Abstract
Background
The U.S. national standards for culturally and linguistically appropriate services (CLAS) in health care provide guidelines on policies and practices aimed at developing culturally competent systems of care. The Cultural Competency Assessment Tool for Hospitals (CCATH) was developed as an organizational tool to assess adherence to the CLAS standards.
Purposes
First, we describe the development of the CCATH and estimate the reliability and validity of the CCATH measures. Second, we discuss the managerial implications of the CCATH as an organizational tool to assess cultural competency.
Methodology/Approach
We pilot tested an initial draft of the CCATH, revised it based on a focus group and cognitive interviews, and then administered it in a field test with a sample of California hospitals. The reliability and validity of the CCATH were evaluated using factor analysis, analysis of variance, and Cronbach’s alphas.
Findings
Exploratory and confirmatory factor analyses identified 12 CCATH composites: leadership and strategic planning, data collection on inpatient population, data collection on service area, performance management systems and quality improvement, human resources practices, diversity training, community representation, availability of interpreter services, interpreter services policies, quality of interpreter services, translation of written materials, and clinical cultural competency practices. All the CCATH scales had internal consistency reliability of .65 or above, and the reliability was .70 or above for 9 of the 12 scales. Analysis of variance results showed that not-for-profit hospitals have higher CCATH scores than for-profit hospitals in five CCATH scales and higher CCATH scores than government hospitals in two CCATH scales.
Practice Implications
The CCATH showed adequate psychometric properties. Managers and policy makers can use the CCATH as a tool to evaluate hospital performance in cultural competency and identify and target improvements in hospital policies and practices that undergird the provision of CLAS.
Keywords: CLAS standards, cultural competency, diversity management
Culture can be viewed as an “integrated pattern of learned beliefs and behaviors” shared by individual members of a group that can affect styles of communication, interpersonal relationships, values, and customs (Betancourt, Green, & Carrillo, 2002). Various sociocultural factors, such as race or ethnicity, nationality, language, gender, and socioeconomic status, embody the cultural background of an individual. Culture is central in the delivery of health care services, because it can influence patients’ health beliefs, medical practices, attitudes toward medical care, and levels of trust (Betancourt et al., 2002; Office of Minority Health [OMH], 2001). Cultural differences can ultimately impact how health information is received, understood, and acted upon (Anderson, Scrimshaw, Fullilove, Fielding, & Normand, 2003). Clinical barriers occur when cultural differences are not adequately addressed in health care delivery, resulting in lower access and quality of care for culturally diverse populations (Cooper & Roter, 2003). For example, prior studies have shown racial or ethnical differences in hospital treatment (Harris, Andrews, & Elixhauser, 1997; Petersen, Wright, Peterson, & Daley, 2002) and patient experiences with hospital care (Hicks et al., 2005; LaVeist, Nickerson, & Bowie, 2000).
As such, addressing cultural differences becomes imperative in an increasingly diverse population, and health care organizations (HCOs) are espousing cultural competency as an organizational strategy (Ngo-Metzger et al., 2006; Weech-Maldonado, Al-Amin, Nishimi, & Salam, 2011). On the basis of an extensive review of the literature and consensus from a cultural competency steering committee, the National Quality Forum (NQF, 2008) recently defined cultural competency as the “ongoing capacity of health care systems, organizations, and professionals to provide for diverse patient populations high-quality care that is safe, patient and family centered, evidence based, and equitable.” Cultural competency is achieved through “policies, learning processes, and structures by which organizations and individuals develop the attitudes, behaviors, and systems that are needed for effective cross-cultural interactions” (NQF, 2008).
The national standards for culturally and linguistically appropriate services (CLAS) in health care, set forth by the U.S. Department of Health and Human Services (DHHS) OMH, provide guidelines on policies and practices aimed at developing culturally appropriate systems of care (OMH, 2001). The 14 CLAS standards are categorized into three themes: culturally competent care (Standards 1–3), language access services (Standards 4–7), and organizational supports for cultural competence (Standards 8–14). The CLAS standards in essence provide a roadmap for HCOs to achieve cultural competency within their care delivery systems. Ultimately, the goal of CLAS is to improve access to health services for culturally diverse populations and facilitate the elimination of racial or ethnic disparities in health (OMH, 2001). To stimulate this, a method to quantify and compare hospitals’ cultural competency based on the CLAS standards is needed. As such, the Cultural Competency Assessment Tool for Hospitals (CCATH) was developed as an organizational tool to assess adherence to the CLAS standards.
