Abstract
Aims and Objectives:
India has an assortment of tribal population living in isolated pockets, and the Santhals are numerically predominant in Jharkhand. This study was aimed at assessing the oral health status and treatment needs of Santhals residing in Dhanbad, Jharkhand.
Materials and Methods:
A cross-sectional survey of 921 Santhals of Topchanchi Block was conducted. A modified World Health Organization (WHO) Oral Health Assessment Form (1997) was utilized and examined according to the WHO methodology (1997). The recorded data was statistically analyzed using the Statistical Package for the Social Sciences version 15.
Results:
Based on the occupation, it was seen that 620 (67.3%) participants practiced agriculture and 206 (22.4%) worked as laborers. The mean decayed missing filled tooth (score was 3.56 ± 1.93 in 2–5-year-old participants. In the higher age groups of 35–44 and 65–74 years, the scores were 5.21 ± 2.34 and 7.42 ± 4.29, respectively. Participants with bleeding gums were predominantly seen in the age group of 35–44 years (0.91 ± 0.08). Approximately 138 (54.1%) participants had a loss of attachment of 4–5 mm in the 35–44 year age group. In the 13–15-year-old age group, 0.14 ± 0.05 teeth needed two surfaces fillings. A total of 118 (12.8%) participants needed one-unit prosthesis in the upper jaw.
Conclusion:
This study showed that a majority of Santhal tribals used twigs to routinely clean their teeth. Poor oral hygiene and periodontal status was seen among the tribes.
Key words: Oral health, treatment needs, tribal people
INTRODUCTION
Oral health is an essential and vital component of overall health and is much more than just healthy teeth. Despite adequate advancements in global oral health, problems still persist in many communities around the world, particularly among the underprivileged.[1,2] Dental disease, especially dental caries, is a disease of ancient times. However, the dietary changes in the 18th century, primarily, increased refinement of foods, lifestyle, and the greater availability of sugar, was found to be responsible for the modern pattern of dental caries.[3] Periodontal disease is the most prevalent dental disease affecting the adult population throughout the world, varying only in degree from mild to severe depending on a host of factors. The prevalence of periodontitis is found to be considerably higher in developing countries.[4]
Numerous studies have been conducted across the world on the tribal populace, and in reference to oral health, to name a few, the Paniya tribes of Wayanad[5] and Kalpetta,[6] Kerala, the Santal tribals of West Bengal,[7] the tribals of the Eastern Ghats,[8] the Orao tribals in Rangpur District, Bangladesh,[9] and the Xukuru ethnic group of Pesqueira, Brazil.[10] The Santhals are predominant in Jharkhand State in Santhal Paragana, Singhbhum, Dhanbad, Hazaribagh, Giridih, and Ranchi Districts.
MATERIALS AND METHODS
Study population
The study population consisted of tribals of “Santhal” origin in the Topchanchi Block of Dhanbad District, Jharkhand. The study was carried out in villages of Dhangi (Dhangi Panchayat; 2274 participants), and Telodih (Singhdaha Panchayath; 334 participants) on 863 (37.95%) and 78 (23.35%) Santhals, respectively.
Study design
A cross-sectional household survey of Santhals in the villages of Dhangi and Telodih was conducted in the months of July to September 2009.
Sampling design
A multi-stage random sampling procedure was used for the sample selection. One out of 9 Blocks in Dhanbad District was randomly selected (Topchanchi Block with 28 Panchayats). Further, Dhangi and Singhdaha Panchayats were randomly selected, with five and four villages, respectively, and further, one village each was selected. The sample size was calculated using the formula: n = z2 pq/d2, where n is sample size, P prevalence of disease, q free from disease, d allowable error, and z is point on the normal deviation. Upon calculating, n was found to be 897. However, all the tribals were included in the study and the sample size thus arrived at was 921 participants.
Official permission and ethical clearance
The ethical clearance was obtained from the Ethical Committee at Rama Dental College Hospital and Research Centre (RDCH and RC), Kanpur. The permission to conduct the study was obtained from the Department of Health, Medical Education and Family Welfare, Government of Jharkhand, Ranchi.
Informed consent
A written informed consent was obtained from all the subjects who were willing to participate in the study.
