Abstract
Introduction
Cancer of the gallbladder is a serious diagnostic and therapeutic problem. According to the literature, 30% of cases are not confirmed before surgery. Other cases are detected incidentally by histopathology. Clinical trials and meta-analyses show that incidental gallbladder cancer (iGBC) occurs in 0.19%–2.8% of patients after cholecystectomy. The aim of this study was to analyze the incidence and severity of iGBC in cholecystectomy procedures performed in the surgical department at the 4th Military Teaching Hospital in Wroclaw during the years 1990–2014.
Patients and methods
In the years 1990–2014, a total of 7,314 cholecystectomies were performed in the surgical department because of cholecystolithiasis: 6,145 were performed using the laparoscopic approach (84.02%), 867 were performed as open surgery (11.8%), and 302 cases required conversion (5.1%). In this group, 5,214 of the patients were females (71.3%) and 2,100 were males (28.7%), with an average age of 54.7 years.
Results
We found 64 iGBC cases which were confirmed by histopathology. This represented 0.87% of all cases. In this group, 50 patients were females (78.1%) and 14 were males (21.8%), with an average age of 67.1 years. Of this group, 40 patients underwent a classic cholecystectomy, while 24 underwent laparoscopic procedures, out of which 13 cases ultimately required traditional surgery. The histopathology showed 15 carcinomas that were classified as G1 (23.4%), 28 were G2 (43.75%), and 21 were G3 (32.8%).
Conclusion
iGBC detected after a cholecystectomy due to cholecystolithiasis is a rare disease. We found iGBC in 0.87% of cases, which is on a comparable scale to the world literature. In the case of cancer, we frequently found it necessary to convert to an open surgical procedure. This cancer is more common in females and in people over 60 years of age.
Keywords: incidental cancer of the gallbladder, cholecystectomy, cholecystolithiasis, laparoscopic cholecystectomy, radicality
Introduction
Gallbladder cancer is a rare, highly malignant tumor constituting 0.6%–1.5% of all cases after cholecystectomy and is the most common bile duct cancer. Sixty percent of the cases affected were females, with an age above 65 years. Although the etiology is not yet fully known, cholecystolithiasis appears to be related to the incidence of proliferative changes. Polyps, particularly those which are larger than 10 mm, also increase the risk of developing a neoplastic disease.1,2 There is a large variation in the incidence of the disease, depending on the ethnicity. In Poland, South America, and India, the incidence is 7.5 per 100,000 males and 23 per 100,000 females, while in Singapore, the US, and Nigeria it is only 2.5 per 100,000.1
The prognosis for gallbladder cancer is poor due to the significant difficulties associated with its diagnosis. It is now believed that the 5-year survival rate is ~32% when the serous membrane is involved. If the tumour is more advanced, the annual survival rate is decreased to ~10%.2 Due to the location of the gallbladder, the symptoms appear late, usually when the disease is already in the advanced stage. Only ~30% of cancers are detected before surgery. The remaining cases are diagnosed during or after surgery by histopathology. We qualify such cases as incidental gallbladder cancer (iGBC).3
Currently, a laparoscopic cholecystectomy is the gold standard for the treatment of cholecystolithiasis. It is one of the most frequently performed surgical procedures in the world; in the US, ~1,000,000 such procedures are performed each year.4
The aim of the study was to analyze the incidence and severity of iGBC in cholecystectomy procedures performed in our surgical department.
Patients and methods
In the years 1990–2014, a total of 7,314 cholecystectomies were performed in the surgical department because of cholecystolithiasis on an elective and an emergency basis: 6,145 (84.02%) of these surgeries were performed laparoscopically, 867 (11.8%) using the traditional open surgery method, and 302 (5.1%) patients required conversion from the laparoscopic method to classic open surgery. Females accounted for 71.3% (5,214) of all patients and males for 28.7% (2,100). The mean age of all patients was 54.7 years, 53.9 years in females and 56.8 years in males. All patients underwent a postoperative histopathological examination of the gallbladder which had been removed. This study was approved by the Lodz Medical University Ethics Committee (approval number RNN/145/15/KB). All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All patients provided written informed consent to have their data used in this study.
