Abstract
Facial paralysis is one of the common problem leading to facial deformation. Bell's palsy (BP) is defined as a lower motor neuron palsy of acute onset and idiopathic origin. BP is regarded as a benign common neurological disorder of unknown cause. It has an acute onset and is almost always a mononeuritis. The facial nerve is a mixed cranial nerve with a predominant motor component, which supplies all muscles concerned with unilateral facial expression. Knowledge of its course is vital for anatomic localization and clinical correlation. BP accounts for approximately 72% of facial palsies. Almost a century later, the management and etiology of BP is still a subject of controversy. Here, we present a review of literature on this neurologically significant entity.
Keywords: Bell's palsy, corticosteroids, facial palsy, neurological disorder
Introduction
Facial paralysis is a disfiguring disorder that has a considerable impact on the patient because it results in the loss of facial expression; it is most commonly caused by a benign self-limiting inflammatory condition known as Bell's palsy (BP).[1] BP is one of the most common neurologic disorders affecting the cranial nerves, and is the most common cause of facial paralysis worldwide. It is thought to account for approximately 60–75% cases of acute unilateral facial paralysis. It is an idiopathic, acute peripheral-nerve palsy involving the facial nerve, which supplies all the muscles of facial expression. The facial nerve also contains parasympathetic fibers to the lacrimal and salivary glands, as well as limited sensory fibers supplying taste to the anterior two-thirds of the tongue.[2]
Historical Aspect
It was first reported by Nicolas A Friedrich two century ago in 1798. BP is named after Sir Charles Bell (1774–1842), who was a Scottish anatomist and Edinburgh graduate. He first described the syndrome along with the anatomy and function of the facial nerve in a lecture “On the nerves: Giving an account of some experiments on their structure and functions, which lead to a new arrangement of the system” to the Royal Society of London in 1821.[3]
Epidemiology
The annual incidence of BP is 15 to 30 per 100,000 persons, with equal numbers of men and women affected. There is no predilection for either side of the face. BP has been described in patients of all ages, with peak incidence noted in the 40s. It occurs more commonly in patients with diabetes and in pregnant women. Patients who have had one episode of BP have an 8% risk of recurrence.[4,5]
Etiology and Pathogenesis
Controversy surrounds the etiology and treatment of BP.[6] The causes of the paresis still remain unknown even if the viral etiology has been discussed by several authors. Herpes viruses seemed to be the most plausible infective agent, determining inflammation and swelling of the nerve with subsequent blockage of the neural activity.[7,8] The natural history of BP is encouraging for the patients because a total recovery of facial function is expected in 70–85% of the patients, and a higher percentage of recovery is achieved if corticosteroid therapy is administered,[9,10] and early physical rehabilitation is performed in severe grades of paresis.[11] The causes include microcirculatory failure of the vasonervorum, viral infection, ischemic neuropathy, autoimmune reactions, surgical procedures such as local anesthesia, tooth extraction, infections, osteotomies, preprosthethic procedures, excision of tumors or cysts, surgery of temporomandibular joint, and surgical treatment of facial fractures and cleft lip/palate.[12]
The literature also reports three mechanisms in which a dental procedure could damage a nervous structure, that are, direct trauma to nerve from a needle, intraneural hematoma formation or compression, and local anesthetic toxicity. Direct trauma seems unlikely because many patients report experiencing trauma to the nerve when they feel the electric shock sensation on injection of the needle. However, virtually, all these symptoms resolve completely with no residual nerve damage.[13]
Clinical Features
Facial paralyses are divided into two types, namely, supranuclear and infranuclear system. The neurones supplying the lower face receive upper motor neurones (UMN) from the contralateral motor cortex, whereas the neurones to the upper face receive bilateral UMN innervation. An UMN lesion, therefore, causes unilateral facial palsy with some sparing of the frontalis and orbicularis oculi muscles because of the bilateral cortical representation. Furthermore, although voluntary facial movements are impaired, the face may still move with emotional responses, for example on laughing. Paresis of the ipsilateral arm (monoparesis) or arm and leg (hemiparesis), or dysphasia may be associated because of more extensive cerebrocortical damage.
