Abstract
Purpose
Adoptive cell transfer, the infusion of large numbers of activated autologous lymphocytes, can mediate objective tumor regression in a majority of patients with metastatic melanoma (52 of 93; 56%). Addition and intensification of total body irradiation (TBI) to the preparative lymphodepleting chemotherapy regimen in sequential trials improved objective partial and complete response (CR) rates. Here, we evaluated the importance of adding TBI to the adoptive transfer of tumor-infiltrating lymphocytes (TIL) in a randomized fashion.
Patients and Methods
A total of 101 patients with metastatic melanoma, including 76 patients with M1c disease, were randomly assigned to receive nonmyeloablative chemotherapy with or without 1,200 cGy TBI before transfer of tumor-infiltrating lymphcytes. Primary end points were CR rate (as defined by Response Evaluation Criteria in Solid Tumors v1.0) and overall survival (OS). Clinical and laboratory data were analyzed for correlates of response.
Results
CR rates were 24% in both groups (12 of 50 v 12 of 51), and OS was also similar (median OS, 38.2 v 36.6 months; hazard ratio, 1.11; 95% CI, 0.65 to 1.91; P = .71). Thrombotic microangiopathy was an adverse event unique to the TBI arm and occurred in 13 of 48 treated patients. With a median potential follow-up of 40.9 months, only one of 24 patients who achieved a CR recurred.
Conclusion
Adoptive cell transfer can mediate durable complete regressions in 24% of patients with metastatic melanoma, with median survival > 3 years. Results were similar using chemotherapy preparative regimens with or without addition of TBI.
INTRODUCTION
During the past 20 years, estimated 5-year survival rates for patients with metastatic melanoma have remained relatively constant at 14% to 16%.1,2 Until the recent development of checkpoint modulators, interleukin-2 (IL-2; a nonspecific stimulator of immune effector cells) was the only US Food and Drug Administration–approved agent capable of inducing objective cancer responses (13%), including durable complete regression (4%).3 The mechanism of that regression, although not fully understood, likely relied on the presence of immune cells in the peritumoral environment. The strategy of adoptive cell transfer (ACT) was developed to take advantage of three methodologic advances: the ability to generate large numbers of tumor-reactive tumor-infiltrating lymphocytes (TIL), to activate cells ex vivo, and to prepare the patient's immune milieu before an influx of effector cells.4-6 ACT, in a tripartite regimen that included lymphodepleting chemotherapy, cell administration, and high-dose IL-2 proved to be capable of mediating durable tumor regression in patients at multiple institutions at rates greater than that of IL-2 alone.7-10 Building on murine data, sequential clinical studies of ACT of TIL performed in the Surgery Branch (National Cancer Institute, National Institutes of Health) suggested that adding total body irradiation (TBI) to the nonmyeloablating (NMA) chemotherapy preparative regimen could increase the complete response rate (12% NMA alone, 20% with 200 cGy TBI, 40% with 1,200 cGy TBI).11,12 We tested the hypothesis that increased lymphodepletion will improve clinical outcomes by adding 1,200 cGy TBI to the preparative chemotherapy regimen in a randomized, prospective fashion to determine rates of complete response and overall survival. Here, we report the analysis of this clinical study with median follow-up of 40.9 months in 101 patients with metastatic melanoma.
PATIENTS AND METHODS
Eligibility Criteria
Patients with histologically proven metastatic melanoma, with at least two measurable target lesions ≥ 1 cm on cross-sectional imaging and Eastern Cooperative Oncology Group performance status < 2 were eligible for screening and metastectomy for TIL. All patients were age ≥ 18 years with a life expectancy > 3 months and with adequate hepatic, renal, and bone marrow function and clear demonstration of progression of disease ≥ 4 weeks after any prior therapy. Exclusion criteria included contraindications to TBI, autoimmune disorders that required immunosuppressive therapy, or any active disease that would preclude the administration of IL-2. Before enrollment, TIL generated from patient tumors had to demonstrate growth in culture sufficient to reach quantities necessary for treatment. All patients provided written informed consent approved by the Institutional Review Board of the National Cancer Institute.
Study Design
Patients were randomly assigned to receive one of two lymphodepleting preparative regimens, designated NMA or 1,200 TBI. With the day of cell administration defined as day 0, both preparative regimens began on day −7. NMA consisted of cyclophosphamide 60 mg/kg/d for 2 days (days −7 and −6) and fludarabine 25 mg/m2/d for 5 days (days −7 to −3). Patients randomly assigned to 1,200 TBI received the same chemotherapy plus TBI 2 Gy twice per day, with a 6-hour interfraction interval for 3 days (days −3 to −1), for a total of 1,200 cGy. Fractions were delivered with 15-MV photons with opposed lateral beams, tissue compensators, and reduced lung doses (median 6 Gy) as previously described.13 On day 0, all patients received an intravenous infusion of autologous TIL and began high-dose IL-2 intravenously at 720,000 IU/kg every 8 hours to physiologic tolerance. Those patients who received TBI also received at least 2 × 106/kg of autologous, purified, cryopreserved CD34+ hematopoietic stem cells from a granulocyte colony-stimulating factor with or without plerixafor-mobilized pheresis. Prophylactic antimicrobials were administered to all patients, with the addition of oral levofloxacin for additional gram-negative coverage in patients who received TBI.
Efficacy
Patient response to treatment was assessed by using Response Evaluation Criteria in Solid Tumors (RECIST) v1.0 guidelines starting approximately 4 weeks from cell administration and proceeding at regular intervals thereafter. Primary end points were complete response (CR) rate and overall survival. Data in this report are updated as of October 1, 2015, with a median follow-up of 40.9 months.
Laboratory Procedures
TIL were grown from resected deposits of metastatic melanoma as previously described.14 Fresh tumor was dissected under sterile conditions. A representative sample was collected for formal pathologic analysis. Single fragments of 2 mm3 to 3 mm3 (goal of 24 per patient) were placed in individual wells of a 24-well plate, maintained in growth media with high-dose IL-2 (6,000 IU/mL), and monitored for destruction of tumor and/or proliferation of TIL. Any tumor that seemed to be viable remaining after processing was enzymatically digested into a single cell suspension and cryopreserved. Successfully grown TIL were sampled for phenotype analysis (CD3, CD4, CD8, and CD56) and tested against autologous tumor when available. TIL were considered reactive if overnight coculture yielded interferon-gamma (IFN-γ) levels > 200 pg/mL and twice background.15 Cultures with evidence of autologous reactivity or sufficient growth patterns were selected for rapid expansion (REP). If the patient was not moved directly to ACT, TIL were cryopreserved and thawed 2 days before REP. REP used OKT3 (anti-CD3) antibody (Miltenyi Biotech, San Diego, CA) and IL-2 (3,000 IU/mL; Prometheus, San Diego, CA) in the presence of irradiated feeder cells, autologous when possible, at a 100:1 ratio.14
Cell phenotypes of cryopreserved samples of infusion bag TIL were analyzed by flow cytometry (FlowJo) for surface markers CD3, CD4, CD8, CCR7, and CD45RA (BD BioSciences). Serum cytokines were measured by using standard enzyme-linked immunosorbent assay techniques. A rise in serum IFN-γ was defined as > 100 pg/mL and greater than 4 × baseline levels.
Statistical Considerations
An accrual ceiling of 56 patients per arm was selected to provide adequate power for both end points, described in detail in the Appendix (online only). Continuous parameters were compared between two groups by using an exact Wilcoxon rank-sum test. An exact Cochran-Armitage test was used to compare ordered categorical parameters between two groups.16 Dichotomous parameters were compared by using Fisher’s exact test, and unordered categorical parameters were compared between groups by using Mehta’s modification.17 When analyzing possible prognostic factors, two separate analyses were performed: CR versus non-CR and patients who achieved objective responses versus those who did not. All P values are two-tailed and not adjusted for multiple comparisons. Kaplan-Meier survival curves were created and analyzed by using the log-rank Mantel-Haenszel technique. Overall survival, duration of response, and progression-free survival were calculated from date of random assignment.
