Abstract
Background
The transition from Medicaid-only to dual Medicare/Medicaid coverage has the potential to reduce financial barriers to health care for patients with serious mental illness (SMI) through increased coverage or expanded access to clinicians as their reimbursement increases.
Aims
To estimate the effect of dual coverage after Medicaid enrollment during the required waiting period among adults with SMI on health care use, overall and related to mental health and substance use disorders (MHSUD).
Methods
Data include enrollment and claims from Medicaid and Medicare in Missouri (MO) and South Carolina (SC), from January 2004 – December 2007. We used an interrupted time series design to estimate the effect of dual coverage on average use of outpatient, emergency (ED), and inpatient care/month.
Results
After 12-months of dual coverage, the probability of outpatient care use increased in both states from 4 – 9%. In MO the mean probability and frequency of ED visits, total and MHSUD-related, increased by 21–32%; the probability of all-cause and MHSUD-related inpatient admissions increased by 10% and 19% respectively. In SC, the mean probability of any inpatient admission increased by 27% and of any MHSUD-related inpatient admission by 42%.
Discussion
The increase in use of outpatient care is consistent with the expected increase in coverage of, and payment for, outpatient services under dual coverage relative to Medicaid-only. Sustained increases in ED and inpatient admissions raise questions regarding the complexity of obtaining care under 2 programs, pent-up demand among beneficiaries pre-transition, and the complementarity of outpatient and inpatient service use.
Keywords: mental illness, disability, Medicaid, Medicare, dual beneficiary
Introduction
Each month non-elderly, adult Medicaid beneficiaries with disabilities transition from Medicaid-only coverage to full dual Medicaid and Medicare coverage.(1) Nearly half of non-elderly dual beneficiaries have a serious mental illness (SMI) including bipolar disorder, major depressive disorder, and schizophrenia.(2) They are a disproportionately expensive population when enrolled in Medicaid alone and as dual beneficiaries in Medicaid and Medicare.(3–6) Health care expenditures are 1.8 times higher for non-elderly dual enrollees with a mental health disorder compared to other non-elderly duals.(4) However, use of medical(7) and mental health care(8–11) (12) among publicly insured adults with SMI often falls short of perceived needs and expert recommendations, increasing the risk of adverse and costly health outcomes for beneficiaries and payers.(13–15)
Medicaid beneficiaries who participate in the Supplemental Security Disability Insurance (SSDI) program acquire Medicare coverage after a required 24-month waiting period.(16) SSDI beneficiaries may additionally qualify for the Supplemental Security Income (SSI) program if their income and assets are sufficiently low. Both federal disability programs share the same disability criteria and determination process. SSDI confers Medicare eligibility after a waiting period while Medicaid eligibility typically accompanies an SSI award.(17) After the transition to dual enrollment, Medicare becomes the primary insurer. The Medicaid program provides supplementary coverage for services that the Medicare program may not provide and assumes responsibility for the Medicare program's patient cost-sharing requirements.(18)
The acquisition of dual coverage requires that individuals navigate two insurance programs, a potential impediment to health care access. However, the transition from Medicaid-only to dual coverage also entails a likely increase in provider reimbursement and covered services. The financial incentive for physicians to provide services after the beneficiary's transition from Medicaid-only to full dual coverage is likely higher.(19) On average Medicare reimbursements for physicians are 39% higher than Medicaid reimbursements, and physician acceptance rates of new Medicare enrollees are substantially higher than for new Medicaid enrollees.(20, 21) Additionally, cost-related barriers to care may decrease for the services that Medicare provides more generously or without limits relative to Medicaid. Limits on covered services and cost-sharing requirements impede health care access among low-income adults with SMI.(22, 23) At least ten Medicaid programs impose monthly or annual limits on medical and/or mental health office visits, after which the patient faces the full price.(24, 25) Medicare does not limit such office visits. The relative generosity of prescription drug coverage between programs is less clear and depends on both the beneficiary's Medicaid program and Medicare Part D plan.(26–28) Neither Medicaid or Medicare limits inpatient psychiatric stays in a general hospital; however, Medicaid does not cover inpatient stays in psychiatric hospitals for adults.(29, 30) Medicare provides such coverage for up to 190 days over the beneficiary's lifetime.(31)
We hypothesize that more generous clinician reimbursement rates and covered services will increase access to health care after receipt of dual coverage. The known effects of Medicare eligibility at age 65 on the use of health care are consistent with our expectations. Upon reaching age 65, health care use generally increases to the extent that Medicare coverage is more generous than prior coverage along one or more of the following dimensions: additional covered services; the relaxation of utilization management practices; and, higher reimbursement for defined services.(32–35)
In this study, we evaluate the effect of newly acquired dual coverage on the use of health care among adults with SMI who were previously enrolled in Medicaid. No previous longitudinal study has evaluated the effects of this significant insurance transition on health care outcomes among adults with SMI.
Methods
Natural Experiment
We separately evaluated receipt of dual coverage after the Medicaid-only coverage in Missouri (MO) and South Carolina (SC). In MO and SC, adults with psychiatric disabilities participated in fee-for-service (FFS) programs while enrolled in Medicaid-only and in dual coverage allowing us to examine the impact of dual coverage while holding constant the service delivery model. After acquiring dual coverage, these enrollees continued to face the Medicaid co-payments charged in their states. They were not responsible for Medicare cost-sharing (e.g., premiums, deductibles, co-insurance) with the exception of prescription drug copayments beginning in 2006; these copayments were comparable to those charged under Medicaid in SC and MO.(36) The transition to dual enrollment increased physician payment rates; the magnitude of that increase varies by procedure code and specialty. In SC the insurance transition also increased coverage for outpatient visits which was then limited to 12 mental health therapy and 12 physician visits annually for adult FFS beneficiaries.(37) Medicare had no such limits.
