Abstract
Objectives. To evaluate the effectiveness of the Safety and Health Involvement For Truckers (SHIFT) intervention with a randomized controlled design.
Methods. The multicomponent intervention was a weight-loss competition supported with body weight and behavioral self-monitoring, computer-based training, and motivational interviewing. We evaluated intervention effectiveness with a cluster-randomized design involving 22 terminals from 5 companies in the United States in 2012 to 2014. Companies were required to provide interstate transportation services and operate at least 2 larger terminals. We randomly assigned terminals to intervention or usual practice control conditions. We assessed participating drivers (n = 452) at baseline and 6 months.
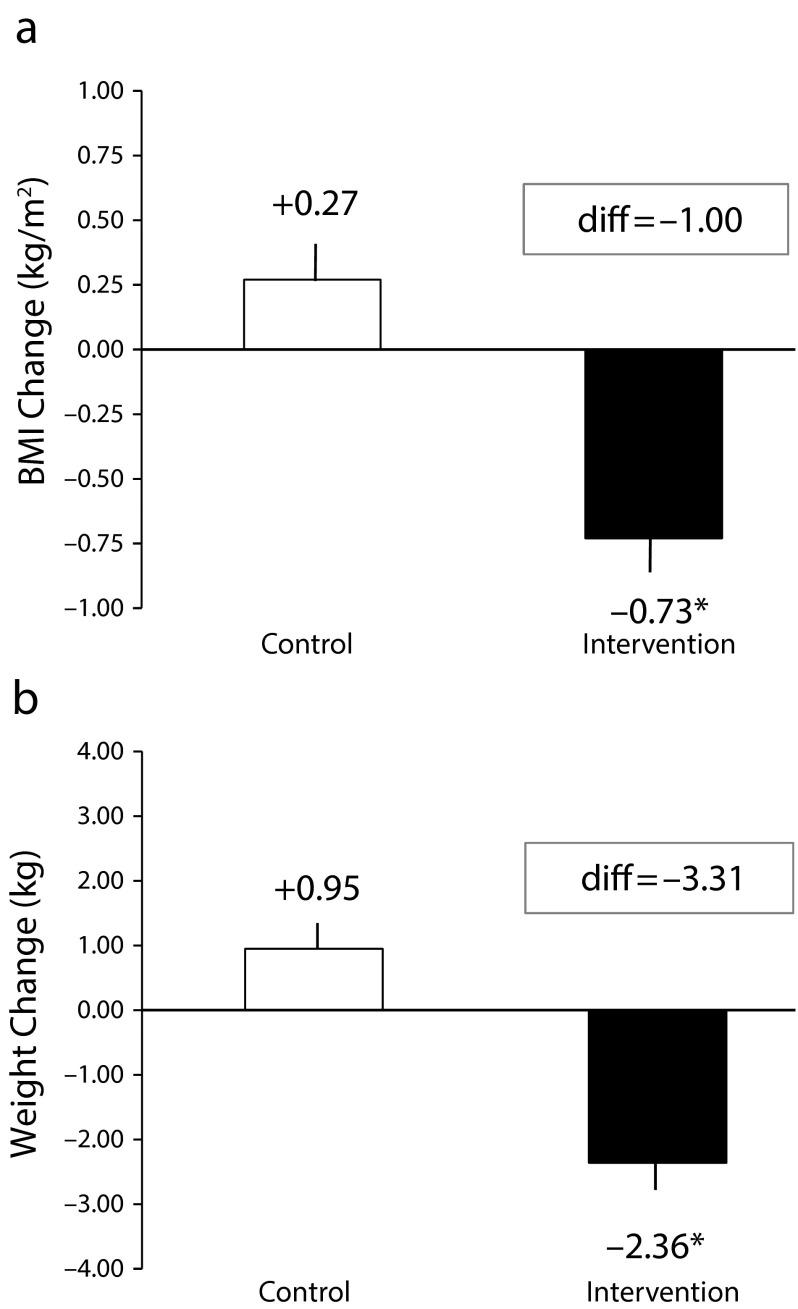
Results. In an intent-to-treat analysis, the postintervention difference between groups in mean body mass index change was 1.00 kilograms per meters squared (P < .001; intervention = −0.73; control = +0.27). Behavioral changes included statistically significant improvements in fruit and vegetable consumption and physical activity.
Conclusions. Results establish the effectiveness of a multicomponent and remotely administered intervention for producing significant weight loss among commercial truck drivers.
Nearly 70% of US freight travels on a truck at some point.1 From this perspective, the men and women who operate large commercial trucks are the backbone of the tangible goods economy. However, the welfare of this workforce is in jeopardy. Obesity is twice as prevalent among US truck drivers compared with the general population (69% vs 31%).2 Regulated medical conditions associated with obesity, such as uncontrolled hypertension, may disqualify drivers from working. In addition to creating stressful precarious employment, obesity and associated sleep disorders3 place drivers at personally imperceptible—yet very real—increased risk of crash involvement. To illustrate, new truck drivers with class II or III obesity (World Health Organization criteria) have greater than 50% higher odds of crash involvement during their first 2 years.4 Obstructive sleep apnea roughly doubles drivers’ crash risk.5 Large truck crashes, although more rare per vehicle mile traveled than those involving personal vehicles, are 20% to 55% more likely to result in a fatality.6 Thus, improving the well-being, health, and safety of commercial truck drivers is a public health priority.