Several contributions to the extant literature were made by this article. First, we describe the development of the CCATH and estimate the reliability and validity of the CCATH measures. Second, we discuss the managerial implications of the CCATH as an organizational tool to assess cultural competency. This furthers the work of other organizations, such as the National Center for Cultural Competence at Georgetown University, which has developed similar organizational assessment tools for human service organizations.
National Standards for CLAS
The CLAS standards were developed in a two-stage process sponsored by the DHHS OMH. In the first stage, the Resources for Cross Cultural Health Care and the Center for the Advancement of Health were asked to review and compare existing cultural and linguistic competence standards and propose a draft of the national standard language where appropriate. Twenty-one recommended standards were produced using a combination of content coding and content analysis techniques. The recommended standards were reviewed by a national advisory committee constituted by representatives from federal and state health agencies, provider groups, and academic research. This group made recommendations for consolidation of the number of standards and making the language of the standards more concise, resulting in a revised set of 14 standards. The revised set of standards was presented to a focus group convened at the October 1998 national conference, Quality Health Care for Diverse Populations, for additional feedback and revisions. In the second stage of the process, the draft of the CLAS standards underwent a national process of public comment. This resulted in a significant input from stakeholder groups on the draft standards and a final revision of the standards in 2000 (OMH, 2001).
Conceptual Framework
The open systems perspective views organizations interacting with their environment to secure resources, process them, and produce some type of output. To survive, it is critical that organizations respond to the demands of their environment to ensure a continuous inflow of resources (Scott & Davis, 2007). For HCOs, the community is the major resource supplier. Therefore, HCOs have to adapt to the changing community needs to ensure their survival.
Related to the open systems perspective is the organizational systems approach. In this approach, the HCO is viewed as a system comprised of interrelated and interdependent subsystems, such as patient care, ancillary services, professional staff, financial, informational, physical, and administrative subsystems (Longest, Rakich, & Darr, 2000). Successful implementation of cultural competency requires an organizational commitment toward a systems approach (Curtis, Dreachslin, & Sinioris, 2007); HCOs that strive toward a systems approach integrate cultural competency practices throughout their management and clinical subsystems. Furthermore, HCOs engage their communities in meaningful participation in the organization’s decision making and power structures.
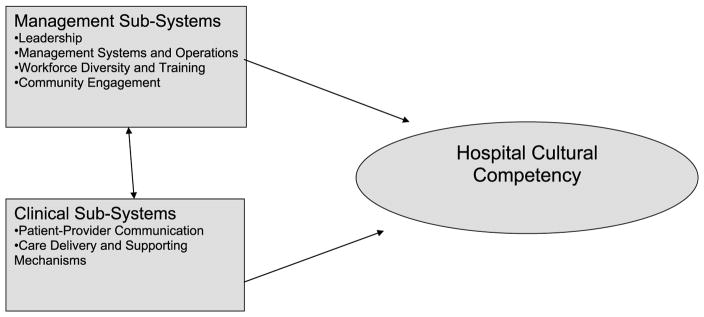
Restructuring the organizational processes to better serve a diverse patient population requires the adoption of a holistic framework. In this section, we provide such a framework. Based on NQF’s (2008) “Comprehensive framework and preferred practices for measuring and reporting cultural competency,” we propose six domains for hospital cultural competency: (a) leadership, (b) integration into management systems and operations, (c) work-force diversity and training, (d) community engagement, (e) patient–provider communication, and (f) care delivery and supporting mechanisms. Although the first four domains pertain to management subsystems, the latter two are considered clinical subsystems. On the basis of the systems approach, organizations become culturally competent by adapting their management and clinical subsystems to the needs of a more diverse workforce and patient population (Figure 1). In this section, we also discuss how the CLAS standards relate to the proposed cultural competency domains (Table 1).