RESULTS
Patient Characteristics and Treatment
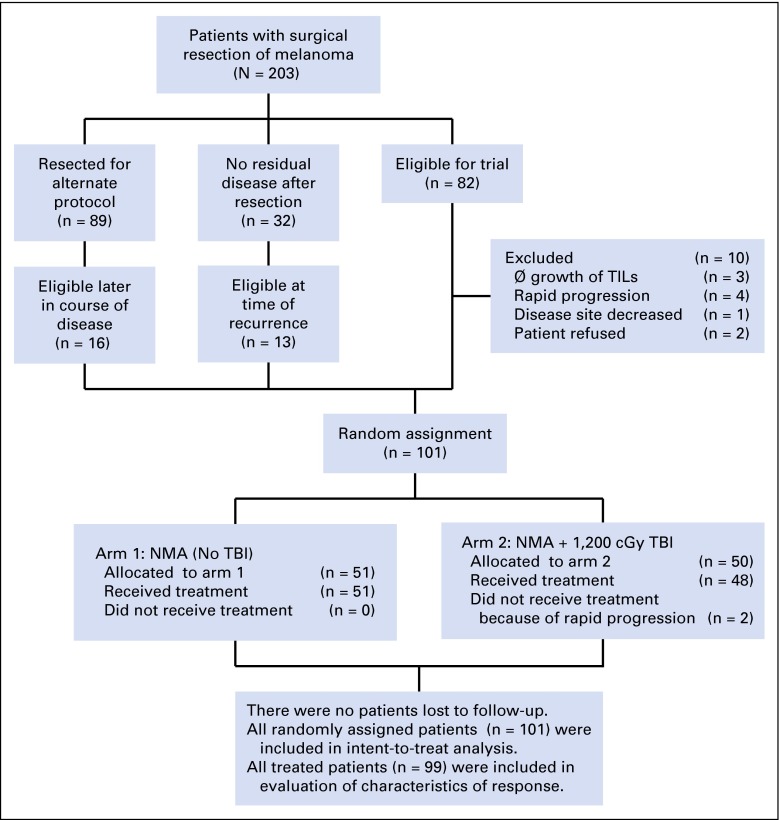
Over the course of this trial, 203 patients had resection of melanoma for various protocols. Of 82 resections specifically designated for this trial, 72 (88%) were randomly assigned. For three patients, TIL did not grow; one demonstrated a delayed response to prior therapy. Two patients withdrew consent postoperatively, and four patients had rapid progression of disease. Twenty-nine patients were not originally designated for this trial (13 had resection of all known disease, and 16 were considered for other protocols) but were enrolled and randomly assigned when progression occurred. Of 101 patients randomly assigned between March 2011 and December 2013, all completed their planned treatment course except two patients in the 1,200 TBI arm, whose treatment was aborted for progressive disease (Fig 1). All randomly assigned patients are included in the response and survival analyses. The Data Safety and Monitoring Board ended accrual in 2014 for a lack of differential efficacy.
Fig 1.
CONSORT diagram of enrollment. NMA, nonmyeloablative chemotherapy; TBI, total body irradiation; TIL, tumor-infiltrating lymphocyte.
There were no significant differences between arms in any measured patient characteristic (Table 1). The majority of patients had advanced disease (76% with M1c disease) and were heavily pretreated, although 26% were treatment naïve. This trial overlapped the clinical investigation and eventual approval of checkpoint modulators for the treatment of patients with metastatic melanoma, and 42 patients had progressed through prior treatment with monoclonal antibodies that targeted cytotoxic T-cell lymphocyte associated protein-4 (n = 31), programmed death-1 (PD-1; n = 3), or both (n = 8).
Table 1.
Patient Characteristics
| Characteristic | Treatment Arm | P | |
|---|---|---|---|
| NMA | 1,200 TBI | ||
| Patients | 51 | 50 | |
| Sex | .54 | ||
| Female | 17 (33) | 20 (40) | |
| Male | 34 (67) | 30 (60) | |
| Age, years | |||
| Median | 45 | 47 | .73 |
| 18-30 | 8 (16) | 3 (6) | .19* |
| 31-45 | 18 (35) | 16 (32) | |
| 46-60 | 22 (43) | 29 (58) | |
| 61-65 | 3 (6) | 2 (4) | |
| HLA | .32 | ||
| A2 | 19 (37) | 24 (48) | |
| Non-A2 | 32 (63) | 26 (52) | |
| Stage† | .63 | ||
| M1a | 3 (6) | 6 (12) | |
| M1b | 8 (16) | 8 (16) | |
| M1c | 40 (78) | 36 (72) | |
| Prior systemic treatment | .44 | ||
| None | 14 (27) | 12 (24) | |
| 1 systemic therapy | 22 (43) | 19 (38) | |
| ≥ 2 systemic therapies | 15 (29) | 19 (38) | |
| Immunotherapy | |||
| High-dose IL-2 | 17 (33) | 12 (24) | .38 |
| Anti–CTLA-4 only | 13 (26) | 18 (36) | .29 |
| Anti–PD-1 only | 1 (2) | 2 (4) | .62 |
| Anti–CTLA-4 and anti–PD-1 | 6‡ (12) | 2 (4) | .27 |
| Adjuvant (IFN-α, vaccine, etc) | 20 (39) | 18 (36) | .84 |
| Chemotherapy | |||
| Dacarbazine or temozolomide | 3 (6) | 8 (16) | .12 |
| BRAF and/or MEK inhibitor | 4 (8) | 5 (10) | .74 |
| Other (including biochemotherapy) | 5 (10) | 5 (10) | 1.0 |
| Select baseline value, median (25th to 75th percentile) | |||
| LDH, U/L | 182 (152-238) | 198 (154-317) | .29 |
| NLR | 2.40 (1.46-4.02) | 3.02 (1.92-4.61) | .05 |
| Platelets, K/μL | 222 (193-313) | 242 (197-305) | .62 |
NOTE. Data are given as No. of patients (%) unless otherwise noted.
Abbreviations: CTLA, cytotoxic T-cell lymphocyte associated protein-4; IFN-α, interferon-alfa; IL-2, interleukin-2; LDH, lactate dehydrogenase; MEK, mitogen-activated kinase kinase; NLR, neutrophil-to-lymphocyte ratio; PD-1, programmed death-1.
P value applies to all age ranges given.
M1a, skin, subcutaneous or nodal metastases; M1b, lung; M1c, all other viscera or elevated LDH.
Only two patients progressed through combination therapy, the others progressed sequentially.
There were no significant differences in the number of cells administered, the phenotype of the cells administered, nor the number of IL-2 doses administered between the two arms. Lymphodepletion is known to increase serum levels of the homeostatic cytokines, IL-7 and IL-15, and this was confirmed in this trial.13 Levels immediately before cell infusion were similar in both groups, although there was a trend toward increased serum IL-15 levels with TBI (Appendix Table A1, online only).
Antitumor Activity
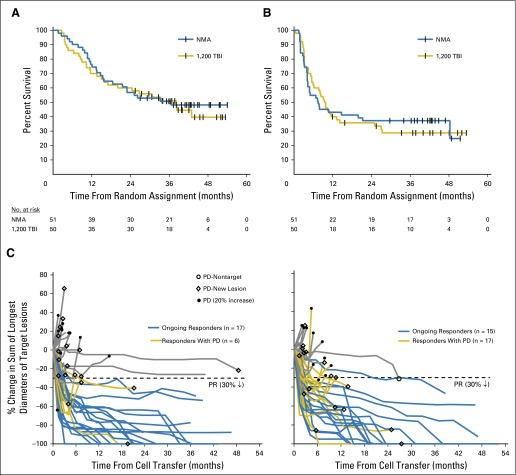
Primary end points of this study were objective CR rate and overall survival, and both were virtually identical between the two experimental arms. Each preparative regimen was able to mediate objective CR in 24% of patients (NMA: 12 of 51 patients; 95% CI, 13% to 37%; TBI: 12 of 50 patients; 95% CI, 13% to 38%; Table 2). Overall survival curves overlapped, with a median survival of 36.6 months in the NMA arm and 38.2 months in the 1,200 TBI arm (hazard ratio [HR], 1.11; 95% CI, 0.65 to 1.91; P = .71; Fig 2A). Progression-free survival curves were similarly indistinguishable, with a median time to progression of 7.5 months for patients who received NMA alone and 9.6 months in patients who received the addition of TBI (HR, 1.02; 95% CI, 0.64 to 1.65; P = .93; Fig 2B). Spider plots that depict the percent change in the sum of the longest diameters of target lesions are shown in Figure 2C. Although the 1,200 TBI arm had more patients with partial responses, they were often of short duration.