Survey proforma
A modified World Health Organization (WHO) Oral Health Assessment Form (1997) was utilized to record the information related to oral health. In this proforma, oral hygiene practice, dietary habits, and the deleterious habits of alcohol consumption and tobacco chewing were also recorded.
Training and calibration
A single examiner was trained and calibrated in the Department of Public Health Dentistry, RDCH and RC, Kanpur to prevent any diagnostic variability among the study participants. The investigator himself conducted all the clinical examinations with the help of recording assistants.
Data collection
The oral health examination of participants was conducted according to the WHO methodology, using the Community Periodontal Index (CPI) probe and a plane mouth mirror. A Type III clinical examination was carried out under adequate natural light. All the participants who were present on the day of examination were included in the study.
Statistical analysis
The recorded data were compiled and entered into a spreadsheet computer program (Microsoft Excel 2007) and analyzed using the Statistical Package for the Social Sciences version 15 (SPSS Inc., Chicago, Illinois, USA). The descriptive statistics included computation of percentages, means, and standard deviation. The statistical tests applied for the analysis were student's t-test and one way analysis of variance. For all the statistical tests, the confidence level and the level of significance were set at 95% and 5%, respectively.
RESULTS
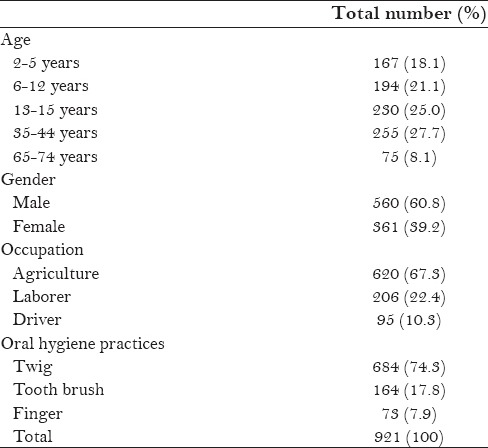
A total of 921 participants were examined in the study. Among them, 560 were males and 361 were females with age ranging from 2–74 years. Based on the occupation, it was seen that 620 (67.3%) participants practiced agriculture and 206 (22.4%) worked as laborers. A total of 684 (74.3%) and 164 (17.8%) participants were using a twig and a toothbrush to clean their teeth, respectively [Table 1].
Table 1.
Characteristics of the study group
When examined for oral mucosal lesions, it was found that 784 (85.1%) participants were quite healthy and had no abnormal conditions. Approximately 25 (2.7%) subjects had leukoplakia, 48 (5.2%) suffered from ulceration, and 51 (5.5%) had abscesses [Figure 1].
Figure 1.
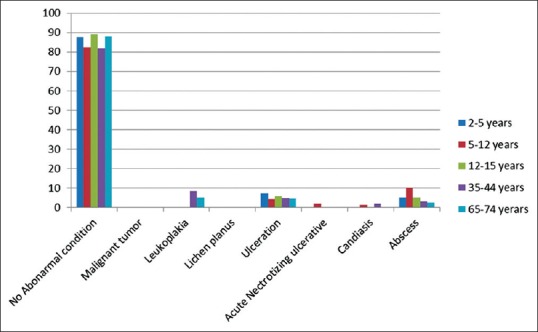
Distribution oral mucosal lesions in the study group
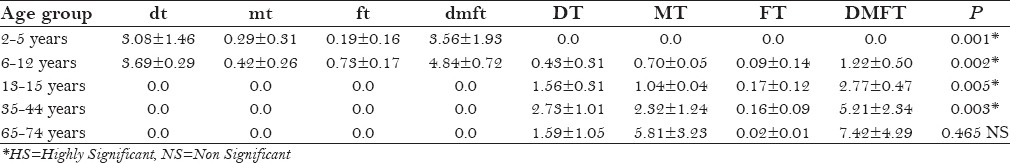
The mean decayed, missing, and filled tooth (DMFT) score was 3.56 ± 1.93 in 2–5-year-old participants, and in the higher age groups of 35–44 years and 65–74 years, the scores were 5.21 ± 2.34 and 7.42 ± 4.29 teeth, respectively. A statistically significant association was found between the various age groups, except for the 65–74 age group [Table 2].
Table 2.
