Abstract
Objectives:
The cardiovascular system may represent a significant pathway by which marriage and stress influence health, but research has focused on married individuals cross-sectionally. This study examined associations among chronic stress, negative spousal relationship quality, and systolic blood pressure over time among middle-aged and older husbands and wives.
Method:
Participants were from the nationally representative longitudinal Health and Retirement Study. A total of 1,356 (N = 2,712) married and cohabitating couples completed psychosocial and biomeasure assessments in waves 2006 and 2010. Analyses examined whether Wave 1 (2006) relationship quality and stress were associated with changes in blood pressure over time.
Results:
The effects of stress and negative relationship quality were dyadic and varied by gender. Husbands had increased blood pressure when wives reported greater stress, and this link was exacerbated by negative spousal relationship quality. Negative relationship quality predicted increased blood pressure when both members of the couple reported negative quality relations.
Discussion:
Findings support the dyadic biopsychosocial model of marriage and health indicating: (a) stress and relationship quality directly effect the cardiovascular system, (b) relationship quality moderates the effect of stress, and (c) the dyad rather than only the individual should be considered when examining marriage and health.
Keywords: Blood pressure, Couples, Marriage, Middle age, Older adults, Stress
Stress, especially when chronic, has lasting and detrimental implications for health and well-being (Juster, McEwen, & Lupien, 2010; Thoits, 2010). Marriage provides an important context for understanding how stress influences health in middle and old age. How couples experience and manage stress together is key for understanding variations in the implications of stress (Berg & Upchurch, 2007). Indeed, individuals are influenced not only by their own stress levels but also those of their partners (Neff & Karney, 2007).
The research on stress in marriage suggests that stress is particularly harmful among couples who have conflictual or negative relationships (Neff & Karney, 2007). In addition, negative aspects of social ties tend to be more highly associated with health, well-being, and marital longevity than the positive aspects of relationships (Bookwala, 2005; Kiecolt-Glaser & Newton, 2001). However, the available evidence is mixed with respect to the effects of negative marital quality on the stress–health link (Antonucci, Birditt, & Webster, 2010; Birditt & Antonucci, 2008). Recent studies of married individuals showed that stress and negative marital quality interact to influence mortality and blood pressure, but studies have yet to address these links among married couples over time (Birditt & Antonucci, 2008; Birditt, Newton, & Hope, 2012).
This study aims to resolve these gaps in knowledge by exploring more deeply the longitudinal associations between chronic stress, negative relationship quality, and systolic blood pressure among husbands and wives. This study focuses on blood pressure as the cardiovascular system is considered a key pathway by which relationships “get under the skin” (Uchino, 2009). First, we examine the direct associations between chronic stress, negative relationship quality, and systolic blood pressure among husbands and wives; second, we assess whether the link between stress and systolic blood pressure is moderated by negative relationship quality among husbands and wives. Hypotheses are tested using dyadic data from a large national sample of middle-aged and older couples.
Theoretical Framework
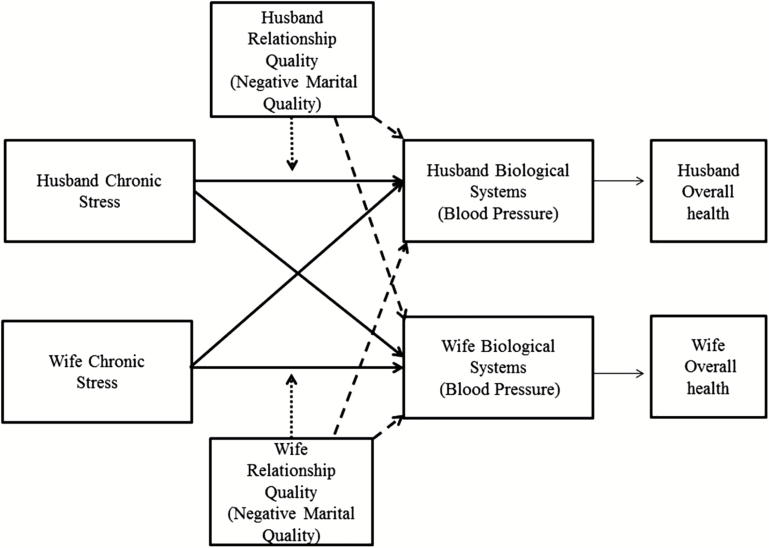
This study draws on the Dyadic Biopsychosocial Model of Marriage and Health (Birditt et al., 2012), which incorporates three approaches: the direct approach, the moderating approach, and biopsychosocial theory (Lindau, Laumann, Levinson, & Waite, 2003; see Figure 1). This model provides an integrative theory for understanding the marriage/health association among couples, and suggests that, consistent with direct effect theories of relationships and health (House, Landis, & Umberson, 1988; Seeman, 1996), greater negative spousal quality predicts higher blood pressure. In addition, the model incorporates the moderating effect approach of social relationships, which suggests that spousal/partner relationships are particularly influential under stressful life circumstances (Cohen & Wills, 1985). Thus, the model holds that highly negative relationships will exacerbate stress or enhance negative reactions to it (August, Rook, & Newsom, 2007). Finally, the model incorporates the biopsychosocial approach to health, which indicates that social and psychological factors (e.g., relationship quality and stress, respectively) influence overall health via biological pathways or mechanisms (Lindau et al., 2003; Seeman, 1996). The cardiovascular system is a key biological pathway that accounts for associations between marital/partner quality, stress, and health (Uchino, 2009) and is particularly important to examine in older adults, given that heart disease is the leading cause of death among this population (Delgado, Jacobs, Lackland, Evans, & de Leon, 2012).
Figure 1.
Dyadic biopsychosocial model of marriage and health. Note. Solid lines test direct effects of stress, dashed lines test direct effects of relationship quality, and dotted lines test the moderating role of negative relationship quality.