Sample
The study population includes adults ages 21–64 with SMI who have at least one month of dual coverage immediately preceded by at least one month of Medicaid-only enrollment between January 1, 2004 through December 31, 2007. In our unbalanced panel, subjects were continuously enrolled on the basis of disability in Medicaid-only and dual coverage; they were eligible for full Medicare and Medicaid benefits. We identified individuals as having a SMI if they had at least one primary or secondary diagnosis1 for bipolar disorder (BP), schizophrenia (SZ), or major depressive disorder (MDD) observed on a claim for outpatient, inpatient or emergency department (ED) services before and/or after transitioning to dual coverage. The analytic sample includes 1,837 adults in SC and 6,012 in MO. We constructed a rolling cohort. The index month for each individual was the month of transition to dual coverage, thus facilitating an interrupted time-series (ITS) design, as in previous work.(38)
Data
We merged enrollment and medical claims data from Medicaid and Medicare for the study population. Enrollment files included dates of enrollment in both programs and beneficiary demographic information. Claims data included the service type, service dates, and diagnoses. Our analytic dataset appends two identical extracts for the years 2004–2005 and 2006–2007. In each extract, we observe Medicaid claims for the pre-transition period back to the start of the extract (i.e., 2004 or 2006). Consequently, there is left censoring of the pre-transition observation time for individuals who transitioned in 2004 or 2006. In our regression models, we account for this variation in observation time by including transition year and the duration of pre- and post- transition observation periods.
Empirical Approach
The study “treatment” is dual coverage. The treatment assignment mechanism is the process that determines the month of transition to dual coverage. This process is a strong approximation of an exogenous assignment mechanism because the transition month is largely out of the individual's control.(16) The Social Security Administration determines the “date of disability onset” during the disability application process. For SSDI beneficiaries, the transition to Medicare occurs 29 months later. During and after this waiting period, all study subjects were enrolled in Medicaid. Beneficiaries were likely aware of the dual transition date in the same way that adults approaching their 65th birthday are aware of their imminent Medicare eligibility. This awareness does not invalidate the assumed exogeneity of treatment assignment. Individuals may alter health care use in anticipation of Medicare coverage for many reasons including generosity of coverage, provider availability, perceived quality, etc. Each of these responses is a potential explanation for a change care use under dual coverage relative to Medicaid-only. This study quantifies the overall beneficiary response to dual coverage.
We used an ITS design to estimate the effect of dual coverage on changes in the level and trend of use of health care. To obtain causal estimates, this design requires a discrete intervention, a sufficient number of observation points to control for the underlying outcome trends, and the absence of a concurrent event that might confound the intervention-outcome relationship.(39) Our time series is sufficiently long time with adequate sample sizes at each point to identify the effect of interest (39–41). In MO, there are up to 23 months before and 46 months after the transition for beneficiaries. In SC, there are up to 21 months before and 44 months after the transition; we excluded two months at either end of the study because there were fewer than 100 observations in each of those months. Two features of this design reduce the likelihood that a confounding concurrent event may bias our results. First, the transition month varies by subject and is distributed throughout the 4-year period. Second, in this rolling cohort, “future transitioners” provide a secular control for individuals that have already transitioned.
Statistical Analysis
We compared unadjusted average monthly health care use per person before and after dual coverage using a t test for count/continuous variables and a Wald test for binary variables. Additionally, we used segmented linear regression to illustrate the unadjusted, mean health care use at the population-level in the months preceding and following receipt of dual coverage. We used generalized estimating equations (GEE) for our preferred, adjusted person-level analyses: a binomial distribution and logit link for binary outcomes and Gamma-log model for count and continuous measures.(42) Standard errors are clustered at the subject-level; we selected the correlation structure, a first-order autoregressive process, using the QIC method.(43)
| Model 1 |
Yit is the health care utilization outcome for subject i in month t. The integer variable baseline trend denotes the month numbered from the start to the end of the study period, 1,…48. The binary variable dual coverage equals 1 if subject i has transitioned to dual status at time t and 0 otherwise. The integer variable trend change reflects the number of months since acquiring dual status. The vector X includes time-invariant person level covariates: age; sex; race; and number of months observed before and after the transition. Finally, vector Z includes indicator variables for each year of transition.
In these non-linear models, the regression coefficients are not directly interpretable as marginal effects. To facilitate interpretation of results, we present several estimates derived from the regression results. We concentrate our presentation and discussion on the average marginal effects of dual coverage at 12 months after receipt of dual coverage, and the counterfactual outcome, the predicted outcome at 12 months in the absence of a change in coverage. Additionally, we include the average marginal effects for each of the key terms, baseline trend, dual coverage, and trend change, in the regression model holding all other variables at their observed values.(44)
Sensitivity Analyses
We excluded the transition month and one month on either side of it to examine whether anticipation of Medicare coverage was a key determinant of a beneficiary's response to dual coverage. To test whether an increase in SMI incidence under dual coverage influenced our results, we restricted the sample to subjects who were unlikely to have acquired the SMI diagnosis during the study period, those with a diagnosis of bipolar disorder or schizophrenia. Finally, we estimated all models including quadratic terms for the baseline trend and trend change. Study findings were robust to each of these alternate specifications and exclusions in MO. In SC, omission of the transition months resulted in a larger increase in outpatient visits under dual coverage and a smaller, non-significant increase in inpatient admissions. (See Appendix A1and A2.)
Outcomes
We measured health care use for each person-month in three service categories: outpatient; ED; and inpatient services. In each category, we analyzed total care use and care use related to a mental health or substance use disorder (MHSUD). The outpatient measures include a binary variable that equals one if the beneficiary had a non-emergency, outpatient visit on at least one day in the month (i.e., physician's office, an outpatient clinic within a hospital, or a community health center.) We assessed the number of days/month on which the beneficiary had at least one outpatient visit. ED outcomes include a binary measure indicating any ED visit in the month and a count of days with an ED visit in the month. We assessed monthly inpatient care use as a binary indicator for any admission, a count of admissions, and the number of days hospitalized.