Table 2.
Response to Adoptive Cell Transfer
| Arm | Total, No. | PR | CR | OR, No. of Patients (%) | ||
|---|---|---|---|---|---|---|
| No. of Patients (%) | Duration of Response, Months | No. of Patients (%) | Duration of Response, Months | |||
| NMA | 51 | 11 (22) | 51+, 43+, 38+, 37+, 29+, 21, 19, 17, 6, 4, 4 | 12 (24) | 48+, 45+, 44+, 42+, 42+, 42+, 42+, 41+, 40+, 39+, 36+, 32+ | 23 (45) |
| 1,200 TBI | 50 | 19 (38) | 51+, 50+, 40+, 25, 19*+, 14, 13, 11, 11, 10, 9, 9, 9, 9, 8, 6, 5, 5, 4 | 12 (24) | 53+, 46+, 45+,42+, 42+, 38*+, 37+, 36+, 27,27+, 25+, 14*+ | 31 (62) |
| Total | 101† | 30 (30) | 24 (24) | 54 (54); P = .11 | ||
Abbreviations: +, ongoing response; CR, complete response; NMA, nonmyeloablative chemotherapy; OR, objective response; PR, partial response; TBI, total body irradiation.
Death with no evidence of progression.
An additional 10 patients underwent resection with intent to treat.
Fig 2.
(A) Overall survival of patients randomly assigned to receive tumor-infiltrating lymphocytes (TILs) with nonmyeloablating chemotherapy (NMA; n = 51) versus those assigned to receive the same chemotherapy with the addition of total body irradiation (TBI) 1,200 cGy (1,200 TBI; n = 50). (B) Progression-free survival of those patients who received TIL with NMA (n = 51) versus NMA with 1,200 TBI (n = 48). (C) Spider plots depicting the pattern of changes in target lesions of patients receiving adoptive cell transfer. (D) Only one patient who achieved a complete response has recurred, as depicted by the diamond on the abscissa of the 1,200 TBI graph. The similar diamond on the NMA graph describes a patient who had an unconfirmed complete response who experienced progression with a new lesion; hence, the best response is partial response (PR). PD, progressive disease.
Of 42 patients treated after experiencing progression on checkpoint blockade inhibition, 23 (55%) experienced objective response (OR), including 11 (26%) who achieved CR, which mirrored results in the total cohort. When looking specifically at patients whose disease had progressed through anti–PD-1 therapy (n = 11), there were two patients who achieved ongoing CR and two patients who experienced short-duration partial response (8 and 9 months).
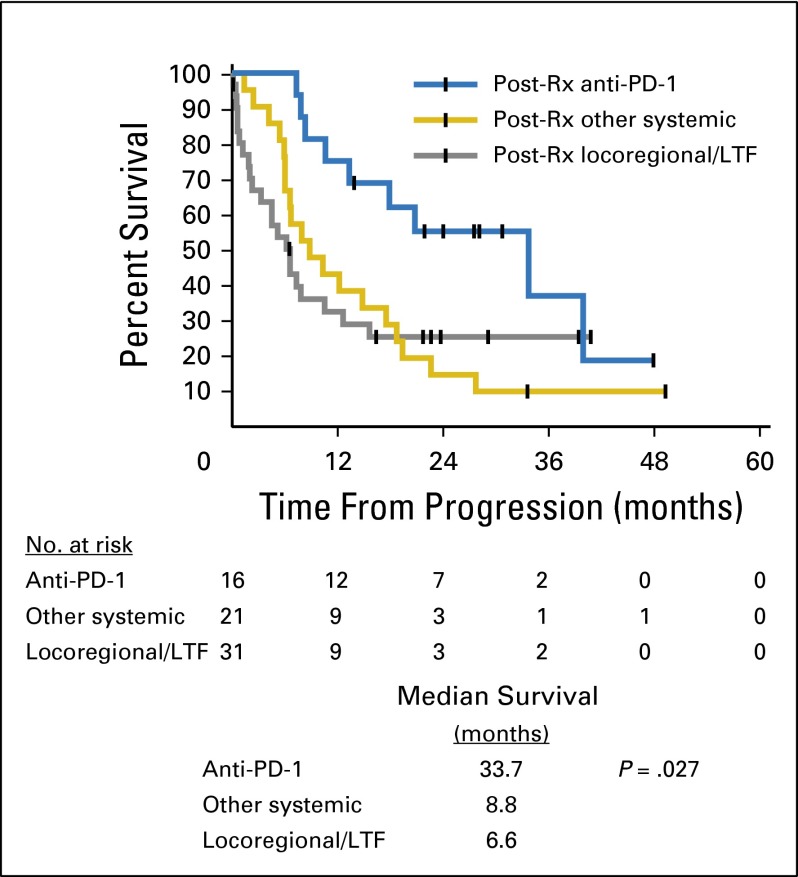
To more fully understand the survival curves, we gathered postprogression treatment data when available. In addition to the two patients who were not treated, an additional 66 patients experienced disease progression after ACT. There were no differences in the pattern of progression; 19 patients in each arm developed new sites of metastasis, and 14 patients in each arm progressed in existing disease. Sixteen patients (10 in the NMA arm) pursued at least one treatment that contained an anti–PD-1 agent. Although this might reflect a better performance status, these patients enjoyed a greater median survival, irrespective of response, than those who pursued locoregional treatments or non–PD-1 related systemic therapy (P = .013 for anti–PD-1 v locoregional; and P = .029 for anti–PD-1 v other systemic therapy, unadjusted; Appendix Fig A1, online only).
Toxicity
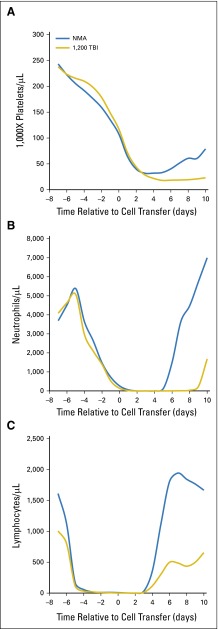
The toxicities of treatment were largely a result of the known adverse effects of nonmyeloablative chemotherapy and administration of high-dose IL-2. Despite infusion of autologous hematopoietic stem cells, patients in the 1,200 TBI arm had a slightly longer period of neutropenia, which resulted in a longer index admission but no increase in infection-related toxicity (Table 3, Appendix Fig A2, online only). Unique to the addition of TBI was the late onset (median time to diagnosis, 6.4 months; range, 4.8 to 11.7 months) of thrombotic microangiopathy (TMA) in 13 patients (27%).18 Although seen more frequently in patients who achieved responses (12 of 31) than in those who did not achieve responses (1 of 19), the diagnosis could be biased toward patients without rapid progression of disease. Management consisted of antihypertensive agents and transfusion support for associated anemia. There was one long-term treatment-related death in a patient who achieved a CR to therapy; complications secondary to TMA led to transfusion-related hemolytic anemia and eventual sepsis from immunosuppressive therapies. The patient died 15 months after treatment with no evidence of melanoma identified at autopsy.
Table 3.
Treatment-Related Toxicities and Clinical Course
| Variable | NMA (n = 51) | 1,200 TBI (n = 48) |
|---|---|---|
| Grade 3 and4 toxicities | ||
| Infectious | ||
| Febrile neutropenia | 25 | 36 |
| Bacteremia | 13 | 5 |
| Urinary tract infection | 0 | 2 |
| Noninfectious | ||
| Atrial fibrillation | 2 | 3 |
| Thrombotic microangiopathy | 0 | 13 |
| ICU transfer on index admission | 4 | 12 |
| Planned observation | 0 | 2 |
| Cytokine-related symptoms (no documented bacteremia) | 0 | 6 |
| Sepsis (documented bacteremia) | 2 | 1 |
| Cardiac arrhythmia | 2 | 3 |
| ICU intervention on index admission | ||
| Vasopressors/antiarrhythmics | 2 | 6 |
| Hemofiltration/hemodialysis | 1 | 2 |
| Intubation | 0 | 2 |
| Death* | ||
| Treatment-related | 0 | 1 |
| Length of stay† in days, median (25th to 75th percentile) | 18 (17-19) | 22 (21-22.8) |
| ICU length of stay in days, median (25th to 75th percentile) | 4 (2.5-4) | 4 (3-7.5) |
| Percent weight change from baseline‡, median (25th, 75th percentile) | −1.4% (−4.5, 0.6) | −9.7% (−14.0, −6.8) |
NOTE. Data are given as No. of patients (%) unless otherwise noted.
