Abstract
The majority of patients with late stage castration-resistant prostate cancer (CRPC) develop bone metastases that often result in significant bone pain. Therapeutic palliation strategies can delay or prevent skeletal complications and may prolong survival. An alpha-particle based therapy, radium-223 dichloride (223RaCl2), has been developed that delivers highly localized effects in target areas and likely reduces toxicity to adjacent healthy tissue, particularly bone marrow. Radiation safety aspects were evaluated for a single comprehensive cancer center clinical phase 1, open-label, single ascending-dose study for three cohorts at 50, 100, or 200 kBq kg−1 body weight. Ten patients received administrations, and six patients completed the study with 1 y follow-up. Dose rates from patients administered 223Ra dichloride were typically less than 2 μSv h−1 MBq−1 on contact and averaged 0.02 μSv h−1 MBq−1 at 1 m immediately following administration. Removal was primarily by fecal excretion, and whole body effective half-lives were highly dependent upon fecal compartment transfer, ranging from 2.5–11.4 d. Radium-223 is safe and straightforward to administer using conventional nuclear medicine equipment. For this clinical study, few radiation protection limitations were recommended post-therapy based on facility evaluations. Specific precautions are dependent on local regulatory authority guidance. Subsequent studies have demonstrated significantly improved overall survival and very low toxicity, suggesting that 223Ra may provide a new standard of care for patients with CRPC and bone metastases.
Keywords: alpha particles, nuclear medicine, radiation, alpha, radium
INTRODUCTION
An estimated 248,740 men in the United States will be diagnosed each year with prostate cancer, and there will be an estimated 28,170 deaths within that group from this disease (Goyal and Antonarakis 2012). Patients in whom the disease progresses may eventually develop a hormone refractory or castration-resistant prostate cancer (CRPC) state (Scher and Sawyers 2005). Bone metastases are the primary cause of death and disability in patients with CRPC (Keller et al. 2001), causing pain, pathologic fractures, cord compression, and marrow insufficiency, among other side effects of cancer (Weinfurt et al. 2005). Androgen deprivation has also been shown to increase the risk of osteoporotic fractures (Autio et al. 2012). Treatment strategies have included chemotherapy, immunotherapy, and radiopharmaceutical agents. External beam radiation therapy has been used effectively for patients with unifocal disease. Pharmacologic agents that target the osteoclast/ osteoblast pathway either without or with the addition of radiopharmaceutical agents (e.g., 89Sr, 153Sm) have been shown to be effective in delaying skeletal-related events (Bauman et al. 2005). Several systematic reviews have addressed the various strategies for the palliation of metastatic bone pain and its control (Bauman et al. 2005; Scher and Sawyers 2005; Saylor et al. 2011; Autio et al. 2012; Goyal and Antonarakis 2012).
Beta-emitting bone-seeking agents used for these treatments have included 153Sm chelated to ethylenediamine-tetramethylene-phosphonate acid (EDTMP), 89Sr-dichloride, 32P-sodium phosphate, 117mSn, and 186Re-chelate. The use of 32P is the oldest technique, which started in the 1940s; however, the use of this isotope demonstrated significant marrow toxicity. Newer techniques developed in the 1980s used 153Sm and 186Re chelated EDTMP. However, the use of these agents may be compromised by renal dysfunction and marrow suppression (Akerley et al. 2002; Tu et al. 2005; Amato et al. 2008; Suttmann et al. 2008; Fizazi et al. 2009; Morris et al. 2009). In studies comparing the efficacy of these agents, there appeared to be no differences among them with respect to pain palliation and no demonstration of increased survival.
An alpha-emitting pharmaceutical, 223RaCl2, was developed by Algeta ASA (Kjelsåsveien 172, 0884 Oslo, Norway) and is manufactured at the Institute for Energy Technology, Kjeller, Norway. Radium-223 is a byproduct material, produced by neutron irradiation of 226Ra to create 227Ac, which decays to 223Ra through 227Th. Radium-223 dichloride is intended for therapeutic use for patients with bone metastases (Bruland et al. 2006). Radium acts as a calcium mimetic and naturally targets areas of bone undergoing changes, such as those induced by tumors like new bone growth in and around bone metastases. The bone-targeting properties of 223Ra are similar to those of 89Sr. However, the radiation therapeutic characteristics of an alpha-emitting radionuclide are inherently more advantageous than the beta emitting radionuclides of other studied agents. Radium-223, with a physical half-life of 11.4 d, emits a high linear transfer (LET) alpha radiation with a range in tissue of less than 100 μm. The relative biological effectiveness (RBE) for alpha radiation for mammalian cell killing ranges from about 1 to 7 (Sgouros et al. 2010), and because of the high LET, alpha radiation induces predomi-nantlynon-repairableDNA double-strandbreaks resultingin a highly localized cytotoxic effect in the target areas (Ritter et al. 1977). Cell killing by alpha irradiation does not depend on oxygen concentration within the tissue; i.e. hypoxic cells are just as sensitive as oxygenated cells (Hall and Giaccia 2012). In addition, the short path length of the alpha radiation should reduce toxicity to adjacent healthy tissue, particularly bone marrow.
Radium-223 decays in six steps via a chain of alpha and beta emissions into a stable isotope of lead, 207Pb. The total amount of emitted energy per the 223Ra decay series is 28.2 MeV, of which 95.3% comes from alpha radiation, 3.6% from beta radiation, and 1.1% from gamma radiation and x-rays (Tables 1 and 2) (Eckerman and Endo 2008). Photon emissions that accompany the decay of 223Ra and its daughter products make possible the use of conventional instrumentation to measure and detect 223Ra (such as dose calibrators, survey meters, and well counters). The principal x-and gamma-radiation emissions occurring during the decay of 223Ra and its progeny are (Eckerman and Endo 2008): 223Ra at 81–84 keV (41% abundance) and 269 keV (13.6% abundance); 219Rn at 271 keV (9.9% abundance) and 402 keV (6.5% abundance); 211Pb at 405 and 427 keV (3.8% and 1.4% abundance, respectively); and 211Bi at 351 keV (13% abundance).
Table 1.
Decay series of 223Ra with primary decay types and energies per nuclear transformation (nt) listed.
| Nuclide | Half-life | Decay mode | Emitted energy (MeV nt−1)
|
|||
|---|---|---|---|---|---|---|
| Alpha | Electron | Photon | Total | |||
| 223Ra | 11.4 d | Alpha | 5.7702 | 0.0781 | 0.1413 | 5.9895 |
| 219Rn | 3.96 s | Alpha | 6.8801 | 0.0068 | 0.0586 | 6.9456 |
| 215Po | 1.781E-3 s | Alpha | 7.5261 | <E-04 | 0.0002 | 7.5263 |
| 211Pb | 36.1 m | Beta | — | 0.4543 | 0.0644 | 0.5187 |
| 211Bi | 2.14 m | Alpha/Beta | 6.6757 | 0.0100 | 0.0473 | 6.7330 |
| 207Tl (0.997) | 4.77 m | Beta | — | 0.4952 | 0.0024 | 0.4975 |
| 211Po (0.003) | 0.516 s | Alpha | 7.5860 | 0.0002 | 0.0082 | 7.5944 |
| 207Pb | Stable | |||||
Table 2.