Chronic Stress and Blood Pressure Among Married Couples
This study focuses on chronic rather than acute stress because stress that is long-lasting tends to be more damaging to health (Juster et al., 2010; Thoits, 2010). Chronic stress is defined as an ongoing circumstance occurring for a year or longer that threatens to overwhelm an individual’s resources. Typical chronic stressors include ongoing financial problems, problems at work, or long-term caregiving.
A great deal of research has established that chronic stress is associated with increased blood pressure and heart problems (Hawkley, Masi, Berry, & Cacioppo, 2006; Steptoe et al., 2003). Studies typically examine links between stress and health within individuals; however, stress is often dyadic. Individuals are influenced not only by their own stress but the stresses experienced by their marital partner (Neff & Karney, 2007). For example, Monin and colleagues (2010) found that greater spousal partner stress predicted greater blood pressure among caregivers. However, it is unclear whether these findings apply when examining marital dyads among the general population.
Husbands and wives may be differentially affected by stress. For example, some studies have shown that wives are more affected by husbands’ stress than the reverse (Katz, Monnier, Libert, Shaw, & Beach, 2000; Rook, Dooley, & Catalano, 1991). However, other studies show that husbands may be more affected by wives’ stress. For instance, in a study of newlyweds over the first 3.5 years of marriage, Neff and Karney (2007) found that husbands reported lower marital satisfaction when wives reported greater stress, but there was no such association for wives. This study assesses whether an individual’s systolic blood pressure is influenced by their own as well as their partner’s reports of chronic stress and whether there are gender differences in these patterns.
Negative Relationship Quality and Blood Pressure Among Married Couples
Married couples are not only influenced by the external stresses experienced in their lives but stresses that are internal to the marriage. Negative aspects of the marital relationship (e.g., negative or hostile behaviors; overall strain) are linked with increased cardiovascular activity (Kiecolt-Glaser & Newton, 2001; Robles & Kiecolt-Glaser, 2003), poorer self-rated health, and greater functional limitations (Ryan, Wan, & Smith, 2014). In a meta-analysis assessing the relationship between marital quality and health, Robles, Slatcher, Trombello, and McGinn (2013) found that marital dissatisfaction was consistently related to structural indicators of cardiovascular disease as well as functional indicators, including blood pressure.
Interestingly, researchers still debate whether there are gender differences in the negative relationship quality/health link, often finding that women are more physiologically reactive than men to marital conflict (Kiecolt-Glaser & Newton, 2001; Whisman, Uebelacker, & Settles, 2010). However, more recent research indicates that there are few gender differences in the link between marital relationship quality and physical health (Robles et al., 2013). To date, the majority of research has assessed gender differences between rather than within couples. A dyadic approach could help resolve the question of gender differences in the negative relationship quality/health link.
Moderating Effect of Negative Marital Quality on the Stress–Blood Pressure Link
Couples who report more negative relationships may be more detrimentally affected by stress. In research on the stress–marital satisfaction link, Neff and Karney (2007) found exacerbating effects of negative relationship quality on the stress–marital satisfaction link. However, Birditt and Antonucci (2008) found that the link between life-threatening illness and mortality was reduced among individuals who reported that their spouses were demanding or critical. Similarly, Birditt and colleagues (2012) found negative associations between stress and blood pressure among people reporting greater demands from their spouse or partner. In contrast, Antonucci and colleagues (2010) found no exacerbating (or buffering) effects for negative spousal relationship quality in the association between chronic illness and mortality. These findings add to the growing body of mixed results concerning the moderating effects of negative relationship quality on the effects of stress and highlight the importance of using dyadic data to test hypotheses about phenomena that may be dyadic in nature.
The majority of studies on the marriage/health link has examined married individuals rather than couples, and it is unclear how husbands’ and wives’ perceptions of negative relationship quality differentially affect the stress–health link. Research using a dyadic approach to test the link between stress and marital satisfaction showed that wives’ stress was more highly associated with husbands’ lower marital satisfaction when couples used poor conflict resolution strategies (Neff & Karney, 2007). Further new research revealed that husbands who reported better quality marriages reported higher life satisfaction when wives also reported higher marital satisfaction (Carr, Freedman, Cornman, & Schwarz, 2014), but there were no such effects for wives, again suggesting the utility of testing for dyadic effects.
This Study
Previous research has found links between stress, negative marital quality, and blood pressure among married individuals, but it is not clear how these links vary between husbands and wives in the same couple, and whether these links exist over time. This study, therefore, uses a dyadic approach to examine links between husbands’ and wives’ perceptions of stress, negative relationship quality, and systolic blood pressure, and to test if the stress–blood pressure link varies by husbands’ and wives’ perceptions of negative relationship quality across two waves of data. We address two questions:
1. Are chronic stress and negative relationship quality reported in Wave 1 associated with systolic blood pressure within couples over time, and do these links vary by gender?
Based on previous research, we predict greater stress and negative relationship quality will be associated with higher blood pressure for wives and husbands, but because the research is inconclusive, we do not make predictions about potential gender differences.
2. Do perceptions of negative marital quality moderate the link between stress and systolic blood pressure within couples over time, and do these links vary by gender?
We predict that greater negative relationship quality will exacerbate the link between stress and blood pressure for wives and husbands. We do not make specific hypotheses about gender due to the conflicting findings in the literature.
Method
Participants
Participants were drawn from the Health and Retirement Study (HRS), a nationally representative multiwave longitudinal study of approximately 22,000 persons born in 1953 or earlier. The sample design involves interviewing individuals and their spouses or live-in partners every 2 years. Since 2006, data concerning social relationships, life circumstances, well-being, and biological indicators have been collected. This portion of the HRS interview is referred to as the enhanced face-to-face interview, and data are obtained biennially from 50% of the panel participants. The enhanced face-to-face interview includes a comprehensive battery of biomeasure assessments and a self-administered psychosocial questionnaire that includes questions about the spousal/partner relationship and chronic stress (Smith et al., 2013). This self-administered questionnaire was left with the respondents at the end of the face-to-face interview, and respondents were asked to complete and mail it back to the main field office at the University of Michigan. Because the enhanced face-to-face interview is conducted with 50% of the sample every 2 years, the 2010 wave provided the first longitudinal biological and psychosocial data from the 2006 participants. Thus, in this study, we included 2 waves of data: 2006 and 2010.