Abbreviations: ICU, intensive care unit; NMA, nonmyeloablative chemotherapy; TBI, total body irradiation.
Three late deaths (> 12 months from treatment; NMA, 1; 1,200 TBI, 2) were not attributable to treatment or melanoma progression.
Length of stay calculated from start of chemotherapy until discharge.
Measured at second follow-up (n = 42 for NMA; n = 46 for 1,200 TBI), excludes patients with progressive disease at first follow-up.
Whereas most patients experienced weight loss from prolonged hospitalization and chemotherapy, it seemed, clinically, that patients who received TBI had more chronic problems regaining appetite and returning to pretreatment body weight. Objectively, weight loss (percent change) at second scheduled follow-up (median 96 days after random assignment) was significantly greater in the TBI arm (−9.7% v −1.4%, respectively; P < .001; Table 3).
Characteristics of Response
Given the near identical CR rates and survival curves between the treatment arms, we combined cohorts to analyze for possible factors associated with response. There were no statistically significant differences in age, sex, stage, or prior therapy (Table 4). Baseline lactate dehydrogenase and neutrophil-to-lymphocyte ratio had statistically different medians but with widely overlapping ranges (Appendix Fig A3, online only).
Table 4.
Patient Characteristics by Response
| Characteristic | Total, No. | CR, No. (%) | PR, No. (%) | NR*, No. | P† | |
|---|---|---|---|---|---|---|
| CR v PR + NR | CR + PR v NR | |||||
| Patients | 101 | 24 | 30 | 47 | ||
| Sex | ||||||
| Female | 37 | 9 (24) | 12 (32) | 16 | 1.0 | .68 |
| Male | 64 | 15 (23) | 18 (28) | 31 | ||
| Age, years | ||||||
| Median | 52.5 | 46 | 46 | .024 | .37 | |
| 18-30 | 11 | 0 (0) | 4 (36) | 7 | .12‡ | .60‡ |
| 31-45 | 34 | 8 (24) | 10 (29) | 16 | ||
| 46-60 | 51 | 15 (29) | 16 (31) | 20 | ||
| 61-65 | 5 | 1 (20) | 0 (0) | 4 | ||
| HLA | ||||||
| A2 | 43 | 15 (35) | 8 (19) | 20 | .03 | 1.0 |
| Non-A2 | 58 | 9 (16) | 22 (38) | 27 | ||
| Stage | ||||||
| M1a | 9 | 2 (22) | 5 (56) | 2 | .37 | .03 |
| M1b | 16 | 6 (38) | 6 (38) | 4 | ||
| M1c | 76 | 16 (21) | 19 (25) | 41 | ||
| Prior systemic treatments | 1.00 | 1.00 | ||||
| None | 26 | 5 (19) | 7 (27) | 14 | ||
| 1 systemic therapy | 41 | 12 (29) | 14 (34) | 15 | ||
| ≥ 2 systemic therapies | 34 | 7 (21) | 9 (26) | 18 | ||
| Immunotherapy | ||||||
| High-dose IL-2 | 29 | 8 (28) | 9 (31) | 12 | .61 | .66 |
| Anti–CTLA-4 only | 31 | 9 (29) | 10 (32) | 12 | .45 | .39 |
| Anti–PD-1 only | 3 | 1 (33) | 1 (33) | 1 | .56 | .14 |
| Anti–CTLA-4 and anti–PD-1 | 8 | 1§ (13) | 1 (13) | 6§ | .68 | .54 |
| Adjuvant (IFN-α, vaccine, etc) | 38 | 9 (24) | 13 (34) | 16 | 1.0 | 1.0 |
| Chemotherapy | ||||||
| Dacarbazine or temozolomide | 11 | 1 (9) | 4 (36) | 6 | .45 | .75 |
| Small-molecule inhibitor | 9 | 0 (0) | 2 (22) | 7 | .11 | .078 |
| Other (including biochemotherapy) | 10 | 3 (30) | 0 (0) | 7 | .70 | .18 |
| Select baseline values, median (25th to 75th percentile | ||||||
| LDH, U/L | 157 (145-212) | 179 (154-230) | 211 (158-322) | .04 | .02 | |
| NLR | 1.99 (1.23-3.18) | 2.69 (1.66-3.96) | 3.12 (2.24-5.23) | .004 | .002 | |
| Platelets, K/μL | 227 (197-316) | 229 (171-282) | 237 (201-326) | .75 | .34 | |
Abbreviations: CR, complete response; CTLA, cytotoxic T-cell lymphocyte associated protein-4; IFN-α, interferon-alfa; IL-2, interleukin-2; LDH, lactate dehydrogenase; NLR, neutrophil-to-lymphocyte ratio; NR, nonresponse; PD-1, programmed death-1; PR, partial response.
Two patients did not receive treatment in the 1,200 TBI arm and are identified as NR.
All P values are uncorrected.
P value applies to all age ranges given.
Two patients had previously been treated with combination therapy, the remainder were treated sequentially.
Furthermore, there were no differences when evaluating the characteristics of the source of TIL. Nodules resected from viscera, lymph nodes, and subcutaneous deposits were all capable of mediating durable CRs (Table 5). For 15 patients, we moved directly to treatment phase without cryopreservation; however, this did not provide any treatment advantage (7 of 15 OR; 47% v 47 of 84 OR; 56%; P = .58). The ability of TIL to recognize autologous fresh tumor in vitro was not predictive of response, nor was the presence of presumed CD8+ tumor recognition (class I blockable reactivity); however, wide variation in target tumor quality and viability may have interfered with the ability to demonstrate recognition. There were no differences in the frequency of reactivity of the TIL fragments from patients who achieved responses and those who did not (Appendix Fig A4, online only).
Table 5.