Distribution of mean DMFT scores across the age groups
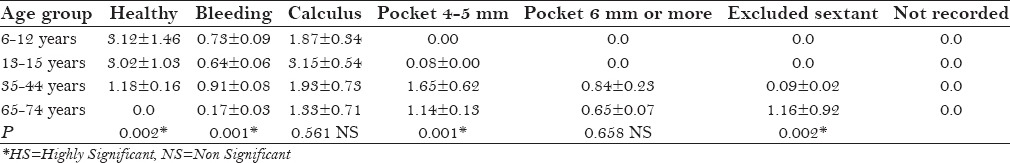
The mean number of sextants with periodontal disease conditions, as scored by CPI, is shown in Table 3. Participants with bleeding gums were predominantly seen in the age group of 35–44 years (0.91 ± 0.08). The participants with shallow pockets were more commonly seen in the age group of 35–44 years (1.65 ± 0.62). Statistically highly significant differences were observed across all the age groups (P < 0.001).
Table 3.
Mean number of sextants as scored by CPI across the age groups
When the study group was examined for the periodontal loss of attachment (LOA), it was found that 205 (89.1%) participants in the 13–15 year age group had an LOA 0–3 mm. A total of 25 (9.8%) and 9 (12%) participants had an LOA of 6–8 mm in the age groups of 35–74 and65–74 years, respectively [Figure 2].
Figure 2.
Prevalence of loss attachment across the age groups
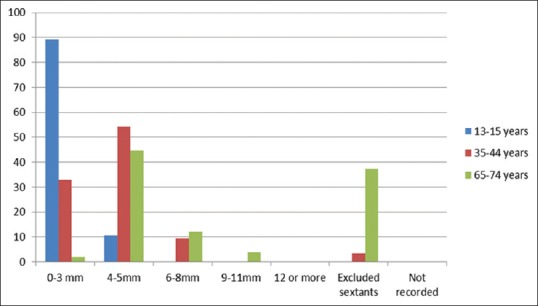
Table 4 depicts the distribution of the study group according to the treatment needs. In the 2–5-year-old age group, 1.23 ± 0.64 teeth needed one surface filling and 0.17 ± 0.06 teeth needed crowns for different reasons. In the 13–15 year age group, 0.72 ± 0.39 teeth needed one surface filling and 0.14 ± 0.05 teeth needed two surfaces fillings. The highest need for “other care” was found in the 35–44 year age group with a mean of 4.47 ± 1.24 teeth.
Table 4.
Distribution of the study group according to treatment needs
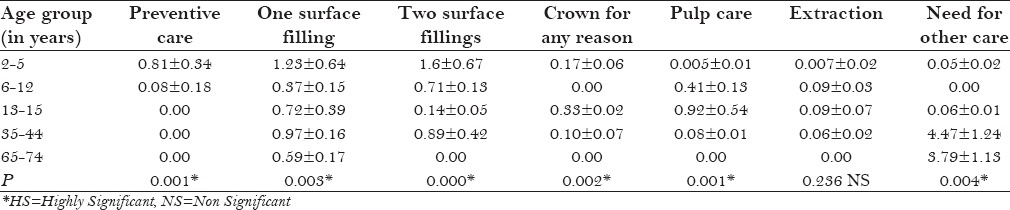
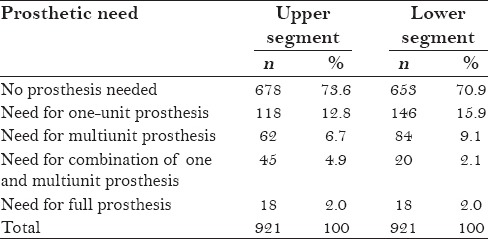
Table 5 shows the distribution of the study participants according to the prosthetic need. A total of 118 (12.8%) participants needed one-unit prosthesis in the upper jaw. There were 18 (2.0%) participants each, requiring full prosthesis in both the jaws.
Table 5.
Distribution of the study participants according to the prosthetic need
DISCUSSION
The tribal people are often characterized by their own language, heritage, love for freedom, and self-identity, and this holds true for the Santhals too. A systematic review of the studies pertaining to the tribal population is scarce and no comprehensive data is available; this study would add to the existing knowledge about these native people.