Figure 1.
Organizational subsystems and hospital cultural competency
Table 1.
NQF cultural competency domains, CCATH subdomains, and CLAS standards
| NQF domains | CCATH subdomains | CLAS standards |
|---|---|---|
| Leadership | Leadership and strategic planning | 8. HCOs should develop, implement, and promote a written strategic plan that outlines clear goals, policies, operational plans, and management accountability or oversight mechanisms to provide CLAS. |
| 14. HCOs are encouraged to regularly make available to the public information about their progress and successful innovations in implementing the CLAS standards and to provide public notice in their communities about the availability of this information. | ||
| Integration into management systems and operations | Data collection on inpatient population | 10. HCOs should ensure that data on the individual patient’s or consumer’s race, ethnicity, and spoken and written language are collected in health records, integrated into the organization’s management information systems, and periodically updated. |
| Data collection on service area | 11. HCOs should maintain a current demographic, cultural, and epidemiological profile of the community as well as a needs assessment to accurately plan for and implement services that respond to the cultural and linguistic characteristics of the service area. | |
| Performance management systems and QI | 9. HCOs should conduct initial and ongoing organizational self-assessments of CLAS-related activities and are encouraged to integrate cultural and linguistic competence-related measures into their internal audits, performance improvement programs, patient satisfaction assessments, and outcome-based evaluations. | |
| Workforce diversity and training | Human resources practices | 2. HCOs should implement strategies to recruit, retain, and promote at all levels of the organization a diverse staff and leadership that are representative of the demographic characteristics of the service area. |
| Diversity training | 3. HCOs should ensure that staff at all levels and across all disciplines receive ongoing education and training in CLAS delivery. | |
| 13. HCOs should ensure that conflict and grievance resolution processes are culturally and linguistically sensitive and capable of identifying, preventing, and resolving cross-cultural conflicts or complaints by patients or consumers. | ||
| Community engagement | Community representation | 12. HCOs should develop participatory, collaborative partnerships with communities and utilize a variety of formal and informal mechanisms to facilitate community and patient/consumer involvement in designing and implementing CLAS-related activities. |
| Patient–provider communication | Availability of interpreter services | 4. HCOs must offer and provide language assistance services, including bilingual staff and interpreter services, at no cost to each patient or consumer with LEP at all points of contact, in a timely manner during all hours of operation. |
| Interpreter services policies | 5. HCOs must offer and provide to patients or consumers in their preferred language both verbal offers and written notices informing them of their right to receive language assistance services. | |
| Quality of interpreter services | 6. HCOs must assure the competence of language assistance provided to limited English proficient patients or consumers by interpreters and bilingual staff. Family and friends should not be used to provide interpretation services (except on request by the patient or consumer). | |
| Translation of written materials | 7. HCOs must make available easily understood patient-related materials and post signage in the languages of the commonly encountered groups and/or groups represented in the service area. | |
| Care delivery and supporting mechanisms | Clinical cultural competency practices | 1. HCOs should ensure that patients or consumers receive from all staff members effective, understandable, and respectful care that is provided in a manner compatible with their cultural health beliefs and practices and preferred language. |
Leadership
The leadership domain recognizes that organizational leaders, including clinical leaders, administrative leaders, and the board of trustees, play an essential role in developing and implementing cultural competency activities, setting organizational policy and strategy, and monitoring organizational performance (Brach, Paez, & Fraser, 2006; Dansky, Weech-Maldonado, De Souza, & Dreachslin, 2003; Weech-Maldonado et al., 2011). The CLAS standards address two aspects of leadership: strategic planning and public relations. The strategic planning process includes environmental scanning, needs assessment of the communities served, and formulation of goals related to cultural competency (CLAS Standard 8). Strategic goals reflect the organizational priorities for resource use and deployment.
Related to strategic planning is having dedicated staff and resources to achieve cultural competency goals. Dedicated resources can be shown by budgeting resources for cultural competency activities (The Lewin Group, 2002; Wilson-Stronks & Galvez, 2007). Dedicated staff can include an executive level staff member, department, or office that focuses on multicultural and/or linguistic issues. This can be instrumental in coordinating organization-wide initiatives and monitoring progress toward cultural competency goals (Brach et al., 2006; Wilson-Stronks & Galvez, 2007).