Diverse multilevel interventions are needed to reduce obesity hazards and support weight loss among commercial truck drivers. Obesogenic factors in trucking include long work hours, prolonged sitting, unfavorable sleeping conditions, prevalent calorie-dense foods, and limited access to whole foods and safe places to walk. Evaluations of corporate health programs for drivers are typically limited to brief case studies.7 Peer-reviewed evaluations of body weight management interventions among truck drivers (or among samples including truck drivers) identified in our literature search included 2 uncontrolled pilot studies,8–10 3 studies with nonrandomly selected control groups,11–13 and 2 randomized controlled trials.14,15 Three of these interventions produced mean or median within-group weight loss greater than 3 kilograms.8,10,15 Only 1 of these more effective approaches, a 12-month lifestyle counseling intervention implemented with Scandinavian truck and bus drivers,15 was established as effective with a randomized controlled design.
The Safety and Health Involvement For Truckers (SHIFT) intervention model involves evidence-based tactics amenable for implementation with isolated workers, including weight-loss competition, behavior and body weight self-monitoring, computer-based training, and motivational interviewing.16–19 In the previously referenced SHIFT pilot study, the intervention produced significant within-group mean weight loss of −3.5 kilograms (7.8 lb).8 However, the lack of a control group and small sample prevent strong conclusions about effectiveness. To address the public health need and research gaps, we conducted a randomized controlled trial of SHIFT with US truck drivers.
METHODS
The project employed a cluster-randomized controlled design with intervention and usual-practice control conditions. The unit of randomization was a company terminal, which was defined as a company-owned facility with driver services or amenities beyond parking (e.g., drivers’ lounge, laundry, maintenance). Driver measurements were collected at baseline and at 6 months. On the basis of an a priori power analysis, we selected a target sample size of 520 drivers to provide a 0.99 probability of detecting a body weight effect of the magnitude observed in the pilot.
Primary hypotheses were that the intervention would be more effective than usual practice at producing (1) reductions in directly measured body weight and body mass index (BMI; defined as weight in kilograms divided by the square of height in meters), (2) improvements in self-reported dietary behaviors (fruit and vegetable intake, calories from fat, sugary food and drink consumption, fast-food consumption), and (3) improvements in self-reported physical activity.
Researchers recruited companies through personal contacts, referrals, and phone calls. Companies were required to provide interstate transportation services and operate at least 2 larger terminals (about 80+ drivers each). Five companies participated with driver employment levels ranging from about 500 to more than 2000 drivers. Some companies offered health programs for drivers, but none offered a structured weight-loss program during the study. Common operational divisions included national line haul, regional, temperature-controlled, heavy haul, and dedicated transportation. At each company, we selected an even number of terminals, matched in pairs by size (number of drivers), and then we randomized 1 terminal from each pair to the intervention condition and assigned the other to the control condition. Companies participated sequentially between April 23, 2012, and March 7, 2014, in 2 waves (2 in wave 1, 3 in wave 2).
Interested drivers responded to advertisements and were screened for eligibility by phone. Qualified drivers were mailed a survey and instructions for attending open enrollment periods at terminals. Eligibility criteria included a BMI of at least 27, an interest in managing or losing weight, and no medical conditions prohibiting increased physical activity. The first and smallest company had an eligibility requirement of 9 months of job tenure. Tenure requirements were removed after the next 2 companies experienced lower-than-expected enrollment at their first terminals.
Operations staff helped route interested drivers to terminals during enrollment. Researchers obtained informed consent before data collection. Ultimately, 452 drivers fully enrolled at baseline (86.9% of planned sample); 275 returned at 6 months (Figure 1). Drivers received $40 and study gear (cinch bag, water bottle, towel) at baseline, and a study t-shirt and $40 (wave 1) or $80 (wave 2) at 6 months. Each time point included lottery drawings for several awards for supplemental compensation (range = $100 to $500). One company allowed study enrollment to substitute for a corporate health screening program that earned a health care premium discount ($600 per year).
FIGURE 1—
Consort Diagram: Safety and Health Involvement For Truckers (SHIFT) Randomized Controlled Trial, United States, 2012–2014
Note. In the intervention arm, we defined completing intervention criteria as submitting 15 or more body weight and behavior logs, passing 4 training units with 80% correct or better, and completing 4 motivational interviewing phone calls.
aIntent-to-treat analyses were performed. All participants who completed enrollment were included in analyses.
Implementation of Conditions
After baseline data collection, participants received immediate feedback on health assessment results relative to normal or healthy standards (plus a mailed follow-up letter). Drivers were then informed of their condition assignment without disclosure that it was dependent on their terminal. Control participants received compensation and materials and concluded enrollment. Intervention drivers completed a supplemental orientation and consent process before finishing enrollment.
Intervention procedures.
The SHIFT intervention as studied in the pilot8 was updated for the current project (technology, methods, and training content). However, core tactics remained the same. As before, the program involved a 6-month weight-loss competition supported with body weight and behavioral self-monitoring, computer-based training, and motivational interviewing. Intervention activities were facilitated through a mobile-friendly Web site.
The intervention began with a brief computer-based orientation training and supplemental consent process. Researchers then helped drivers set up a Web site account, select a weight-loss goal (8%, 10%, or 12% of body weight), and schedule their first coaching appointment. Drivers received a business card with their login and technical support contact information, a step counter, and a resource book. Intervention terminals were loaned 1 laptop for the drivers’ lounge and another for check out with a paid wireless Internet card.
Within companies, drivers were organized into weight-loss squads of 10 to 18 individuals (mean = 14.31; SD = 2.77) based on terminal and enrollment time. Squads within each company competed to achieve the highest percentage of their collective weight-loss goals. Drivers were asked to complete weekly Web site logs of their body weight and the number of days they met their chosen behavioral goal(s). Options were stop or reduce a high-calorie habit, reduce portion sizes, eat more fruit and vegetable servings, walk (or do other similar exercise) on most days each week (4 of 7), and sleep 7 to 8 hours each day. Drivers also logged completed training and coaching (see next paragraph). Competition and participation feedback was provided at individual, intrasquad, and intersquad levels.