Lower motor neurone (LMN) facial palsy is characterized by unilateral paralysis of all muscles of facial expression for both voluntary and emotional responses. The forehead is unfurrowed and the patient is unable to close the eye on that side. Attempted closure causes the eye to roll upwards (Bell's sign). Tears tend to overflow on to the cheek (epiphora), the corner of the mouth droops, and the nasolabial fold is obliterated. Saliva may dribble from the commissure and may cause angular stomatitis. Food collects in the vestibule and plaque accumulates on the teeth on the affected side. Depending on the site of the lesion, other defects such as loss of taste or hyperacusis may be associated.[14]
Differential Diagnosis
Many conditions can produce isolated facial nerve palsy identical to BP. Structural lesions in the ear or parotid gland (e.g., cholesteatoma, salivary tumors) can produce facial nerve compression and paralysis. Other causes of peripheral nerve palsies include Guillain–Barré syndrome, Lyme disease, otitis media, Ramsay Hunt syndrome (an outbreak of herpes zoster in the facial nerve distribution), sarcoidosis, and some influenza vaccines. Although these conditions can present as isolated facial nerve palsies, they usually have additional features that distinguish them from BP. Patients with Lyme disease often have a history of tick exposure, rash, or arthralgias. Facial nerve palsies from acute and chronic otitis media have a more gradual onset, with accompanying ear pain and fever. Patients with Ramsay Hunt syndrome have a pronounced prodrome of pain and often develop a vesicular eruption in the ear canal and pharynx, although cases without the vesicular eruption (i.e., zoster sine herpete) have been reported. Polyneuropathies (e.g., Guillain–Barré syndrome, sarcoidosis) more often affect both facial nerves. Tumors present with a more insidious onset of symptoms over weeks or months. Central nervous system lesions (e.g., multiple sclerosis, stroke, tumor) can also cause facial nerve palsy. However, some motor neurons to the forehead cross sides at the level of the brainstem, and hence, the fibers in the facial nerve going to the forehead come from both cerebral hemispheres. Supranuclear (central) lesions affecting the facial nerve do not paralyze the forehead on the affected side, resulting in a unilateral facial paralysis with forehead sparing. Often, there is at least some weakness of extremities on the affected side as well. Influenza vaccines in the past have been associated with peripheral neuropathies.[4,15,16,17]
Diagnostic Evaluation
Determining whether facial nerve paralysis is peripheral or central is a key step in the diagnosis. In facial palsy, facial weakness is demonstrated by asking the patient to:
Close the eyes against resistance
Raise the eyebrows
Raise the lips to show the teeth
Try to whistle.
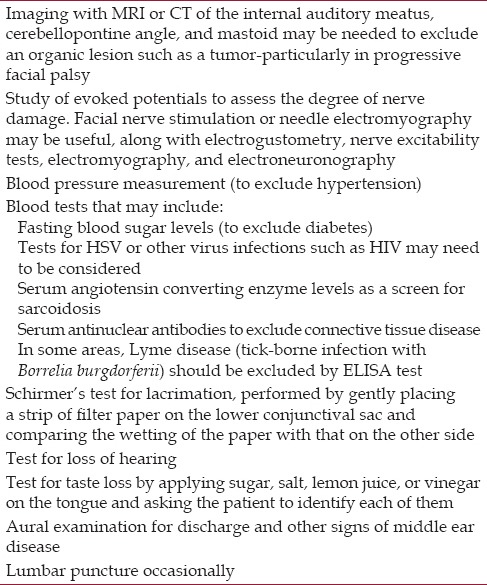
Full neurological examination is needed, looking particularly for signs suggesting a central lesion, such as hemiparesis, tremor, loss of balance, involvement of the Vth, VIth, or VIIIth cranial nerves. The following investigations may be indicated [Table 1].
Table 1.