To identify MHSUD care use we adapted Goldman and colleagues' method.(45) Inpatient stays and ED visits were considered related to MHSUD if the primary diagnosis was a behavioral health condition or if a self-injury/suicide code was indicated (i.e., ICD-9 Codes 290.xx – 319.xx, 648.3x 648.4x, and E950.0-E959.9, V6284). MHSUD outpatient care included outpatient visits for a procedure that was specific to MHSUD care (e.g., psychotherapy) or an outpatient visit with a primary diagnosis of MHSUD.
Results
Descriptive results
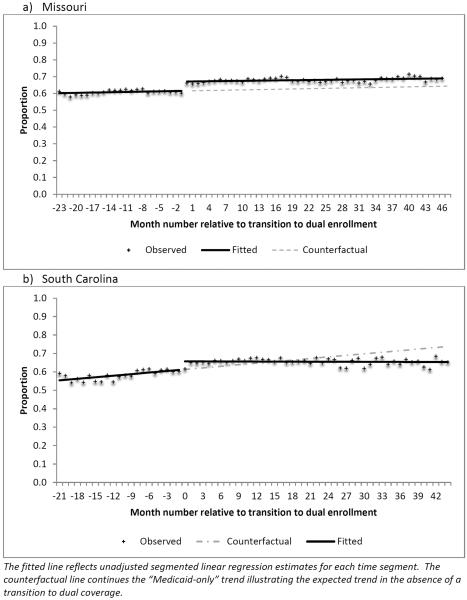
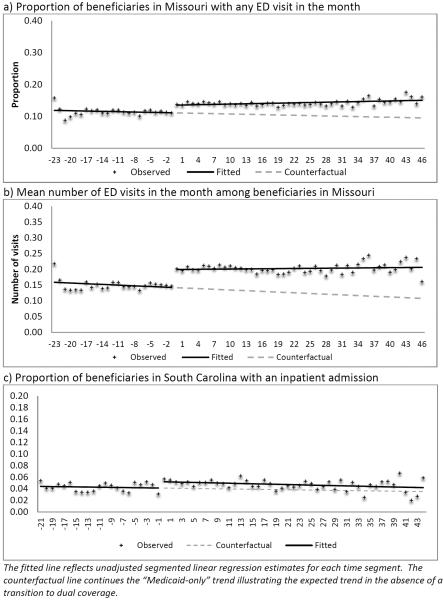
The average age of subjects was 40 in both states with women comprising more than 60% of the study population. (Table 1) In SC, approximately 38% of the study subjects were non-White while in MO that figure was approximately 16%. We observed an average of 10 months of Medicaid-only coverage for study subjects and approximately 20 months of dual coverage following receipt of dual coverage. Average unadjusted monthly health care use is summarized in Table 2. All results presented in the text were statistically significant at p <0.05. In MO, total and MHSUD-related use of outpatient and ED services was higher under dual coverage relative to Medicaid-only period. In SC, total health care use was higher in most service categories after dual enrollment relative to the Medicaid-only period; MHSUD-related inpatient days were relatively higher under dual coverage. Results from unadjusted segmented linear regression models are presented in Figures 1 and 2. In MO, the trend in outpatient care shows an abrupt increase in the probability of an outpatient visit in the month upon receipt of dual coverage (Figure 1a). The probability and quantity of ED use also increase after receipt of dual coverage (Figures 2a and 2b). In SC, the transition to dual enrollment increased the probability of having an outpatient visit in the month relative to the Medicaid-only period Figure 1b). The positive slope observed during the baseline period reversed direction after dual coverage, eliminating the initial level increase by the end of the observation period. The probability of an inpatient admission for any cause also increased from the baseline period.
Table 1.
Characteristics of the study population: Adults with serious mental illness who are dually eligible for Medicaid and Medicare
| SC | MO | |
|---|---|---|
| Unique subjects | 1837 | 6012 |
| Person-months | 59,224 | 179,806 |
| Year of transition, N | ||
| 2004 | 598 | 1770 |
| 2005 | 566 | 1769 |
| 2006 | 396 | 1433 |
| 2007 | 277 | 1040 |
| Average Number of Months Observed | ||
| Medicaid-only | 9.9 | 10.4 |
| Dual Medicaid and Medicare | 22.4 | 19.5 |
| Mean Age (January 2004) | 39.5 | 41 |
| Male (%) | 36.2 | 38.9 |
| Non-White race (%) | 37.9 | 15.6 |
Authors' calculations using merged Medicare and Medicaid claims and enrollment data.
Table 2.
Unadjusted average monthly health care use in the Medicaid-only and Dual coverage periods
| Medicaid-only | Dual | Medicaid-only | Dual | ||
|---|---|---|---|---|---|
| Probability of Any Use (95% C.I.) | Visits, Admissions, or Days (95% C.I.) | ||||
|
|
|||||
| Missouri, N= 6,012 persons | |||||
| Outpatient | Total | 0.6 (0.59, 0.61) | 0.66** (0.65, 0.67) | 2.08 (2.01, 2.15) | 2.22** (2.15, 2.28) |
| MHSUD | 0.4 (0.39, 0.41) | 0.42** (0.41, 0.43) | 1.39 (1.33, 1.46) | 1.34 (1.28, 1.40) | |
| Emergency Department | Total | 0.11 (0.11, 0.12) | 0.14** (0.14, 0.15) | 0.15 (0.14, 0.16) | 0.20** (0.19, 0.22) |
| MHSUD | 0.03 (0.02, 0.03) | 0.03** (0.03, 0.03) | 0.03 (0.03, 0.03) | 0.04** (0.04, 0.04) | |
| Inpatient Admissions | Total | 0.05 (0.05, 0.05) | 0.05 (0.05, 0.06) | 0.05 (0.05, 0.06) | 0.06 (0.06, 0.06) |
| MHSUD | 0.02 (0.02, 0.02) | 0.03 (0.02, 0.03) | 0.02 (0.02, 0.03) | 0.03 (0.02, 0.03) | |
| Inpatient Days | Total | 0.4 (0.36, 0.44) | 0.62** (0.56, 0.69) | ||
| MHSUD | 0.21 (0.18, 0.24) | 0.37** (0.33, 0.41) | |||
| South Carolina, N=1,837 persons | |||||
| Outpatient | Total | 0.59 (0.57, 0.60) | 0.64** (0.63, 0.66) | 1.87 (1.72, 2.01) | 1.92 (1.80, 2.05) |
| MHSUD | 0.34 (0.32, 0.36) | 0.35 (0.33, 0.36) | 0.96 (0.85, 1.08) | 0.94 (0.84, 1.05) | |
| Emergency Department | Total | 0.13 (0.12, 0.14) | 0.14* (0.13, 0.15) | 0.19 (0.17, 0.20) | 0.22* (0.20, 0.24) |
| MHSUD | 0.02 (0.02, 0.03) | 0.02 (0.02, 0.03) | 0.03 (0.02, 0.04) | 0.03 (0.02, 0.03) | |
| Inpatient Admissions | Total | 0.04 (0.04, 0.05) | 0.05* (0.05, 0.05) | 0.05 (0.04, 0.05) | 0.06* (0.05, 0.06) |
| MHSUD | 0.02 (0.01,0.02) | 0.02 (0.02, 0.02) | 0.02 (0.01, 0.02) | 0.02 (0.02, 0.02) | |
| Inpatient Days | Total | 0.41 (0.34, 0.49) | 0.65** (0.54, 0.75) | ||
| MHSUD | 0.2 (0.14, 0.25) | 0.33** (0.26, 0.41) | |||
Authors' calculations using merged Medicare and Medicaid claims and enrollment data.