Computer-based training was administered in cTRAIN software (Northwest Education Training and Assessment, Lake Oswego, OR), which integrates evidence-based behavioral instruction principles. Content featured a Total Worker Health20 orientation by emphasizing the cross-cutting benefits of healthy sleep for both body weight management21 and occupational safety.22,23 Topics included the orientation, SHIFT 10% (healthy sustainable weight loss), SHIFT exercise, SHIFT eating, and SHIFT sleep. Each required about 20 to 45 minutes to complete and 80% correct on a posttest to pass.
Four trained female coaches (3 were members of the Motivational Interviewing Network of Trainers) provided up to 4 motivational interviewing calls. The role of coaches was to provide motivational interviewing–adherent counseling to help drivers develop and implement personalized plans for achieving their weight-loss goals. The first call was typically scheduled within 2 weeks of enrollment and included a coaching overview; exploring the driver’s history and reasons for change; discussing his or her weight-loss goal and exploring behavioral goal options; eliciting ideas, commitments, and a change plan; and a summary with follow-up. Subsequent calls were spaced according to driver preference and followed protocols tailored to time in the program. Coaching adhered to all relevant federal and corporate cell phone safety laws and policies for commercial truck drivers. A lead coach supervised the process and monitored adherence to motivational interviewing technique.
Winning weight loss squads received SHIFT jackets and $100 gift certificates. Drivers completing 15 or more logs and all training and coaching earned SHIFT Certification and a $100 gift certificate. In wave 2, drivers earned $40 for completing their first log, training, and coaching call during the first 3 weeks, and then $60 for SHIFT Certification.
Control of information about the intervention.
Intervention feedback and results were not posted at terminals, and were withheld from corporate leadership and control drivers until data collection was completed. Controls were offered intervention training when the study concluded.
Primary Outcome Measures
We computed BMI from directly measured body weight (resolution 0.5 lb; Tanita TBF-310GS scale, Tanita Corporation, Tokyo, Japan) and height (nearest 1/8 inch; SECA 213 stadiometer, SECA, Hamburg, Germany). We verified scale calibration daily with a 25-pound weight (11.34 kg). Drivers were weighed in work clothes after removing shoes, socks, belts, watches, and items from pockets.
Dietary measures included daily fruit and vegetable consumption,24 percentage of calories from fat,25 and frequency of sugary snacks, sugary drinks, and fast-food meals.26 We measured physical activity with the healthy physical activity scale.27 We measured sleep duration and quality with the Pittsburgh Sleep Quality Index.28 Dietary, exercise, and sleep questions asked participants to report their behaviors during the past month.
We computed mean blood pressure from 3 measures, each taken 1 minute apart, after an initial 3-minute rest period (Omron HEM-907XL, Kyoto, Japan). We measured blood lipids and glucose by fingerstick following a minimum 3-hour fast (Cholestech LDX, Alere Incorporated, Waltham, MA). Supplemental anthropometric measures included body fat percentage (Tanita TBF-310GS scale, Tanita Corporation, Tokyo, Japan) and waist and hip circumferences (Gulick II measuring tape, Country Technology Co, Gays Mills, WI). Safety measures included self-reported driving safety incidents and total workdays missed because of injury and illness in the past 6 months.
We collected a range of driver demographics and work or health history variables, including reported lifetime diagnoses and current treatments for high blood pressure, diabetes, and obstructive sleep apnea.
Statistical Analysis
Before conducting the main analyses, we explored differences in baseline characteristics between experimental groups by using generalized estimating equations to account for the nesting of drivers within terminals (i.e., each driver belonged to a terminal). We also examined differences in baseline characteristics between study completers and dropouts. We included variables on which groups differed at baseline, or that were associated with drop out, as covariates in the main analyses.
We used generalized estimating equations for main analyses and we included all fully enrolled drivers as randomized. We used negative binomial or binomial models when appropriate. We included group assignment, time (baseline and 6 months), and the group-by-time interaction in the models, with drivers nested within terminals.
RESULTS
Control (n = 223) and intervention (n = 229) groups were predominantly male (86.0% and 86.9%, respectively) and had mean BMIs in the class II obesity range (35.44 and 35.73, respectively). At baseline, groups did not differ significantly in BMI, age, gender, or race (see Table 1 for demographics). However, we observed significant (P < .05) differences between control and intervention groups at baseline for Hispanic ethnicity (6.9% and 13.3%, respectively), days away from home per dispatch (mean = 4.1 days and mean = 3.7 days, respectively [scale interval 3 = 5 to 7 days; scale interval 4 = 8 days to 2 weeks]), proportion working 5 or more days away from home per dispatch (61.5% and 50.0%, respectively), frequency of manual material handling (mean = 1.3 and mean = 0.9, respectively [scale interval 1 = more than once per year]), and self-reported high blood pressure diagnosis (28.1% and 40.2%, respectively). Compared with drivers who returned at 6 months, drivers lost to follow-up were significantly younger (mean = 45.4 years vs completers mean = 49.3 years), had fewer years as a truck driver (mean = 9.2 years vs completers mean = 13.0 years), and spent more days away from home per dispatch (mean = 4.3 vs completers mean = 3.6 [scale interval 3 = 5 to 7 days; scale interval 4 = 8 days to 2 weeks]). We included all variables in which we observed significant baseline differences (between groups or associated with drop out) except years as a truck driver (highly correlated with age), proportion working 5 or more days away from home per dispatch (correlated with days away per dispatch), and high blood pressure diagnosis (blood pressure was a secondary outcome) as covariates in the main analyses.