Investigations required to rule out the diagnosis of facial palsy
Management and Prognosis
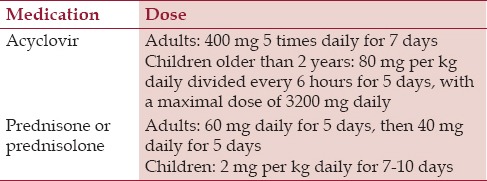
Treatment of BP should be conservative and guided by the severity and probable prognosis in each particular case. Studies have shown the benefit of high dose corticosteroids for acute BP. Although antiviral treatment has been used in recent years, evidence is now available indicating that it may not be useful.[18,19,20,21,22] Because of acyclovir's relatively poor bioavailability (15 to 30%), newer drugs in its class are being trialed. Better bioavailability, dosing regimens, and clinical effectiveness in treating shingles have been shown with valaciclovir (prodrug of aciclovir), famciclovir (prodrug of penciclovir), and sorivudine. A recent study showed a significantly better outcome in patients with BP treated with valacyclovir and prednisone as compared with patients who were given no medical treatment [Table 2]. If presentation is early, most clinicians give prednisolone for 5 days, the aim being to reduce neuronal edema. Most recent studies, therefore, advocate prednisolone as the predominant medical treatment, especially if begun within the first 72 hours; it is less effective after 7 days. It has been shown to improve the primary outcome, i.e., recovery of facial function, as rated on the House–Brackmann scale, and secondary outcomes such as the quality of life, appearance, and pain.[10,22,23,24]
Table 2.
Medicinal treatment
Additional measures include eye protection, physiotherapy, acupuncture, botulinum toxin, or possibly surgery. An eye patch is of value to protect the cornea. Topical ocular therapy is useful in most cases, with the exception of those in which the condition is severe or prolonged. In these cases, surgical management is best. Surgical techniques [Table 3] aimed at improving function and cosmetics include nerve repair, graft, or transposition. Attachment of the distal end of the affected facial nerve to another afferent cranial nerve trunk, for example, the contralateral facial nerve, or a hypoglossal jump graft was a part of nerve transposition. This technique must be undertaken within 2 years of paralysis. Several procedures are aimed at protecting the cornea from exposure and achieving facial symmetry. These procedures reduce the need for constant use of lubrication drops or ointments, may improve cosmesis, and may be needed to preserve vision on the affected side. These include the occlusion of eyelids with tape or patch in case of corneal erosions;[25] external eyelid weights to improve mechanical blink; injection of hyaluronic acid gel in the prelevator aponeurosis region and/or pretarsal region in patients who are poor surgical candidates and/or as a temporary measure;[26] tarsorraphy with suture or cynoacylate glue as a temporary/permanent measure;[27] taping to prevent lower lid ectropion, botulinum toxin injected at upper border of taisus to produce temporary ptosis, and Botulinum toxin[28] for synkinetic eyelid movements secondary to aberrant regeneration in which there are eye movements such as blinking associated with oral movements.[29,30] Several physical therapies, including massage and facial exercises, are recommended to patients, however, there are few controlled clinical trials reporting their effectiveness. Some recent evidence supports facial retraining (mime therapy) with biofeedback. Prognosis of BP is fair with complete recovery in approximately 80% of the cases, 15% experience some kind of permanent nerve damage and 5% remain with severe sequelae.[31]
Table 3.
