Abstract
We conducted a feasibility study of a home telehealth system that monitored blood pressure and bodyweight. A total of 34 participants with hypertension (10 males and 24 females) had the telemedicine system installed in their homes. Their mean age was 72 years and 94% of them self-identified as Hispanic. The telehealth system transmitted blood pressure and bodyweight data to a server. There was also a messaging function that was used to send a daily reminder to the participants. Participants used the telehealth system for six months. Ten participants were lost to follow up and 24 participants completed the entire study. Participants had strong positive perceptions regarding the usability and usefulness of the telemedicine system. Most of them (92%) found the device easy to use and 96% felt that the training they received prepared them to use the device. The providers indicated that use of the system improved their ability to manage their patients. The results of the study suggest that use of the telehealth system for home monitoring in Hispanic patients with hypertension is feasible.
Introduction
Approximately one in three adults in the US has hypertension, a total of approximately 67 million people.1 Hypertension is significantly linked to heart attacks, heart failure and stroke: 69% of people who have a first heart attack, 77% of people who have a first stroke and 74% of people with chronic heart failure have high blood pressure (BP), which is also a major risk factor for kidney disease.1 Hypertension among African Americans and Hispanics is relatively high with 85% of African Americans and 74% of Hispanics aged 65 years and older having high BP.2 Hypertension represents a high economic burden for society, costing the nation $47.5 billion annually in direct medical expenses, and is also a major reason for use of ambulatory medical care facilities.1
One increasingly common approach in the management of hypertension is for patients to measure their own BP in their homes and to have this information communicated in real time to their healthcare providers. Studies have shown that home BP monitoring is as reliable as ambulatory BP monitoring and avoids the “white coat” phenomenon.3 Taking their own BP can also cause patients to think about and manage their condition. In addition, for many older people commuting to physician offices is difficult and often necessitates making arrangements for transport, which can be time consuming and stressful and lead to missed visits. The ability to avoid some of these face-to-face visits by monitoring BP at home may be beneficial for both patients and providers. Telemonitoring lends itself to a shared control model of healthcare and improves the continuity of care.4 Home monitoring of BP also enables providers to have access to larger and more continuous datasets which can improve treatment decision-making.
However, home monitoring of BP may be challenging for older adults with limited experience of technology or those who live alone with little support. In addition, for many older adults who are managing their condition at home, a critical factor, apart from monitoring their BP, is to have their BP and bodyweight information remotely monitored as part of their treatment strategy. This can add to the complexity of the demands of the monitoring task as it typically entails use of more equipment. Even though studies have shown that telehealth can be used to help manage BP,5 there is limited evidence about the efficacy of these systems with older adults. One concern is whether elderly people would be able to successfully use more advanced telehealth equipment that incorporates messaging functions, such as reminders from providers. Another concern is how elderly users will cope with system malfunctions. Finally, the willingness of healthcare providers to monitor and interact with the complex data management systems that complement these systems also needs to be considered.
We conducted a feasibility study to identify problems associated with the implementation and functioning of a home telehealth system. We also studied the participants’ experience in using the system.
Methods
The system allowed measurements of the patient’s BP and bodyweight to be sent to health care providers at a healthcare clinic. It also enabled the providers to send pre-defined daily reminder messages to patients regarding their BP measurement. Our goal was to study the use of the system by older adults who were primarily Hispanic. The number of Hispanic older adults is expected to increase to about 17 million people by 2050.6 Hypertension is more common among minorities and disparities in access to healthcare are common among ethnic minorities, especially Hispanics.7
The study participants were receiving home care from an independent non-profit home care service (HCS), which specialized in home care for the elderly. All HCS staff members were certified as chronic care professionals.
Telehealth system
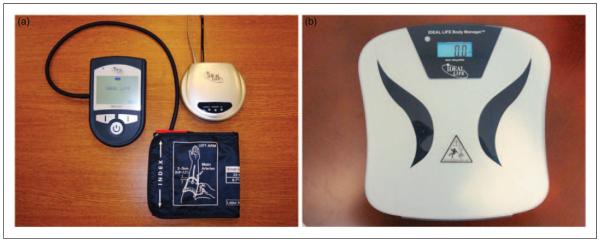
The telehealth system (IDEAL Life, Toronto, Canada) consisted of three devices: a blood pressure measuring unit, a bodyweight scale and a wireless unit to transmit the data to a website through a telephone line (Figure 1). The HCS nurses were trained to use the database management system to monitor their clients’ data.