The response rate for the psychosocial questionnaire in 2006 was about 90%; considering the 90% response rate for the enhanced face-to-face interview, the overall response rate was then calculated at 74%. In 2010, individuals who completed the 2006 wave were contacted again, as well as a random 50% of the new cohort that entered the HRS. For this analysis, we focused on married or cohabiting couples who participated in 2006 and 2010. Individuals were removed from the present analytic sample if they were not married or cohabiting; only one member of a couple completed the survey; or they were a member of a same-sex couple.
Thus, 2,712 individuals (or 1,356 couples) were included in this study. Of selected participants, 97% were married and 3% were living with partners. Mean ages for husbands and wives were 66 (standard deviation [SD] = 8.8) and 63 years (SD = 9.2), respectively. A total of 91% were White and 7% were Black. Both husbands and wives had an average of 13 years of education. Couples were married an average of 36 years (SD = 15.3). Overall, the selected sample was healthier, younger, had more years of education, was more likely to be White, and reported less chronic stress than the total sample. A follow-up analysis revealed that all of these variations were most likely due to the fact that our selected sample was married or cohabitating.
Measures
Blood pressure
Blood pressure was assessed in Waves 1 (2006) and 2 (2010) with an Omron HEM-780 Intellisense automated blood pressure monitor with ComFit cuff, a validated instrument (Crimmins et al., 2008). Three measurements of blood pressure were taken 45 s apart on the respondent’s left arm after respondents were instructed to sit down with both feet on the floor, with their left arm comfortably supported (e.g., on a table) with the palm facing up. We focused on systolic pressure, which is the point of contraction representing peak pressure. The measurements were averaged to create an overall systolic score. An individual can be considered hypertensive if systolic pressure is greater than 140mm Hg (Williams, Pham-Kanter, & Leitsch, 2009).
Chronic stress
In Wave 1 (2006), participants completed seven items regarding chronic stressors (Troxel, Matthews, Bromberger, & Sutton-Tyrrell, 2003). Participants were asked whether any of the seven items were current and ongoing problems that had lasted 12 months or longer, and to indicate how upsetting they had been. Items included: physical or emotional problems (in spouse or child); problems with alcohol or drug use of family member; difficulties at work; financial strain; housing problems; problems in a close relationship; and helping at least one sick, limited, or frail family member or friend on a regular basis. For each item, participants received the following response choices: 1 = No, didn’t happen, 2 = Yes, but not upsetting, 3 = Yes, somewhat upsetting, and 4 = Yes, very upsetting. To create a measure of exposure to chronic stress, responses were recoded as 1 (Yes, the stressor happened: scores 2 through 4) or 0 (No, it did not happen) and summed to create separate stress scores for husbands and wives. Due to the positive skew in the distribution, scores were then truncated so that they ranged from 0 to 5 or more. The most frequent problems in Wave 1 included an ongoing health problem of spouse or child (38%), ongoing financial strain (31%), and helping at least one sick or disabled person (33%).
Negative spousal/partner relationship quality
In Wave 1 (2006), participants completed brief but widely used and valid items assessing the negative qualities of the spousal/partner relationship (Schuster, Kessler, & Aseltine, 1990; Walen & Lachman, 2000): How often does your spouse or partner make too many demands on you? How often does he or she criticize you? How often does he or she let you down when you are counting on them? and How often does he or she get on your nerves? Response options ranged from 1 (a lot) to 4 (not at all); all items were reverse-coded so that higher scores indicated higher negative relationship quality. We created negative relationship quality scores for both husband and wife in Wave 1 (husbands: α = .75, wives: α = .79).
Covariates
Years of education, years married, age, race, and blood pressure medication were included as covariates. Education, years married, and age were continuous variables. Race was coded as 1 (White) or 0 (not White), and hypertension medication was coded as 0 (not taking hypertension medication) or 1 (taking hypertension medication).
Analysis Strategy
First, descriptives were calculated and we examined whether there were differences between husbands and wives with paired t-tests. Research questions were addressed using Actor-Partner Interdependence Models (APIMs; Kenny, Kashy, & Cook, 2006) and estimated with multilevel modeling (SAS PROC MIXED). There are two parts to the relationship between predictor and outcome in APIM: the actor effect describes the unique effect of a person’s own predictor on his or her (the actor) own outcome, whereas the partner effect describes the unique effect of their partner’s predictor on the actor’s outcome. The multilevel models had 2 levels: Level 1 refers to individuals and Level 2 refers to the couple. All models controlled for Wave 1 blood pressure, education, years married, race, age, and blood pressure medicine. All continuous variables were grand mean-centered, and all categorical variables were effect-coded (−1, 1) before entering them in the models.
To answer the research questions, we estimated a series of four models. Model 1 examined whether blood pressure reported in Wave 2 varied by Wave 1 indicators of actor and partner chronic stress and Wave 1 actor and partner negative relationship quality. Model 2 included gender interactions to assess whether the effects of stress or negative relationship quality varied by gender. Model 3 included two-way interactions between Wave 1 stress and Wave 1 negative relationship quality to assess whether negative relationship quality moderated the stress–blood pressure link. Finally, Model 4 included three-way interactions among stress, negative relationship quality, and gender to assess whether the moderating role of negative relationship quality on the stress–blood pressure link varied by gender. We explored significant interactions with graphs and tests of simple slopes. We examined whether there was a significant difference between the fit of the models by subtracting the −2 log likelihood estimations of models and examining the difference on a chi-square distribution with degrees of freedom equaling the change in number of parameters (Singer & Willett, 2003). Because models need to be restricted to the same number of participants to test the model fit, we selected only participants with complete data on all predictors and covariates to estimate the multilevel models (N = 2,221). Findings were similar when using both the full sample and the restricted sample.