Surgical procedure
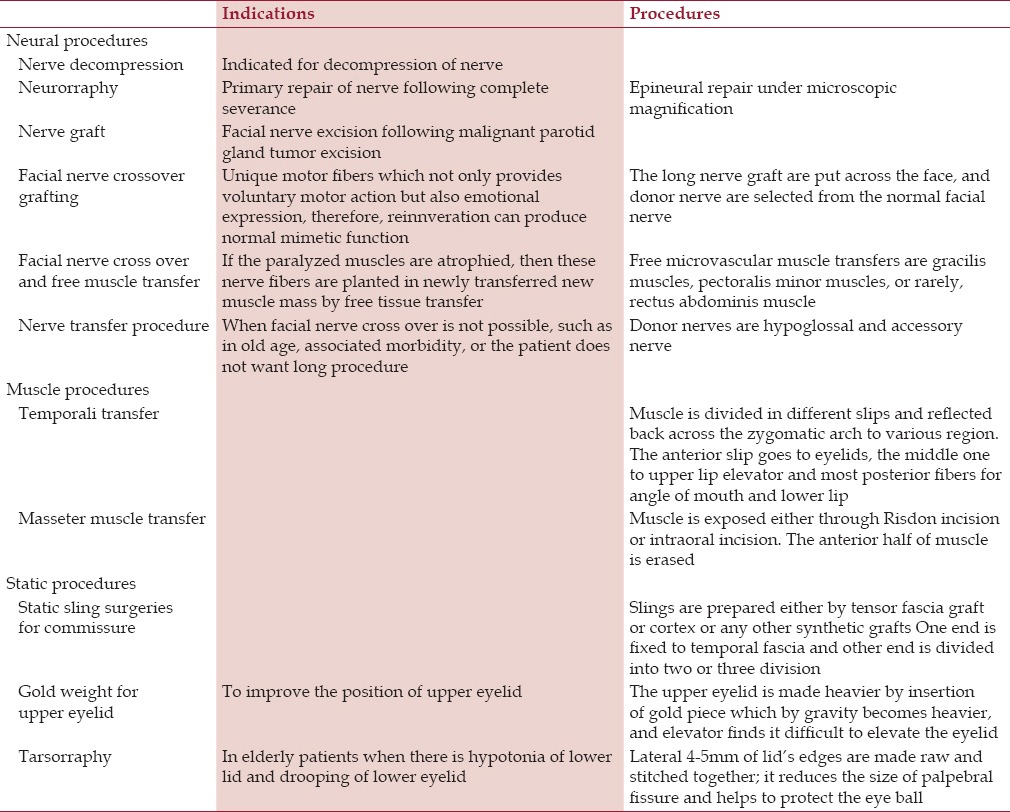
A multidisciplinary team approach (general practitioners, otolaryngologists, ophthalmologists, plastic surgeons, dental surgeons, physiotherapists, and psychologists) is essential when there is no prospect of further recovery of facial nerve function. Facial reanimation may be possible by a combination of static and dynamic surgical techniques and may result in functional as well as cosmetic improvements.[32,33] The most common complication of surgery is postoperative hearing loss, which affects 3–15% of patients. Based on the significant potential for harms and the paucity of data supporting benefit, the American Academy of Neurology does not currently recommend surgical decompression for BP.[34]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The Author would like to thank to Dr. Rohan Newadkar, for the guidance and support.
References
- 1.Chan EH, Tan HM, Tan TY. Facial Palsy from temporal bone lesions. Ann Acad Med Singapore. 2005;34:322–9. [PubMed] [Google Scholar]
- 2.Katusic SK, Beard CM, Wiederholt WC, Bergstralh EJ, Kurland LT. Incidence, clinical features, and prognosis in Bell's palsy, Rochester, Minnesota 1968-1982. Ann Neurol. 1986;20:622–7. doi: 10.1002/ana.410200511. [DOI] [PubMed] [Google Scholar]
- 3.Friedrich NA. De paralysis musculorum facier rheumatica. J Erfindungen (Gotha) 1798;8:25. [Google Scholar]
- 4.Gilden DH. Clinical practice. Bell's palsy. N Engl J Med. 2004;351:1323–31. doi: 10.1056/NEJMcp041120. [DOI] [PubMed] [Google Scholar]
- 5.Morris AM, Deeks SL, Hill MD, Midroni G, Goldstein WC, Mazzulli T, et al. Annualized incidence and spectrum of illness from an outbreak investigation of Bell's palsy. Neuroepidemiology. 2002;21:255–61. doi: 10.1159/000065645. [DOI] [PubMed] [Google Scholar]
- 6.Doshi D, Saab M. Bell's palsy in children: Is there any role of steroid or acyclovir? Hong Kong J Emerg Med. 2007;14:233–6. [Google Scholar]
- 7.Hato N, Kohno H, Yamada H, Takahashi H, Gyo K. Role of nitric oxide in the onset of facial nerve palsy by HSV-1 infection. JAMA Otolaryngology Head Neck Surg. 2013;139:1339–42. doi: 10.1001/jamaoto.2013.5542. [DOI] [PubMed] [Google Scholar]
- 8.Turriziani O, Falasca F, Maida P, Gaeta A, De Vito C, Mancini P, et al. Early collection of saliva specimens from Bell's palsy patients: Quantitative analysis of HHV-6, HSV-1, and VZV. J Med Virol. 2014;86:1752–8. doi: 10.1002/jmv.23917. [DOI] [PubMed] [Google Scholar]
- 9.Engström M, Berg T, Stjernquist-Desatnik A, Axelsson S, Pitkäranta A, Hultcrantz M, et al. Prednisolone and valaciclovir in Bell's palsy: A randomised, doubleblind, placebo-controlled, multicentre trial. Lancet Neurol. 2008;7:993–1000. doi: 10.1016/S1474-4422(08)70221-7. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan FM, Swan IR, Donnan PT, Morrison JM, Smith BH, McKinstry B, et al. Early treatment with prednisolone or acyclovir in Bell's palsy. N Eng J Med. 2007;357:1598–607. doi: 10.1056/NEJMoa072006. [DOI] [PubMed] [Google Scholar]