Figure 1.
Telehealth system – patient equipment (a) Blood pressure measuring unit (left) and wireless transmission unit (top right); (b) Bodyweight scale.
The BP device contained a display, which enabled the participants to receive a daily greeting message reminding them to take BP and weight readings. Participants were instructed to take a daily reading of their BP and weight. The time of the reminder was programmed into the device as was an individually tailored BP reading alert plan for systolic and diastolic BP readings, which was determined by the HCS nurse in consultation with the participants’ physicians. An alert email was sent to the HCS nurse when the participant had two consecutive out of range BP readings. A message was also displayed on the participant’s BP device instructing them to relax and take a reading again in 45 min. The HCS nurse contacted the participant with further instructions if the BP readings remained high.
Inclusion/exclusion criteria
Study participants were aged 55 years or older and had been treated for hypertension for at least one year (systolic blood pressure >140 mmHg, diastolic blood pressure >90 mmHg),8 and were receiving home care services from the HCS agency but were not monitoring their own BP. Additional inclusion criteria were having a telephone line in the home and able to provide written consent. The exclusion criteria were: having a history of myocardial infarction, stroke or congestive heart failure within six months prior to study enrolment; visual or motor impairments sufficiently severe to preclude home BP monitoring; being wheel-chair bound; being cognitively impaired; or exhibiting symptoms of depression.
Potential participants were screened at the initial home assessment, using the Mini Mental State Examination (MMSE).9 A criterion was set at ⩾26 for the MMSE (age and education corrected). Participants also had to have a score of <17 on the Center for Epidemiologic Studies Depression Scale (CES-D).10
Procedure
A baseline assessment was conducted for participants who met the inclusion criteria. An assessor, who was trained in administration of the measurement battery, conducted the assessment in the patient’s home. Participants were initially presented with the informed consent form, which was also verbally explained to them. They were then administered the MMSE and the CESD, and those who were eligible completed the assessment battery (Table 2). All materials were available in English and Spanish, and the study assessors were bi-lingual.
Table 2.
The patient assessment tests.
| Description | Baseline | Follow-up | |
|---|---|---|---|
| Demographic Questionnaire15 | 16 questions related to age, education, occupational status, income, culture ethnicity, living arrangements and perceptions of health and health functioning. |
X | |
| Test of Functional Health Literacy in Adults (STOFHLA)16 |
The STOFHLA rates ability to perform health-related tasks requiring reading and computational skills. It contains 4 numeracy items and 2 prose passages. Scores range from 0 to 36; 0-16 inadequate health literacy; 17-22 marginal health literacy and 18-36 adequate health literacy. |
X | |
| Functional Health and Well-being (SF-36)17 |
A 36-item questionnaire that assesses 8 different dimensions of health and well-being. |
X | X |
| Formal Care and Services Utilization18 |
A 13-item questionnaire with questions about the type (e.g. homemaker, home health aide, transportation, senior day care) and frequency of services received during the past month. A higher score reflects greater service use. |
X | X |
| Technology, Computer, Internet Experience Questionnaire15 |
36 questions to assess use of technology and experience with computer technology and the Internet. |
X | X |
| System Evaluation Questionnaire (developed for the present study) |
A 13-item instrument to measure participants’ satisfaction with the telemedicine system, and the training they received to use it. Responses for each question ranged from strongly agree to strongly disagree. |
X |
Following the baseline assessment, the assessor installed the telemedicine system in the participant’s home and instructed the participant how to use it. Two practice measurements were taken to ensure consistency in readings. The assessor then instructed the participant on use of the bodyweight scale and asked the participant to weigh him or herself on the scale several times to ensure consistency in readings. The assessor also verified that the readings were being transmitted to the data management system.