All data were weighted with the psychosocial weight, which incorporates the HRS respondent-level weight and a nonresponse adjustment factor (Smith et al., 2013). The nonresponse adjustment factor was obtained from a model predicting the likelihood of completing the leave-behind questionnaire as a function of demographics (e.g., age, sex, race/ethnicity), health (e.g., disease), and participant cooperativeness (e.g., completed prior wave). The inverse of the fitted probabilities of completion formed the nonresponse adjustment factor.
Results
Descriptives
Overall, husbands and wives reported low levels of chronic stress and negative relationship quality. There were also variations between husbands and wives in stress, negative relationship quality, and blood pressure. Wives reported greater chronic stress (mean [M] = 1.61) and greater negative spousal/partner quality (M = 1.94) compared with husbands (M = 1.44 [t = −3.69, p < .001] and M = 1.89 [t = −3.02, p < .01], respectively). Husbands had higher systolic blood pressure in 2006 (M = 132.21) and in 2010 (M = 133.93) compared with wives (M = 126.51 [t = 8.06, p < .001] and M = 128.60 [t = 7.18, p < .001], respectively). The within-couple correlations for reports of stress, negative relationship quality, and systolic blood pressure were .32 (p < .001), .38 (p < .001), and .13 in 2006 and .15 in 2010 (p < .001), respectively.
According to the American Heart Association guidelines for both systolic and diastolic blood pressure, 35% of husbands and 26% of wives had hypertension in Wave 1 and 37% of husbands and 30% of wives had hypertension in Wave 2. Husbands and wives reported using blood pressure medication with similar frequency, 49% and 46%, respectively. Paired t-tests revealed that systolic blood pressure increased over time among both husbands (t = 3.39, p < .001) and wives (t = 3.63, p < .001). We also examined correlations between stress, negative relationship quality, and blood pressure (Supplementary Table 1), and results showed that these variables were moderately correlated.
Does Chronic Stress Predict Blood Pressure?
We first assessed whether blood pressure at Wave 2 varied by actor and partner reports of chronic stress at Wave 1 (Table 1, Model 1). Counter to our hypothesis, there was a negative effect of actor stress on systolic blood pressure, such that greater stress predicted decreased blood pressure. There was no main effect of partner stress on blood pressure.
Table 1.
Multilevel Models Examining Blood Pressure as a Function of Chronic Stress, Negative Relationship Quality, and Gender
| Model 1: Direct effects of stress and NRQ | Model 2: Do direct effects vary by gender? | Model 3: Moderating role of negative quality on stress–BP link | Model 4: Does the moderating role vary by gender? | |
|---|---|---|---|---|
| Systolic BP, b | Systolic BP, b | Systolic BP, b | Systolic BP, b | |
| Actor stress | −.62* | −.62* | −.56* | −.55* |
| Partner stress | .44 | .34 | .25 | .20 |
| Actor × partner stress | −.00 | −.06 | .01 | .06 |
| Actor NRQ | −.07 | .22 | −.16 | −.22 |
| Partner NRQ | −.22 | −.64 | −.33 | −.48 |
| Actor × partner NRQ | 3.23*** | 3.40*** | 3.10** | 3.15** |
| Actor stress × actor NRQ | .05 | .39 | ||
| Actor stress × partner NRQ | −.73 | −.93 | ||
| Partner stress × actor NRQ | .25 | .30 | ||
| Partner stress × partner NRQ | 1.12* | .99* | ||
| Actor stress × gender | −.16 | −.08 | ||
| Partner stress × gender | .75** | .80** | ||
| Actor stress × partner stress × gender | .33* | |||
| Actor NRQ × gender | −.25 | −.30 | ||
| Partner NRQ × gender | .55 | .26 | ||
| Actor NRQ × partner NRQ × gender | −.13 | |||
| Actor stress × actor NRQ × gender | −.22 | |||
| Actor stress × partner NRQ × gender | .28 | |||
| Partner stress × actor NRQ × gender | 1.10* | |||
| Partner stress × partner NRQ × gender | −.39 | |||
| −2 Log likelihood | 17,680.0 | 17,662.7 | 17,669.8 | 17,652.5 |
| Change in likelihood | 20.4** | 17.3** | 10.2* | 17.3* |
Notes: BP = blood pressure; NRQ = negative relationship quality. Change in likelihood in Model 1 is based on comparison with a covariates-only model. Change in likelihood for Models 2 and 3 is change from Model 1. Change in likelihood of Model 4 is based on comparison with Model 3. To compare model fit across models, we restricted all four models to individuals with complete data on all predictors and covariates (N = 2,221).
*p < .05. **p < .01. ***p < .001.
Does the Association Between Chronic Stress and Blood Pressure Vary Between Husbands and Wives?