Treatment Characteristics by Response
| Characteristic | Total, No. | CR, No. (%) | PR, No. (%) | NR, No. | P* | |
|---|---|---|---|---|---|---|
| CR v PR + NR | CR + PR v NR | |||||
| Patients treated | 99 | 24 | 30 | 45 | ||
| Source of TIL | ||||||
| Subcutaneous deposit | 31 | 7 (23) | 13 (42) | 11 | .47 | .31 |
| Lymph node | 33 | 6 (18) | 9 (27) | 18 | ||
| Viscera | 35 | 11 (31) | 8 (23) | 16 | ||
| Fresh TIL | 15 | 4 (26) | 3 (20) | 8 | .75 | .58 |
| Cryopreserved TIL | 84 | 20 (24) | 27 (32) | 37 | ||
| Treatment characteristic | ||||||
| CD3+ cells | ||||||
| < 5 × 1010 | 21 | 3 (14) | 5 (24) | 13 | .16 | .005 |
| 5.1-7.0 × 1010 | 26 | 6 (23) | 6 (23) | 14 | ||
| 7.1-9.0 × 1010 | 18 | 4 (22) | 6 (33) | 8 | ||
| 9.1-11.0 × 1010 | 16 | 5 (31) | 4 (25) | 7 | ||
| > 11 × 1010 | 18 | 6 (33) | 9 (50) | 3 | ||
| Cell phenotype, median (25th to 75th percentile ×10−9) | ||||||
| CD3+ | 87.7 (61.1-117) | 83.3 (54.8-114) | 65.7 (46.4-86.3) | .10 | .0059 | |
| CD8+ | 79.7 (49.5-96.5) | 61.2 (31.5-106) | 39.4 (25.7-58) | .014 | .0007 | |
| CD4+ | 8.9 (4.8-17.4) | 11.1 (4.3-22.8) | 12.0 (7.5-25.8) | .19 | .13 | |
| T-cell subsets, median (25th to 75th percentile), % | ||||||
| TN | 0.02 (0.007-0.08) | 0.02 (0.005-0.13) | 0.07 (0.02-0.20) | .26 | .013 | |
| TCM | 0.37 (0.22-0.51) | 0.33 (0.20-0.40) | 0.36 (0.22-0.58) | .82 | .31 | |
| TEM | 96.3 (93.6-98.7) | 97.1 (90.9-98.6) | 91.7 (80.7-97.2) | .21 | .002 | |
| TEMRA | 3.3 (1.0-6.0) | 2.6 (1.0-8.9) | 8.2 (2.5-18.9) | .20 | .002 | |
| IL-2 doses | ||||||
| 0-2 | 11 | 0 (0) | 3 (27) | 8 | .46 | .53 |
| 3-5 | 39 | 12 (31) | 13 (33) | 14 | ||
| 6-8 | 41 | 10 (24) | 11 (27) | 20 | ||
| > 8 | 8 | 2 (25) | 3 (38) | 3 | ||
| Median (25th to 75th percentile) | 5.5 (5-7) | 5 (4-6.3) | 6 (3.5-7) | .34 | .55 | |
| Laboratory characteristics† | ||||||
| IL-7, median (25th to 75th percentile), pg/mL | 37 (31.9-49.5) | 32.5 (27.8-45.8) | 39.8 (34.8-51.5) | .98 | .07 | |
| IL-15, median (25th to 75th percentile), pg/mL | 33 (29.4-42) | 35.5 (31-51.3) | 38.8 (32.9-52.1) | .07 | .08 | |
| Peak absolute lymphocyte count, cells/μL | ||||||
| 0-500 | 45 | 7 (16) | 15 (33) | 23 | .013 | .25 |
| 501-2,000 | 34 | 9 (26) | 12 (35) | 13 | ||
| 2,001-5,000 | 11 | 4 (36) | 0 | 7 | ||
| 5,001-10,000 | 6 | 1 (17) | 3 (50) | 2 | ||
| >10,000 | 3 | 3 (100) | 0 | 0 | ||
| Median (25th to 75th percentile), ×10−3/μL | 0.9 (0.4-3.5) | 0.5 (0.2-1.2) | 0.5 (0.2-1.3) | .033 | .40 | |
Abbreviations: CR, complete response; IL, interleukin; NR, nonresponse; PR, partial response; TCM, CD3+CD45RA−CCR7+; TEM, CD3+CD45RA−CCR7−; TEMRA, CD3+CD45RA+CCR7−; TIL, tumor-infiltrating lymphocyte; TN, CD3+CD45RA+CCR7+.
All P values are uncorrected.
IL-7 and IL-15 measured on day 0, maximum absolute lymphocyte count from day 0 to day +9.
When analyzing treatment variables, patients who achieved OR received significantly higher cell doses (P = .0059) and significantly more total CD8+ T cells (P = .0007). This trial was not designed to answer the question of cell dose, as each patient received as many cells as could be manufactured during the clinical REP. In vitro growth may be an intrinsic quality of successful TIL, but there was no evidence of a meaningful threshold to predict response. The vast majority of all infused TIL were within an effector memory subpopulation, as defined by lack of CCR7 and CD45RA surface expression.19 There was a trend toward more terminally differentiated effector memory cells that coexpressed CD45RA (TEMRA) in the treatments that did not result in response but that trend was of borderline statistical significance (P = .05, unadjusted; Table 5, Appendix Fig A5, online only).
Patients varied greatly in their tolerance to IL-2 (range, zero to 10 doses) but without observed differences between patients who achieved responses and those who did not (five v six median doses; P = .53). There is a trend toward higher peak circulating absolute lymphocyte counts after cell infusion in patients who experienced CR (P = .036; Appendix Fig A5). There were no differences in postlymphodepletion serum IL-7 and IL-15 levels (Table 5). A serum IFN-γ surge within the first 3 days of cell administration was not predictive of response (34 of 97 patients, with four CRs, 11 partial responses, and 19 nonresponses).
DISCUSSION
In this study, ACT of TIL mediated objective CRs in 24% of 101 patients with metastatic melanoma, with 51% overall survival at 3 years. Addition of TBI did not increase CR rates or impact overall survival, but did introduce a new toxicity in the form of TMA. The nonmyeloablative chemotherapy regimen thus seemed to provide sufficient lymphodepletion for successful adoptive transfer without the need to add TBI. It is likely that the high response rates in our earlier studies of TBI can be attributed to patient selection and highlights the need for random assignment to overcome that bias.
There were no clinical or laboratory parameters that could predict response. Even those with statistically different means had sufficient overlap to make them ineffective predictors. Our group previously demonstrated that longer telomere length and persistence of administered lymphocytes at 1 month were associated with response.20 Others have demonstrated that a higher proportion of CD8+BTLA4+ TIL correlated with response.9 Recently, analyses of patients who received checkpoint blockade identified neutrophil-to-lymphocyte ratio < 3 and normal lactate dehydrogenase as positive predictors of response; however, in our lymphodepleted patient population, neither separated patients who achieved responses from those who did not clearly enough to warrant use as an inclusion criterion.21,22
Our understanding of TIL antigen specificity in both melanoma and epithelial cancers has evolved since this study was begun. Whole-exome sequencing of melanoma tumors identified nonsynonymous somatic mutations that were recognized by autologous TIL, separate from well-characterized reactivity against shared melanoma differentiation antigens.23,24 These mutation-reactive cells were identified in the PD-1+ population.25 In a single patient with cholangiocarcinoma, a TIL treatment with enriched mutation reactive cells led to objective tumor response now ongoing beyond 2 years.26 A careful evaluation of mutation-reactive cells in both patients who achieve response and those who do not among patients with melanoma treated with TIL is now underway and may yield important new insights. By using tandem mini-gene techniques to display personalized nonsynonymous mutations on autologous antigen-presenting cells as targets, we may overcome the inconsistencies inherent in testing TIL against autologous tumor preparations of variable quality.
Recent advances in clinical immunotherapy have provided new therapeutic options for patients with melanoma. In the largest trial of ipilimumab, a humanized monoclonal antibody against cytotoxic T-cell lymphocyte associated protein-4, there were objective tumor regressions (OR 38 of 540 patients; 7%; CR in three patients) combined with severe adverse effects, most notably immune-mediated colitis (3% to 5%).27 A pooled analysis of patients who received ipilimumab confirmed the durability of those responses with a 3-year survival of 22% that remained relatively constant out to 10 years.28 Monoclonal antibodies that target PD-1 can mediate CRs with a more tolerable adverse-effect profile and fewer episodes of colitis.29,30 Nivolumab can mediate ORs in 32% of ipilimumab-refractory patients and 40% of treatment-naïve patients.31,32 Pembrolizumab is similarly effective in those populations (OR, 26% and 33%, respectively).33,34 The combination of ipilimumab and nivolumab can mediate even greater ORs in 58% of patients (11% CR), but with a high rate of immune-mediated adverse effects.35
When evaluating the efficacy of either checkpoint blockade or ACT, one must consider the durability of clinical benefit. At the time of this writing, median potential follow-up for patients treated with combination checkpoint blockade is < 2 years. Of 24 patients who achieve CR in this study, plus the 20 patients reported previously by our group, only two have developed recurrent melanoma at 19 and 27 months with a median potential follow-up of 53.4 months.
The patients in this study whose disease had progressed through checkpoint blockade had outcomes almost identical to the group as a whole, but the small experience prevents a meaningful analysis of any one specific regimen or agent. This suggests that tumor regression that is mediated by ACT may exploit additional mechanisms distinct from or in addition to those used by checkpoint blockade. In a currently accruing trial, we have evaluated an additional eight patients with disease that had progressed through PD-1 blockade, with two ORs. Efficacy of ACT after progression of disease through anti–PD-1 therapy remains an open question and is currently being investigated.
The tripartite regimen developed at the Surgery Branch of the National Cancer Institute is capable of providing complete, durable, and likely curative responses in patients with metastatic melanoma and is a viable experimental therapeutic option. The relative contributions of augmenting the antitumor repertoire through ACT and manipulating the tumor microenvironment are not yet known, and optimal treatment may require both, which is a hypothesis we are currently testing with the addition of pembrolizumab to ACT. Alternatively, cell transfer therapy may find a role as a salvage treatment for patients who are refractory to other approaches.