The frequency of use measure is unconditional and includes all monthly observations per subject. For the statistical comparison of Medicaid-only and Dual observations, Wald tests were used for binary variables and t-tests for count/continuous variable.
p < 0.01;
p<0.05.
Standard errors account for within person correlation over time.
Figure 1.
Unadjusted proportion of the population with any outpatient visit in the month. Adults with serious mental illness who transitioned from Medicaid to dual coverage, 2004–2007
Figure 2.
Unadjusted monthly emergency department and inpatient use among adults with serious mental illness who transitioned from Medicaid-only to dual coverage, 2004–2007
Adjusted Interrupted Time Series Results: Missouri
Outpatient
Controlling for the baseline Medicaid-only trend, dual coverage increased the probability of a visit by 5.56 percentage points relative to the predicted proportion of 0.61/month, a relative increase of approximately 9%.(Table 3) The number of visits increased by 0.15 visits/month or 7.2%. The probability of a MHSUD visit in the month increased by 3.8% relative to the expected proportion of 0.41/month. There was no relative increase in the number of MHSUD visits under dual coverage. (See Appendix A3 and A4 for complete regression results.)
Table 3.
Change in average monthly health care use following the transition from Medicaid-only to dual coverage among adults with psychiatric disabilities, 2004–2007
| Average Marginal Effect (se) | 1-year After Transition to Dual Coverage | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Baseline Trend | Dual Coverage | Trend Change | Predicted Outcome Absent the Transition | Predicted Absolute Change Attributable to Dual Coverage | Predicted Relative Change Attributable to Dual Coverage | |
| MISSOURI (N =175,711 person-months) | (1) | (2) | (3) | (4) | (5) | (6) |
| Any Use (Binomial-logit GEE) | Percentage | Percentage Point | Percentage Change | |||
| Outpatient, all cause | 0.03 | 5.56** | −0.08 | 61.45 | 5.56** | 9.08** |
| 0.05 | 0.50 | 0.06 | 0.50 | 0.51 | 0.89 | |
| Outpatient, MHSUD | 0.22** | 1.58** | −0.28** | 41.47 | 1.58** | 3.82** |
| 0.06 | 0.50 | 0.07 | 0.52 | 0.50 | 1.25 | |
| Emergency Dept., all cause | −0.04 | 2.34** | 0.06 | 11.28 | 2.32** | 21.61** |
| 0.03 | 0.31 | 0.04 | 0.28 | 0.30 | 3.10 | |
| Emergency Dept., MHSUD | −0.04* | 0.57** | 0.04* | 2.37 | 0.55** | 23.32** |
| 0.02 | 0.20 | 0.02 | 0.13 | 0.13 | 6.75 | |
| Inpatient, all cause | −0.05* | 0.49* | 0.05* | 4.66 | 0.48* | 10.23* |
| 0.02 | 0.20 | 0.02 | 0.18 | 0.19 | 4.36 | |
| Inpatient, MHSUD | −0.05** | 0.40** | 0.05** | 1.93 | 0.38** | 19.44** |
| 0.01 | 0.13 | 0.01 | 0.05 | 0.12 | 7.00 | |
| Quantity of Use (Gamma-log GEE) | Mean | Number | Percentage Change | |||
| Outpatient visits, all cause | 0.004 | 0.153** | −0.014** | 2.12 | 0.15** | 7.22** |
| 0.005 | 0.028 | 0.005 | 0.033 | 0.027 | 1.36 | |
| Outpatient visits, MHSUD | 0.006 | −0.013 | −0.015** | 1.39 | −0.013 | −0.91 |
| 0.004 | 0.023 | 0.005 | 0.03 | 0.022 | 1.61 | |
| Emergency department visits, all cause | −0.0004 | 0.046** | 0.0009 | 0.147 | 0.045** | 30.88** |
| 0.0006 | 0.005 | 0.0006 | 0.005 | 0.005 | 4.16 | |
| Emergency department visits, MHSUD | −0.0005* | 0.009** | 0.0005* | 0.03 | 0.01** | 32.26** |
| 0.0002 | 0.002 | 0.0002 | 0.002 | 0.002 | 8.04 | |
| Inpatient admissions, all cause | −0.0005* | 0.006** | 0.0004 | 0.05 | 0.006** | 11.07* |
| 0.0002 | 0.002 | 0.0002 | 0.002 | 0.002 | 4.54 | |
| Inpatient admissions, MHSUD | −0.0005** | 0.004** | 0.0005** | 0.02 | 0.004** | 18.09* |
| 0.0001 | 0.001 | 0.0002 | 0.001 | 0.001 | 7.21 | |
| Inpatient days, all cause | −0.006 | 0.209** | 0.009* | 0.37 | 0.20** | 54.96** |
| 0.004 | 0.036 | 0.004 | 0.028 | 0.032 | 12.33 | |
| Inpatient days, MHSUD | −0.006 | 0.165** | 0.01* | 0.19 | 0.16** | 81.34** |
| 0.004 | 0.033 | 0.004 | 0.023 | 0.028 | 22.42 | |
| SOUTH CAROLINA (N = 52,899) | (1) | (2) | (3) | (4) | (5) | (6) |