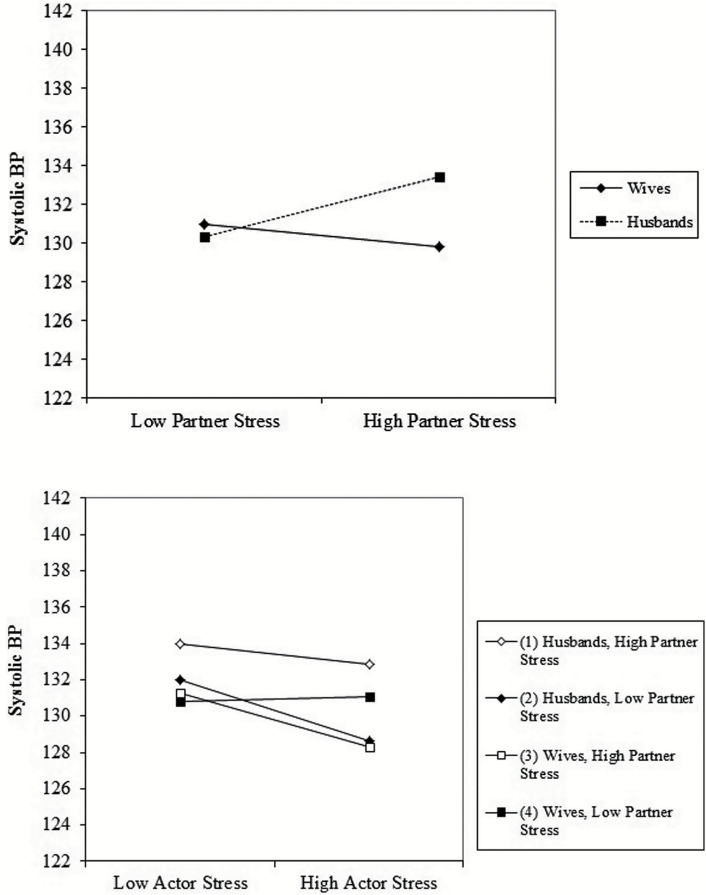
There was a significant interaction between partner reports of stress and gender when predicting systolic blood pressure (Table 1, Model 2; Figure 2a). An examination of the simple slope tests for the partner stress × gender interactions revealed that husbands had higher systolic blood pressure when their wives reported greater stress (b = 1.10, p < .01), but there was no effect for wives.
Figure 2.
(a) Effects of partner stress on blood pressure by gender. (b) Effects of actor stress on blood pressure by partner stress and gender.
There was also a significant three-way interaction among actor stress × partner stress × gender predicting systolic blood pressure (Figure 2b). Simple slopes analyses showed that husbands who reported greater stress had lower blood pressure when their wives reported lower stress (b = −1.17, p < .05), whereas wives who reported greater stress had lower blood pressure when their husband reported greater stress (b = −1.02, p < .05). Thus, husbands appeared to be more distressed by wives’ stress than the reverse. Interestingly, wives’ stress appeared to be buffered by greater stress among husbands.
Does Negative Relationship Quality Predict Blood Pressure?
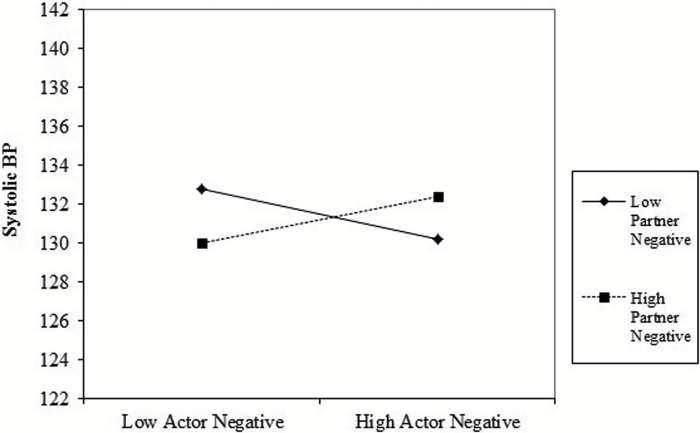
Inconsistent with our hypothesis, there were no main effects of negative spousal relationship quality of actor or partner on blood pressure. However, there was a significant two-way interaction between actor and partner reports of negative relationship quality when predicting systolic blood pressure (Table 1, Model 1, Figure 3). Simple slopes analyses showed that greater actor negative relationship quality was associated with higher blood pressure when partner negative relationship quality was higher (b = 1.93, p < .05) and lower blood pressure when partner negative relationship quality was lower (b = −2.08, p < .05). Thus, it appears that higher levels of negative relationship quality are only detrimental when both partners feel negative about the relationship.
Figure 3.
Effects of actor and partner negative relationship quality on blood pressure.
Does the Association Between Negative Relationship Quality and Blood Pressure Vary by Gender?
There were no significant interactions between negative relationship quality and gender, indicating that the associations between negative relationship quality and blood pressure were similar for husbands and wives. (Table 1).
Does Negative Marital Quality Moderate the Stress–Blood Pressure Link?
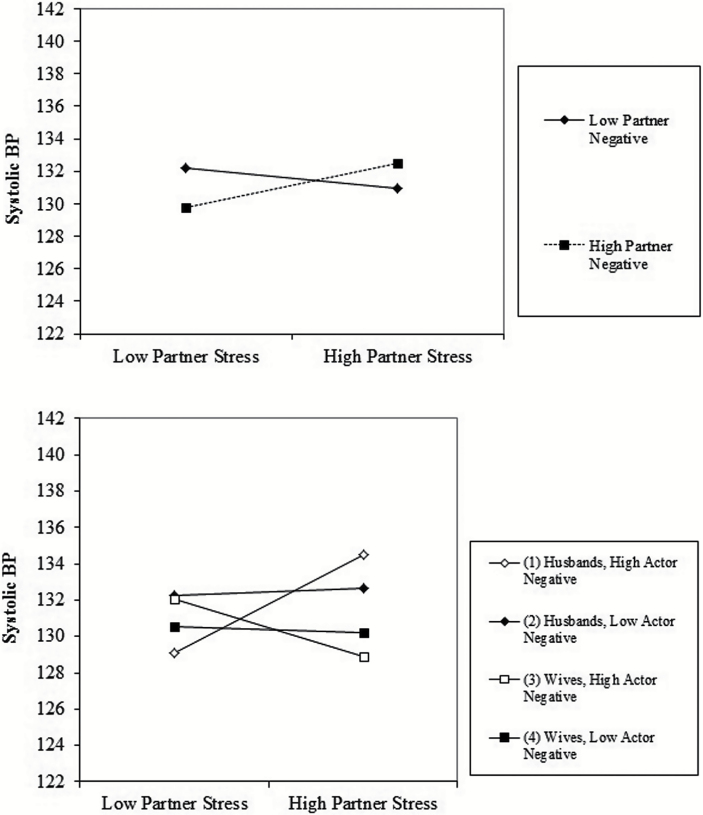
There was a statistically significant two-way interaction between partner stress and partner negative quality predicting systolic blood pressure (Table 1, Model 3; Figure 4a). An examination of the simple slopes revealed that, as predicted, partner stress was associated with increased blood pressure when partners reported higher levels of negative relationship quality (b = 0.95, p < .01). The slope was not significant for lower levels of negative relationship quality. Thus, it appears that negative relationship quality exacerbates the effects of stress.