- 11.Nicastri M, Mancini P, De Seta D, Bertoli G, Prosperini L, Toni D, et al. Efficacy of early physical therapy in severe Bell's palsy: A randomized controlled trial. Neurorehabil Neural Repair. 2013;27:542–51. doi: 10.1177/1545968313481280. [DOI] [PubMed] [Google Scholar]
- 12.Garg KN, Gupta K, Singh S, Chaudhary S. Bell's palsy: Aetiology, classification, differential diagnosis and treatment consideration: A review. J Dentofacial Sci. 2012;1:1–8. [Google Scholar]
- 13.Vasconcelos BC, Bessa-Nogueira RV, Maurette PE, Aguiar Carneiro SC. Facial nerve paralysis after impacted lower third molar surgery: A literature review and case report. Med Oral Patol Oral Cir Bucal. 2006;11:E175–8. [PubMed] [Google Scholar]
- 14.Scully C, Felix DH. Oral Medicine-Update for the dental practitioner Disorders of orofacial sensation and movement. Br Dent J. 2005;199:703–9. doi: 10.1038/sj.bdj.4812966. [DOI] [PubMed] [Google Scholar]
- 15.Makeham TP, Croxson GR, Coulson S. Infective causes of facial nerve paralysis. Otol Neurotol. 2007;28:100–3. doi: 10.1097/01.mao.0000232009.01116.3f. [DOI] [PubMed] [Google Scholar]
- 16.Redaelli de Zinis LO, Gamba P, Balzanelli C. Acute otitis media and facial nerve paralysis in adults. Otol Neurotol. 2003;24:113–7. doi: 10.1097/00129492-200301000-00022. [DOI] [PubMed] [Google Scholar]
- 17.Keane JR. Bilateral seventh nerve palsy: Analysis of 43 cases and review of the literature. Neurology. 1994;44:1198–202. doi: 10.1212/wnl.44.7.1198. [DOI] [PubMed] [Google Scholar]
- 18.Numthavaj P, Thakkinstian A, Dejthevaporn C, Attia J. Corticosteroid and antiviral therapy for Bell's palsy: A network meta-analysis. BMC Neurol. 2011;5:1. doi: 10.1186/1471-2377-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quant EC, Jeste SS, Muni RH Cape AV, Bhussar MK, Peleg AY. The benefits of steroids versus steroids plus antivirals for treatment of Bell's palsy: A meta-analysis. BMJ. 2009;7:b3354. doi: 10.1136/bmj.b3354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lockhart P, Daly F, Pitkethly M, Comerford N, Sullivan F. Antiviral treatment for Bell's palsy (Idiopathic facial paralysis) Cochrane Database Syst Rev. 2009;7:CD001869. doi: 10.1002/14651858.CD001869.pub4. [DOI] [PubMed] [Google Scholar]
- 21.Yeo SG, Lee YC, Park DC, Cha CI. Acyclovir plus steroid vs steroid alone in the treatment of Bell's palsy. Am J Otolaryngol. 2008;29:163–6. doi: 10.1016/j.amjoto.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 22.Tiemstra JD, Khatkhate N. Bell's palsy: Diagnosis and management. Am Fam Physician. 2007;76:997–1002. [PubMed] [Google Scholar]