The present study was carried out on Santhals residing in the Topchanchi Block of Dhanbad District, Jharkhand. The sample size was 921 participants divided into five age groups, that is, 2–5, 6–12, 13–15, 35–44, and 65–74 years. The present study evidently showed that a majority (74.2%) of Santhali tribals routinely used twigs of sakhua trees (Shorearobusta) to clean their mouth. The results of the present study are in agreement with the studies conducted by Mandal et al.,[7] Vaish et al.,[11] Bhowate et al.,[12] Varenne et al.,[13] Abdul-Kadir Yassin,[14] Vaish,[15] and John et al.[16]
Bhowate et al.[12] in their study found a lower use of the toothpaste and tooth brush in comparison to other materials used for cleaning the teeth. Vaish et al.[15] in their study found that all the Kandha tribals used datum twigs to clean their teeth. Ikeda et al.[17] in their study found a total of 71 oral mucosal lesions among 64 (4.9%) study participants. Leukoplakia was found in 1.1% and candidiasis in 1.4% of the study participants. These findings are in accordance with the findings of the present study.
The present study showed that a majority of the Santhals suffered from various forms of periodontal disease. This finding was comparable to the findings of the study carried out by Peterson and Razanamihaja[18] on Malagasy tribes in Madagascar. The traditional habit of chewing betel quid in the region might be a factor for the abundance of periodontal disease in the study group. Dental calculus was most commonly seen in all the age groups. The findings of the present study are in accordance with the findings of the study conducted by Varenne et al.[13] and Naheeda et al.[19]
The mean number of sextants in the age groups of 13–15 years and above affected by bleeding gums were 0.64, 0.91, and 0.17 sextants, respectively. Similarly, the mean number of sextants affected by dental calculus was 3.15, 1.93, and 1.33 sextants, respectively. Deep pockets (6 mm or more) were seen only in the 35–44 year (0.84) and 65–74 year (0.65) age groups, and this was in agreement with the findings of the study conducted by Kumar et al.[20] and Singh et al.[21] In the study by Kumar et al.[22] among age groups 35–44 and 45–54 years, it was found that the mean number of sextants with dental calculus were 1.71 and 0.47 sextants, respectively. Similarly, the scores for shallow pockets were 1.84 and 1.27 sextants, respectively. These findings are similar to the findings of the present study.
Spalj and Plancak[23] in their study among individuals aged 15 years and older found that the mean number of healthy sextants varied from 3–5 and the mean number of sextants with bleeding gums or dental calculus varied from 1–3. These findings are in accordance with the findings of the present study.
Schamschula et al.[24] in their study observed that the mean scores for periodontal involvement increased from 1.7 sextants at 20 years to 4.8 sextants at 43 years and above. These findings were not in conformity with the findings of the present study. It was interesting to note that the tribals' relegation of oral health to general health might have contributed to the existing burden of periodontal disease. To combat such a situation, education and motivation of the laity is required to improve their oral health. Efforts directed in curtailing them from the harmful habits of alcohol consumption, smoking, pan chewing, and the use of smokeless tobacco would go a long way in ensuring good oral health for these masses.
In the present study, high dental caries prevalence was seen among the study participants, and this finding is consistent with the study findings conducted by Maurya et al.[25] and Lang et al.,[26] where the mean DMFT scores were quite high. However, this was in disagreement with the study findings of Jayashantha and Johnson.[27]
Vaish[11] in his study demonstrated that the caries prevalence in the 6–10 year age group was 32% followed by 24% in the age group of 11–15 years. The findings were in agreement with the findings of the present study. Schamschula et al.[24] showed that the prevalence of dental caries increased from 17.1 teeth at 20 years to 20.7 teeth at 35 years. These finding were in conformity with the findings of the present study. It might be hypothesized that the increase in caries prevalence might be due to the ill effects of lifestyle due to increased access to cariogenic foods and beverages.
Jalili et al.[28] conducted a study on tribal children aged 6–13 years, living in the villages of Mandu in Dhar District, Madhya Pradesh, and showed that nearly 30% of the children needed some sort of conservative care. These findings are similar to the findings of the present study.
Naidu et al.[29] conducted a study of children aged 6–8, 12, and 15 years and found that 77% of the children had a need for some form of treatment, and the most frequently occurring need was for dental fillings. These findings are similar to the findings of the present study. This might be because of the fact that dental treatment is usually expensive and remains inaccessible to most of the tribal people. In addition, the remoteness of these tribal clusters from the nearest care provider adds to the difficulty in seeking regular dental care.