TABLE 1—
Participant Characteristics by Condition at Baseline: Safety and Health Involvement For Truckers (SHIFT) Randomized Controlled Trial: United States, 2012–2014
| Control (n = 223) |
Intervention (n = 229) |
||||
| Variables | No. | Mean (SD) or % | No. | Mean (SD) or % | P |
| Age, y | 220 | 47.6 (11.6) | 225 | 47.9 (11.2) | .80 |
| Gender = male | 190 | 86.0 | 199 | 86.9 | .77 |
| Race | .06 | ||||
| American Indian/Alaskan Native | 2 | 0.9 | 4 | 1.8 | |
| Asian | 1 | 0.4 | 0 | 0.0 | |
| Native Hawaiian/Pacific Islander | 3 | 1.4 | 0 | 0.0 | |
| Black/African American | 11 | 5.0 | 22 | 9.8 | |
| White | 181 | 82.6 | 168 | 74.7 | |
| > 1 race | 13 | 5.9 | 14 | 6.2 | |
| Other | 8 | 3.7 | 17 | 7.6 | |
| Hispanica | 14 | 6.9 | 28 | 13.3 | .029 |
| Married or living with partner | 148 | 66.7 | 143 | 62.5 | .35 |
| Dependent children ≥ 1 | 66 | 29.9 | 82 | 36.1 | .16 |
| Education | .37 | ||||
| High-school diploma or GED | 99 | 47.4 | 120 | 56.3 | |
| Vocational/technical certificate | 66 | 31.6 | 50 | 23.5 | |
| Associate degree | 26 | 12.4 | 24 | 11.3 | |
| Bachelor’s degree | 14 | 6.7 | 15 | 7.0 | |
| Graduate degree | 4 | 1.9 | 4 | 1.9 | |
| Days away per dispatcha,b | 221 | 4.1 (1.4) | 228 | 3.7 (1.6) | .002 |
| Away ≥ 5 nights per dispatcha | 136 | 61.5 | 114 | 50.0 | .014 |
| Weekly work hours | .86 | ||||
| 0–54.99 | 47 | 21.4 | 43 | 19.4 | |
| 55–64.99 | 84 | 38.2 | 85 | 38.3 | |
| ≥ 65 | 89 | 40.5 | 94 | 42.3 | |
| Tenure as truck driver, y | 220 | 11.2 (10.8) | 229 | 11.8 (10.0) | .49 |
| Tenure current company, y | .98 | ||||
| < 1 | 79 | 35.6 | 82 | 36.0 | |
| 1–2.49 | 37 | 16.7 | 38 | 16.7 | |
| 2.5–4.99 | 28 | 12.6 | 26 | 11.4 | |
| ≥ 5 | 78 | 35.1 | 82 | 36.0 | |
| Manual material handlinga,c | 222 | 1.3 (1.4) | 228 | 0.9 (1.2) | .001 |
| Smoker (past month) | 65 | 29.3 | 71 | 31.0 | .69 |
| Health conditions | |||||
| Diabetes | 29 | 13.1 | 27 | 11.8 | .68 |
| Meds for diabetesd | 23 | 85.2 | 23 | 88.5 | .73 |
| High blood pressurea | 62 | 28.1 | 92 | 40.2 | .007 |
| Meds for high blood pressured | 52 | 82.5 | 69 | 75.8 | .32 |
| Obstructive sleep apnea | 48 | 21.6 | 33 | 14.5 | .051 |
| Treatments for obstructive sleep apnead | 44 | 91.7 | 27 | 84.4 | .70 |
Note. GED = general equivalency diploma. The sample size was n = 452.
Statistically significant between-group differences observed at baseline. For continuous variables, P values are based on a 2-sample nonparametric test. For dichotomous or categorical variables, P values are based on the χ2 test. Percentage calculations are based on number of participants responding to each item and are not adjusted for missingness.
We assessed days away from home per dispatch with frequency intervals of 1 = home every night; 2 = 2 to 4 days; 3 = 5 to 7 days; 4 = 8 days to 2 weeks; and 5 = more than 2 weeks.
We assessed manual material handling with a 5-level frequency scale: 0 = never; 1 = more than once per year; 2 = more than once per month; 3 = 1 or more times per week; 4 = daily.
Rows represent subsets of participants with the condition reporting some form of treatment. Levels of primary outcome variables did not significantly differ between groups at baseline.
Effects on Primary and Secondary Outcomes
Group-by-time interactions were statistically significant for BMI, body weight, fruit and vegetable servings, and days per week of physical activity (Table 2). At 6 months, the model-adjusted mean difference between groups in BMI changes was 1.00 unit (intervention −0.73; control +0.27; Figure 2). The adjusted standardized effect size for BMI was d = −0.14 (Cohen's d; adjusted mean difference in between-group changes divided by the average within-cluster baseline standard deviation [pooled across groups]). In body weight, the model-adjusted between-group difference was −3.31 kilograms (−7.29 lb; d = −0.13; intervention −2.36 kg [−5.20 lb]; control +0.95 kg [+2.09 lb]).