Equilibrium dose constants for alpha decay emissions associated with 223Ra decay.
| Radionuclide | Branching ratio | Alpha energy per 223Ra decay series (J) |
|---|---|---|
| 223Ra | 1.0 | 9.2425 E-13 |
| 219Rn | 1.0 | 1.0808 E-12 |
| 215Po | 1.0 | 1.1824 E-12 |
| 211Bi | 0.9972 | 1.0478 E-12 |
| 211Po | 0.0028 | 3.3 E-15 |
| Total | 4.239 E-12 |
A significant 223Ra anti-tumor effect has been demonstrated in an experimental skeletal metastases model in nude rats intraventricularly inoculated with human breast cancer cells. All of the tumor-bearing control animals had to be sacrificed because of induced paralysis 20–30 d after tumor cell injection, whereas rats treated with 110 kBq kg−1 body weight showed a significantly increased symptom-free survival (p < 0.05). Approximately 40% of the rats treated with 110 kBq kg−1 body weight Alpharadin were alive beyond the 67-d follow-up period compared to none in the control animals (Henriksen et al. 2002). Based on the encouraging results from pre-clinical testing, 223Ra dichloride entered clinical development in August 2001. As of August 2013, 223Ra dichloride had been administered to more than 900 patients with bone metastases from CRPC in Phase I–III clinical trials worldwide (Nilsson et al. 2005, 2011, 2012; Parker et al. 2011; Sartor et al. 2012). In a Phase I trial, no dose-limiting toxicity was observed (Nilsson et al. 2005). In Phase II/III trials, 223Ra showed a statistically significant improvement in overall survival as compared to placebo (Nilsson et al. 2007, 2011, 2012; Parker et al. 2011; Sartor et al. 2012), a consistent improvement in disease-related biomarkers (Nilsson et al. 2011, 2012; Parker et al. 2011) and pain (Nilsson et al. 2012), and a highly tolerable medical safety profile (Nilsson et al. 2007, 2011, 2012; Parker et al. 2011; Sartor et al. 2012).
Over the past several years, Memorial Sloan-Kettering Cancer Center (MSKCC) investigators have focused on targeted therapies for prostate cancer using unique clinical trial designs (Kelly et al. 1993; Graham et al. 1999; Scher et al. 1999; Tu et al. 2005; Morris et al. 2009). This Phase 1 study evaluated single ascending-doses of 223Ra and its ability to target the bone stroma, using gamma camera imaging and other bioassay data to evaluate biodistribution of the agent at multiple time points post administration and assess clinical outcome (Carrasquillo et al. 2013). The purpose of this paper is to report on and evaluate the radiation safety aspects associated with the use of 223Ra as a targeted radiotherapy for prostate cancer patients in a Phase 1 study.
MATERIALS AND METHODS
Radiation safety aspects were evaluated as associated with a single oncology center (Memorial Sloan-Kettering Cancer Center, MSKCC) clinical Phase 1, open-label, single ascending-dose study to assess safety, pharmacokinetics, bio-distribution and radiation dosimetry of intravenous doses of 223Ra dichloride in patients with CRPC, and skeletal metastases. No control groups were used in the study.
Radionuclide, dose, and mode of administration
Radium-223 dichloride solution for injection is a clear, colorless, ready-to-use aqueous solution, sterile and free of endotoxins, for intravenous administration. In the present study, eligible patients were enrolled into one of three cohorts with successive cohorts receiving increasing doses of 223Ra dichloride. The doses studied were 50, 100, or 200 kBq kg−1 body weight. A conventional 3+3 design for dose-escalation of oncology products was used. A minimum of nine and a maximum of 18 patients were to be included. A minimum of three evaluable patients were entered into each dose level cohort, and each dose level was separated by at least 4 wk to allow review of safety data before dose escalation in the next cohort of patients. Each patient received a single dose of 223Ra dichloride at the assigned dose level during the study. The required volume of 223Ra dichloride was calculated using the patient’s body weight, the dose level, and a correction factor for physical decay of 223Ra. An optional second injection of 223Ra dichloride, fixed at 50 kBq kg−1, was permitted after the initial 6-wk safety assessment if the referring physician judged that the patient showed a treatment benefit and there were no clinical safety concerns.
The selection of doseswas based on non-clinical studies of radiation dose to bone marrow and previous clinical experience. Using highly conservative assumptions of 70% uptake in the skeleton (based on the highest value observed in rodent and dog studies), distributed 50% on bone surface and 50% in bone volume, and a 6-d biological clearance of the parent 223Ra and its progeny (in agreement with the measured skeletal clearance in humans as well as radionuclide decay and dosimetry data) (Nilsson et al. 2005), the radiation dose to bone marrow, presumed to be the organ receiving the highest dose following the starting dose of 50 kBq kg−1, was estimated to be 116 cGy, well below the accepted 200 cGy dose-limiting toxicity (DLT) for this organ.
For this clinical study, 223Ra dichloride was handled only by individuals qualified by training and experience in the safe handling of radionuclides. The drug was secured when not in use and administered only to patients under direct supervision of an authorized user as approved by the Center’s committee on radiation. Authorized nuclear pharmacists verified the administration volume and the total radioactivity injected. The vial code and volume per injection were recorded in each patient’s chart.
Radiation regulatory environment
This study was performed under a broad scope human-use radioactive material license that allows for the use of any radioactive material with atomic number greater than 83 as a radiopharmaceutical or radiobiologic for therapy with an “Investigational New Drug” (IND) designation accepted by the FDA. The study material was used under an active FDA IND safety review, which found that for 223Ra dichloride, the proposed clinical investigation for radiotherapy treatment of skeletal metastases of castration-resistant prostate cancer could proceed. The study was performed under a protocol reviewed and approved by the institution’s committee on radiation (COR) and institutional review board (IRB).
Eligibility criteria
Patients entered in the trial were at least 18 y of age and met the following criteria: histological or cytological evidence of adenocarcinoma of the prostate, demonstrated progressive castrate resistant metastatic bone disease as shown by imaging or biochemical progression, had at least two bone metastases confirmed by bone scintigraphy within the 4 wk pre-administration, showed castrate levels of testosterone, had a life expectancy of greater than or equal to 6 mo, met specific laboratory requirements, and were able and willing to sign an informed consent and to comply with the protocol requirements. Patientswere excluded if they had predominantly visceral metastases, other active malignant disease or other serious illness, or if they had received an investigational drug within 4 wk of the 223Ra dichloride administration; any chemotherapy, immunotherapy, or external radiotherapy in the previous 4 wk; or prior hemibody radiotherapy or systemic radionuclide therapy within 24 wk prior to administration of the study drug. Bisphosphonates were allowed if the dose had not changed in the previous 4 wk.