| Any Use (Binomial-logit GEE) | Average Marginal Effect (se) | Percentage | Percentage Point | Percentage Change | ||
| Outpatient, all cause | 0.33** | 2.28* | −0.33** | 62.42 | 2.25* | 3.61* |
| 0.10 | 0.94 | 0.11 | 0.91 | 0.93 | 1.54 | |
| Outpatient, MHSUD | 0.17 | 1.13 | −0.28* | 34.68 | 1.14 | 3.28 |
| 0.11 | 0.92 | 0.11 | 0.92 | 0.92 | 2.74 | |
| Emergency Dept., all cause | 0.05 | 1.09 | −0.06 | 12.75 | 1.1 | 8.64 |
| 0.07 | 0.61 | 0.07 | 0.59 | 0.61 | 5.11 | |
| Emergency Dept., MHSUD | −0.02 | 0.35 | 0.01 | 1.98 | 0.33 | 17.01 |
| 0.03 | 0.24 | 0.03 | 0.21 | 0.22 | 13.01 | |
| Inpatient, all cause | 0 | 1.01** | −0.02 | 3.77 | 1.00** | 26.60* |
| 0.04 | 0.34 | 0.04 | 0.31 | 0.32 | 10.51 | |
| Inpatient, MHSUD | −0.005 | 0.53** | −0.02 | 1.23 | 0.52* | 42.03* |
| 0.02 | 0.19 | 0.02 | 0.16 | 0.17 | 18.87 | |
| Quantity of Use (Gamma-log GEE) | Mean | Number | Percentage Change | |||
| Outpatient visits, all cause | 0.024** | −0.004 | −0.028** | 1.94 | −0.005 | −0.23 |
| 0.009 | 0.046 | 0.010 | 0.064 | 0.048 | 2.47 | |
| Outpatient visits, MHSUD | 0.011 | 0.019 | −0.015 | 0.94 | 0.019 | 2.05 |
| 0.007 | 0.033 | 0.008 | 0.052 | 0.033 | 3.66 | |
| Emergency department visits, all cause | −0.0001 | 0.018 | 0.0008 | 0.19 | 0.018 | 9.48 |
| 0.001 | 0.012 | 0.001 | 0.011 | 0.012 | 6.73 | |
| Emergency department visits, MHSUD | −0.0002 | 0.001 | −0.0001 | 0.026 | 0.0013 | 4.81 |
| 0.0004 | 0.004 | 0.0004 | 0.003 | 0.003 | 13.48 | |
| Inpatient admissions, all cause | −0.00003 | 0.012** | −0.0002 | 0.04 | 0.012** | 29.70** |
| 0.0004 | 0.004 | 0.0005 | 0.003 | 0.004 | 11.22 | |
| Inpatient admissions, MHSUD | −0.0001 | 0.006** | −00001 | 0.012 | 0.006** | 45.29* |
| 0.0002 | 0.002 | 0.0003 | 0.002 | 0.002 | 20.35 | |
| Inpatient days, all cause | 0.007 | 0.265** | −0.014 | 0.37 | 0.27** | 72.98* |
| 0.009 | 0.075 | 0.009 | 0.058 | 0.067 | 27.81 | |
| Inpatient days, MHSUD | −0.001 | 0.212** | −0.005 | 0.145 | 0.20** | 138.68* |
| 0.007 | 0.058 | 0.008 | 0.03 | 0.045 | 58.27 | |
Authors' calculations using merged Medicare and Medicaid claims and enrollment data. Table 3 results are estimated from GEE regression models that include age, sex, race, months observed pre-transition, months observed post-transition and transition year fixed effects. Quantity of use reflects unconditional use. Columns 1–3 are average marginal effects holding all other variables at their observed values. Column 4 is the predicted counterfactual 1-year after the transition. Column 5 is the average marginal effect of dual coverage 1-year after the transition where `baseline trend' and `trend change' are held at fixed values to align with 1-year post transition, and all other variables are held at their observed values. Column 6 is a function of Columns 4 and 5. Standard errors for all derived estimates were calculated using the Delta method.
p-value < 0.05;
p-value <0.01.
Emergency Department and Inpatient
The likelihood and number of total ED visits/month increased by 21.6% and 30.9% respectively after 12 months of dual coverage relative to predicted use under Medicaid. The probability of an MHSUD-related ED visit increased 23.3% from an expected proportion of 0.024/month; the number of visits increased by 32.3% relative to an expected 0.03 visits/month. One year after dual coverage, the likelihood of an inpatient admission, all-cause and MHSUD, increased by 10.2% and 19.4% respectively from expected monthly proportions of 0.047 and 0.02. The relative increase in mean total- and MHSUD- days hospitalized was large in magnitude relative to small expected values.
Adjusted Interrupted Time Series Results: South Carolina
Outpatient
The mean probability of a visit in the month increased by 2.3 percentage points compared to an expected proportion of 0.62/month, one-year after the transition. (Table 3) There was no change in the probability of an MHSUD visit or the frequency of total or MHSUD visits.