The main limitation of this study is that it is a cross-sectional study and the findings cannot be extrapolated to the other development blocks in the District because of the vast differences in the sociodemographic factors. However, this limitation can be overcome by a larger sample size drawn from across the District and undertaking studies of a longitudinal nature.
The results of this study could form a baseline data for the health administrators for planning suitable programs for the betterment of oral health among the tribals in the District of Dhanbad, as well as across the State of Jharkhand.
CONCLUSION
The present study was conducted to assess the oral health status and treatment needs of Santhali tribals residing in Dhanbad District, Jharkhand. The study showed that a majority (74.2%) of Santhals used twigs of sakhua tree to routinely clean their teeth. There was a lower use of the toothpaste and tooth brush in comparison to other materials used for cleaning the teeth. In the present study, high dental caries and periodontal disease prevalence was seen among the study participants. A state-wide study would be required to obtain a realistic picture of the oral health status and treatment needs of the Santhals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Petersen PE. Improvement of oral health in Africa in the 21st century – The role of the WHO Global Oral Health Programme. Develop Dentistry. 2004;5:9–20. [Google Scholar]
- 2.Yadav P, Kaur B, Srivastava R, Srivastava S. Oral health disparities: Review. J Dent Med Sci. 2014;13:69–72. [Google Scholar]
- 3.Kshatriya G. Changing perspectives of tribal health in the context of increasing lifestyle diseases in India. J Environ Soc Sci. 2014;1:1–7. [Google Scholar]
- 4.Baelum V, Fejerskov O, Manji F. Periodontal diseases in adult Kenyans. J Clin Periodontol. 1988;15:445–52. doi: 10.1111/j.1600-051x.1988.tb01599.x. [DOI] [PubMed] [Google Scholar]
- 5.Deepan Kumar CV, Mohamed S, Janakiram C, Joseph J. Validation of dental impact on daily living questionnaire among tribal population of India. Contemp Clin Dent. 2015;6:S235–41. doi: 10.4103/0976-237X.166841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janakiram C, Joseph J, Vasudevan S, Taha F, Deepan Kumar CV, Venkitachalam R, et al. Prevalence and dependency of tobacco use in an indigenous population of Kerala, India. J Oral Hyg Health. 2016;4:198. [Google Scholar]
- 7.Mandal S, Ghosh C, Sarkar S, Pal J, Kar S, Bazmi BA. Assessment of oral health status ofSantal (tribal) children of West Bengal. J Indian Soc Pedod Prev Dent. 2015;33:44–7. doi: 10.4103/0970-4388.148976. [DOI] [PubMed] [Google Scholar]
- 8.Raju PK, Vasanti D, Kumar JR, Niranjini K, Kumar MS. Oral hygiene levels in children of tribal population of Eastern Ghats: An epidemiological study. J Int Oral Health. 2015;7:108–10. [PMC free article] [PubMed] [Google Scholar]
- 9.Ahmad MS, Al-Mamun MA, Begum S, Islam MS, Habib MA, Rahman MM. Knowledge and practice about oral hygiene by tribal people (Orao) in Rangpur Region, Bangladesh. Int J Dent Med. 2015;1:28–32. [Google Scholar]
- 10.Gonçalves ÉM, Cavalcanti LC, Firmino RT, Ribeiro GL, Granville-Garcia AF, Menezes VA. Dental caries experience among indigenous children and adolescents. J Oral Sci. 2015;57:123–9. doi: 10.2334/josnusd.57.123. [DOI] [PubMed] [Google Scholar]
- 11.Vaish RP. Prevalence of caries among school-going tribal children in Ganjam district in Orissa. J Indian Dent Assoc. 1982;54:375–7. [PubMed] [Google Scholar]
- 12.Bhowate RR, Borle SR, Chinchkhede DH, Gondhalekar RV. Dental health amongst 11-15-year-old children in Sevagram, Maharashtra. Indian J Dent Res. 1994;5:65–8. [PubMed] [Google Scholar]