Proactive leadership raises public awareness of the cultural competency activities and progress in meeting goals (CLAS Standard 14). This can include a statistical annual report on patient demographics, interpreter use and availability, translated materials, staff training in cultural competency, and survey results of patient experiences with care (Weech-Maldonado et al., 2011).
Integration Into Management Systems and Operations
The integration into management systems and operations domain focuses on whether cultural competency is integrated throughout all management practices of the organization. The CLAS standards address three aspects of integration into management systems and operations: data collection on inpatient population, data collection on service area, and use of cultural competence-related measures in performance management systems and quality improvement (QI). Data collection on inpatient population include mechanisms for collecting data on cultural subgroups, such as race or ethnicity, language preferences, education, and income of patients; and integrating these data into the information systems (CLAS Standard 10). These data are important for strategic and service planning and can be used to monitor health care disparities as well as for QI (Betancourt et al., 2002). The Joint Commission now requires collection of patients’ language and communication needs in the patient record (Wilson-Stronks & Galvez, 2007). Data collection on service area includes maintaining a current demographic, cultural, socioeconomic, and epidemiological profile and needs assessment of the communities served and using the data for strategic planning purposes, QI, and public reporting initiatives (CLAS Standard 11).
CLAS Standard 9 recommends the inclusion of cultural competence-related measures in the organizational performance management systems, such as balanced score cards, organizational climate surveys, adverse events reports, and outcome-based evaluations. Examples of metrics that can be incorporated are patient and human resource outcomes for different cultural groups. Including these measures in performance management systems elevates their importance for the institution. Furthermore, this facilitates QI activities as organizations strive to reduce patient and workforce disparities (Weech-Maldonado et al., 2011).
Workforce Diversity and Training
The workforce diversity and training domain pertains to providing more effective services for culturally diverse populations via proactive human resource practices and state-of-the-art cultural competency training. Human resources practices include proactive recruitment and retention strategies to ensure diversity at all levels of the organization (Weech-Maldonado et al., 2011). Organizational efforts should go beyond recruitment strategies and include retention strategies. Otherwise, organizations can become a “revolving door” for diverse employees, as they leave the organization in pursuit of better opportunities or a more welcoming environment. Retention strategies include efforts to create a welcoming climate for diverse populations, identifying barriers that prevent employees from achieving their full potential and providing equitable promotional opportunities (CLAS Standard 2). Formal mentoring programs, professional development and training, work–life balance and flexible benefits, and affinity groups are among the human resource retention strategies that can be used (Dreachslin & Hobby, 2008).
Organizations also ensure that managers and staff at all levels of the organization receive appropriate and ongoing training in cultural competency (CLAS Standard 3). Whereas staff training curriculum can emphasize the knowledge and skills for culturally competent clinical care, leadership training should include content on management practices and policies that foster organizational cultural competency (Weech-Maldonado et al., 2011). Cultural competency training can be delivered as a stand-alone program, or it can be integrated into other training programs. These trainings should be conducted by qualified staff that are trained in cultural competency and should be periodically updated and repeated. The trainings should be assessed for effectiveness and relevance in meeting the cultural needs of patients.
Training should pay particular attention to addressing and resolving cross-cultural conflicts or complaints by patients (CLAS Standard 13). Individuals from diverse backgrounds are more vulnerable to face experiences where their cultural differences are not accommodated or respected by the HCO. Some of the mechanisms that HCOs can adopt to identify and resolve cross-cultural conflicts are “providing cultural competence training to staff who handle complaints and grievances or other legal or ethical conflict issues; providing notice in other languages about the right of each patient/consumer to file a complaint or grievance; providing the contact name and number of the individual responsible for the disposition of a grievance; and offering ombudsperson services” (OMH, 2001, p. 19).
Community Engagement
The community engagement domain refers to active outreach as well as community inclusion and partnership in organizational decision-making. Organizations can use both formal and informal mechanisms for community involvement, such as community advisory groups or committees in service planning and implementation (CLAS Standard 12).