Results
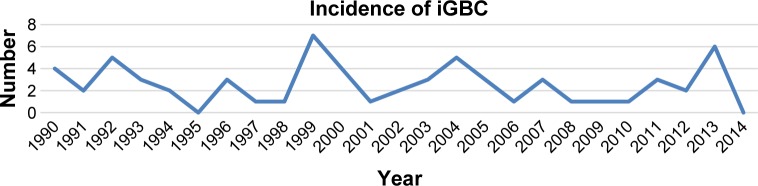
Out of a total of 7,314 cholecystectomies performed, iGBC occurred in 64 cases, which accounted for 0.87% of all surgical patients (Figure 1). The average age of patients diagnosed with iGBC was 67.1 years (the youngest being 44 and the oldest 89 years of age). iGBC affected 48 (75%) females and 16 (25%) males, with the average age being 66.2 years for females and 69.8 years for males. Forty patients were treated on an elective basis, and 24 underwent emergency procedures due to the development of acute cholecystolithiasis in 19 patients and symptoms of a gastrointestinal obstruction in five patients. Forty (62.5%) patients underwent an open surgery cholecystectomy, ten (15.6%) underwent a laparoscopic procedure, and in 14 cases (21.9%) laparoscopic surgery was started but it became necessary to convert to classic open surgery. In this group of 14 patients, the conversion was made in four cases because of visible tumor-like lesions and in ten cases because of the difficult anatomy. In the course of 20 surgeries, the surgery was simultaneously extended due to the resection of segments 4b and 5 in seven cases, widening the margin of the resection in eight cases, the removal of lymph nodes in twelve patients, and the resection of the duodenum with partial resection of the stomach in two patients. Seventeen patients underwent radical resections which did not require further surgery. Thirteen patients needed another surgery in order to widen the margins of the first one. In 14 patients, the changes were inoperable due to metastases (eight patients) or vascular or bile duct invasion (six patients). In this group, five cases required gastrointestinal bypass anastomosis during the first surgery. Within 1 year of initially being hospitalized, two consecutive patients in this group underwent surgery due to the obstruction of the gastrointestinal tract and four patients needed biliary prosthesis due to increasing jaundice. Three patients did not consent to the proposed further surgery. All patients who were operated on were referred for further oncological treatment. According to the histopathological evaluation, 62 cases (96.8%) had adenocarcinoma and two cases (3.2%) had a squamous cell carcinoma. Based on the histological stage, 15 (23.4%) were diagnosed with G1 carcinomas, 28 (43.8%) with G2, and 21 (32.8%) with G3. In 14 cases (21.9%), the diagnosis was made intraoperatively, while in the other 50 (78.1%) cases, the final diagnosis was made based on a postoperative examination. Taking into account the tumor node metastasis (TNM) classification, stage 0 (TisN0M0) was not observed in any of the patients, stage I (T1a–bN0M0) in eight (12.5%), stage II (T2N0M0) in 12 (18.7%), stage IIIa (T3N0M0) in 18 (28.1%), stage IIIb (T1–3N1M0) in 12 (18.8%), stage IVA (T4N0–1M0) in six (9.4%), and stage IVB (TxNxM1) in eight (12.5%) (Table 1).
Figure 1.
Incidence of iGBC.
Abbreviation: iGBC, incidental gallbladder cancer.
Table 1.
The patients’ characteristics
| Sociodemographic factors | Number of patients |
|---|---|
| Sex, males/females | 16/48 |
| Elective/emergency surgery | 40/24 |
| Classic cholecystectomy | 40 |
| Laparoscopic cholecystectomy | 10 |
| Conversion | 14 |
| Stage 0 | 0 |
| Stage IA/IB | 3/5 |
| Stage II | 12 |
| Stage IIIA/IIIB | 18/12 |
| Stage IVA/IVB | 6/8 |
| Diagnosis intraoperative | 14 |
| Diagnosis postoperative | 50 |
| Histopathological type – adenocarcinoma | 62 |
| Histopathological type – squamous cell carcinoma | 2 |
| Grade G1 | 15 |
| Grade G2 | 28 |
| Grade G3 | 21 |
Discussion
The data that has been collected indicates that the occurrence of incidentally detected gallbladder cancer is 0.87%, which gives a value close to that suggested in the literature (0.19%–2.8%).3,5–16 The very high percentage of changes (68.75%) which are highly advanced is striking, which is mainly due to insufficient preoperative diagnosis. In our material, stage IIIA occurred in 18 (28.1%) patients, stage IIIB in 12 (18.8%), stage IVA in six (9.4%), and eight iGBC patients (12.5%) presented distant metastases at the time of surgery (stage IVB). These results differ greatly from the results reported in the literature. In a similar patient population (7,582 with cholecystectomy and 69 iGBC), Tian et al found 19 cases (30%) defined as stage IIIA/B and no patients in stage IV.3 In the same study, as many as 38 (55%) patients at the time of iGBC diagnosis were classified as stage IA and IB compared to eight (12.5%) patients in our material.3 In contrast, Choi et al5 conducted a meta-analysis of 26 works on the iGBC occurrence and found a primary tumor at stage T1 in 23% (4.2%–61%), T2 in 47% (13.2%–75%), T3 in 25.1% (0%–69.8%), and T4 in 4.2% (0%–21.1%) of the cases. Also in this study, we observed a significant prevalence of less advanced stages of tumors compared to our material.5–12 Based on these data, we conclude that gallbladder cancer in Poland is still a very serious diagnostic problem. Even decades of analysis have not resulted in a downward trend in the number of advanced changes: stage > IIIA in 20/28 (71%) in the years 1990–1999, in 16/24 (66%) in the years 2000–2009, and in 8/12 (66%) in the years 2010–2014.