Participants were instructed to take daily measurements. They were informed that a nurse from their HCS would be monitoring their BP remotely during normal working hours (08:00–17:00, Monday-Friday) and would contact them if they saw any atypical changes in their measurements. Participants were encouraged to call the assessor if they had questions or technical problems. Participants were also instructed that that they would complete a follow-up assessment following use of the system for six months.
Participants completed a follow-up assessment six months after the intervention period, which included six assessment instruments (see Table 2). The System Evaluation Questionnaire, a 13-item instrument, was designed to measure participants’ satisfaction with the telemedicine system (Appendix). Lower scores reflected more positive perceptions, with scores in the range 13–65. A trained assessor administered the tests.
Appendix.
System Evaluation Questionnaire. The following questions refer to the user’s experience with the blood pressure monitoring device.
| Item | Response* |
|---|---|
| 1. I feel that this device provides me with extra security knowing that my provider has an easier ability to monitor my blood pressure. |
|
| 2. I feel comfortable using this device to monitor my blood pressure. | |
| 3. This device was easy to use. | |
| 4 .The training I received prepared me to use this device. | |
| 5. I had trouble remembering how to use this device. | |
| 6. I felt that the use of this device helped me to better manage my health. | |
| 7. I felt that the device helped me be more compliant in following my medical plan. | |
| 8. I feel that my health is better today as a result of using this device. | |
| 9. I would recommend the use of this device to other patients. | |
| 10. I had concerns about where my information was being sent and who was looking at my information. | |
| 11. I felt that my blood pressure information was just as private using this device as when I had my blood pressure taken in my physician’s office. |
|
| 12. I feel that the use of this device has made it easier for me to manage my blood pressure. | |
| 13. Use of this device has made me more knowledgeable of my health. |
Strongly agree, Agree, Neither agree nor disagree, Disagree, Strongly disagree.
At the conclusion of the study, a study investigator conducted a telephone survey and interview with the two HCS nurses who were responsible for monitoring remotely the data from the participants. Responses to the survey and interview were transcribed verbatim. The survey consisted of 15 items in the form of statements, to which the nurses indicated their degree of agreement on a 5-point scale ranging from strongly agree to strongly disagree. The items were related to training, the usefulness of the system with respect to patient compliance, comfort using the system, concerns about privacy, usability of the system, confidence in the data being transmitted, the patients’ ability to use the system and perceptions of the impact of use of the system on patient management activities. The interview addressed three areas: system likes and dislikes, and suggestions for system improvements.
The patients received $30 for completing the baseline assessment, and were informed that they would receive an additional $30 if they completed the six-month assessment. The appropriate ethics committee approved the study.
Results
A total of 34 participants (10 males and 24 females) met the inclusion criteria and were willing to have the telemedicine system in their homes. Their mean age was 72 years (SD 11) and 94% of them self-identified as Hispanic. The participants had fairly low educational attainment and only 50% had any prior computer experience (Table 1).
Table 1.
Baseline characteristics (n=34).
| Number (%) | |
|---|---|
| Mean age, years (SD) | 72 (11) |
| Gender | |
| Male (%) | 10 (29) |
| Female (%) | 24 (71) |
| Education | |
| Less or equal to high school (%) | 17 (50) |
| Some college (%) | 9 (27) |
| College (%) | 8 (23) |
| Ethnicity | |
| Hispanic (%) | 32 (94) |
| Non-Hispanic White (%) | 1 (3) |
| Non-Hispanic Black (%) | 1 (3) |
| Computer experience (%) | 17 (50) |
| Internet experience (%) | 15 (44) |
| In general, would you say your health is | |
| Poor (%) | 5 (15) |
| Fair (%) | 17 (50) |
| Good (%) | 12 (35) |
| Compared to other people of your age, your health is |
|
| Poor (%) | 5 (15) |
| Fair (%) | 11 (32) |
| Good (%) | 14 (41) |
| Very good (%) | 4 (12) |
| How satisfied are you with your present health? | |
| Not satisfied (%) | 14 (41) |
| Neutral (%) | 3 (10) |
| Satisfied (%) | 17 (50) |
Participants used the telehealth system for six months. Of the 34 initial participants, ten were lost at the six-month follow-up assessment due to illness, relocation or loss of interest in the study. Thus there were 24 participants who completed the entire study (9 males and 15 females). Their mean age was 71 years (range 54–88).