Immediately before 223Ra dichloride was administered, it was confirmed that the patient remained eligible for dosing, with particular regard to hematologic parameters. Clinical safety was evaluated after each administration based on assessment of adverse events, clinical laboratory safety tests, vital signs, electrocardiograms, and physical examination. Potential long-term toxicity, bone marrow biopsy, and survival were assessed during the 1-y follow-up period.
Pharmaceutical preparation
When a patient had participated in an informed consent discussion, signed the informed consent form, and was deemed eligible for the study, the AU (Nuclear Medicine physician) entered an electronic order and written directive for the specific dose level to be administered. At that time, an order request was sent to the supplier. The supplier shipped the 223Ra solution in a sealed glass vial, held in leaded containers of approximately 4 mm thickness, over-packed in a sealed tin, and again packed in a carton totaling a “Type A” package as defined by the U.S. Department of Transportation (DOT) and the International Air Transport Association (IATA). Documentation included with the shipment provided the following information: Activity, e.g., 6 MBq 223Ra dichloride injection, 1,000 kBq mL−1; form - 223Ra dichloride; half-life -11.4 d; volume - 6.0 mL; calibration date, expiration date, study number, center number, investigator, batch number, patient identification, radiation symbol, a “Caution Radioactive Material” label, along with storage conditions.
For this clinical study, the radiopharmaceutical product was initially shipped internationally by plane to a freight custom broker to assist in clearance of the overseas order with U.S. customs. Ground transportation was provided by a broker according to DOT shipment regulations for radiopharmaceuticals. The vials were stored inside their lead container in a secure facility and used within the 28 d of shelf-life.
Radium-223 dichloride was manufactured in accordance with current good manufacturing practice. The product was supplied in 20-mL single-dose glass vials with a radioactivity concentration of 1,000 kBq mL−1 as of the reference date. The volume per vial was 6 mL, corresponding to 6 MBq as of the reference date. The product had a pre-calibration period of 14 d. Each vial was labeled with a unique vial number, identifying the specific vial as well as the batch number.
The estimated dose rate to the skin or shallow dose at contact from an unshielded plastic syringe was assessed with an ionization chamber (Fluke model 451B-RYR, Ohio). The estimate of shallow dose was made by taking the difference between the open slide window contact radiation reading from the syringe and the closed slide window radiation reading from the syringe. The mean shallow dose rate on contact with the syringe was 4.8 μGy min−1 MBq−1 (SD 1.4). Shallow dose rates on contact with the shipped glass vial demonstrated lower levels at 0.6 μGy min−1 MBq−1 (SD 0.2), likely due to geometry and additional beta shielding from the glass container.
The activity in each vial was verified using a dial setting dose calibrator (Capintec Model Ultra, Ramsey, New Jersey) with a setting calibrated according to a National Institute of Standards and Technology (NIST)-traceable standard of 223Ra provided by the study sponsor. A 20-mL sealed glass vial containing 6 mL of 223Ra dichloride standard solution (containing approximately 6 MBq 223Ra at reference date) was dedicated as a calibration source for determining an appropriate dial setting for the dose calibrators used for activity verification measurements of patient doses. Dose calibrators were adjusted for the specific isotope, 223Ra, based on the decay corrected activity of the reference standard. Three repeat measurements at this setting were verified to be within ± 5% of the decay corrected activity of 223Ra in the standard reference solution.
Radiation safety considerations
The activity administered is considerably lower than the levels administered in standard diagnostic nuclear medicine studies and consequently should be expected to result in a negligible external radiation exposure hazard to family and surrounding persons. Assuming a conservative theoretical exposure rate constant for an unshielded point source of 223Ra in equilibrium with progeny of approximately 0.05 μSv h−1 MBq−1 (Smith and Stabin 2012) and the U.S. Nuclear Regulatory Commission (NRC) methodology for evaluating the external exposure to others (USNRC 2008), the dose was estimated to be 17, 34, or 69 μSv for the study dose activity levels of 50, 100, or 200 kBq kg−1, respectively, in a 70 kg typical patient. Therefore, all patients recruited into this study, at all dose levels, were treated as outpatients in accordance with International Commission on Radiological Protection (ICRP), National Council on Radiation Protection and Measurements (NCRP), and NRC guidance in that the estimated dose to a member of the public is expected to be well below 1 mSv and the estimated dose to a patient caregiver is well below 5 mSv (ICRP 2008; USNRC 2008). Both treatment and routine follow-up visits were performed on an outpatient basis.
As 223Ra dichloride emits alpha, beta, and gamma radiation, a wide range of instrumentation can be used to perform general area surveys. Indeed, conventional probes, such as a GM pancake probe, that detect betas and photons are useful for such surveys. Wipe test contamination surveys are a necessary means of demonstrating compliance with DOT and IATA package contamination limits and license commitments such as weekly contamination surveys where unsealed forms of radioactive materials are prepared or in use.
U.S. regulatory guidance includes model procedures that suggest surface contamination trigger levels for removable alpha contamination in restricted areas of 3.3 Bq 100 cm−2 (USNRC 2008). In addition, regulations on the transport of dangerous goods require that the external surfaces of regulated packages containing radioactive material be less than 0.4 Bq cm−2 of removable alpha contamination (i.e., 49CRF173.443, Table 9, “all other alpha emitting radionuclides”), and U.S. regulations require that labeled packages (i.e., White I, Yellow II, and Yellow III) be monitored for contamination upon receipt to demonstrate compliance with the limits for alpha contamination referenced from the transportation regulations. The transportation package contamination limits are further complicated by a wipe removal efficiency of 0.1 (Frame and Abelquist 1999), rendering the contamination wipe action level for packages containing 223Ra to be 0.04 Bq cm−2. This action level may be averaged over an area wiped of 300 cm2, resulting in a contamination threshold of approximately 12 Bq 300 cm−2 of alpha radiation per wipe.