Patient–Provider Communication
The patient–provider communication domain includes all communication between the patient and clinicians, as well as support staff. The CLAS standards mandate the provision of both interpreter services and translated materials for limited English proficiency (LEP) patients. High-quality interpreter services are needed at all points of patient contact to improve provider and staff communication with LEP patients (CLAS Standards 4, 5, and 6). Accurate communication increases the likelihood of receiving appropriate care (Anderson et al., 2003; OMH, 2001; Wilson-Stronks & Galvez, 2007). When evaluating the quality of interpreter services, it is important to distinguish between professional and ad hoc interpreters (Ngo-Metzger et al., 2006). Ad hoc interpreters are “individuals whose primary job function in the health care setting is something other than interpretation and includes the patient’s family members, friends, clinic staff, or even fellow patients” (Grant Makers in Health, 2003, p. 20). On the other hand, professional interpreters are “those individuals whose sole function in the health care setting is to interpret” (Grant Makers in Health, 2003, p. 22). Prior research has shown the effectiveness of professional interpreters compared with ad hoc interpreters (Enguidanos & Rosen, 1997; Jacobs et al., 2001). Professional interpreter services may be in person or remote. Remote interpreter services include telephone language lines, video links, and other remote systems.
Patient-related written materials must be translated into the most common languages of the patient population (CLAS Standard 7). Examples of relevant patient-related materials include applications, consent forms, preventive and treatment instructions, and patient education materials (Weech-Maldonado et al., 2011). Translated materials should be evaluated for linguistic and cultural appropriateness with respect to both content and context (Weech-Maldonado, Weidmer, Morales, & Hays, 2001). Qualitative methods, such as focus groups and cognitive interviews, are particularly useful in assessing the cultural appropriateness of translated materials.
Care Delivery and Supporting Mechanisms
The care delivery and supporting mechanisms domain encompasses the delivery of care, the physical environment of where the care is delivered, and links to supportive services and providers (CLAS Standard 1). It includes the use of tools to elicit culturally relevant information on health beliefs, behaviors, and practices (The Lewin Group, 2002). These data can be used to assist with establishing a physical environment and care delivery that are culturally appropriate for the community served.
Methods
CCATH Development
The development of the CCATH included the following steps: (a) draft of the CCATH, (b) pilot testing, (c) focus groups, and (d) cognitive interviews (Hays et al., 2006).
Draft of the CCATH
The CCATH measures were developed to reflect the 6 NQF domains and 14 CLAS standards as shown on Table 1. A committee of project staff members was involved in the development and review of the CCATH items. Project staff were guided by a comprehensive literature review on organizational, leadership, and clinical best practices associated with the delivery of CLAS (Dreachslin & Curtis, 2004; Dreachslin, Weech-Maldonado, & Dansky, 2004; OMH, 2001). Additional feedback was provided by the project advisory committee, which was constituted by cultural competency and diversity management experts from the hospital industry and government.
Pilot testing of the CCATH
The pilot testing had two major goals: (a) ensure ease of administration, understandability, and clarity and (b) minimize response burden. A convenience sample of five hospitals that completed the CCATH surveys represented a diverse group in terms of size, specialization, population served, and experience in implementing the CLAS standards. Of the five hospital pilot sites, three were located in California and two were in Pennsylvania. To facilitate survey administration, the CCATH was divided into four major sections: culturally competent care (30 items); human resource management (30 items); translation and interpreters (35 items); and leadership, climate, and strategies (33 items). Administrators of the participating hospitals were debriefed by phone after completion of the survey. On the basis of the pilot test results, we redesigned and significantly shortened the CCATH to one survey of 28 items.
Focus groups
Focus groups are a research tool that relies on group discussions to collect data on a given topic (Morgan, 1996). The revised version of the CCATH was presented to a focus group of potential survey respondents at a National Research Corporation/Picker annual meeting in 2005. Individuals were recruited from the meeting’s participant list of individuals that held a hospital management position (i.e., title of CEO, VP, CFO, director, or manager). The purpose of this focus group was to discuss the survey content, administration, and application of the CCATH instrument. A protocol was developed to guide the discussion of the focus group. The focus group had nine participants from hospital systems in seven states (Illinois, Idaho, California, Florida, Illinois, Nebraska, and Texas), and it lasted approximately 2 hours. A transcript of the focus group study was obtained, and two project staff members analyzed the statements of the participants to identify major themes.