Supplementary Material
Acknowledgment
We thank Lien Ngo, Melissa Corbitt, Lynette Nixon, and Paul Robbins, PhD.
Appendix
Statistical Considerations
The initial accrual ceiling of the trial was 112 evaluable patients, which was determined to provide adequate power for two primary end point comparisons: complete response rate and overall survival (OS) between the two arms, with a 0.025 two-tailed significance level for each. Fifty-six patients per arm would provide 80% power to compare 8% versus 33% complete responses between the two arms. In addition, this accrual number would provide 88% power to compare the arms, assuming median OS of 8 and 16 months and accrual over 3 years, with 2 years of additional follow-up.
Data Safety and Monitoring Board Monitoring
The protocol called for a futility evaluation at the first Data Safety and Monitoring Board meeting after 56 total patients were randomly assigned and observed for at least 6 months. Because of rapid accrual, the futility evaluation performed at the annual first meeting included 78 total patients and did not result in closing the study as the conditional power on the basis of survival exceeded 10% at that time. A year later, when 101 total patients were enrolled (95 evaluable), survival curves were not significantly different (P = .86). Because the accrual rate had slowed during the year, the Data Safety and Monitoring Board voted to close the trial to future enrollment as a result of of a lack of differential efficacy between the arms with respect to OS.
Toxicity
There were three patient deaths that would be censored in an analysis of disease-specific survival. In the arm that received total body irradiation 1,200 cGy, one patient who achieved a complete response developed an endometrial carcinosarcoma 33 months after therapy, and one patient who had a partial response died of complications of normal pressure hydrocephalus (19 months). A third patient (partial response; nonmyeloablative chemotherapy arm) died of operative complications after her disease progressed (14.7 months).
Fig A1.
Postprogression survival measured from date of progression to date of death (n = 50) or data cutoff date (n = 17) in patients who progressed after treatment with adoptive cell transfer. Groups were designated by type of therapy initiated without further data on response to that therapy. LTF, lost to follow-up or unable to obtain treatment details; PD-1, programmed death-1; Rx, treatment.
Fig A2.
Mean hematopoietic cell counts were transiently depressed in patients who received adoptive cell transfer, with a slightly longer period of neutropenia in patients who received total body irradiation 1,200 cGy TBI. Mean absolute counts were based on daily clinical CBCs. (A) Platelet counts, (B) absolute neutrophil counts, (C) absolute lymphocyte counts. NMA, nonmyeloablative chemotherapy.
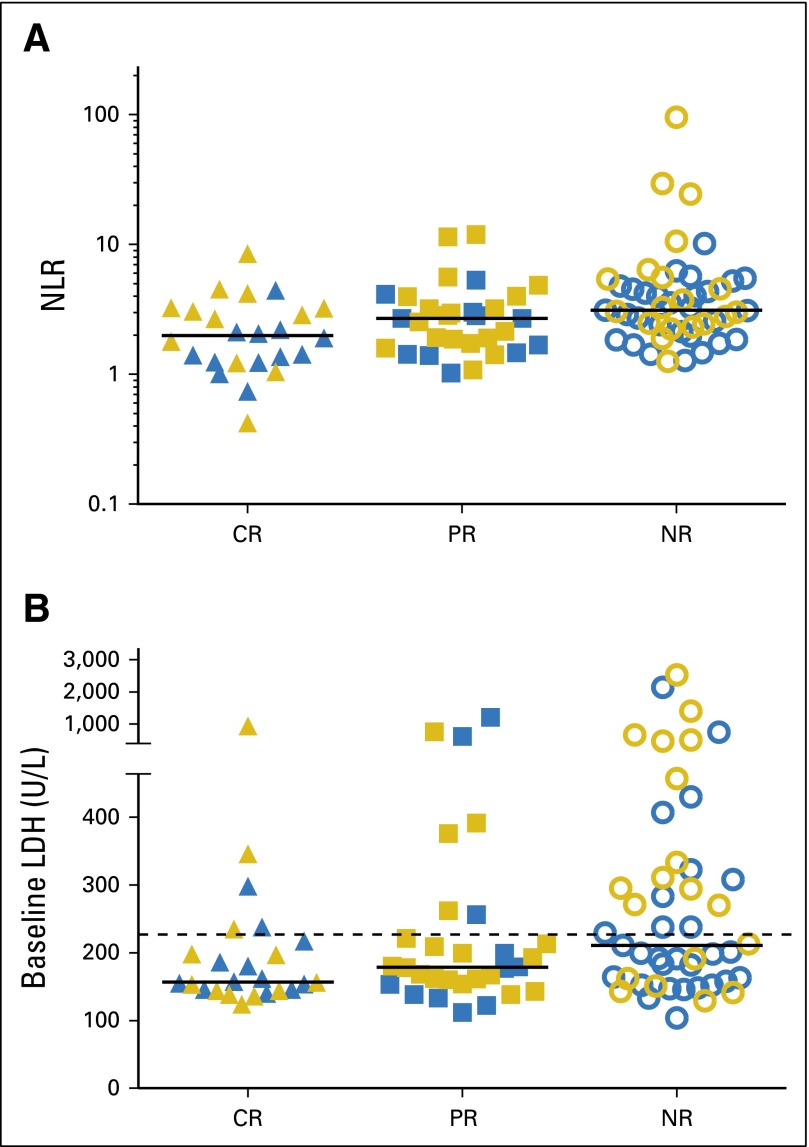
Fig A3.
Peripheral blood was sampled before the start of chemotherapy for all 101 randomly assigned patients. (A) The median neutrophil-to-lymphocyte ratios (NLRs) were significantly different between response groups but without predictive value. (B) Baseline lactate dehydrogenase (LDH) values also had significantly different medians, and 34 patients had elevated values, including 5 who achieved complete response (CR). Color denotes arm of trial (blue, nonmyeloablative chemotherapy; gold, total body irradiation) and shape denotes response (▲, CR; ■, partial response [PR]; ○, no response [NR]). Lines denote median values, dashed line denotes upper limit of normal.
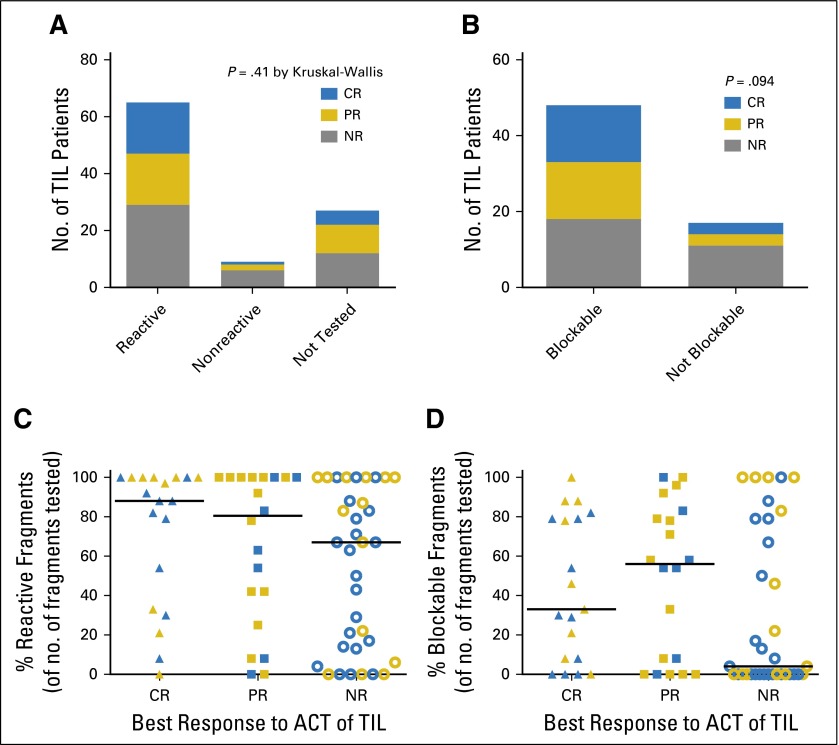
Fig A4.
