [Google Scholar]
- 10.Keib CN, Reynolds NR, Ahijevych KL. Poor use of cardiac rehabilitation among older adults: a self-regulatory model for tailored interventions. Heart & lung : the journal of critical care. 2010;39(6):504–11. doi: 10.1016/j.hrtlng.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respiratory research. 2013;14:109. doi: 10.1186/1465-9921-14-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sedkaoui K, Leseux L, Pontier S, Rossin N, Leophonte P, Fraysse JL, et al. Efficiency of a phone coaching program on adherence to continuous positive airway pressure in sleep apnea hypopnea syndrome: a randomized trial. BMC pulmonary medicine. 2015;15:102. doi: 10.1186/s12890-015-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zullig LL, Peterson ED, Bosworth HB. Ingredients of successful interventions to improve medication adherence. JAMA : the journal of the American Medical Association. 2013;310(24):2611–2. doi: 10.1001/jama.2013.282818. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds NR, Testa MA, Su M, Chesney MA, Neidig JL, Frank I, et al. Telephone support to improve antiretroviral medication adherence: a multisite, randomized controlled trial. J Acquir Immune Defic Syndr. 2008;47(1):62–8. doi: 10.1097/QAI.0b013e3181582d54. [DOI] [PubMed] [Google Scholar]
- 15.Kalichman SC, Kalichman MO, Cherry C, Swetzes C, Amaral CM, White D, et al. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. AIDS Patient Care STDs. 2011;25(5):303–10. doi: 10.1089/apc.2010.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amico KR, Harman JJ, Johnson BT. Efficacy of antiretroviral therapy adherence interventions: a research synthesis of trials, 1996 to 2004. J Acquir Immune Defic Syndr. 2006;41(3):285–97. doi: 10.1097/01.qai.0000197870.99196.ea. [DOI] [PubMed] [Google Scholar]
- 17.Sabin LL, Bachman DeSilva M, Gill CJ, Zhong L, Vian T, Xie W, et al. Improving Adherence to Antiretroviral Therapy With Triggered Real-time Text Message Reminders: The China Adherence Through Technology Study. J Acquir Immune Defic Syndr. 2015;69(5):551–9. doi: 10.1097/QAI.0000000000000651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orr JA, King RJ. Mobile phone SMS messages can enhance healthy behaviour: a meta-analysis of randomised controlled trials. Health psychology review. 2015;9(4):397–416. doi: 10.1080/17437199.2015.1022847. [DOI] [PubMed] [Google Scholar]
- 19.Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PLoS ONE. 2014;9(2):e88166. doi: 10.1371/journal.pone.0088166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amico KR. Evidence for Technology Interventions to Promote ART Adherence in Adult Populations: a Review of the Literature 2012-2015. Curr HIV/AIDS Rep. 2015 doi: 10.1007/s11904-015-0286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mbuagbaw L, van der Kop ML, Lester RT, Thirumurthy H, Pop-Eleches C, Ye C, et al. Mobile phone text messages for improving adherence to antiretroviral therapy (ART): an individual patient data meta-analysis of randomised trials. BMJ open. 2013;3(12):e003950. doi: 10.1136/bmjopen-2013-003950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pellowski JA, Kalichman SC, Finitsis DJ. Reliability and validity of a single-item rating scale to monitor medication adherence for people living with HIV and lower health literacy. HIV Clin Trials. 2015;16(1):1–9. doi: 10.1179/1528433614Z.0000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Bruin M, Viechtbauer W, Hospers HJ, Schaalma HP, Kok G. Standard care quality determines treatment outcomes in control groups of HAART-adherence intervention studies: implications for the interpretation and comparison of intervention effects. Health Psychol. 2009;28(6):668–74. doi: 10.1037/a0015989. [DOI] [PubMed] [Google Scholar]
- 24.Kenya: Female Condom Shortage. Humanitarian News and Analysis. 2009 [Google Scholar]
- 25.Reynolds NR. The problem of antiretroviral adherence: a self-regulatory model for intervention. AIDS Care. 2003;15(1):117–24. doi: 10.1080/0954012021000039815. [DOI] [PubMed] [Google Scholar]
- 26.Conn VS, Ruppar TM, Chase JA, Enriquez M, Cooper PS. Interventions to Improve Medication Adherence in Hypertensive Patients: Systematic Review and Meta-analysis. Current hypertension reports. 2015;17(12):94. doi: 10.1007/s11906-015-0606-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gribble JN, Miller HG, Cooley PC, Catania JA, Pollack L, Turner CF. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35(6-8):869–90. doi: 10.3109/10826080009148425. [DOI] [PubMed] [Google Scholar]
- 28.Bangsberg D, Hecht FM, Charlebois ED, Chesney M, Moss A. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS and Behavior. 2001;5:275–81. [Google Scholar]
- 29.Kalichman S, Amaral CM, Cherry C, Flanagan JA, Pope H, Eaton L, et al. Monitoring Antiretroviral adherence by unannounced pill counts conducted by telephone: Reliability and criterion-related validity. HIV Clinical Trials. 2008;9:298–308. doi: 10.1310/hct0905-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- 31.Kalichman SC, Cain D, Fuhrel A, Eaton L, Di Fonzo K, Ertl T. Assessing medication adherence self-efficacy among low-literacy patients: Development of a pictographic visual analogue scale. Health Education Research. 2005;20(1):24–35. doi: 10.1093/her/cyg106. [DOI] [PubMed] [Google Scholar]
- 32.Catz SL, Kelly JA, Bogart LM, Benotsch EG, McAuliffe TL. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19(2):124–33. [PubMed] [Google Scholar]
- 33.Kalichman SC, Cain D, Cherry C, Kalichman M, Pope H. Pillboxes and antiretroviral adherence: Prevalence of use, perceived benefits, and implications for electronic medication monitoring devices. AIDS Patient Care STDs. 2005;19:49–55. doi: 10.1089/apc.2005.19.833. [DOI] [PubMed] [Google Scholar]
- 34.Jurs S, Glass G. The effect of experimental mortality on the internal and external validity of the randomized comparative experiment. Journal of Experimental Education. 1971;40:62–6. [Google Scholar]
- 35.Nunes EV, Pavlicova M, Hu MC, Campbell AN, Miele G, Hien D, et al. Baseline matters: the importance of covariation for baseline severity in the analysis of clinical trials. Am J Drug Alcohol Abuse. 2011;37(5):446–52. doi: 10.3109/00952990.2011.596980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 37.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods. 2008;40(3):879–91. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 38.da Costa TM, Barbosa BJ, Gomes e Costa DA, Sigulem D, de Fatima Marin H, Filho AC, et al. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. International journal of medical informatics. 2012;81(4):257–69. doi: 10.1016/j.ijmedinf.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pop-Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, de Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25(6):825–34. doi: 10.1097/QAD.0b013e32834380c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ware NC, Pisarski EE, Tam M, Wyatt MA, Atukunda E, Musiimenta A, et al. The meanings in the messages: How SMS reminders and real-time adherence monitoring improve ART adherence in rural uganda. AIDS. 2016 doi: 10.1097/QAD.0000000000001035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haberer JE, Kahane J, Kigozi I, Emenyonu N, Hunt P, Martin J, et al. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav. 2010;14(6):1340–6. doi: 10.1007/s10461-010-9799-4. [DOI] [PMC free article] [PubMed] [Google Scholar]