TABLE 2—
Generalized Estimating Equations Model-Adjusted Means (SE), Group Mean Differences, and Inferential Test Results for Primary and Secondary Outcomes: Safety and Health Involvement For Truckers (SHIFT) Randomized Controlled Trial, United States, 2012–2014
| Control, Mean (SE) |
Intervention, Mean (SE) |
|||||
| Variables | Baseline | 6 Mo | Baseline | 6 Mo | Mean Group Diff. (95% CI) | Interaction P |
| Primary outcomes | ||||||
| Body weight, lba | 234.09 (4.31) | 236.18 (4.40) | 237.34 (4.17) | 232.14 (4.32) | −7.29 (−9.76, −4.81) | |
| Body weight, kga | 106.40 (1.96) | 107.35 (2.00) | 107.88 (1.90) | 105.52 (1.96) | −3.31 | NA |
| Body mass indexa | 35.44 (0.60) | 35.71 (0.62) | 35.73 (0.58) | 35.00 (0.59) | −1.00 (−1.39, −0.62) | |
| Daily fruit or vegetable servingsa,b | 2.90 (0.08) | 2.59 (0.08) | 2.63 (0.08) | 3.02 (0.07) | 0.70 | .005 |
| % energy from fat | 33.26 (0.35) | 32.33 (0.37) | 33.63 (0.32) | 32.06 (0.35) | −0.64 (−1.55, 0.27) | |
| Sugary snacksb,c | 4.15 (0.04) | 3.78 (0.05) | 4.14 (0.04) | 3.54 (0.04) | −0.23 | .19 |
| Sugary drinksb,c | 4.58 (0.05) | 4.02 (0.06) | 4.68 (0.05) | 3.87 (0.06) | −0.25 | .32 |
| Fast foodb,c | 4.01 (0.04) | 3.75 (0.04) | 3.84 (0.03) | 3.38 (0.04) | −0.20 | .12 |
| Days per week with 30 min physical activitya,d | 1.39 (0.11) | 1.44 (0.12) | 1.19 (0.10) | 1.90 (0.12) | 0.67 (0.40, 0.94) | |
| Secondary outcomes | ||||||
| Sleep | ||||||
| Sleep quality indexe | 7.10 (0.32) | 6.63 (0.33) | 6.85 (0.30) | 6.36 (0.34) | −0.02 (−0.68, 0.63) | |
| Sleep duration, hours | 7.77 (0.16) | 7.75 (0.16) | 7.82 (0.15) | 8.04 (0.18) | 0.24 (−0.12, 0.60) | |
| Physical measures | ||||||
| Waist circumference, cma | 44.27 (0.52) | 44.47 (0.53) | 44.42 (0.47) | 43.86 (0.50) | −0.76 (−1.25, −0.27) | |
| Waist-to-hip ratio | 0.94 (0.01) | 0.95 (0.01) | 0.94 (0.01) | 0.94 (0.01) | −0.01 (−0.02, 0.00) | |
| % body fata | 35.82 (0.82) | 36.98 (0.85) | 36.71 (0.75) | 35.79 (0.80) | −2.09 (−2.99, −1.19) | |
| Systolic BP | 125.30 (1.22) | 124.92 (1.41) | 128.00 (1.29) | 126.75 (1.52) | −0.87 (−3.66, 1.92) | |
| Diastolic BP | 80.50 (0.96) | 79.28 (1.04) | 81.47 (0.97) | 80.47 (1.13) | 0.23 (−1.74, 2.19) | |
| Total cholesterol, mg/dL | 180.13 (3.81) | 171.29 (4.06) | 184.91 (3.45) | 182.45 (3.99) | 6.38 (−2.49, 15.25) | |
| HDL, mg/dL | 40.36 (1.02) | 39.10 (1.12) | 38.69 (1.00) | 38.89 (1.16) | 1.46 (−0.51, 3.44) | |
| LDL, mg/dL | 107.90 (3.29) | 101.77 (3.41) | 110.68 (2.76) | 109.22 (2.95) | 4.67 (−1.45, 10.80) | |
| Triglycerides, mg/dL | 178.70 (11.76) | 169.23 (10.84) | 187.62 (9.68) | 169.57 (10.51) | −8.58 (−30.76, 13.60) | |
| Blood glucose risk—moderate or highf,g | 0.06 (0.33) | 0.10 (0.36) | 0.11 (0.28) | 0.15 (0.33) | 0.00 | .84 |
| Safety | ||||||
| Driving safety incidents (count)b,h | 0.56 (0.16) | 0.40 (0.20) | 0.57 (0.15) | 0.55 (0.19) | 0.14 | .14 |
| Days missed illness or injury, (count)b,i | 0.32 (0.20) | 0.38 (0.25) | 0.35 (0.21) | 0.31 (0.22) | −0.10 | .30 |
Note. BP = blood pressure; CI = confidence interval; HDL = high-density lipoprotein; LDL = low-density lipoprotein; NA = not applicable.
Statistically significant intervention effects.
Negative binomial distribution. In the negative binomial models, intervention effect parameters are multiplicative functions of the transformed outcome means from the statistical model rather than additive functions (i.e., group differences in mean differences over time). To minimize potential confusion in interpretation, we report specific P values rather than confidence intervals for transformed negative binomial model parameters.
Items related to sugary snacks, drinks, and fast food were reported on 10 frequency intervals, in which a mean frequency interval of 4 represented 1 to 2 times per week.
We scored the healthy physical activity scale as the mean of 4 questions assessing days per week (0–7) with moderate or vigorous aerobic activity or strength training.
Global Pittsburgh Sleep Quality Index.
Binomial distribution. In the binomial model, intervention effect parameters are nonlinear (logit) functions of the transformed outcome means from the statistical model rather than additive functions (i.e., group differences in mean differences over time). To minimize potential confusion in interpretation, we report a specific P value rather than a confidence interval for the transformed binomial parameter.
We categorized blood glucose scores with standards based on fasting hours (random or fasting), and each participant was then given a score as normal or moderate-to-high risk. We coded blood glucose risk as 1 for those at moderate or high risk and 0 for none or low risk.
Sum of 3 questions asking about the number of moving violations, curb strikes, and collisions with property damage. Each question had answer options on a 6-point scale ranging from 0 to 5+.
Simple sum of scores from 2 questions asking for reports of days missed because of illness and injury. Each question had answer options on a 6-point scale, with responses assigned scores from 0 to 5: 0 = no missed days; 1 = 1 d; 2 = 2 d; 3 = 3–5 d; 4 = 6–10 d; 5 = 10+ d.
FIGURE 2—
Intervention Effects Over 6 Months in an Intent-to-Treat Analysis Indicated by Adjusted Mean Changes in (a) Body Mass Index (BMI) and (b) Body Weight: Safety and Health Involvement For Truckers (SHIFT) Randomized Controlled Trial, United States, 2012–2014
Note. BMI SE = 0.14 for both intervention and control. Weight SE = 0.38 for control and 0.44 for intervention.