Figure 4.
(a) Effects of partner stress on blood pressure by partner negative relationship quality. (b) Effects of partner stress on blood pressure by actor negative relationship quality and gender.
Does the Moderating Effect of Negative Marital Quality Differ for Wives and Husbands?
Finally, we estimated models that included three-way interactions between actor and partner stress, actor and partner negative relationship quality, and gender to assess whether the effects of actor and partner stress were moderated by actor and partner reports of negative relationship quality and gender (Table 1, Model 4 , Figure 4b). There was a statistically significant three-way interaction between partner stress, actor negative quality, and gender predicting systolic blood pressure. An examination of the simple slopes for the three-way interaction revealed that wives’ reports of stress predicted greater blood pressure among husbands when husbands reported greater negative relationship quality (b = 1.87, p < .01). Thus, husbands appeared to be more negatively affected by wives’ stress when they felt more negative about the relationship.
Discussion
The purpose of this study was to examine links among stress, relationship quality, and blood pressure over time among older couples. This study moved beyond the previous literature examining married individuals cross-sectionally, and considered whether the complex links among negative spousal relationship quality, stress, and blood pressure vary among husbands and wives in the same relationship over time. Findings support the dyadic biopsychosocial model of marriage and health, which suggests that: (a) stress and relationship quality have both direct and moderating effects on the cardiovascular system and (b) it is important to consider the dyad rather than only the individual when examining marriage and health. Most importantly, this study revealed that wives’ stress has important implications for husbands’ blood pressure, particularly in more negative relationships. In addition, the effects of negative relationship quality were truly dyadic in that there were no effects when examining individuals, but there were effects when examining interactions between both members of the dyad.
Effects of Chronic Stress on Blood Pressure Among Couples
The effects of stress on blood pressure were dyadic in nature and varied by gender. Husbands had higher blood pressure when wives reported greater stress. This finding is consistent with previous research regarding stress and marital satisfaction in which husbands reported lower marital satisfaction when wives reported greater stress (Neff & Karney, 2007). Husbands tend to rely on spouses for support, which may not be provided when wives are experiencing high levels of stress.
There was also evidence that the effects of individuals’ own experiences of stress on systolic blood pressure varied as a function of partner stress and gender. Husbands who reported greater stress had lower blood pressure when their wives reported lower stress, whereas wives who reported greater stress had lower blood pressure when their husbands reported greater stress. These complex findings indicate that husbands and wives may benefit from different dyadic patterns of stress. Women tend to provide more support to husbands than the reverse (Monin & Clark, 2000); husbands also tend to rely on their wives for support, whereas wives rely on their broader social networks for support. Women also prefer to discuss their relationships and stress with husbands, whereas husbands are more likely to withdraw (Holley, Haase, & Levenson, 2013), and “relationship talk” is more strongly linked to marital satisfaction among wives than husbands (Badr & Acitelli, 2005). Thus, husbands may have lower blood pressure when wives are less stressed because wives are better able to provide support in that circumstance, whereas wives may benefit when husbands are more stressed because they prefer to engage with husbands more openly about stress and relationships.
Effects of Negative Marital Quality on Blood Pressure Among Couples
Overall, we found that the association between negative relationship quality and blood pressure is also a dyadic phenomenon. Links between individual feelings of negative spousal relationship quality and blood pressure were either exacerbated or buffered by how partners felt about the relationship. When both partners reported higher levels of negative relationship quality, there were negative health effects. In contrast, spousal partners’ lack of negative feelings about the relationship appeared to buffer the detrimental effects of negative quality on blood pressure. Thus, it appears that the association between negative relationship and blood pressure is a dyadic phenomenon in which high levels of negative relationship quality are only detrimental when both partners feel negative about the relationship.
Interestingly, we found no gender differences in the links between negative relationship quality and blood pressure. This finding is consistent with a recent meta-analysis (Robles et al., 2013), which found few gender differences in the association between marital quality and health. This study moves beyond the previous literature by examining marital quality among marital dyads rather than married individuals. By doing so, we were able to show that negative spousal quality alone does not have negative health effects; it is the marital dyad that determines whether negative marital quality is detrimental.
Moderating Role of Negative Marital Quality on the Stress–Blood Pressure Link
This study showed that the partner stress–blood pressure link is exacerbated by negative spousal relationship quality. Partner stress was associated with higher blood pressure when partners reported greater negative relationship quality. It is possible that greater stress coupled with greater feelings of negativity about the relationship is communicated to the spouse via more negative or destructive strategies. This finding is inconsistent with previous studies, which showed that negative relationship quality can act as a buffer for the link between stress and blood pressure (e.g., Birditt et al., 2012). Although the previous research examined married individuals, this study showed that partners’ reports of stress and negative relationship quality interact to influence an individual’s blood pressure.
The link between partner stress and blood pressure was also moderated by actor perception of negative relationship quality, and this effect occurred only among husbands. Previous studies did not find gender differences in the links between stress, negative relationship quality, and blood pressure; again, however, those studies focused on married individuals rather than dyads. The link between wives’ stress and husbands’ blood pressure appeared to be exacerbated when husbands reported greater negative relationship quality. This is in consistent with behavioral observation research findings that women tend to be more physiologically reactive than men to marital conflict (Kiecolt-Glaser & Newton, 2001). These findings may be explained by role theory, which posits that men and women are socialized to behave according to particular roles: for men, being strong and competent; for women, the ability to nurture. According to Eagly and Wood (2013) these roles, in turn, are “internalized as personal standards for individuals’ behavior, thus facilitating self-regulatory behavior.” For example, men are expected to be stoic and regulate their emotions. Women, on the other hand, are expected to be expressive and emotionally labile (Grossman & Wood, 1993). Thus, husbands may react physiologically (e.g., with heightened blood pressure) in response to stress and negative marital quality, given their propensity to internalize their emotions (Rauer & Volling, 2005).