- 13.Varenne B, Petersen PE, Ouattara S. Oral health status of children and adults in urban and rural areas of Burkina Faso, Africa. Int Dent J. 2004;54:83–9. doi: 10.1111/j.1875-595x.2004.tb00260.x. [DOI] [PubMed] [Google Scholar]
- 14.Abdul-Kadir R, Yassin AT. Periodontal status (CPITN) of six- to fifteen-year-old West Malaysian Aborigines (Proto-Malays) J Nihon Univ Sch Dent. 1989;31:612–8. doi: 10.2334/josnusd1959.31.612. [DOI] [PubMed] [Google Scholar]
- 15.Vaish RP. Prevalence of caries among school children in Phulbani district, Orissa. J Indian Dent Assoc. 1983;55:455–7. [PubMed] [Google Scholar]
- 16.John JB, Asokan S, Aswanth KP, Priya PG, Shanmugaavel AK. Dental caries and the associated factors influencing it in tribal, suburban and urban school children of Tamil Nadu, India: A cross sectional study. J Public Health Res. 2015;4:23–8. doi: 10.4081/jphr.2015.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ikeda N, Handa Y, Khim SP, Durward C, Axéll T, Mizuno T, et al. Prevalence study of oral mucosal lesions in a selected Cambodian population. Community Dent Oral Epidemiol. 1995;23:49–54. doi: 10.1111/j.1600-0528.1995.tb00197.x. [DOI] [PubMed] [Google Scholar]
- 18.Peterson PE, Razanamihaja N. Oral health status of children and adults in Madagascar. Indian Dent J. 1996;46:41–7. [PubMed] [Google Scholar]
- 19.Naheeda, Asif SM, Padma M, Paul A. Assessment of Periodontal Status of Konda Reddy Tribe in Bhadrachalam, Khammam District, India. J Clin Diagn Res. 2015;9:23–5. doi: 10.7860/JCDR/2015/13430.6051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kumar V, Agarwal V, Khatri M, Singh G, Sunny Prevalence of periodontitis in rural and urban population. Indian J Comm Health. 2015;27:366–71. [Google Scholar]
- 21.Singh K, Bhandari SB, Anandani C, Pani P, Kansal S, Chaudhary H. Prevalence of periodontal diseases and oral hygiene practices among drug addicted inmates. Oral Health Dent Manag. 2014;13:911–4. [Google Scholar]
- 22.Kumar TS, Dagli RJ, Mathur A, Jain M, Balasubramanyam G, Prabu D, et al. Oral health status and practices of dentate Bhil Adult tribes of southern Rajasthan, India. Int Dent J. 2009;59:133–40. [PubMed] [Google Scholar]
- 23.Spalj S, Plancak D. Comparison of periodontal health of two different rural population types in Croatia. ActaStomatol Croat. 2000;34:183–7. [Google Scholar]
- 24.Schamschula RG, Cooper MH, Wright MC, Agus HM, Un PS. Oral health of adolescent and adult Australian Aborigines. Community Dent Oral Epidemiol. 1980;8:370–4. doi: 10.1111/j.1600-0528.1980.tb01310.x. [DOI] [PubMed] [Google Scholar]
- 25.Maurya R, Kundu D, Singh H, Mishra H. Oral health status, dental caries experience and treatment needs of population of Jammu city. Int J Oral Health Dent. 2015;1:164–7. [Google Scholar]
- 26.Lang WP, Hamard MA, Mackenzie RC. Rural dental program in Haiti. Community Dent Oral Epidemiol. 1984;12:233–6. doi: 10.1111/j.1600-0528.1984.tb01446.x. [DOI] [PubMed] [Google Scholar]
- 27.Jayashantha P, Johnson NW. Oral Health Status of the Veddas – Sri Lankan Indigenous People. J Health Care Poor Underserved. 2016;27:139–47. doi: 10.1353/hpu.2016.0039. [DOI] [PubMed] [Google Scholar]
- 28.Jalili VP, Sidhu SS, Kharbanda OP. Status of dental caries and treatment needs in tribal children of Mandu (Central India) J Pierre Fauchard Acad. 1993;7:7–15. [PubMed] [Google Scholar]
- 29.Naidu R, Prevatt I, Simeon D. The oral health and treatment needs of schoolchildren in Trinidad and Tobago: Findings of a national survey. Int J Paediatr Dent. 2006;16:412–8. doi: 10.1111/j.1365-263X.2006.00755.x. [DOI] [PubMed] [Google Scholar]