The percentage of surgeries that required conversion from a laparoscopic procedure to open surgery is much higher in patients with iGBC. Our material indicates that out of 6,145 cholecystectomies performed, conversion was necessary in 302 cases (5.1%), whereas in patients diagnosed with iGBC it was required in 58% (14/24 surgeries). Only four conversions were made due to visible proliferative lesions. In ten cases (41.6%), difficult anatomical conditions were the reason for choosing a laparotomy and the tumors were recognized only after a histopathological examination. Based on these results, we observe that when difficult anatomical conditions are encountered during a laparoscopy and when it becomes necessary to perform the conversion to open procedure, we should always keep in mind the greater likelihood of neoplastic lesions in the gallbladder.4,5,7–13 We should consider the radicality of the surgery, which should be as wide as possible, and we should avoid perforation of the gallbladder and bile spilling into the peritoneal cavity, which is a factor that worsens the iGBC prognosis.3,5,7,9 The literature indicates a much higher percentage of conversion in patients with iGBC.3,4,8,11,12
An important role in the diagnosis of iGBC is the use of an intraoperative histological examination.3,13,14 This is a quick and easy test done when a qualified pathologist is available. In our study, this test was performed in 14 cases and always managed to confirm malignancy. Intraoperative diagnosis greatly facilitates further management in case of doubt, giving the opportunity to perform radical surgery. This eliminates the need for another surgical procedure, which is always more difficult to implement than the original surgery.3,15–17
Conclusion
Gallbladder cancer, although rare, is still a serious diagnostic and therapeutic problem. Despite the increase in the availability of qualified medical staff and diagnostic procedures, the number of iGBC remains at a similar level.
The advancement of changes after the surgery is alarming. Our material proves a very high percentage of patients have advanced tumor lesions whose prognosis is poor with a 1-year survival rate of 44% for stage III and of 30% for stage IV.1 We find these results very poor compared to those reported in the literature.3,5–11
This demonstrates an insufficient diagnosis or difficulties in its accessibility and a low public awareness of gallbladder cancer. It is important to diagnose cancer as soon as possible because it is the most important factor in improving the survival of patients.
Our experience, and the literature indicate that an intraoperative histological examination is a very useful method that should be carried out as often as possible. It helps to plan the extent of the surgery properly and judge its radicality. Unfortunately, there are still few centers that have their own histopathological laboratories, and this greatly restricts the applicability of this diagnostic method. The high frequency of cholecystectomy performed on an emergency basis also limits the availability of an intraoperative examination.
Footnotes
Disclosure
The authors report no other conflicts of interest in this work.