Using a criterion of 40% adherence to the BP protocol (i.e. a BP measurement was taken on at least 40% of the 180 days of the data collection protocol), the 24 participants were divided into two groups: an Adherence group and a Non-adherence group. There were 12 participants in each group. We used a criterion of 40% as this clearly separated those who adhered to the measurement protocol from those who did not. There were no significant correlations between degree of adherence and either technology experience, computer experience, Internet experience, health literacy or income.
A mixed design repeated measures analysis of variance procedure (SPSS version 21) was used to test for differences between the two time periods (baseline and six months), between the two groups (adherers and non-adherers), and for the interaction between group and time period. A significant effect was found for time period for the 10-item Functional Health questionnaire (P=0.012), such that participants reported worse health over time, with the non-adherence group reporting worse health. There were no significant effects for the overall SF-36. We also examined the physical health functioning subscale of the SF-36 and found a significant effect of time period. Specifically, physical functioning was perceived to be significantly worse at six months relative to baseline (P=0.005), with participants in the non-adherence group indicating more decline (from 46.7 to 37.1 compared to 55.0 to 51.3 for the adherers). For the 15-item Formal Care and Services questionnaire, the group effect approached significance (P=0.078) in the direction of a greater use of services by the participants in the adherence group. Finally, a significant effect of time period was found for the measure of technology experience (P=0.006), with both groups indicating significantly greater use of technology at six months as compared to baseline.
Evaluation by participants
The median response scores on the System Evaluation questionnaire were 22.5 (interquartile range, IQR=14.5 – 28.3) for the adherence group and 27.0 (IQR=19.0 – 28.0) for the non-adherence group, indicating relatively strong positive perceptions regarding the usability and usefulness of the telemedicine system. Most of the participants (92%) found the device to be easy to use and 96% felt that the training they received prepared them to use the device. The majority of the participants (92%) also felt that use of the device made them more compliant in following their medical plan and made them more knowledgeable about their health. Further, 67% felt that use of the device improved their health. Most of the participants (96%) indicated that they would strongly recommend the use of the device to other patients. A few participants indicated that they had trouble remembering how to use the device and expressed concerns about where their information was being sent and who was looking at the information. We examined differences between adherers and non-adherers in responses to the evaluation questionnaire using the Mann Whitney U test and found no significant differences (Table 3).
Table 3.
Evaluation by participants.
| Non-adherer (n=12) |
Adherer (n=12) |
Overall (n=24) |
|
|---|---|---|---|
| I feel the device provides me with extra security knowing that my provider has an easier ability to monitor my blood pressure. |
|||
| Strongly agree/Agree | 11 (92) | 10 (83) | 21 (88) |
| Neutral | 1 (8) | 1 (8) | 2 (8) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
| I feel comfortable using this device to monitor my blood pressure. | |||
| Strongly agree/Agree | 12 (100) | 11 (92) | 23 (96) |
| Neutral | 0 (0) | 0 (0) | 0 (0) |
| Strongly disagree/Disagree | 0 (0) | 1(8) | 1 (4) |
| The device was easy to use. | |||
| Strongly agree/Agree | 11 (92) | 11 (92) | 22 (92) |
| Neutral | 0 (0) | 0 (0) | 0 (0) |
| Strongly disagree/Disagree | 1 (8) | 1 (8) | 2 (8) |
| The training I received prepared me to use this device. | |||
| Strongly agree/Agree | 11 (92) | 12 (100) | 23 (96) |
| Neutral | 0 (0) | 0 (0) | 0 (0) |
| Strongly disagree/Disagree | 1 (8) | 0 (0) | 1 (4) |
| I had trouble remembering how to use this device. | |||
| Strongly agree/Agree | 2 (16) | 2 (16) | 4 (16) |
| Neutral | 1 (8) | 1 (8) | 2 (8) |