*P < .001.
The fruit and vegetable consumption effect size was d = 0.33, with the intervention group increasing servings per day from 2.63 to 3.02 (control group declined from 2.90 to 2.59 servings). The physical activity effect size was d = 0.34, with the intervention group increasing mean days per week with at least 30 minutes of physical activity from 1.19 to 1.90 (control group was stable with 1.39 to 1.44 days per week). Unadjusted effect sizes (unadjusted mean difference in between-group changes divided by a simple pooled baseline standard deviation) for significant outcomes were BMI d = −0.22; body weight d = −0.21; fruit and vegetable consumption d = 0.38; and physical activity d = 0.59.
Parallel “completers only” analyses and descriptive statistics were highly consistent with results of the intent-to-treat analyses. Unadjusted descriptive statistics for completers only over time are provided in Table A (available as a supplement to the online version of this article at http://www.ajph.org).
Consistent with BMI and body weight changes, we observed statistically significant between-group differences for waist circumference (d = −0.11; unadjusted d = −0.21) and percentage body fat (d = −0.23; unadjusted d = −0.28), with the intervention group showing reductions relative to increases in the control group.
Between-group differences in the remaining 12 secondary outcomes were not statistically significant. However, the trend for sleep duration is salient because it was a behavioral goal in the intervention. For intervention drivers, self-reported total sleep time increased from 7.82 to 8.04 hours (stable from 7.77 to 7.75 hours in the control group). This represents a between-group difference of about 15 minutes per night (or per day for daytime sleepers).
Process Measures
Relative to total driver employment at participating terminals (total eligible drivers were unknown) participation rates ranged from 2.6% to 10.9% across companies (unweighted mean = 7.1%; SD = 3.19%). For enrolled drivers, retention percentages at 6 months ranged from 47.4% to 80.1% across companies (unweighted mean = 61.4%; SD = 10.5%). Job turnover and job transfer were the most common reasons for attrition (Figure 1).
Of the 229 intervention drivers enrolled at baseline, 41 completed the full intervention dose (i.e., earned SHIFT Certification), 160 completed a portion of intervention activities, and 28 did not participate after orientation. On average, intervention drivers completed 1.81 (SD = 1.83) training units, 2.73 (SD = 1.52) coaching calls, and submitted 6.77 (SD = 7.33) logs. Knowledge gains measured by training pre–post tests were large (mean d = 1.95; range = 1.56–2.63). SHIFT Certified drivers who were able to report for 6-month testing (n = 34 of 41) lost an average of −5.36 kilograms (11.81 lb; −1.61 BMI), which was about twice the adjusted mean weight loss of the intervention group as a whole.
DISCUSSION
The intervention produced statistically significant weight loss among commercial truck drivers. Behavior changes that potentially impacted energy balance and weight loss included significant increases in exercise and fruit and vegetable consumption. The magnitude of the effect on BMI is medically and economically meaningful. A 1-unit BMI reduction would predict decreased risk of a range of long-term health problems. For example, among men in a 7-year longitudinal study, each unit increase in BMI at follow-up was associated with a 1.19 odds ratio for becoming hypertensive.29 Even smaller weight changes may have an impact on diabetes risk. In a longitudinal study of participants in a diabetes prevention program, each kilogram of weight loss reduced diabetes risk by 16%.30 Economically, a sustained reduction of 1 unit of BMI would produce an estimated annual savings of $200 in health care costs for employers.31 Even in traditional workplaces, where employees report to the same worksite and see each other every day, body weight management interventions can and do fail.32 Thus, in the extremely challenging commercial trucking context, any effective body weight intervention is a notable achievement.
The intervention effect observed is within range or exceeds effects reported in the general workplace obesity intervention literature. The between-groups difference in weight change of –3.31 kilograms (7.29 lb) exceeds the median effect of −2.95 kilograms (–6.50 lb) for workplace weight-loss competitions with incentives reported in a previous meta-analysis.33 The effect size for BMI (d = −0.13; unadjusted d = −0.24) is within the range of effects reported in a meta-analysis of 46 lifestyle interventions to prevent obesity among occupational, community, and patient populations (BMI mean effect d = 0.06; range = −0.09 to 0.45; negative reflects a change in the unexpected direction).34 Another relevant contrast is with the previous randomized controlled trial of a lifestyle counseling intervention with Scandinavian truck and bus drivers.15 Our observed between-group difference was −3.31 kilograms over 6 months compared with −4.00 kilograms observed over 12 months.15
Study strengths support the robust and important nature of findings. Methodological strengths include the cluster-randomized design with an intent-to-treat analysis, objective body measurements, and the use of validated or established scales for behavioral outcomes. We also employed methods to minimize bias and maximize data quality. Retention efforts were rigorous, and resulted in retention of just over 60% of the original sample at 6 months in a population with annual job turnover rates that often exceed 100%. Furthermore, within the trial, the intervention proved to be scalable and repeatable, as it was implemented at 5 companies (11 intervention terminals) with similar results at each site. Trial effects were also similar to those produced in the earlier pilot study.8
Limitations and Future Directions
Study limitations suggest areas for future investigation. The intervention was evaluated as a multicomponent package, which means future process evaluation studies or factorial designs are needed to elucidate contributions of individual components. Findings also represent immediate postintervention effects. Longitudinal follow-up analyses are needed to assess the durability of effects over time and to compare body-weight changes during a no-intervention follow-up period to comparable studies with other populations.