Limitations and Future Directions
This research has some limitations. Measurement of all constructs of interest—marital quality, stress, and blood pressure—could have been more thorough, a situation common to survey research. As an example, only four items assessed relationship quality. Thus, we lack information regarding the relationship processes that underlie the reports of relationship quality, leading to questions such as: how are spousal or partner feelings of being let down or getting on nerves expressed? We need to include more extensive measures of spousal/partner quality in future studies (e.g., conflict, coping strategies, and satisfaction with support), given that research—including this study—has revealed important dyadic effects of spousal relationship quality (Michalowski, Hoppmann, & Gerstorf, 2014). Further, the measurement of blood pressure did not include controls such as a specified rest time prior to measurement or prohibition of caffeinated beverages, which are often included in more controlled laboratory or clinical settings.
We may also be missing nuances in how couples assess marital quality by failing to include other individual difference variables, such as personality; for example, neuroticism or trait hostility (Li & Fung, 2012; Robles et al., 2013), which may in turn affect the attributions that spouses make for their partners’ behaviors, as well as the degree to which they disclose their emotions. Additionally, the mechanism linking these processes may also be best measured through the use of daily diaries and/or measuring cardiovascular function repeatedly over short periods of time.
This study highlights the often-complicated nature of spouse/partner relationship quality, stress, and their associations with biological pathways over time. These findings emphasize the importance of examining the influence of both marital partners on individual health, given that spouses are influenced by their partner’s feelings of stress and negative marital quality. Individual reports of stress or relationship quality provide an incomplete picture of the factors influencing blood pressure, and we hope that this study leads to more research examining dyadic models of marriage and physical health.
Supplementary Material
Please visit the article online at http://gerontologist.oxfordjournals.org/ to view supplementary material.
Funding
The Health and Retirement Study is sponsored by the National Institute on Aging (NIA U01AG009740) and is conducted by the University of Michigan.
Supplementary Material
Acknowledgments
We would like to thank Angela Turkelson for her assistance with the analyses. Previous versions of this project were presented at the Association for Psychological Science meeting in May 2014 and the Gerontological Society of America meeting in November 2014.
References
- Antonucci T. C., Birditt K. S., Webster N. J. (2010). Social relations and mortality: A more nuanced approach. Journal of Health Psychology, 15, 649–659. doi:10.1177/1359105310368189 [DOI] [PubMed] [Google Scholar]
- August K. J., Rook K. S., Newsom J. T. (2007). The joint effects of life stress and negative social exchanges on emotional distress. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, S304–S314. doi:10.1093/geronb/62.5.s304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badr H., Acitelli L. K. (2005). Dyadic adjustment in chronic illness: Does relationship talk matter? Journal of Family Psychology, 19, 465–469. doi:10.1037/0893-3200.19.3.465 [DOI] [PubMed] [Google Scholar]
- Berg C. A., Upchurch R. (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133, 920–954. doi:10.1037/0033-2909.133.6.920 [DOI] [PubMed] [Google Scholar]
- Birditt K., Antonucci T. C. (2008). Life sustaining irritations? Relationship quality and mortality in the context of chronic illness. Social Science & Medicine (1982), 67, 1291–1299. doi:10.1016/j.socscimed.2008.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birditt K. S., Newton N., Hope S. (2012). Implications of marital/partner relationship quality and perceived stress for blood pressure among older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbs123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala J. (2005). The role of marital quality in physical health during the mature years. Journal of Aging and Health, 17, 85–104. doi:10.1177/0898264304272794 [DOI] [PubMed] [Google Scholar]
- Carr D., Freedman V. A., Cornman J. C., Schwarz N. (2014). Happy marriage, happy life? Marital quality and subjective well-being in later life. Journal of Marriage and the Family, 76, 930–948. doi:10.1111/jomf.12133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Wills T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. doi:10.1037/0033-2909.98.2.310 [PubMed] [Google Scholar]
- Crimmins E. Guyer H. Langa K. Ofstedal M. B. Wallace R., & Weir D (2008). Documentation of physical measures, anthropometrics, and blood pressure in the Health and Retirement Study Retrieved from http://hrsonline.isr.umich.edu/sitedocs/userg/dr-011.pdf. doi:10.7826/isr-um.06.585031.001.05.0014.2008
- Delgado J., Jacobs E. A., Lackland D. T., Evans D. A., de Leon C. F. (2012). Differences in blood pressure control in a large population-based sample of older African Americans and non-Hispanic whites. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 67, 1253–1258. doi:10.1093/gerona/gls106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagly A. H., & Wood W (2013). The nature-nurture debates: 25 Years of challenges in understanding the psychology of gender. Perspectives on Psychological Science, 8, 340–357. doi:10.1177/1745691613484767 [DOI] [PubMed] [Google Scholar]
- Grossman M., Wood W. (1993). Sex differences in intensity of emotional experience: A social role interpretation. Journal of Personality and Social Psychology, 65, 1010–1022. doi:10.1037//0022-3514.65.5.1010 [DOI] [PubMed] [Google Scholar]
- Hawkley L. C., Masi C. M., Berry J. D., Cacioppo J. T. (2006). Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging, 21, 152–164. doi:10.1037/0882-7974.21.1.152 [DOI] [PubMed] [Google Scholar]