Emergency Department and Inpatient
The average probability and frequency of ED visits did not change after receipt of dual coverage. One-year after obtaining dual coverage, beneficiaries experienced a 26.6% relative increase in the likelihood of any inpatient admission from an expected proportion of 0.04/month at 12-months. The likelihood of a MHSUD-related inpatient admission increased by 0.52 percentage points from an expected proportion of 0.012, a 42% increase. The average number of inpatient admissions increased by 29.7% (0.012 admissions per month/0.04 expected admissions per month) after acquiring dual coverage. The significant increase in the mean number of MHSUD-related admissions/month mirrored the binary results. The mean inpatient days/month increased by 73% relative to an expected 0.37 days/month. The MHSUD-related inpatient days/month increased by over 100% relative to an expected 0.145 days/month at 12-months post-transition.
Discussion
We conducted the first longitudinal study examining the effects of transitioning from Medicaid-only coverage to dual Medicaid and Medicare coverage on the use of health care among adults with psychiatric disabilities. There were three notable findings. First, health care use did not decline in any service category. Second, the increases in health care use attributable to dual coverage were widespread and not concentrated in MHSUD-related services. Third, increases in hospital-based care were not transient but evident even 12 months after obtaining dual coverage. Further research is needed to ascertain the value of the increased use of care among adults with SMI after the transition to dual coverage.
Receipt of dual coverage increased the likelihood of using outpatient health care. This trend in increased use of outpatient services is consistent with our understanding that dual coverage in MO and SC increased the generosity of physician payment and covered services (in SC) relative to Medicaid-only. Additionally, the Medicare program provides a “Welcome to Medicare” visit for new beneficiaries which may contribute to the increase in probability and (in MO) frequency of outpatient care.(46) More generally, the effects of dual coverage on use of outpatient, ED and hospital-based care were not concentrated in MHSUD-related services. Although dual enrollees with SMI use a substantial amount of mental health care, it is the frequent co-occurrence of mental illness, medical and substance use disorders, and functional impairment that results in particularly high levels of health care utilization.(4)
The increased use of ED and inpatient care under dual coverage is more difficult to interpret. There were no changes in patient cost sharing for ED visits or for inpatient care received in a multi-specialty hospital. One might expect a short-term rise in ED visits following the transition to the extent that acquiring a new primary insurer temporarily disrupts treatment or access. However, in MO after 12 months ED use was substantially higher than expected, indicating a more sustained phenomenon. The increase in ED care use in MO also coincided with an increase in outpatient visits suggesting that ED care did not simply substitute for outpatient care. This complementary relationship between outpatient and ED care use is not a unique finding within publicly insured populations that experience expanded insurance coverage.(47, 48) Increased use of the ED may result from greater access to outpatient clinicians that refer patients to emergency care for acute events.
Use of inpatient care, overall and MHSUD-related, increased in both states. Among elderly Medicare populations, pent-up patient demand for elective admissions and/or a potential increase in the profitability of procedure-intensive admissions under Medicare has been offered to explain some of the increased use of inpatient services.(33) This explanation is less compelling for the observed increase in MHSUD-related admissions because they are not typically procedure-intensive or elective. Inpatient psychiatric admissions result from acute episodes of illness that are characterized by severe symptoms and/or low functioning. The increased MHSUD admissions with dual coverage in SC reflect either an increase in the incidence of acute episodes and/or an increase in the likelihood of hospitalization for any given episode. These explanations lead to very different conclusions about health care access for dual beneficiaries with SMI relative to Medicaid-only coverage in SC. A higher rate of acute psychiatric episodes after the transition may signal decreased access to treatment for dual enrollees relative to Medicaid-only beneficiaries. By contrast, dual coverage may facilitate greater contact with clinicians in general that increases the likelihood of an MHSUD inpatient admission when needed.
Several study limitations merit discussion. The acquisition of dual coverage is a collection of changes in health insurance characteristics that patients and clinicians experience including (but not necessarily limited to) changes in covered services and reimbursement. Our estimates reflect the average effect of dual coverage rather than the effect of any specific mechanism (e.g., anticipation of higher quality care.) We do not observe health care use that was entirely paid by a source other than Medicare or Medicaid. For example, Medicare coverage for long-term psychiatric stays in psychiatric hospitals may partly explain the increase in inpatient care use because this service was not covered under Medicaid-only. However, when we exclude subjects with any inpatient stay greater than 90 days before or after dual coverage, our results are consistent. (Appendix A1 and A2) Our findings may not generalize to other geographic areas or to the approximately 18 states in which the dominant medical or behavioral health delivery system for adults with disabilities in Medicaid and/or dual coverage is managed care.(49, 50)
Conclusion
Our findings demonstrate that the transition from Medicaid to dual coverage increased use of health care among beneficiaries with SMI, whose care has previously been shown to be suboptimal throughout the US.(4) Given the low rates of outpatient treatment for psychiatric and medical conditions in this vulnerable and costly population,(7, 8, 10, 11) it is likely that some patients benefitted from the increased use of outpatient care. Additional research is needed to assess the impact of this coverage change on beneficiaries' health, functioning, and satisfaction, as well as the efficiency of the resulting care. There are 50 ongoing natural experiments on the transition from Medicaid to dual coverage that researchers may exploit to answer these questions. This largely untapped research opportunity complements the lessons emerging from focused demonstration projects to improve the quality and efficiency of health care for dual beneficiaries.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge funding for this work from the National Institute of Mental Health (K01 MH 092338), the Agency for Healthcare Research and Quality (R01 HS018577) and the sponsorship of the Department of Population Medicine at Harvard Medical School where Dr. Burns began this work. Earlier versions of this paper were presented at the American Society of Health Economists Biennial Conference at the University of Southern California, June 23, 2014 and the Academy Health Disability Research Interest Group Meeting in Minneapolis, MN on June 13, 2015. We appreciate Dan Gilden's collegial and expert analytical contributions, and the very thoughtful input from 4 anonymous reviewers.
Footnotes
Conflicts: There are no potential conflicts of interest for any of the authors.
ICD-9 Codes 295.**, 296.0*–296.7*, 296.80 – 296.82, or 296.89.