To evaluate wipe test efficiencies and minimum detectable activities, aliquots of 223Ra solution from a NIST traceable standard were diluted, pipetted onto standard wipe test filter disks, and evaluated with various radiation contamination instrumentation: thin windowed Geiger Mueller (GM) probe (Model 44-9, Ludlum, Sweetwater, TX), sodium iodide low energy gamma (NaI-LEG) probe (Model 44-3, Ludlum, Sweetwater, TX), zinc sulfide (ZnS) probe (Model 43-2, Ludlum, Sweetwater, TX), liquid scintillation counter (Model TriCarb 2900TR, Perkin Elmer, Shelton, CT), and gamma counter (Model Wizard2, Perkin Elmer, Shelton, CT). The filter disks were allowed to air dry and placed in a reproducible wipe test evaluation geometry at a distance of 0.32 cm (0.125 inches) with contamination probes coupled to an integrating scaler. After counting with portable instrumentation, the disks were analyzed in a gamma and liquid scintillation counter. Based on the background count rate, an integrated count time of 1 min, and the activity of the sample, the minimal detectable activity (MDA) for each array was estimated including systematic error bounds (Dauer and Mayer 1993). Total activity in the samples includes 223Ra and its progeny in equilibrium. Table 3 summarizes measured contamination detection efficiencies and MDAs of various 1-min integrated survey modalities for 223Ra removable surface contamination wipe tests.
Table 3.
Measured removable contamination detection efficiencies and minimum detectable activities (MDA) of various 1 min integrated survey modalities for 223Ra wipe tests.
| Instrument | Background (cpm) | Efficiency (cpm/dpm) | Minimum detectable activity
|
|
|---|---|---|---|---|
| (dpm) | (Bq) | |||
| Alpha Probe (Zinc Sulfide)a | 0 | 0.08 | 71 | 1.2 |
| Thin Window Beta/Gamma Probe (GM)a | 28 | 0.13 | 350 | 5.8 |
| Low Energy Gamma Probe (Sodium Iodide)a | 94 | 0.29 | 1296 | 21.6 |
| Liquid Scintillation Counter | 49 | 0.97 | 64 | 1.1 |
| Gamma Counter | 210 | 0.40 | 333 | 5.6 |
For wipe test evaluations in a fixed geometry at a distance of 0.32 cm.
Regulatory guidance estimates the efficiency of an alpha sensitive ZnS probe for 230Th (an alpha emitter) at 0.259 (USNRC 1998) as determined with the detector in contact with an electroplated disc source. An increase in the source-to-detector distance, distributing the activity over a larger area, and self-absorption are expected to decrease the efficiency of the array significantly. For evaluating removable contamination wipe tests, the authors’ estimated MDAwith a ZnS probe and 223Ra was 1.2 Bq (71 dpm), and the overall efficiency was 0.08, consistent with expectations.
Based on the resulting MDAs, ease of operation, space, and maintenance, a ZnS contamination probe coupled to a scaler and set up in alpha mode could be considered for evaluating wipes to simply demonstrate regulatory package and restricted area contamination survey compliance. Alternatively, a thin-windowed GM coupled to a scaler, a well counter used for wipes, or other beta mode detectors may also similarly meet the alpha contamination goals using alpha to beta/gamma ratios and additional assumptions. While liquid scintillation offers an efficiency of greater than 90% for wipe assays (Scarpitta and Fisenne 1996; Floeckher 2012), smaller clinics typically do not possess a larger scintillation counter as compared to a more compact handheld detector/scaler array. In order to demonstrate a lower alpha MDA for unrestricted area contamination surveys, the background count rate, count time, or other factors affecting efficiency should be modified as appropriate. Note that for general area scanning surveys conducted at typical 1–2 cm distances to the surface, as opposed to wipe test evaluations at close range, more conventional probes, such as a GM pancake probe, that detect betas and photons are appropriate instruments.
For this clinical study, in the event of spillage of the study drug, members of the radiation safety staff were available to make the necessary measurements and carry out any required decontamination procedures. While radium will not typically be absorbed strongly onto work surfaces or floors, a complexing agent such as 0.01 M ethylene-diaminetetraacetic (EDTA) solution was available.
The administration of 223Ra dichloride is similar to that for any other ready-to-use radiopharmaceutical, except that external radiation dose rates are considerably lower. As part of the institution’s procedures with all radiopharmaceuticals, doses were drawn into the syringe in a biosafety cabinet. Personnel donned appropriate personnel protective clothing prior to preparation, syringe filling, and administration. Although the administered patient activity is calculated by volume using the certified activity stated on the vial, the radioactivity in the vial was verified in a dose calibrator before dispensing. The calculated volume of 223Ra dichloride was drawn into a syringe by the radiopharmacist, and the activity in the vial was verified again after dispensing.
The radiopharmaceutical was administered to patients in a controlled area for radionuclide administration under the supervision of an authorized user (AU, nuclear medicine physician). As part of this study protocol, the patients remained in a setting under clinical supervision for up to 4–8 h post injection to secure timely scanning, blood sampling, radiation safety surveys, and evaluation of any early adverse events.
The area beneath the administration site was protected with a bench liner sheet (e.g., plastic-backed absorbent material). The AU inserted the intravenous cannula for injection and intravenous access was verified by flushing with saline prior to injection of the study drug in order to minimize the risk of extravasation. The syringe containing the study drug was fitted directly to a two/three-way adapter. The 223Ra dichloride was administered as a slow intravenous injection. After the administration of the study drug, the cannula was flushed with saline to ensure that to the extent possible, all of the drug had been administered. For the purpose of drug accountability in the clinical trial setting, residual measurements were made via dose calibrator on the study syringe and equipment used to administer the drug. After administration, the equipment used to prepare and administer the drug was treated as short-lived radioactive waste and stored/disposed of in accordance with hospital radioactive waste procedures.
The potential for radiation dose to the extremities of the personnel preparing the syringe and performing the administration of 223Ra was assessed. Based on the measured mean shallow dose rates of 4.8 μGy min−1 MBq−1 and 0.6 μGy min−1 MBq−1 from the syringe and vial respectively, avial activity of 6 MBq, and typical syringe activity of about 3.5 MBq (for a 70 kg patient treated at 50 KBq kg−1), and further assuming that preparation of the dose takes 2 min of vial handling and 1 min of syringe handling while administering the activity takes an additional 1 min of syringe handling, it was estimated that a worker might receive approximately 41 μSv for each administration. Therefore, a worker could perform over 1,200 administrations of 223Ra dichloride before reaching the threshold for monitoring of the extremities, which is 50 mSv (i.e., one tenth of the annual extremity dose limit of 500 mSv).
Radiation safety surveys and instructions
As part of the institution’s radiation safety procedures, dose rates from patients undergoing radionuclide therapy are measured to assess the potential radiation exposure to the patient’s family and to members of the general public coming within the proximity of the patient. The photon (gamma) dose rates emanating from these patients were measured for each administration at time 0, 24, 48, and 144 h after injection at distances of direct contact of 0.3 m and 1.0 m using an appropriately calibrated ion chamber (Model 451B-RYR, Fluke Biomedical, Cleveland, OH). Net measured values were obtained by subtracting the background dose rate (i.e., background dose rate measured in the nuclear medicine injection area due to the presence of other patients administered radioactive material and proximity to a radiopharmacy dispensing room) from the gross measured values (i.e., the raw measurements before any background correction) from patients.