The brief dietary screeners employed in the study are valid and widely used, but are not in-depth food-frequency questionnaires and did not address portion sizes. The current analyses also lacked objective indicators of self-reported behavior changes (e.g., actigraphy analyses, biomarkers of dietary changes). Although we observed favorable trends in secondary outcomes (e.g., 15-minute increase in daily sleep time among intervention participants relative to control), physical outcomes that are regulated in the trucking industry, such as hypertension, did not change significantly. Prevalent pharmacological control of health conditions such as hypertension may have limited our ability to detect effects, but it is also possible that greater or longer-sustained weight loss is needed.
To specify or enhance impacts on lagging physical indicators of health behavior changes, further research is needed to investigate whether intervention effects on physical outcomes were moderated by certain driver characteristics or behaviors (e.g., baseline demographics, intervention participation, degree of weight loss). Further longitudinal intervention research is also encouraged to support weight-loss maintenance or further weight loss to maximize health and safety benefits for drivers, companies, and the general public.
Successful interventions with truck drivers are important and rare, but even larger effects may be feasible. For example, Brownell et al.16 reported a mean effect of −5.5 kilograms across 3 weight-loss competitions (12–15 weeks in duration) with banking and manufacturing employees. However, the dispersed nature of trucking may weaken some potent dimensions of social competitions. Only about 18% of drivers in the current trial experienced the intended full intervention dose. As higher intervention participation was associated with larger effects, future experimentation to increase engagement is encouraged, and could include increased gamification of the logging process (e.g., additional virtual trophies or badges for achievements, point systems, time constraints, levels or intermediate objectives, stories or themes), altering training dimensions (segmentation, spacing, content), or adjusting incentive dependencies and amounts. Adding organizational or systems intervention components may also enhance health outcomes, such as changes to supervision and route assignments, work hours, or improvements to truck cabs to support healthy sleep, eating, or exercise.
Conclusions
Our findings support the efficacy of competition-based weight-loss programs in the trucking industry that involve participatory moderate goal setting along with tailored and evidence-based self-monitoring, training, and coaching. The use of mobile-friendly technologies facilitated the scalability and repeatability of the program. Because of the interactions between sleep deficiency and appetitive and metabolic processes,21 and the impact of poor health and sleep problems on crash risk in trucking, future research and practice related to driver body-weight management should pay integrated attention to sleep, dietary, and exercise behaviors. Finally, to address the full scope and magnitude of the public health problem, driver-level interventions should be complemented with research and innovation at other sociotechnical levels that have an impact on driver health, such as experimentation with operational systems, environmental and equipment engineering, and job design.
ACKNOWLEDGMENTS
The research was supported with a grant from the National Heart, Lung, and Blood Institute (R01HL1054950).
We would like to acknowledge expert motivational interviewing providers Denise Ernst, Laura Blue, Carol Defrancesco, and Sharon Thompson. Research assistants and student workers, who invested much time and effort meeting with drivers across the country and preparing data for analyses, included Emma Robson, Kevin Bransford, Sydney Running, Luke Puerini, Andrew Kirk, Elliot Hohn, Louis Moore, Kristy Luther Rhoten, Kelly Tilmanis, Annie Cannon, and Rossmary Vasquez. We thank Ginger Hanson and Ana Gabriela Rosales for statistical services under the supervision of author Nancy Perrin, and Kelsey Parker for assistance with article formatting for submission. Glorian Sorensen, PhD, MPH, and Victor Stevens, PhD, each provided valuable early stage consultation on the project. We thank our corporate partners for their long-time support and operational assistance accommodating drivers who wanted to participate. Finally, we are most grateful to our driver participants who volunteered and spent precious time for the benefit of their own health, but also in service of the many future drivers who may benefit from the knowledge produced by the research.
This study is registered as a clinical trial (NCT02105571): https://clinicaltrials.gov/ct2/show/NCT02105571?term=SHIFT+truck&rank=1.
Note: Oregon Health & Science University and W. K. Anger have a significant financial interest in Northwest Education Training and Assessment, a company that may have a commercial interest in the results of this research and technology. This potential conflict was reviewed and managed by OHSU Conflict of Interest in Research Committee.
HUMAN PARTICIPANT PROTECTION
The study protocol was reviewed and approved by the human participants institutional review board at OHSU.
REFERENCES
- 1.American Trucking Associations. Reports, trends, and statistics. 2015. Available at: http://www.trucking.org/News_and_Information_Reports.aspx. Accessed October 18, 2015.
- 2.Sieber WK, Robinson CF, Birdsey J et al. Obesity and other risk factors: the national survey of U.S. long-haul truck driver health and injury. Am J Ind Med. 2014;57(6):615–626. doi: 10.1002/ajim.22293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Janson C, Lindberg E, Gislason T, Elmasry A, Boman G. Insomnia in men: a 10-year prospective population based study. Sleep. 2001;24(4):425–430. doi: 10.1093/sleep/24.4.425. [DOI] [PubMed] [Google Scholar]
- 4.Anderson JE, Govada M, Steffen TK et al. Obesity is associated with the future risk of heavy truck crashes among newly recruited commercial drivers. Accid Anal Prev. 2012;49:378–384. doi: 10.1016/j.aap.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Tregear S, Reston J, Schoelles K, Phillips B. Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med. 2009;5(6):573–581. [PMC free article] [PubMed] [Google Scholar]
- 6.Moonesinghe R, Longthorne A, Shankar U, Singh S, Subramanian R, Tessmer J. An analysis of fatal large truck crashes. Washington, DC: National Highway Traffic and Safety Administration, National Center for Statistics and Analysis; 2003: 1–44. Publication no. HS-809 569.