| Strongly disagree/Disagree | 9 (75) | 9 (75) | 18 (75) |
| I felt that the use of this device helped me to better manage my health. |
|||
| Strongly agree/Agree | 11 (92) | 11 (92) | 22 (92) |
| Neutral | 0 (0) | 1 (8) | 1 (4) |
| Strongly disagree/Disagree | 1 (8) | 0 (0) | 1 (4) |
| I felt that the device helped me be more compliant in following my medical plan. |
|||
| Strongly agree/Agree | 11 (92) | 11 (92) | 22 (92) |
| Neutral | 1 (8) | 0 (0) | 1 (4) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
| I feel that my health is better today as a result of using this device. | |||
| Strongly agree/Agree | 6 (50) | 10 (83) | 16 (67) |
| Neutral | 6 (50) | 1 (8) | 7 (29) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
| I would recommend the use of this device to other patients. | |||
| Strongly agree/Agree | 12 (100) | 11 (92) | 23 (96) |
| Neutral | 0 (0) | 0 (0) | 0 (0) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
| I had concerns about where my information was being sent and who was looking at my information. |
|||
| Strongly agree/Agree | 2 (16) | 4 (33) | 6 (26) |
| Neutral | 1 (8) | 2 (16) | 3 (13) |
| Strongly disagree/Disagree | 8 (72) | 6 (50) | 14 (61) |
| I felt that my blood pressure information was just as private using this device as when I had my blood pressure taken in my physician’s office. |
|||
| Strongly agree/Agree | 10 (83) | 9 (75) | 19 (79) |
| Neutral | 0 (0) | 2 (16) | 2 (8) |
| Strongly disagree/Disagree | 2 (16) | 1 (8) | 3 (13) |
| I feel that the use of this device has made it easier for me to manage my blood pressure. |
|||
| Strongly agree/Agree | 10 (83) | 11 (92) | 21 (88) |
| Neutral | 2 (16) | 0 (0) | 2 (8) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
| Use of this device has made me more knowledgeable of my health. | |||
| Strongly agree/Agree | 11 (92) | 11 (92) | 22 (92) |
| Neutral | 1 (8) | 0 (0) | 1 (4) |
| Strongly disagree/Disagree | 0 (0) | 1 (8) | 1 (4) |
Values in parentheses are percentages.
Evaluation by nurses
Both nurses assigned a score of 3 or higher to each of the 15 items (Nurse 1, mean=3.9; Nurse 2, mean=4.1), indicating a fairly positive response overall (Table 4). Both nurses indicated that they would recommend the use of the device and felt that the use of the system made them more knowledgeable about their patients’ health.
Table 4.
Evaluation by nurses (n=2).
| Agree | Neutral | Disagree | |
|---|---|---|---|
| I felt that the system made it easier for me to monitor my patient’s/client’s blood pressure. |
2 (100) | 0 (0) | 0 (0) |
| I did not feel comfortable using this system to monitor my patient’s/client’s blood pressure. |
0 (0) | 0 (0) | 2 (100) |
| The system was easy to use. | 2 (100) | 0 (0) | 0 (0) |
| The training I received prepared me to use this system. | 1 (50) | 1 (50) | 0 (0) |
| I had trouble remembering how to use this system. | 0 (0) | 0 (0) | 2 (100) |
| I felt that the use of this system helped me to better manage my patient’s/client’s health. |
2 (100) | 0 (0) | 0 (0) |
| I felt that the blood pressure device helped my patient’s/client’s to be more compliant in following their medical plan. |
1 (50) | 1 (50) | 0 (0) |
| I felt that the patient’s’ use of the blood pressure device helped to improve their health. |
1 (50) | 1 (50) | 0 (0) |
| I would recommend the use of this device to other patient’s/client’s. | 2 (100) | 0 (0) | 0 (0) |
| I had concerns about the privacy of my patient’s/client’s information using this system. |
0 (0) | 0 (0) | 2 (100) |
| I did not feel that the use of the blood pressure monitoring device helped my patient’s/client’s better manage their health. |
0 (0) | 0 (0) | 2 (100) |
| I did not feel confident that I was receiving accurate information from the blood pressure monitoring device. |
0 (0) | 0 (0) | 2 (100) |
| I felt confident that my patient’s/client’s were able to use the blood pressure monitoring device. |
1 (50) | 1 (50) | 0 (0) |
| I did not feel that the use of this device has made it easier for my patient’s/client’s to manage their blood pressure. |
0 (0) | 0 (0) | 2 (100) |
| I feel that the use of the system made me more knowledgeable about my patient’s/ client’s health. |
2 (100) | 0 (0) | 0 (0) |
Values in parentheses are percentages.