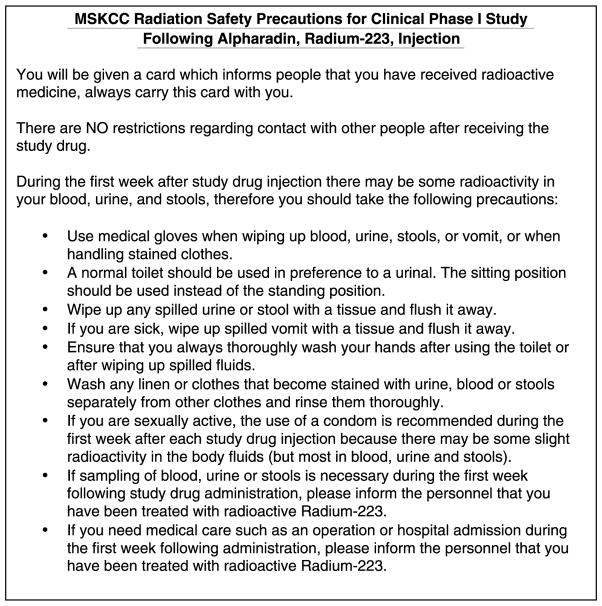
U.S. and international regulatory guidance suggests thresholds for patient instruction and release based on the estimated dose to a member of a public (ICRP 2008; USNRC 2008). As demonstrated previously, the estimated doses to others were all well below 1 mSv; therefore, no instructions were specifically required to be provided. However, in the course of this clinical study, communication for control of personnel excreta was recommended and implemented to reduce the risk of contamination and unintentional internal exposure to members of the public. Radiation safety staff provided patients with verbal and written instructions describing simple steps to be followed at home in connection with blood, urine, or stools for a period of one week after dosing. An example is given in Fig. 1. Such instructions are, of course, highly dependent on local regulatory guidance.
Fig. 1.
An example of radiation safety instructions for patients receiving 223Ra dichloride for this clinical Phase 1 study protocol. (Note that specific recommendations may differ based on local regulatory guidance that may differ from one facility or region to another.)
Biodistribution, pharmacokinetics, radiation dosimetry, and gamma scintigraphy imaging
Biodistribution measurements, pharmacokinetics, organ dosimetry, and gamma scintigraphy imaging were performed to evaluate whole-body retention and individual organ uptake/retention in blood, and the results are reported elsewhere (Carrasquillo et al. 2013).
RESULTS
Patient Information
In total, 10 patients were enrolled, three in each of the 50 and 100 kBq kg−1 dose groups and four in the 200 kBq kg−1 dose group. Six patients (two in each dose group) completed the study, including a 12-mo follow-up period. Four subjects chose to discontinue: one in each dose group died from disease progression, and one subject in the 200 kBq kg−1 dose group withdrew consent 5 wk after the first injection. Patients had the following mean (range) demographics: age of 69 y (58–81 y), height of 176 cm (161–188 cm), weight of 83 kg (67.5–123 kg), and BMI of 26.8 kg m−2 (23.52). All patients had evidence of bone metastases on a 99mTc-MDP bone scan and on a 18F-FDG PET/CT scan. Table 4 summarizes the administered activities by dose level. In accordance with the study protocol, if a second injection was given, it was a fixed dose of 50 kBq kg−1, regardless of the initial dose. One patient in the 200 kBq kg−1 dose group had a minor leak (about 3% of the activity) around the connector during administration. Other doses were given as planned. The maximum injected activity for any patient was 23 MBq for a patient in the 200 kBq kg−1 dose group.
Table 4.
Individual activity of 223Ra per treatment administration of patients in the three cohorts.
| Patient | Initial treatment kBq kg−1 body weight | Total activity first treatment kBq | Total activity second treatment (50kBq kg−1) kBq |
|---|---|---|---|
| 1 | 50 | 4,588 | 4,514 |
| 2 | 50 | 4,366 | 4,292 |
| 3 | 50 | 3,774 | nta |
| 4 | 100 | 7,585 | nt |
| 6 | 100 | 8,251 | 4,144 |
| 7 | 100 | 8,288 | 4,366 |
| 8 | 200 | 13,320 | nt |
| 9 | 200 | 14,763 | 3,737 |
| 10 | 200 | 16,835 | nt |
| 11 | 200 | 24,272 | 6,216 |
nt = not treated.
Radiation surveys
Closed and open window dose rate readings at contact from the 223Ra loaded syringe were also measured immediately before administration. The mean dose rate measured was 19 μGy h−1 MBq−1 with a closed window configuration, and the dose rates were 308 μGy h−1 MBq−1 (16-fold higher) in the open window configuration. The difference in the open and closed window configuration averaged 289 μGy h−1 MBq−1. It is noted that a glass vial reduces the difference in open and closed window configuration to a mean dose rate of 38 μGy h−1 MBq−1.
Tables 5 and 6 summarize the dose rate measurements (μSv h−1) and normalized dose rates per injected activity (μSv h−1 injected MBq−1) at 0, 24, 48, and 144 h and distances of 0, 0.3, 1.0 m from patients administered 223Ra dichloride. Normalized dose rates from patients administered 223Ra dichloride were typically <2 μSv h−1 injected MBq−1 on contact. In some cases, the contact and 0.3 m dose rates rose slightly from time of injection through 48 h, presumably as the agent left the systemic blood compartment and concentrated in gut and bone compartments (Carrasquillo et al. 2013), as can be clearly seen on gamma camera images (Fig. 2). The maximum measured dose rate on contact from any patient was 13 μSv h−1 with one patient at 48 h after administration of the study drug. The mean measured normalized dose rate per injected activity at 1 m was 0.02 μSv h−1 injected MBq−1 immediately following administration.
Table 5.
Mean normalized neta (gross) dose rates per injected activity (μSv h−1 injected MBq−1) at 0, 24, 48, and 144 h and distances of 0, 0.3, 1.0 m from study patients administered 223Ra dichloride by administered activity group.
| Time post administration (h) | 50 kBq kg−1 Group
|
100 kBq kg−1 Group
|
200 kBq kg−1 Group
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| 0.0 m | 0.3 m | 1.0 m | 0.0 m | 0.3 m | 1.0 m | 0.0 m | 0.3 m | 1.0 m | |
| 0 | 0.58 (0.77) | 0.12 (0.32) | 0.03 (0.18) | 0.43 (0.45) | 0.10 (0.13) | 0.01 (0.03) | 0.43 (0.44) | 0.10 (0.11) | 0.02 (0.03) |
| 24 | 0.91 (0.95) | 0.12 (0.16) | 0.03 (0.06) | 0.50 (0.60) | 0.25 (0.35) | 0.03 (0.13) | — | — | — |
| 48 | 0.19 (0.24) | 0.01 (0.06) | 0.01 (0.02) | 1.68 (1.71) | 0.30 (0.33) | 0.04 (0.07) | — | — | — |
| 144 | 0.05 (0.11) | 0.01 (0.05) | 0.01 (0.03) | 0.04 (0.07) | 0.01 (0.01) | 0.01 (0.01) | — | — | — |
Net measured values were obtained by subtracting the background dose rate (i.e., background dose rate measured in the nuclear medicine injection area due to the presence of other patients administered radioactive material and proximity to a radiopharmacy dispensing room) from the gross measured values (i.e., the raw measurements before any background correction) from patients.