References
- 1.Misra S, Chaturvedi A, Misra NC, Sharma ID. Carcinoma of the gallbladder. Lancet Oncol. 2003;4(3):167–176. doi: 10.1016/s1470-2045(03)01021-0. [DOI] [PubMed] [Google Scholar]
- 2.Lazcano-Ponce EC, Miquel JF, Munoz N, et al. Epidemiology and molecular pathology of gallbladder cancer. CA Cancer J Clin. 2001;51(6):349–364. doi: 10.3322/canjclin.51.6.349. [DOI] [PubMed] [Google Scholar]
- 3.Tian YH, Ji X, Liu B, et al. Surgical treatment of incidental gallbladder cancer discovered during or following laparoscopic cholecystectomy. World J Surg. 2015;39(3):746–752. doi: 10.1007/s00268-014-2864-9. [DOI] [PubMed] [Google Scholar]
- 4.Pitt SC, Jin LX, Hall BL, Strasberg SM, Pitt HA. Incidental gallbladder cancer at cholecystectomy: when should the surgeon be suspicious? Ann Surg. 2014;260(1):128–133. doi: 10.1097/SLA.0000000000000485. [DOI] [PubMed] [Google Scholar]
- 5.Choi KS, Choi SB, Park P, Kim WB, Choi SY. Clinical characteristics of incidental or unsuspected gallbladder cancers diagnosed during or after cholecystectomy: a systematic review and meta-analysis. World J Gastroenterol. 2015;21(4):1315–1323. doi: 10.3748/wjg.v21.i4.1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi SB, Han HJ, Kim CY, et al. Incidental gallbladder cancer diagnosed following laparoscopic cholecystectomy. World J Surg. 2009;33(12):2657–2663. doi: 10.1007/s00268-009-0249-2. [DOI] [PubMed] [Google Scholar]
- 7.Pawlik TM, Gleisner AL, Vigano L, et al. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg. 2007;11(11):1478–1486. doi: 10.1007/s11605-007-0309-6. [DOI] [PubMed] [Google Scholar]
- 8.Clemente G, Nuzzo G, De Rose AM, et al. Unexpected gallbladder cancer after laparoscopic cholecystectomy for acute cholecystitis: a worrisome picture. J Gastrointest Surg. 2012;16(8):1462–1468. doi: 10.1007/s11605-012-1915-5. [DOI] [PubMed] [Google Scholar]
- 9.Fuks D, Regimbeau JM, Le Treut Y-P, et al. Incidental gallbladder cancer by the AFC-GBC-2009 Study Group. World J Surg. 2011;35(8):1887–1897. doi: 10.1007/s00268-011-1134-3. [DOI] [PubMed] [Google Scholar]
- 10.Glauser PM, Strub D, Kaeser SA, Mattiello D, Rieben F, Maurer CA. Incidence, management, and outcome of incidental gallbladder carcinoma: analysis of the database of the Swiss association of laparoscopic and thoracoscopic surgery. Surg Endosc. 2010;24(9):2281–2286. doi: 10.1007/s00464-010-0952-y. [DOI] [PubMed] [Google Scholar]
- 11.Choi SB, Han HJ, Kim CY, et al. Incidental gallbladder cancer diagnosed following laparoscopic cholecystectomy. World J Surg. 2009;33(12):2657–2663. doi: 10.1007/s00268-009-0249-2. [DOI] [PubMed] [Google Scholar]
- 12.Ferrarese AG, Solej M, Enrico S, et al. Diagnosis of incidental gallbladder cancer after laparoscopic cholecystectomy: our experience. BMC Surg. 2013;13(Suppl 2):S20. doi: 10.1186/1471-2482-13-S2-S20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butte JM, Waugh E, Meneses M, Parada H, De La Fuente HA. Incidental gallbladder cancer: analysis of surgical findings and survival. J Surg Oncol. 2010;102(6):620–625. doi: 10.1002/jso.21681. [DOI] [PubMed] [Google Scholar]
- 14.Cavallaro A, Piccolo G, Panebianco V, et al. Incidental gallbladder cancer during laparoscopic cholecystectomy: managing an unexpected finding. World J Gastroenterol. 2012;18(30):4019–4027. doi: 10.3748/wjg.v18.i30.4019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shimizu T, Arima Y, Yokomuro S, et al. Incidental gallbladder cancer diagnosed during and after laparoscopic cholecystectomy. J Nippon Med Sch. 2006;73(3):136–140. doi: 10.1272/jnms.73.136. [DOI] [PubMed] [Google Scholar]
- 16.Kapoor VK. Incidental gallbladder cancer. Am J Gastroenterol. 2001;96(3):627–629. doi: 10.1111/j.1572-0241.2001.03597.x. [DOI] [PubMed] [Google Scholar]
- 17.Gil L, Lendoire J, Duek F, et al. Radical surgery for incidental gallbladder cancer: the value of a deferred pathological finding of residual disease. Cir Esp. 2014;92(3):168–174. doi: 10.1016/j.ciresp.2013.11.010. [DOI] [PubMed] [Google Scholar]