- Holley S. R., Haase C. M., Levenson R. W. (2013). Age-related changes in demand-withdraw communication behaviors. Journal of Marriage and the Family, 75, 822–836. doi:10.1111/jomf.12051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J. S., Landis K. R., Umberson D. (1988). Social relationships and health. Science (New York, N.Y.), 241, 540–545. doi:10.1126/science.3399889 [DOI] [PubMed] [Google Scholar]
- Juster R. P., McEwen B. S., Lupien S. J. (2010). Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews, 35, 2–16. doi:10.1016/j.neubiorev.2009.10.002 [DOI] [PubMed] [Google Scholar]
- Katz J., Monnier J., Libet J., Shaw D., Beach S. R. H. (2000). Individual and crossover effects of stress on adjustment in medical student marriages. Journal of Marital and Family Therapy, 26, 341–351. doi:10.1111/j.1752-0606.2000.tb00303.x [DOI] [PubMed] [Google Scholar]
- Kenny D. A. Kashy D. A., & Cook W. L (2006). Dyadic data analysis. New York, NY: Guilford Press. [Google Scholar]
- Kiecolt-Glaser J. K., Newton T. L. (2001). Marriage and health: His and hers. Psychological Bulletin, 127, 472–503. doi:10.1177/1094428108324689 [DOI] [PubMed] [Google Scholar]
- Li T., Fung H. H. (2012). Partner discrepancies and age differences in marital quality: Distinguishing the ideal, expected, and perceived partner. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 417–422. doi:10.1093/geronb/gbr119 [DOI] [PubMed] [Google Scholar]
- Lindau S. T., Laumann E. O., Levinson W., Waite L. J. (2003). Synthesis of scientific disciplines in pursuit of health: The Interactive Biopsychosocial Model. Perspectives in Biology and Medicine, 46, S74–S86. doi:10.1353/pbm.2003.0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalowski V. I. Hoppmann C. A., & Gerstorf D (2014). Associations between perceived support in older adult marriages and dyadic covariations in momentary affect and aches. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. doi:10.1093/geronb/gbu151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monin J. K., & Clark M. S (2000). Why do men benefit more from marriage than do women? Thinking more broadly about interpersonal processes that occur within and outside of marriage. Sex Roles, 65, 320–326. doi:10.1007/s11199-011-0008-3 [Google Scholar]
- Monin J. K., Schulz R., Martire L. M., Jennings J. R., Lingler J. H., Greenberg M. S. (2010). Spouses’ cardiovascular reactivity to their partners’ suffering. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B, 195–201. doi:10.1093/geronb/gbp133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neff L. A., & Karney B. R (2007). Stress crossover in newlywed marriage: A longitudinal and dyadic perspective. Journal of Marriage and Family, 69, 594–607. doi:10.1111/j.1741-3737.2007.00394.x [Google Scholar]
- Rauer A. J., & Volling B. L (2005). The role of husbands’ and wives’ emotional expressivity in the marital relationship. Sex Roles, 52, 577–587. doi:10.1007/s11199-005-3726-6 [Google Scholar]
- Robles T. F., Kiecolt-Glaser J. K. (2003). The physiology of marriage: Pathways to health. Physiology & Behavior, 79, 409–416. doi:10.1016/s0031-9384(03)00160-4 [DOI] [PubMed] [Google Scholar]
- Robles T. F., Slatcher R. B., Trombello J. M., McGinn M. M. (2013). Marital quality and health: A meta-analytic review. Psychological Bulletin. doi:10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rook K. Dooley D., & Catalano R (1991). Stress transmission: The effects of husbands’ job stressors on the emotional health of their wives. Journal of Marriage and Family, 53, 165–177. doi:10.2307/353141 [Google Scholar]
- Ryan L. H., Wan W. H., Smith J. (2014). Spousal social support and strain: Impacts on health in older couples. Journal of Behavioral Medicine, 37, 1108–1117. doi:10.1007/s10865-014-9561-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuster T. L., Kessler R. C., Aseltine R. H., Jr (1990). Supportive interactions, negative interactions, and depressed mood. American Journal of Community Psychology, 18, 423–438. doi:10.1007/BF00938116 [DOI] [PubMed] [Google Scholar]
- Seeman T. E. (1996). Social ties and health: The benefits of social integration. Annals of Epidemiology, 6, 442–451. doi:10.1016/s1047-2797(96)00-6 [DOI] [PubMed] [Google Scholar]
- Singer J. D., & Willett J. B (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press. [Google Scholar]
- Smith J. Fisher G. Ryan L. Clarke P. House J., & Weir D (2013). Psychosocial and lifestyle questionnaire, 2006–2010. Document Report Core Section LB Ann Arbor, MI: Survey Research Center, Institute for Social Research, University of Michigan. [Google Scholar]
- Steptoe A. Kunz-Ebrecht S. Owen N. Feldman P. J. Willemsen G. Kirschbaum C., & Marmot M (2003). Socioeconomic status and stress-related biological responses over the working day. Psychosomatic Medicine, 65, 461–470. doi:10.1097/01.psy.0000035717.78650.a1 [DOI] [PubMed] [Google Scholar]
- Thoits P. A. (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51, S41–S53. doi:10.1177/0022146510383499 [DOI] [PubMed] [Google Scholar]
- Troxel W. M., Matthews K. A., Bromberger J. T., Sutton-Tyrrell K. (2003). Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychology, 22, 300–309. doi:10.1037/0278-6133.22.3.300 [DOI] [PubMed] [Google Scholar]
- Uchino B. N. (2009). Understanding the links between social support and physical health. Perspectives on Psychological Science, 4, 236–255. doi:10.1111/j.1745-6924.2009.01122.x [DOI] [PubMed] [Google Scholar]
- Walen H. R., & Lachman M. E (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17, 5–30. doi:10.1177/0265407500171001 [Google Scholar]
- Whisman M. A., Uebelacker L. A., Settles T. D. (2010). Marital distress and the metabolic syndrome: Linking social functioning with physical health. Journal of Family Psychology, 24, 367–370. doi:10.1037/a0019547 [DOI] [PubMed] [Google Scholar]
- Williams S. R., Pham-Kanter G., Leitsch S. A. (2009). Measures of chronic conditions and diseases associated with aging in the national social life, health, and aging project. The Journals of Gerontology: Social Sciences, 64, i67–i75. doi:10.1093/geronb/gbn015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.