Table 6.
Overall mean and range of net dose rate measurements (μSv h−1) and normalized net dose rates per injected activity (μSv h−1 injected MBq−1) at 0, 24, 48, and 144 h and distances of 0, 0.3, 1.0 m from study patients administered 223Ra dichloride.
| Time post administration (h) | Distance (m) | μSv h−1
|
μSv h−1 injected MBq−1
|
||
|---|---|---|---|---|---|
| Mean | Range | Mean | Range | ||
| 0 | 0.0 | 3.95 | 1.0–11 | 0.49 | 0.1–1.0 |
| 0 | 0.3 | 0.95 | 0.2–2.2 | 0.11 | 0.04–0.2 |
| 0 | 1.0 | 0.18 | 0.05–0.5 | 0.02 | 0.01–0.1 |
| 24 | 0.0 | 3.93 | 1.8–5.3 | 0.80 | 0.5–1.2 |
| 24 | 0.3 | 0.84 | 0.3–1.9 | 0.15 | 0.07–0.2 |
| 24 | 1.0 | 0.13 | 0.05–0.2 | 0.03 | 0.01–0.05 |
| 48 | 0.0 | 3.78 | 0.2–13 | 0.57 | 0.05–1.7 |
| 48 | 0.3 | 0.65 | 0.05–2.3 | 0.09 | 0.01–0.3 |
| 48 | 1.0 | 0.11 | 0.05–0.3 | 0.02 | 0.01–0.04 |
| 144 | 0.0 | 0.25 | 0.2–0.3 | 0.05 | 0.04–0.05 |
| 144 | 0.3 | 0.05 | 0.05–0.05 | 0.01 | 0.01–0.01 |
| 144 | 1.0 | 0.05 | 0.05–0.05 | 0.01 | 0.01–0.01 |
Fig. 2.
Whole-body scan showing multiple metastatic disease sites in bone. Images of whole-body scans showing anterior (A) and posterior (B) 99mTc MDP bone uptake as compared with anterior (C) and posterior (D) 223Ra uptake following intravenous injection. Although 223Ra images are lower counts and noisier than the bone scan, they clearly show focal accumulation in the most obvious bone metastases: for example, the left scapula and several vertebrae. In addition, excretion into the ascending and transverse colon is noted.
Whole body effective half-lives based on measured dose rate readings for a subset of nine administrations and a mono-exponential fit (Microsoft Excel) were highly dependent upon fecal compartment transfer and ranged from about 2.6–11.4 d with a mean effective half-life of 6.5 ± 3.1 d.
DISCUSSION
Once injected, both alpha and beta particles are effectively stopped by the patient’s own tissue. The range of alpha radiation in human tissue is less than 100 μm. Due to distribution in the body and attenuation in the patient’s body mass, the gamma-radiation outside the patient’s body was expected to be low. In this study, the mean measured normalized dose rate per injected activity at 1 m was 0.02 μSv h−1 injected MBq−1 immediately following administration. As expected, this is less than the conservative theoretical exposure rate constant for an unshielded point source of 223Ra in equilibrium with progeny of approximately 0.05 μSv h−1 MBq−1 (Smith and Stabin 2012). The measurement of dose rates in this low range can be affected by statistical variability, background fluctuations (especially in an active nuclear medicine department), and geometry (Willegaignon et al. 2007; de Carvalho et al. 2011). For example, in one patient, the normalized exposure rate at 1 m was measured as 0.1 μSv h−1 injected MBq−1 immediately following administration, a value that was likely artificially high due to background fluctuations in the nuclear medicine injection area during the measurement.
Based on these measurements, there are no restrictions on family contact after administration of 223Ra dichloride. The product can be given on an outpatient basis, and there are no restrictions on normal interactions with friends, relations, or co-workers. Radium-223 is mainly excreted from the patient through the feces, although either urine or blood may contain low levels of radium. For this clinical study, radiation safety staff provided patients with verbal and written instructions describing simple steps to be followed at home in connection with blood, urine, or stools for a period of 1 wk after dosing. An example is given in Fig. 1. Such instructions are, of course, highly dependent on local regulatory guidance.
At 1 wk post-administration, most of the remaining in vivo activity is bound to the skeleton. In case of subsequent orthopedic surgery or invasive post-mortem examinations within 2 mo after administration of the study drug, all involved personnel should be notified of the potential presence of radioactivity in order to minimize potential contamination. Biological waste from surgery or autopsies should be evaluated for radioactive material and disposed according to local regulations and procedures. Cremation of a body containing 223Ra does not present a significant risk to the local population or to the crematorium workers themselves, even if the worst-case scenarios are employed. When crematorium workers receive a body that contains any type of radioactivity, they should be suitably trained, informed beforehand, and given suitable personal protection equipment. The general discussion in NCRP Report number 155 should serve as a template for these considerations (NCRP 2006). The short half-life of the radionuclide and its decay products, combined with the very short penetration depth of alpha radiation, means that there is virtually no radiation dose received during a burial process.
CONCLUSION
The use of 223Ra dichloride has been shown to be safe and straightforward to administer using conventional nuclear medicine equipment. Surface dose rates from vials and syringes containing 223Ra dichloride are generally lower than those from other common radiopharmaceuticals. Dose rates from patients administered 223Ra dichloride were typically less than 2 μSv h−1 MBq−1 on contact and averaged 0.02 μSv h−1 MBq−1 at 1 m immediately following administration. Such low external dose rates from treated patients are well within regulatory guidelines for patient release following administration.
There is some evidence from this study and subsequent studies that demonstrate significantly improved overall survivalwith very low toxicity, suggesting that 223Ra may provide a new standard of care for patients with CRPC and bone metastases. The use of a safely implementable alpha-particle based therapy may be the most significant development in the treatment of CRPC in many years.
Acknowledgments
This study was sponsored in part by Algeta ASA, Oslo, Norway.
Footnotes
Jorge A. Carrasquillo, John L. Humm and Joseph O’Donoghue consult for Algeta ASA. Anne-Kirsti Aksnes, Colin Biggin and Vigdis Reinton are employees of Algeta ASA. All other authors declare no conflicts of interest.