The nurses felt that the greatest benefit of the system was that it helped prevent hospital readmissions. They also found the bodyweight scale useful. Both nurses found the alert messages to be very useful. Their main dislike was that the bodyweight scale required frequent recalibration. One of the nurses felt that this contributed to a degree of mistrust in the system by some patients. The nurses were in agreement that the most important improvement was to ensure that the weight scale could be calibrated more easily.
Discussion
The present study examined the feasibility and acceptability of a telehealth system intended to enable frail, hypertensive and predominantly Hispanic older adults receiving care from a home care service to make BP and bodyweight measurements in their home while being monitored remotely by their HCS nurses. The results indicated that the participants were receptive to and able to use the system. The findings also suggest that use of the system resulted in improvements in their self-reported health management behaviours. For example, most participants indicated that use of the system facilitated their ability to manage their health and that their health was better because of it. In addition, almost all of the participants reported that the BP device was relatively easy to use. The providers also found the system to be beneficial. They noted that use of the system facilitated their ability to monitor their patient’s health and prevented many hospital readmissions.
Although there was no effect on self-reported measures of health, the data indicated a trend toward use of more healthcare services over time among people who had higher rates of adherence to the measurement protocol. This suggests the possibility that use of the system heightened awareness of their health and thus induced them to use more health related services. The majority of the participants (92%) indicated that use of the system increased awareness of their health. Examining this data more closely showed that those who had higher adherence rates were more likely to strongly agree with this statement. However, the health of both groups generally declined over time. Both groups also reported greater technology experience at six months. This finding is important in view of the proliferation of technology in health care. Our data11 indicate that experience with technology can result in more positive attitudes towards technology.
Although the telemedicine equipment was modern, we experienced some challenges with the implementation of the system and system reliability. For example, many participants had low incomes and lived in crowded conditions, and sometimes the use of the telephone in these homes interfered with the transmission of measurement data. Problems with data transmission also occurred due to equipment failure. In addition, movement of furniture in the home sometimes resulted in equipment becoming disconnected and participants were unaware of the disconnection. There were also difficulties in calibrating the scales and there were complaints by some participants about the extensive time the device sometimes required for a measurement to be recorded. Technical and logistical problems should be expected with any sophisticated equipment that is expected to transmit data remotely from various locations, especially with low-income older adults many of whom lived alone.
Overall, these challenges are viewed as lessons learned that can be incorporated into future and larger-scale studies. These challenges also need to be taken into consideration by system designers for the design of future systems. In particular, they need to consider the needs, preferences and abilities of diverse populations of older adults in the design of telehealth systems. The prevalence of hypertension is higher among older adults who are of lower socio-economic status. The likelihood of living alone increases with age and is more prevalent among those over the age of 75 years.6 In this regard our findings point to the importance of incorporating a user-centred design approach in the design of telemedicine systems and including the needs and abilities of diverse samples of older adults in the design process. They also underscore the importance of training and the need for technical support for users of these systems. As noted by Charness12 the benefit of telehealth systems is increased if the system is designed to work in symbiosis with the person being monitored.
Despite the challenges encountered, half of the 24 participants who completed the study achieved adherence rates in the use of the BP monitoring system of at least 40% over a six-month period. This suggests that the prospects for achieving successful outcomes in compliance with telemedicine technologies are relatively high. In fact, problems with non-adherence to health management protocols are common among people with this condition. For example, Lee and colleagues,13 in a study investigating the efficacy of a mobile phone health application for elderly patients with diabetes, required participants to monitor blood glucose levels four times per day but patients only averaged twice per day. Charness and colleagues14 had an adherence rate of greater than 80% with a small sample of older adults using a multi-component home monitoring system. However, the participants received daily telephone reminders. In our case the participants received a reminder via the system. Also, our sample was older, largely minority and somewhat frail. In addition, the majority had limited technical experience and low levels of education. Our participants also indicated that their health declined over the course of the study, which may have contributed to lower rates of adherence. The sample in the Charness study was relatively healthy.