(A) Autologous fresh tumor was available for use as targets in a coculture to measure interferon-gamma (IFN-γ) release by tumor-infiltrating lymphocyte (TIL) fragments for 74 patients. (B) Ability of HLA class I antibodies to block IFN-γ release was used as an indirect measure of CD8+ tumor recognition in the 65 patients with a positive screen. It was not uncommon to witness variation between fragments for a single patient. To demonstrate TIL heterogeneity in the 74 patients whose TILs were tested, we show (C) reactive fragments and (D) blockable fragments (number of positive wells/total number of wells tested (median/patient 24, range 6 to 36). Color denotes arm of trial (blue, nommyeloablative chemotherapy; gold, total body irradiation) and shape denotes response (▲, complete response [CR]; ■, partial response [PR]; ○, no response [NR]). Lines denote median values. ACT, adoptive cell transfer.
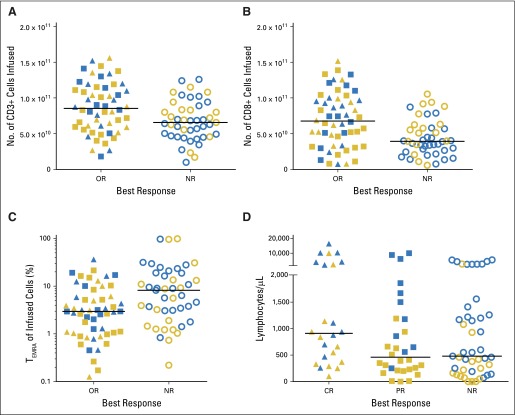
Fig A5.
Characteristics of administered tumor-infiltrating lymphocytes and evaluation of peak circulating lymphocytes in post-treatment days 0 to 9. Color denotes arm of trial (blue, nommyeloablative chemotherapy; gold, total body irradiation) and shape denotes response (▲, complete response [CR]; ■, partial response [PR]; ○, no response [NR]). Lines denote median values. (A) Number of CD3+ T cells in infusion bag in patients who achieved response (CR + PR) versus those who did not (NR). (B) Number CD8+ cells. (C) Percent of infused T cells that were CD3+CD45RA+CCR7− (TEMRA). (D) Maximum absolute lymphocyte count as measured in the peripheral blood of patients in treatment days 0 to 9. OR, objective response.
Table A1.
Treatment Characteristics by Arm
| Characteristic | Total, No. | NMA, No. (%) | 1,200 TBI, No. (%) | P* |
|---|---|---|---|---|
| Patients treated | 99 | 51 | 48 | |
| Source of TIL | ||||
| Subcutaneous deposit | 31 | 16 (52) | 15 (48) | .96 |
| Lymph node | 33 | 16 (48) | 17 (52) | |
| Viscera | 35 | 19 (54) | 16 (46) | |
| Fresh TIL | 15 | 7 (47) | 8 (53) | .78 |
| Cryopreserved TIL | 84 | 44 (52) | 40 (48) | |
| Treatment characteristics | ||||
| CD3+ cells | ||||
| < 5 × 1010 | 21 | 13 (62) | 8 (38) | .94 |
| 5.1-7.0 × 1010 | 26 | 12 (46) | 14 (54) | |
| 7.1-9.0 × 1010 | 18 | 7 (39) | 11 (61) | |
| 9.1-11.0 × 1010 | 16 | 9 (56) | 7 (44) | |
| > 11 × 1010 | 18 | 10 (56) | 8 (44) | |
| Cell phenotype, median (25th to 75th percentile ×10−9) | ||||
| CD3+ | 70.1 (49.4-104) | 73.1 (56.6-104) | .83 | |
| CD8+ | 41.3 (28.7-78.9) | 56.5 (33.4-90.9) | .22 | |
| CD4+ | 12.6 (7.4-22.7) | 10.4 (4.2-18.1) | .09 | |
| T-cell subsets, median (25th to 75th percentile), % | ||||
| TN | 0.03 (0.01-0.16) | 0.02 (0.007-0.14) | .32 | |
| TCM | 0.36 (0.26-0.44) | 0.31 (0.19-0.51) | .50 | |
| TEM | 94.9 (82-97) | 96.6 (89.6-98.6) | .014 | |
| TEMRA | 4.6 (2.8-17.1) | 3.2 (1.0-9.1) | .014 | |
| IL-2 doses | ||||
| 0-2 | 11 | 4 (36) | 7 (64) | .32 |
| 3-5 | 39 | 20 (51) | 19 (49) | |
| 6-8 | 41 | 22 (54) | 19 (46) | |
| > 8 | 8 | 5 (63) | 3 (37) | |
| Median (25th to 75th percentile) | 6 (4-7) | 5 (3.3-6) | .15 | |
| Laboratory characteristics | ||||
| Day 0 IL-7, median (25th to 75th percentile), pg/mL | 37 (31.0-51.5) | 39 (29.8-48) | .70 | |
| Day 0 IL-15, median (25th to 75th percentile), pg/mL | 34 (29.5-44.5) | 39 (33-53.5) | .05 |
Abbreviations: IL, interleukin; NMA, nonmyeloablative chemotherapy; TBI, total body irradiation; TCM, CD3+CD45RA−CCR7+; TEM, CD3+CD45RA−CCR7−; TEMRA, CD3+CD45RA+CCR7−; TIL, tumor-infiltrating lymphocyte; TN, CD3+CD45RA+CCR7+.
All P values are uncorrected.
Footnotes
Supported by the Center for Cancer Research at the National Cancer Institute of the US National Institutes of Health, by a generous gift from the Adelson Medical Research Foundation, and through a cooperative research and development agreement with Lion Biotechnologies.
Authors’ disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHOR CONTRIBUTIONS
Conception and design: Mark E. Dudley, Deborah E. Citrin, James C. Yang, Richard M. Sherry, Christopher A. Klebanoff, Marybeth S. Hughes, Nicholas P. Restifo, Steven A. Rosenberg
Administrative support: Daniel A. Zlott, Kathleen E. Morton, Mary Ann Toomey
Collection and assembly of data: Stephanie L. Goff, Mark E. Dudley, Deborah E. Citrin, Robert P. Somerville, John R. Wunderlich, David N. Danforth, Daniel A. Zlott, James C. Yang, Richard M. Sherry, Christopher A. Klebanoff, Marybeth S. Hughes, Michelle M. Langhan, Thomas E. Shelton, Lily Lu, Mei Li M. Kwong, Sadia Ilyas, Nicholas D. Klemen, Eden C. Payabyab, Kathleen E. Morton, Mary Ann Toomey, Donald E. White, Steven A. Rosenberg
Data analysis and interpretation: Stephanie L. Goff, Robert P. Somerville, James C. Yang, Richard M. Sherry, Udai S. Kammula, Lily Lu, Seth M. Steinberg, Steven A. Rosenberg
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Randomized, Prospective Evaluation Comparing Intensity of Lymphodepletion Before Adoptive Transfer of Tumor-Infiltrating Lymphocytes for Patients With Metastatic Melanoma
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Stephanie L. Goff
No relationship to disclose
Mark E. Dudley
Employment: Novartis
Research Funding: Kite Pharma (Inst)
Patents, Royalties, Other Intellectual Property: Immunotherapy with in vitro–selected antigen-specific lymphocytes after nonmyeloablative lymphodepleting chemotherapy; patent application No. US 8287857 B2
Deborah E. Citrin
No relationship to disclose
Robert P. Somerville
No relationship to disclose
John R. Wunderlich
No relationship to disclose
David N. Danforth
Stock or Other Ownership: Pfizer, Gilead Sciences, Biomarin
Daniel A. Zlott
No relationship to disclose
James C. Yang
Stock or Other Ownership: Pfizer, Express Scripts
Patents, Royalties, Other Intellectual Property: T-cell receptors recognizing cancer antigens
Richard M. Sherry
No relationship to disclose
Udai S. Kammula
No relationship to disclose
Christopher A. Klebanoff
No relationship to disclose
Marybeth S. Hughes
No relationship to disclose
Nicholas P. Restifo
No relationship to disclose
Michelle M. Langhan
No relationship to disclose
Thomas E. Shelton
No relationship to disclose
Lily Lu
No relationship to disclose
Mei Li M. Kwong
No relationship to disclose
Sadia Ilyas
No relationship to disclose
Nicholas D. Klemen
No relationship to disclose
Eden C. Payabyab
No relationship to disclose
Kathleen E. Morton
No relationship to disclose
Mary Ann Toomey
No relationship to disclose
Seth M. Steinberg
Patents, Royalties, Other Intellectual Property: Patent pending for method of selecting cancer patients for antiangiogenesis therapy in combination with chemotherapy
Donald E. White
No relationship to disclose
Steven A. Rosenberg
No relationship to disclose
REFERENCES
- 1. American Cancer Society: Cancer Facts and Figures 2015. Atlanta, GA, American Cancer Society, 2015.