References
- 1.Rupp K, Davies P, Strand A. Disabiltiy Benefit Coverage and Program Interactions in the Working-Age Population. Social Security Bulletin. 2008;68:1–30. [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission . Report to Congress: Aligning Incentives in Medicare. Washington, D.C.: 2010. pp. 1–287. [Google Scholar]
- 3.U.S. Government Accountability Office . Medicaid: A small share of enrollees consistently accounted for a large share of expenditures. Washington, D.C.: 2015. GAO-15-4604. [Google Scholar]
- 4.Frank RG, Epstein AM. Factors Associated With High Levels Of Spending For Younger Dually Eligible Beneficiaries With Mental Disorders. Health Affairs. 2014;33:1006–1013. doi: 10.1377/hlthaff.2013.0769. [DOI] [PubMed] [Google Scholar]
- 5.Buck JA, Teich JL, Bae J, et al. Mental health and substance abuse services in ten state Medicaid programs. Administration and Policy in Mental Health. 2001;28:181–192. doi: 10.1023/a:1007855901228. [DOI] [PubMed] [Google Scholar]
- 6.Riley GF, Rupp K. Expenditure Patterns Under the Four Major Public Cash Benefit and Health Insurance Programs for Working-Age Adults With Disabilities. Journal of Disability Policy Studies. 2014;25:71–80. [Google Scholar]
- 7.Druss BG, Zhao LP, Cummings JR, et al. Mental Comorbidity and Quality of Diabetes Care Under Medicaid A 50-state Analysis. Medical Care. 2012;50:428–433. doi: 10.1097/MLR.0b013e318245a528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fullerton CA, Busch AB, Normand SLT, et al. Ten-Year Trends in Quality of Care and Spending for Depression 1996 Through 2005. Archives of General Psychiatry. 2011;68:1218–1226. doi: 10.1001/archgenpsychiatry.2011.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Busch AB, Huskamp HA, Neelon B, et al. Longitudinal Racial/Ethnic Disparities in Antimanic Medication Use in Bipolar-I Disorder. Medical Care. 2009;47:1217–1228. doi: 10.1097/MLR.0b013e3181adcc4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Busch AB, Lehman AF, Goldman H, et al. Changes Over Time and Disparities in Schizophrenia Treatment Quality. Medical Care. 2009;47:199–207. doi: 10.1097/MLR.0b013e31818475b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burns ME, Busch AB, Madden JM, et al. Effects of Medicare Part D on Guideline-Concordant Pharmacotherapy for Bipolar I Disorder Among Dual Beneficiaries. Psychiatric Services. 2014;65:323–329. doi: 10.1176/appi.ps.201300123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration . Results from the 2013 National Survey on Drug Use and Health. Rockville, MD: [Accessed January 19, 2015]. 2014. Availalble at: http://www.samhsa.gov/data/sites/default/files/2013MHDetTabs/NSDUH-MHDetTabs2013.htm. [Google Scholar]
- 13.Zhang YT, Adams AS, Ross-Degnan D, et al. Effects of Prior Authorization on Medication Discontinuation Among Medicaid Beneficiaries With Bipolar Disorder. Psychiatric Services. 2009;60:520–527. doi: 10.1176/ps.2009.60.4.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu CY, Adams AS, Ross-Degnan D, et al. Association Between Prior Authorization for Medications and Health Service Use by Medicaid Patients With Bipolar Disorder. Psychiatric Services. 2011;62:186–193. doi: 10.1176/appi.ps.62.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li JM, McCombs JS, Stimmel GL. Cost of treating bipolar disorder in the California Medicaid (Medi-Cal) program. Journal of Affective Disorders. 2002;71:131–139. doi: 10.1016/s0165-0327(01)00394-9. [DOI] [PubMed] [Google Scholar]
- 16.Office of Retirement and Disability Policy . Annual statistical supplement to the Social Security Bulletin, 2013. Social Security Administration; Washington, D.C.: 2014. Document No. 13-11700. [Google Scholar]
- 17.Duggan MK, Kearney MS, Rennane S. The Supplemental Security Income (SSI) Program. NBER Working Paper. 2015;21209:1–78. [Google Scholar]
- 18.Carpenter L. Evolution of Medicaid coverage of Medicare cost sharing. Health Care Financing Review. 1998;20:11–18. [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell JB, Haber SG. State payment limitations on medicare cost-sharing: Impact on dually eligible beneficiaries. Inquiry. 2004;41:391–400. doi: 10.5034/inquiryjrnl_41.4.391. [DOI] [PubMed] [Google Scholar]
- 20.Zuckerman S, Williams AF, Stockley KE. Trends In Medicaid Physician Fees, 2003–2008. Health Affairs. 2009;28:W510–W519. doi: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 21.Hing E, Decker SL, Jamoon E. [Accessed on 11/30/15];Acceptance of new patients with public and private insurance by office-based physicians: United States, 2013. NCHS Data Brief: Centers for Disease Control and Prevention. 2015 Available at: http://www.cdc.gov/nchs/data/databriefs/db195.pdf. [PubMed]
- 22.Soumerai SB, McLaughlin TJ, Ross-Degnan D, et al. Effects of Limiting Medicaid Drug-Reimbursement Benefits on the Use of Psychotropic Agents and Acute Mental-Health-Services by Patients with Schizophrenia. New Engl J Med. 1994;331:650–655. doi: 10.1056/NEJM199409083311006. [DOI] [PubMed] [Google Scholar]
- 23.Zeber JE, Grazier KL, Blow FC, et al. The effect of a medication copayment increase on veterans with schizophrenia. Schizophrenia Bulletin. 2005;31:555–556. [PubMed] [Google Scholar]
- 24.Centers for Medicare and Medicaid Services Proposed Rule: Application of mental health parity requirements to coverage offered by Medicaid managed care organizations, the Children's Health Insurance Program(CHIP), and Alternative Benefit Plans. Federal Register 2015. 2015 Apr 10; [PubMed]
- 25.Kaiser Family Foundation . State Health Facts Medicaid Benefits [database online] Kaiser Family Foundation; Washington, D.C.: [Accessed on 8/26/14]. 2012. Available at: http://kff.org/medicaid/state-indicator/physician-services/ [Google Scholar]
- 26.Madden JM, Adams AS, LeCates RF, Ross-Degnan D, Zhang F, Huskamp HA, Gilden DM, Soumerai SB. Changes in drug coverage generosity and untreated serious mental illness: Transitioning from Medicaid to Medicare Part D. JAMA Psychiatry. 2015;72:179–188. doi: 10.1001/jamapsychiatry.2014.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Office of Inspector General . Dual eligibles' transition: Part D formularies' inclusion of commonly used drugs. Department of Health and Human Services; Washington, D.C.: 2006. Report Number OEI-05-06-00090. [Google Scholar]
- 28.Kaiser Family Foundation . State Health Facts Medicaid Benefits: Prescription Drugs [database online] Washington, D.C.: [Accessed on 12/11/15]. 2012. Available at: http://kff.org/medicaid/state-indicator/prescription-drugs/ [Google Scholar]
- 29.Social Security Act. 1905(a)(B). [Google Scholar]
- 30.Centers for Medicare and Medicaid Services . Medicaid emergency psychiatric demonstration: Demonstration design and solicitation. The CMS Innovation Center; Baltimore, MD: [Accessed on 12/5/15]. 2012. Available at: https://innovation.cms.gov/files/x/medicaidemerpsy_solicitation.pdf. [Google Scholar]
- 31.Centers for Medicare and Medicaid Services [Accessed on 11/30/15];Your Medicare Coverage. 2015 Available at : https://www.medicare.gov/coverage/inpatient-mental-health-care.html.