With an increasing population of elderly adults and the high prevalence of chronic disease, home healthcare is important to allow people to remain at home and not in institutional settings. Our study suggests that telehealth systems have potential in terms of helping older adults to manage conditions such as hypertension at home. However, the present study had some limitations. The sample size was relatively small and the patients were mainly Hispanic older adults living in an urban setting. Clearly, the system needs to be evaluated with a larger and more diverse sample in other settings. In addition, our focus was primarily on feasibility, and clinical outcomes now need to be evaluated. Finally, studies are needed to examine the cost effectiveness of home telehealth systems.
Acknowledgments
This research was supported by NIH/NIA grant P01-AG017211.
References
- 1.Centers for Disease Control and Prevention High Blood Pressure Facts. See http://www.cdc.gov/bloodpressure/facts.htm (last checked 10 March 2014)
- 2.Centers for Disease Control and Prevention Hypertension, ages 20+: US, 1988–2010. See http://205.207.175.93/HDI/TableViewer/tableView.aspx?ReportId=75 (last checked 10 March 2014)
- 3.Stergiou GS, Argyraki KK, Moyssakis I, et al. Home blood pressure is as reliable as ambulatory blood pressure in predicting target-organ damage in h pertension. Am J Hypertens. 2007;20:616–21. doi: 10.1016/j.amjhyper.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 4.Archer N, Fevrier-Thomas U, Lokker C, McKibbon KA, Straus SE. Personal health records: a scoping review. J Am Med Inform Assoc. 2011;18:515–22. doi: 10.1136/amiajnl-2011-000105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bondmass M, Bolger N, Castro G, Avitall B. The effect of home monitoring and telemanagement on blood pressure control among African Americans. Telemed J. 2000;6:15–23. [Google Scholar]
- 6.Administration on Aging A Statistical Profile of Hispanic Older Americans Aged 65+ See http://www.aoa.gov/AoARoot/Aging_Statistics/Minority_Aging/Facts-on-Hispanic-Elderly.aspx (last checked 10 March 2014)
- 7.Agency for Healthcare Research and Quality Disparities in Healthcare Quality Among racial and Ethnic Minority Groups: Selected Findings from the 2010 National Healthcare Quality Disparities Reports. See http://www.ahrq.gov/research/findings/nhqrdr/nhqrdr10/minority.pdf (last checked 10 March 2014)
- 8.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 11.Czaja SJ, Sharit J. Age differences in attitudes toward computers. J Gerontol B Psychol Sci Soc Sci. 1998;53:P329–40. doi: 10.1093/geronb/53b.5.p329. [DOI] [PubMed] [Google Scholar]
- 12.Charness N. Utilizing technology to improve older adult health. Occup Ther Health Care. 2014;28:21–30. doi: 10.3109/07380577.2013.865859. [DOI] [PubMed] [Google Scholar]
- 13.Lee HJ, Lee SH, Ha KS, et al. Ubiquitous healthcare service using Zigbee and mobile phone for elderly patients. Int J Med Inform. 2009;78:193–8. doi: 10.1016/j.ijmedinf.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 14.Charness N, Fox M, Papadopoulos A, Crump C. Metrics for assessing the reliability of a telemedicine remote monitoring system. Telemed J E Health. 2013;19:487–92. doi: 10.1089/tmj.2012.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Czaja SJ, Charness N, Fisk AD, et al. Factors predicting the use of technology: findings from the Center for Research and Education on Aging and Technolog Enhancement (CREATE) Psychol Aging. 2006;21:333–52. doi: 10.1037/0882-7974.21.2.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 17.Ware JE. SF-36 health survey update. Spine (Phila Pa 1976) 2000;25:3130–9. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 18.Wisniewski SR, Belle SH, Coon DW, et al. The Resources for Enhancing Alzheimer’s Caregiver Health (REACH): project design and baseline characteristics. Psychol Aging. 2003;18:375–84. doi: 10.1037/0882-7974.18.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]