Overall, participants thought the CCATH was covering the right issues, and some of them were able to relate the survey content to their own institutional experiences with cultural and linguistic diversity. Participants noted that completing the survey would most likely be a group effort because no single individual or department would have all the required information. Therefore, they felt that the survey should be directed to the CEO to ensure distribution to the appropriate individuals. The CCATH was revised based on feedback from the focus group study.
Cognitive interviews
Cognitive interviews were conducted with hospital administrators to assess the ease of administration, understandability, and clarity of the survey instrument. Cognitive interviewing in survey development has been described as “the administration of draft survey questions while collecting additional verbal information about the survey responses, which is used to evaluate the quality of the response or to help determine whether the question is generating the information that its author intends” (Beatty & Willis, 2007, p. 287). Cognitive interviews can be used to detect and minimize some sources of measurement error by identifying question items or terms that are difficult to comprehend, questions that are misinterpreted by the respondents, and response options that are inappropriate for the question or that fail to capture a respondent’s experience (Jared & David, 1991).
The hospitals participating in the cognitive interviews were recruited through the Institute for Diversity in Health Management and the Diversity Rx’s CLAS listserve. Participants represented both hospitals and health systems’ central administration. There were three in-person and six phone cognitive interviews that were conducted during 2006. Cognitive interview participants estimated that the time required to complete the survey ranged from 1 to 3 hours and agreed that it was not difficult to locate the correct department to access information needed to complete the survey. Respondents did indicate that the wording of some items and definitions of some terms produced confusion over the appropriate response. Final revisions were done to the CCATH on the basis of feedback from cognitive interviews.
Sample
The sampling frame for the CCATH mail survey consisted of all general and children hospitals listed in the California Hospital Association Directory (344 hospitals) in 2006. To ensure a higher response rate, we followed a modified approach to the Total Design Method suggested by Dillman (1978). A cover letter explaining the purpose of the survey along with the actual survey was mailed to the CEO. In addition, an incentive payment was included for the survey coordinator. A reminder was mailed to those who had not returned the survey within 2 weeks. A second mailing targeted participants not responding within 1 month, and a new survey was included with the mailing. If the survey has not been returned within 7 weeks, phone calls were made to request respondents to complete the survey. This was followed by E-mail reminders for those who had not returned the survey within 10 weeks. Finally, an E-mail with an electronic version of the survey was sent to those who had not responded within 14 weeks. We obtained a 36% response rate (125 hospitals) with this multistage approach. We assessed potential nonresponse bias by comparing respondent hospitals with nonrespondent hospitals on several organizational and market level variables. Respondent hospitals were less likely to be part of a system (59% vs. 70%). However, respondent hospitals were not significantly different (p < .05) from nonrespondent hospitals in terms of teaching status, ownership (government, for-profit, and not-for-profit), size, percentage of non-White inpatients, percentage of Medicaid patient days, percentage of managed care patient days, total profit margin, market competition (Herfindahl index), percentage of non-White population in the county, percentage of non-English speakers in the county, being in a metropolitan area, and per capita income.
Analysis
CCATH survey items were factor analyzed in Statistical Analysis Software (SAS) using principal components analysis with Varimax and oblique rotations. The number of factors retained was determined by (a) Guttman’s weakest lower bound (principal components eigenvalues greater than 1), (b) the scree plot to examine the point at which the plot of eigenvalues begins to level off, and (c) the interpretability of factors. Items with factor loadings equal or greater than 0.4 were retained. The fit of the model identified using exploratory factor analysis was evaluated using fit indices from a confirmatory factor analysis estimated using Mplus (Muthén & Muthén, 2010). Mplus allows for the modeling of categorical as well as continuous variables.