- 32.Decker SL. Medicare and the health of women with breast cancer. Journal of Human Resources. 2005;40:948–968. [Google Scholar]
- 33.Card D, Dobkin C, Maestas N. The Impact of Nearly Universal Insurance Coverage on Health Care Utilization: Evidence from Medicare. American Economic Review. 2008;98:2242–2258. doi: 10.1257/aer.98.5.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McWilliams JM, Zaslavsky AM, Meara E, et al. Impact of Medicare coverage on basic clinical services for previously uninsured adults. Journal of the American Medical Association. 2003;290:757–764. doi: 10.1001/jama.290.6.757. [DOI] [PubMed] [Google Scholar]
- 35.McWilliams JM, Meara E, Zaslavsky AM, et al. Use of health services by previously uninsured medicare beneficiaries. New England Journal of Medicine. 2007;357:143–153. doi: 10.1056/NEJMsa067712. [DOI] [PubMed] [Google Scholar]
- 36.Kaiser Family Foundation . State Health Facts: Medicaid Benefits Prescription Drugs [database online] Washington, D.C.: [Accessed on 12/11/15]. 2004. Available at: http://kff.org/medicaid/state-indicator/prescription-drugs/ [Google Scholar]
- 37.South Carolina Department of Health and Human Services . Medicaid Physician Provider Manual. Columbia, SC: [Accessed 09/29/2010]. 2009. pp. 1–252. Available at https://www.scdhhs.gov/provider-manual-list, 09/01/09 update. [Google Scholar]
- 38.Wharam JF, Zhang F, Landon BE, et al. Low-Socioeconomic-Status Enrollees In High-Deductible Plans Reduced High-Severity Emergency Care. Health Affairs. 2013;32:1398–1406. doi: 10.1377/hlthaff.2012.1426. [DOI] [PubMed] [Google Scholar]
- 39.Shadish W, Cook T, Campbell D. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Wadsworth; Belmont, CA: 2002. [Google Scholar]
- 40.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysisof interrupted time series studies in medication use research. J Clin Pharm Therapeutics. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 41.Fretheim A, Zhang F, Ross-Degnan D, et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. Journal of Clinical Epidemiology. 2015;68:324–333. doi: 10.1016/j.jclinepi.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 42.Hardin JW, Hilbe JM. Generalized Estimating Equations. Chapman & Hall/CRC; Boca Raton, FL: 2003. [Google Scholar]
- 43.Cui J. QIC program and model selection in GEE analyses. The Stata Journal. 2007;7:209–220. [Google Scholar]
- 44.Williams R. Using the margins command to estimate and interpret adjusted predictions and marginal effects. The Stata Journal. 2012;12:308–331. [Google Scholar]
- 45.Goldman HH, Frank RG, Burnam MA, et al. Behavioral health insurance parity for Federal Employees. New England Journal of Medicine. 2006;354:1378–1386. doi: 10.1056/NEJMsa053737. [DOI] [PubMed] [Google Scholar]
- 46.Centers for Medicare and Medicaid Services . The ABCs of the Initial Preventive Physical Examination. Baltimore, MD: [Accessed on 11/30/15]. Available at: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/MPS_QRI_IPPE001a.pdf. [Google Scholar]
- 47.DeLeire T, Dague L, Leininger L, et al. Wisconsin Experience Indicates That Expanding Public Insurance To Low-Income Childless Adults Has Health Care Impacts. Health Affairs. 2013;32:1037–1045. doi: 10.1377/hlthaff.2012.1026. [DOI] [PubMed] [Google Scholar]
- 48.Taubman SL, Allen HL, Wright BJ, et al. Medicaid Increases Emergency-Department Use: Evidence from Oregon's Health Insurance Experiment. Science. 2014;343:263–268. doi: 10.1126/science.1246183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Medicaid and CHIP Payment and Access Commission . Report to Congress on Medicaid and CHIP. Washington, D.C.: [Accessed on 12/4/15]. Jun, 2015. Available at: https://www.macpac.gov/wp-content/uploads/2015/06/June-2015-Report-to-Congress-on-Medicaid-and-CHIP.pdf. [Google Scholar]
- 50.Centers for Medicare and Medicaid Services . 2013 Enrollment data by program and population. Baltimore, MD: [Accessed 12/8/15]. Available at: http://www.medicaid.gov/medicaid-chip-program-information/by-topics/data-and-systems/medicaid-managed-care/medicaid-managed-care-enrollment-report.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.