References
- Akerley W, Butera J, Wehbe T, Noto R, Stein B, Safran H, Cummings F, Sambandam S, Maynard J, Di Rienzo G, Leone L. A multiinstitutional, concurrent chemoradiation trial of strontium-89, estramustine, and vinblastine for hormone refractory prostate carcinoma involving bone. Cancer. 2002;94:1654–1660. doi: 10.1002/cncr.10437. [DOI] [PubMed] [Google Scholar]
- Amato RJ, Hernandez-McClain J, Henary H. Bone-targeted therapy: phase II study of strontium-89 in combination with alternating weekly chemohormonal therapies for patients with advanced androgen-independent prostate cancer. Am J Clin Oncol. 2008;31:532–538. doi: 10.1097/COC.0b013e318172aa92. [DOI] [PubMed] [Google Scholar]
- Autio KA, Scher HI, Morris MJ. Therapeutic strategies for bone metastases and their clinical sequelae in prostate cancer. Curr Treat Options Oncol. 2012;13:174–188. doi: 10.1007/s11864-012-0190-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman G, Charette M, Reid R, Sathya J. Radiopharmaceuticals for the palliation of painful bone metastasis-a systemic review. Radiother Oncol. 2005;75:258–70. doi: 10.1016/j.radonc.2005.03.003. [DOI] [PubMed] [Google Scholar]
- Bruland OS, Nilsson S, Fisher DR, Larsen RH. High-linear energy transfer irradiation targeted to skeletal metastases by the alpha-emitter 223Ra: adjuvant or alternative to conventional modalities? Clin Cancer Res. 2006;12:6250s–6257s. doi: 10.1158/1078-0432.CCR-06-0841. [DOI] [PubMed] [Google Scholar]
- Carrasquillo JA, O’Donoghue JA, Pandit-Taskar N, Humm JL, Rathkopf DE, Slovin SF, Williamson MJ, Lacuna K, Aksnes A, Larson SM, Scher HI, Morris MJ. Phase 1 pharmacokinetic and biodistribution study with escalating doses of 223Radichloride in men with castration-resistant metastatic prostate cancer. Eur J Nucl Med Mol Imaging. 2013;40(9):1384–93. doi: 10.1007/s00259-013-2427-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauer LT, Mayer D. Applications of systematic error bounds to detection limits for practical counting. Health Phys. 1993;65:89–91. doi: 10.1097/00004032-199307000-00011. [DOI] [PubMed] [Google Scholar]
- de Carvalho AB, Jr, Stabin MG, Siegel JA, Hunt J. Comparison of point, line and volume dose calculations for exposure to nuclear medicine therapy patients. Health Phys. 2011;100:185–190. doi: 10.1097/HP.0b013e3181eacf38. [DOI] [PubMed] [Google Scholar]
- Eckerman K, Endo A. ICRP Publication 107. Nuclear decay data for dosimetric calculations. Ann ICRP. 2008;38:7–96. doi: 10.1016/j.icrp.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Fizazi K, Beuzeboc P, Lumbroso J, Haddad V, Massard C, Gross-Goupil M, Di Palma M, Escudier B, Theodore C, Loriot Y, Tournay E, Bouzy J, Laplanche A. Phase II trial of consolidation docetaxel and samarium-153 in patients with bone metastases from castration-resistant prostate cancer. J Clin Oncol. 2009;27:2429–2935. doi: 10.1200/JCO.2008.18.9811. [DOI] [PubMed] [Google Scholar]
- Floeckher J. Application note: alpha/beta swipe assays. Meriden, CT: Packard Instrument Company; 2012. p. ABA-006. [Google Scholar]
- Frame P, Abelquist EW. Use of smears for assessing removable contamination. Health Phys. 1999;76:S57–S66. [Google Scholar]
- Goyal J, Antonarakis ES. Bone-targeting radiopharmaceuticals for the treatment of prostate cancer with bone metastases. Cancer Lett. 2012;323:135–146. doi: 10.1016/j.canlet.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham MC, Scher HI, Liu GB, Yeh SD, Curley T, Daghighian F, Goldsmith SJ, Larson SM. Rhenium-186-labeled hydroxyethylidene diphosphonate dosimetry and dosing guidelines for the palliation of skeletal metastases from androgen-independent prostate cancer. Clin Cancer Res. 1999;5:1307–1318. [PubMed] [Google Scholar]
- Hall E, Giaccia A. Radiobiology for the radiologist. New York: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- Henriksen G, Breistol K, Bruland OS, Fodstad O, Larsen RH. Significant antitumor effect from bone-seeking, alpha-particle-emitting (223)Ra demonstrated in an experimental skeletal metastases model. Cancer Res. 2002;62:3120–3125. [PubMed] [Google Scholar]
- ICRP. Radiological protection in medicine. Vol. 37. Oxford: Elsevier Ann ICRP; 2008. pp. 1–63. ICRP Publication 105. [Google Scholar]
- Keller ET, Zhang J, Cooper CR, Smith PC, McCauley LK, Pienta KJ, Taichman RS. Prostate carcinoma skeletal metastases: cross-talk between tumor and bone. Cancer Metastasis Rev. 2001;20:333–349. doi: 10.1023/a:1015599831232. [DOI] [PubMed] [Google Scholar]
- Kelly WK, Scher HI, Mazumdar M, Vlamis V, Schwartz M, Fossa SD. Prostate-specific antigen as a measure of disease outcome in metastatic hormone-refractory prostate cancer. J Clin Oncol. 1993;11:607–615. doi: 10.1200/JCO.1993.11.4.607. [DOI] [PubMed] [Google Scholar]
- Morris MJ, Pandit-Taskar N, Carrasquillo J, Divgi CR, Slovin S, Kelly WK, Rathkopf D, Gignac GA, Solit D, Schwartz L, Stephenson RD, Hong C, Delacruz A, Curley T, Heller G, Jia X, O’Donoghue J, Larson S, Scher HI. Phase I study of samarium-153 lexidronam with docetaxel in castration-resistant metastatic prostate cancer. J Clin Oncol. 2009;27:2436–2442. doi: 10.1200/JCO.2008.20.4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Council on Radiation Protection and Measurements. Management of radionuclide therapy patients. Bethesda, MD: NCRP; 2006. Report No. 155. [Google Scholar]
- Nilsson S, Franzen L, Parker C, Tyrrell C, Blom R, Tennvall J, Lennernas B, Petersson U, Johannessen DC, Sokal M, Pigott K, Yachnin J, Garkavij M, Strang P, Harmenberg J, Bolstad B, Bruland OS. Bone-targeted radium-223 in symptomatic, hormone-refractory prostate cancer: a randomised, multicentre, placebo-controlled phase II study. Lancet Oncol. 2007;8:587–594. doi: 10.1016/S1470-2045(07)70147-X. [DOI] [PubMed] [Google Scholar]