- 23.Salinas R, Alavarez G, Ferreira J. Corticosteroids for Bell's Palsy (Idiopathic facial paralysis) Cochrane database Syst Rev. 2004;18:CD001942. doi: 10.1002/14651858.CD001942.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Salinas RA, Alavarez G, Daly F, Ferreira J. Corticosteroids for Bell's Palsy. (Idiopathic facial paralysis) Cochrane database Syst. Rev. 2010;17:CD 001942. doi: 10.1002/14651858.CD001942.pub4. [DOI] [PubMed] [Google Scholar]
- 25.Seiff SR, Boerner M, Carter SR. Treatment of facial palsies with external eyelids weights. Am J Ophthalmol. 1995;120:652–7. doi: 10.1016/s0002-9394(14)72212-3. [DOI] [PubMed] [Google Scholar]
- 26.Mancini R, Taban M, Lowinger A, Nakra T, Tsirbas A, Dougles RS, et al. Use of hylauronic acid gel in the management of paralytic lagophthalmos: The hyaluronic Acid gel “gold weight”. Ophthal Plast Reconstr Surg. 2009;25:23–6. doi: 10.1097/IOP.0b013e318192568d. [DOI] [PubMed] [Google Scholar]
- 27.Donnenfeld ED, Perry HD, Nelson DB. Cynoacylate temporary tarsorrhaphy in the management of corneal epithelial defects. Ophthalmic Surg. 1991;22:591–3. [PubMed] [Google Scholar]
- 28.Ellis MF, Daniell M. An evaluation of the safety and efficacy of botulinum toxin type A (BOTOX) when used to produce a protective ptosis. Clin Experiment Ophthalmol. 2001;29:394–9. doi: 10.1046/j.1442-9071.2001.d01-28.x. [DOI] [PubMed] [Google Scholar]
- 29.Chen C, Malhotra R, Muecke J, Davis G, Selva D. Abberrant facial nerve regeneration (AFR): An under recognized cause of ptosis. Eye. 2004;18:159–62. doi: 10.1038/sj.eye.6700599. [DOI] [PubMed] [Google Scholar]
- 30.Chua CN, Quhill F, Jones E, Voon LW, Ahad M, Rowson N. Treatment of abberrant facial nerve regeneration with botulinum toxin A. Orbit. 2004;23:213–8. doi: 10.1080/01676830490512233. [DOI] [PubMed] [Google Scholar]
- 31.Tate JR, Tollefson TT. Advances in facial reanimation. Curr Opin Otolaryngol Head Neck Surg. 2006;14:242–8. doi: 10.1097/01.moo.0000233594.84175.a0. [DOI] [PubMed] [Google Scholar]
- 32.Horlock N, Sanders R, Harrison DH. The SOOF lift: Its role in correcting midfacial and lower facial asymmetry in patients with partial facial palsy. Plast Reconstr Surg. 2002;109:839–49. doi: 10.1097/00006534-200203000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Mackinnon SE. New directions in peripheral nerve surgery. Ann Plast Surg. 1989;22:257–73. doi: 10.1097/00000637-198903000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Grogan PM, Gronseth GS. Practice parameter: Steroids, acyclovir, and surgery for Bell's palsy (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56:830–6. doi: 10.1212/wnl.56.7.830. [DOI] [PubMed] [Google Scholar]