- 7.Krueger GP, Brewster RM, Dick V, Inderbitzen RE, Staplin L. Commercial Truck and Bus Safety Synthesis Program: Synthesis 15: Health and Wellness Programs for Commercial Drivers. Washington, DC: Transportation Research Board; 2007. pp. 1–80. [Google Scholar]
- 8.Olson R, Anger KW, Elliot DL, Wipfli B, Gray M. A new health promotion model for lone workers: results of the SHIFT pilot study (Safety & Health Involvement for Truckers) J Occup Environ Med. 2009;51(11):1233–1246. doi: 10.1097/JOM.0b013e3181c1dc7a. [DOI] [PubMed] [Google Scholar]
- 9.Wipfli B, Olson R, Koren M. Weight-loss maintenance among SHIFT pilot study participants 30-months after intervention. J Occup Environ Med. 2013;55(1):1–3. doi: 10.1097/JOM.0b013e31827db848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thiese MS, Effiong A, Ott U et al. A clinical trial on weight loss among truck drivers. Int J Occup Environ Med. 2015;6(2):104–112. doi: 10.15171/ijoem.2015.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sorensen G, Stoddard A, Quintiliani L et al. Tobacco use cessation and weight management among motor freight workers: results of the Gear Up for Health Study. Cancer Causes Control. 2010;21(12):2113–2122. doi: 10.1007/s10552-010-9630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes SM, Power ML, Walter CK. A motor carrier wellness program: development and testing. Transp J. 1996;35(3):33–48. [Google Scholar]
- 13.Hedberg GE, Wikström-Frisén L, Janlert U. Comparison between two programmes for reducing the levels of risk indicators of heart diseases among male professional drivers. Occup Environ Med. 1998;55(8):554–561. doi: 10.1136/oem.55.8.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong CK, Fung CS, Siu S et al. A short message service (SMS) intervention to prevent diabetes in Chinese professional drivers with pre-diabetes: a pilot single-blinded randomized controlled trial. Diabetes Res Clin Pract. 2013;102(3):158–166. doi: 10.1016/j.diabres.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Puhkala J, Kukkonen-Harjula K, Mansikkamaki K et al. Lifestyle counseling to reduce body weight and cardiometabolic risk factors among truck and bus drivers—a randomized controlled trial. Scand J Work Environ Health. 2015;41(1):54–64. doi: 10.5271/sjweh.3463. [DOI] [PubMed] [Google Scholar]
- 16.Brownell KD, Cohen RY, Stunkard AJ, Felix MR, Cooley NB. Weight loss competitions at the work site: impact on weight, morale and cost-effectiveness. Am J Public Health. 1984;74(11):1283–1285. doi: 10.2105/ajph.74.11.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eckerman DA, Lundeen CA, Steele A, Fercho HL, Ammerman TA, Anger WK. Interactive training versus reading to teach respiratory protection. J Occup Health Psychol. 2002;7(4):313–323. [PubMed] [Google Scholar]
- 18.Olson R, Winchester J. Behavioral self-monitoring of safety and productivity in the workplace: a methodological primer and quantitative literature review. J Organ Behav Manag. 2008;28:9–75. [Google Scholar]
- 19.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol. 2003;71(5):843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- 20.Schill AL, Chosewood LC. The NIOSH total worker HealthTM program: an overview. J Occup Environ Med. 2013;55(12) suppl:S8–S11. doi: 10.1097/JOM.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 21.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bunn TL, Slavova S, Struttmann T, Browning SR. Sleepiness/fatigue and distraction/inattention as factors for fatal versus nonfatal commercial motor vehicle driver injuries. Accid Anal Prev. 2005;37(5):862–869. doi: 10.1016/j.aap.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 23.Wiegand DM, Hanowski RJ, McDonald SE. Commercial drivers’ health: a naturalistic study of body mass index, fatigue, and involvement in safety-critical events. Traffic Inj Prev. 2009;10(6):573–579. doi: 10.1080/15389580903295277. [DOI] [PubMed] [Google Scholar]
- 24.Thompson FE, Subar AF, Smith AF et al. Fruit and vegetable assessment: performance of 2 new short instruments and a food frequency questionnaire. J Am Diet Assoc. 2002;102(12):1764–1772. doi: 10.1016/s0002-8223(02)90379-2. [DOI] [PubMed] [Google Scholar]
- 25.Thompson FE, Kipnis V, Subar AF et al. Performance of a short instrument to estimate usual dietary intake of percent calories from fat. Eur J Clin Nutr. 1998;52(suppl 2):S63. [Google Scholar]
- 26.Buxton OM, Quintiliani LM, Yang MH et al. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. Am J Public Health. 2009;99(suppl 3):S636–S643. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elliot DL, Goldberg L, Kuehl KS, Moe EL, Breger RKR, Pickering MA. The PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007;49(2):204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 28.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index (PSQI): a new instrument for psychiatric research and practice. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 29.Williams PT. Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity (Silver Spring) 2008;16(11):2541–2548. doi: 10.1038/oby.2008.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamman RF, Wing RR, Edelstein SL et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29(9):2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang F, McDonald T, Bender J, Reffitt B, Miller A, Edington DW. Association of healthcare costs with per unit body mass index increase. J Occup Environ Med. 2006;48(7):668–674. doi: 10.1097/01.jom.0000225045.77734.f4. [DOI] [PubMed] [Google Scholar]
- 32.Williams AE, Stevens VJ, Albright CL, Nigg CR, Meenan RT, Vogt TM. The results of a 2-year randomized trial of a worksite weight management intervention. Am J Health Promot. 2014;28(5):336–339. doi: 10.4278/ajhp.100127-ARB-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Archer WR, Batan MC, Buchanan LR et al. Promising practices for the prevention and control of obesity in the worksite. Am J Health Promot. 2011;25(3):e12–e26. doi: 10.4278/ajhp.090421-QUAN-144. [DOI] [PubMed] [Google Scholar]
- 34.Kremers S, Reubsaet A, Martens M et al. Systematic prevention of overweight and obesity in adults: a qualitative and quantitative literature analysis. Obes Rev. 2010;11(5):371–379. doi: 10.1111/j.1467-789X.2009.00598.x. [DOI] [PubMed] [Google Scholar]