- 2.Wingo PA, Tong T, Bolden S. Cancer statistics, 1995. CA Cancer J Clin. 1995;45:8–30. doi: 10.3322/canjclin.45.1.8. [DOI] [PubMed] [Google Scholar]
- 3.Smith FO, Downey SG, Klapper JA, et al. Treatment of metastatic melanoma using interleukin-2 alone or in conjunction with vaccines. Clin Cancer Res. 2008;14:5610–5618. doi: 10.1158/1078-0432.CCR-08-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenberg SA, Lotze MT, Muul LM, et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med. 1985;313:1485–1492. doi: 10.1056/NEJM198512053132327. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg SA, Yannelli JR, Yang JC, et al. Treatment of patients with metastatic melanoma with autologous tumor-infiltrating lymphocytes and interleukin 2. J Natl Cancer Inst. 1994;86:1159–1166. doi: 10.1093/jnci/86.15.1159. [DOI] [PubMed] [Google Scholar]
- 6.Dudley ME, Wunderlich JR, Yang JC, et al. A phase I study of nonmyeloablative chemotherapy and adoptive transfer of autologous tumor antigen-specific T lymphocytes in patients with metastatic melanoma. J Immunother. 2002;25:243–251. doi: 10.1097/01.CJI.0000016820.36510.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Besser MJ, Shapira-Frommer R, Itzhaki O, et al. Adoptive transfer of tumor-infiltrating lymphocytes in patients with metastatic melanoma: Intent-to-treat analysis and efficacy after failure to prior immunotherapies. Clin Cancer Res. 2013;19:4792–4800. doi: 10.1158/1078-0432.CCR-13-0380. [DOI] [PubMed] [Google Scholar]
- 8.Pilon-Thomas S, Kuhn L, Ellwanger S, et al. Efficacy of adoptive cell transfer of tumor-infiltrating lymphocytes after lymphopenia induction for metastatic melanoma. J Immunother. 2012;35:615–620. doi: 10.1097/CJI.0b013e31826e8f5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Radvanyi LG, Bernatchez C, Zhang M, et al. Specific lymphocyte subsets predict response to adoptive cell therapy using expanded autologous tumor-infiltrating lymphocytes in metastatic melanoma patients. Clin Cancer Res. 2012;18:6758–6770. doi: 10.1158/1078-0432.CCR-12-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dudley ME, Wunderlich JR, Yang JC, et al. Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. J Clin Oncol. 2005;23:2346–2357. doi: 10.1200/JCO.2005.00.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenberg SA, Yang JC, Sherry RM, et al. Durable complete responses in heavily pretreated patients with metastatic melanoma using T-cell transfer immunotherapy. Clin Cancer Res. 2011;17:4550–4557. doi: 10.1158/1078-0432.CCR-11-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wrzesinski C, Paulos CM, Kaiser A, et al. Increased intensity lymphodepletion enhances tumor treatment efficacy of adoptively transferred tumor-specific T cells. J Immunother. 2010;33:1–7. doi: 10.1097/CJI.0b013e3181b88ffc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dudley ME, Yang JC, Sherry R, et al. Adoptive cell therapy for patients with metastatic melanoma: Evaluation of intensive myeloablative chemoradiation preparative regimens. J Clin Oncol. 2008;26:5233–5239. doi: 10.1200/JCO.2008.16.5449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dudley ME, Wunderlich JR, Shelton TE, et al. Generation of tumor-infiltrating lymphocyte cultures for use in adoptive transfer therapy for melanoma patients. J Immunother. 2003;26:332–342. doi: 10.1097/00002371-200307000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goff SL, Smith FO, Klapper JA, et al. Tumor infiltrating lymphocyte therapy for metastatic melanoma: Analysis of tumors resected for TIL. J Immunother. 2010;33:840–847. doi: 10.1097/CJI.0b013e3181f05b91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agresti A. Categorical data analysis. New York, NY: Wiley; 1990. [Google Scholar]
- 17.Mehta CR, Patel NR. A network algorithm for performing Fisher’s exact test in r × c contingency tables. J Am Stat Assoc. 1983;78:427–434. [Google Scholar]
- 18.Tseng J, Citrin DE, Waldman M, et al. Thrombotic microangiopathy in metastatic melanoma patients treated with adoptive cell therapy and total body irradiation. Cancer. 2014;120:1426–1432. doi: 10.1002/cncr.28547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geginat J, Lanzavecchia A, Sallusto F. Proliferation and differentiation potential of human CD8+ memory T-cell subsets in response to antigen or homeostatic cytokines. Blood. 2003;101:4260–4266. doi: 10.1182/blood-2002-11-3577. [DOI] [PubMed] [Google Scholar]
- 20.Zhou J, Shen X, Huang J, et al. Telomere length of transferred lymphocytes correlates with in vivo persistence and tumor regression in melanoma patients receiving cell transfer therapy. J Immunol. 2005;175:7046–7052. doi: 10.4049/jimmunol.175.10.7046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferrucci PF, Ascierto PA, Pigozzo J, et al. Baseline neutrophils and derived neutrophil-to-lymphocyte ratio: Prognostic relevance in metastatic melanoma patients receiving ipilimumab. Ann Oncol. 2016;27:732–738. doi: 10.1093/annonc/mdw016. [DOI] [PubMed] [Google Scholar]
- 22.Diem S, Kasenda B, Spain L, et al. Serum lactate dehydrogenase as an early marker for outcome in patients treated with anti-PD-1 therapy in metastatic melanoma. Br J Cancer. 2016;114:256–261. doi: 10.1038/bjc.2015.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu YC, Yao X, Crystal JS, et al. Efficient identification of mutated cancer antigens recognized by T cells associated with durable tumor regressions. Clin Cancer Res. 2014;20:3401–3410. doi: 10.1158/1078-0432.CCR-14-0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Robbins PF, Lu YC, El-Gamil M, et al. Mining exomic sequencing data to identify mutated antigens recognized by adoptively transferred tumor-reactive T cells. Nat Med. 2013;19:747–752. doi: 10.1038/nm.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gros A, Robbins PF, Yao X, et al. PD-1 identifies the patient-specific CD8⁺ tumor-reactive repertoire infiltrating human tumors. J Clin Invest. 2014;124:2246–2259. doi: 10.1172/JCI73639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tran E, Turcotte S, Gros A, et al. Cancer immunotherapy based on mutation-specific CD4+ T cells in a patient with epithelial cancer. Science. 2014;344:641–645. doi: 10.1126/science.1251102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33:1889–1894. doi: 10.1200/JCO.2014.56.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti-PD-1) in melanoma. N Engl J Med. 2013;369:134–144. doi: 10.1056/NEJMoa1305133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Topalian SL, Hodi FS, Brahmer JR, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366:2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): A randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16:375–384. doi: 10.1016/S1470-2045(15)70076-8. [DOI] [PubMed] [Google Scholar]
- 32.Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med. 2015;372:320–330. doi: 10.1056/NEJMoa1412082. [DOI] [PubMed] [Google Scholar]
- 33.Robert C, Ribas A, Wolchok JD, et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: A randomised dose-comparison cohort of a phase 1 trial. Lancet. 2014;384:1109–1117. doi: 10.1016/S0140-6736(14)60958-2. [DOI] [PubMed] [Google Scholar]
- 34.Robert C, Schachter J, Long GV, et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med. 2015;372:2521–2532. doi: 10.1056/NEJMoa1503093. [DOI] [PubMed] [Google Scholar]
- 35.Larkin J, Chiarion-Sileni V, Gonzalez R, et al. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N Engl J Med. 2015;373:23–34. doi: 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.