- Nilsson S, Haugen I, Aksnes A, O’Bryan-Tear CG, Parker C. 7008 Poster Discussion. Twenty-four-month safety data from phase II studies of radium-223 chloride, a first-in-class alpha-pharmaceutical with a highly favorable safety profile for patients with castration-resistant prostate cancer (CRPC) and bone metastases. Eur J Cancer. 2011;47:S486. [Google Scholar]
- Nilsson S, Larsen RH, Fossa SD, Balteskard L, Borch KW, Westlin JE, Salberg G, Bruland OS. First clinical experience with alpha-emitting radium-223 in the treatment of skeletal metastases. Clin Cancer Res. 2005;11:4451–4459. doi: 10.1158/1078-0432.CCR-04-2244. [DOI] [PubMed] [Google Scholar]
- Nilsson S, Strang P, Asknes AK, Franzen L, Olivier P, Pecking A, Staffurth J, Vasanthan S, Andersson C, Bruland OS. A randomized, dose-response, multicenter phase II study of radium-223 chloride for the palliation of painful bone metastases in patients with castration-resistant prostate cancer. Eur J Cancer. 2012;48:678–686. doi: 10.1016/j.ejca.2011.12.023. [DOI] [PubMed] [Google Scholar]
- Parker C, Heinrich D, O’Sullivan JM, Fossa S, Chadacki A, Demkow T, Cross A, Bolstad B, Garcia-Vargas J, Sartor O. Overall survival benefit of radium-223 chloride (Alpharadin™) in the treatment of patients with symptomatic bone metastases in castration-resistant prostate cancer (CRPC): a phase III randomized trial (ALSYMPCA) Eur J Cancer. 2011;47(3) [Google Scholar]
- Ritter MA, Cleaver JE, Tobias CA. High-LET radiations induce a large proportion of non-rejoining DNA breaks. Nature. 1977;266:653–655. doi: 10.1038/266653a0. [DOI] [PubMed] [Google Scholar]
- Sartor AO, Heinrich D, Helle SI, O’Sullivan JM, Fossa SD, Chodacki A, Demkow T, Logue JP, Seke M, Widmark A, Johannessen DC, Nilsson S, Hoskin P, Solberg A, James ND, Syndikus I, Vogelzang NJ, O’Bryan-Tear CG, Shan M, Parker C. Radium-223 chloride impact on skeletal-related events in patients with castration-resistant prostate cancer (CRPC) with bone metastases: a phase III randomized trial (ALYSYMPCA) J Clin Oncol. 2012;30:Abs 9. [Google Scholar]
- Saylor PJ, Lee RJ, Smith MR. Emerging therapies to prevent skeletal morbidity in men with prostate cancer. J Clin Oncol. 2011;29:3705–3714. doi: 10.1200/JCO.2010.34.4994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarpitta SC, Fisenne IM. Calibration of a liquid scintillation counter for alpha, beta and Cerenkov counting. New York: U.S. Department of Energy Environmental Measurements Laboratory; 1996. Report EML-583. [Google Scholar]
- Scher HI, Kelly WM, Zhang ZF, Ouyang P, Sun M, Schwartz M, Ding C, Wang W, Horak ID, Kremer AB. Post-therapy serum prostate-specific antigen level and survival in patients with androgen-independent prostate cancer. J Natl Cancer Inst. 1999;91:244–251. doi: 10.1093/jnci/91.3.244. [DOI] [PubMed] [Google Scholar]
- Scher HI, Sawyers CL. Biology of progressive, castration-resistant prostate cancer: directed therapies targeting the androgen-receptor signaling axis. J Clin Oncol. 2005;23:8253–8261. doi: 10.1200/JCO.2005.03.4777. [DOI] [PubMed] [Google Scholar]
- Sgouros G, Roeske JC, McDevitt MR, Palm S, Allen BJ, Fisher DR, Brill AB, Song H, Howell RW, Akabani G, Bolch WE, Meredith RF, Wessels BW, Zanzonico PB. MIRD Pamphlet No. 22 (abridged): radiobiology and dosimetry of alpha-particle emitters for targeted radionuclide therapy. J Nucl Med. 2010;51:311–328. doi: 10.2967/jnumed.108.058651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DS, Stabin MG. Exposure rate constants and lead shielding values for over 1,100 radionuclides. Health Phys. 2012;102:271–291. doi: 10.1097/hp.0b013e318235153a. [DOI] [PubMed] [Google Scholar]
- Suttmann H, Grgic A, Lehmann J, Zwergel U, Kamradt J, Gouverneur E, Pinkert J, Stockle M, Kirsch CM, Nestle U. Combining 153Sm-lexidronam and docetaxel for the treatment of patients with hormone-refractory prostate cancer: first experience. Cancer Biother Radiopharm. 2008;23:609–618. doi: 10.1089/cbr.2008.0487. [DOI] [PubMed] [Google Scholar]
- Tu SM, Kim J, Pagliaro LC, Vakar-Lopez F, Wong FC, Wen S, General R, Podoloff DA, Lin SH, Logothetis CJ. Therapy tolerance in selected patients with androgen-independent prostate cancer following strontium-89 combined with chemotherapy. J Clin Oncol. 2005;23:7904–7910. doi: 10.1200/JCO.2005.01.2310. [DOI] [PubMed] [Google Scholar]
- U.S. Nuclear Regulatory Commission. Minimum detectable concentrations with typical radiation survey instruments for various contaminants and field conditions. Washington, DC: United States Nuclear Regulatory Comission; 1998. NUREG-1507. [Google Scholar]
- U.S. Nuclear Regulatory Commission. Program specific guidance about medical use licenses. Vol. 9. Washington, DC: Division of Industrial and Medical Nuclear Safety. Office of Nuclear Material Safety and Safeguards; United States Nuclear Regulatory Commission; 2008. Consolidated guidance about materials licenses. Final report; NUREG-1556. Rev. 2. [Google Scholar]
- Weinfurt KP, Li Y, Castel LD, Saad F, Timbie JW, Glendenning GA, Schulman KA. The significance of skeletal-related events for the health-related quality of life of patients with metastatic prostate cancer. Ann Oncol. 2005;16:579–584. doi: 10.1093/annonc/mdi122. [DOI] [PubMed] [Google Scholar]
- Willegaignon J, Guimaraes MI, Stabin MG, Sapienza MT, Malvestiti LF, Marone MM, Sordi GM. Correction factors for more accurate estimates of exposure rates near radioactive patients: experimental, point, and line source models. Health Phys. 2007;93:678–688. doi: 10.1097/01.HP.0000275298.69543.5c. [DOI] [PubMed] [Google Scholar]