Internal consistency reliability of the CCATH composites was assessed using Cronbach’s alphas. Construct validity of the CCATH scales was evaluated by examining sensitivity to hospital ownership type. Not-for-profit hospitals and government hospitals are expected to have greater adherence to the CLAS standards compared with for-profit hospitals. Not-for-profit and government hospitals hold their assets in trust for their local communities and are expected to manage their assets for their welfare rather than advance private profit (Chait, Ryan, & Taylor, 1995). Therefore, these hospitals are more likely to abide by community expectations than for-profit hospitals. The dependent variables were the CCATH multi-item composite mean scores, which were obtained by (a) linear transformation of each item to a 0–100 possible range (e.g., for a dichotomous item: yes = 100, no = 0) and (b) calculating the average of the items within each composite. The independent variable was hospital ownership type, which consisted of a categorical variable with three levels: government, not-for-profit, for-profit hospitals. Analysis of variance was used to examine the relationship between CCATH scores and hospital ownership type. Post hoc analysis using Tukey’s analysis was conducted to test for differences in CCATH scores by ownership type.
Findings
The exploratory and confirmatory factor analysis supported 12 CCATH composite scales (subdomains): leadership and strategic planning, data collection on inpatient population, data collection on service area, performance management systems and QI, human resources practices, diversity training, community representation, availability of interpreter services, interpreter services policies, quality of interpreter services, translation of written materials, and clinical cultural competency practices (OMH, 2011). The 12-factor model provided good fit to the data: Chi-square = 90.8 (p = .17), comparative fit index = 0.96, Tucker–Lewis index = 0.97, and root mean square error of approximation = 0.035.
Table 1 shows the relationship between the NQF domains, the CCATH scales, and the CLAS standards. Table 2 provides coefficient alpha and mean score for each CCATH scale. Nine of the twelve CCATH scales had alphas greater than .70, and the reliability was .65 or above for all scales. Ware et al. (1980) have suggested that alpha coefficients that are ≥.60 are considered acceptable when developing new scales. Results indicate that California hospitals achieved the highest CCATH scores (representing greater implementation) for the scales of data collection on inpatients (x̄ = 87), cultural competency practices (x̄ = 81), and availability of interpreter services (x̄ = 70). On the other hand, they had the lowest scores for the scales of performance management systems and QI (x̄ = 33), leadership and strategic planning (x̄ = 36), and community representation (x̄ = 40).
Table 2.
Cultural Competency Assessment Tool for Hospitals (CCATH) scales, number of hospitals, number of items, internal consistency reliabilities (alphas), means, and standard deviations
| CCATH scale | n | Number of items | Alpha | Meana | SD |
|---|---|---|---|---|---|
| Leadership and strategic planning | 123 | 6 | 0.79 | 35.8 | 33.6 |
| Data collection on inpatient population | 125 | 2 | 0.70 | 87.1 | 29.8 |
| Data collection on service area | 125 | 7 | 0.84 | 60.5 | 31.3 |
| Performance management systems and QI | 112 | 3 | 0.78 | 33.3 | 35.0 |
| Human resources practices | 125 | 8 | 0.66 | 62.2 | 21.4 |
| Diversity training | 125 | 3 | 0.68 | 53.7 | 35.5 |
| Community representation | 123 | 2 | 0.84 | 40.2 | 45.6 |
| Availability of interpreter services | 124 | 4 | 0.87 | 70.2 | 25.7 |
| Interpreter services policies | 122 | 4 | 0.65 | 61.1 | 32.5 |
| Quality of interpreter services | 124 | 3 | 0.75 | 58.1 | 40.7 |
| Translation of written materials | 124 | 6 | 0.81 | 52.3 | 22.8 |
| Clinical cultural competency practices | 123 | 4 | 0.76 | 81.4 | 23.3 |
Range is from 0 to 100, with a score of 100 indicating full adherence to each respective CCATH scale.
Analysis of variance results show that not-for-profit hospitals had significantly higher scores than for-profit hospitals on five CCATH scales: leadership and strategic planning, data collection on inpatient population, human resources practices, interpreter services policies, and quality of interpreter services (Table 3). In addition, not-for-profit hospitals had higher CCATH scores than government hospitals for two CCATH scales: human resources practices and diversity training.
Table 3.
Analysis of variance of Cultural Competency Assessment Tool for Hospitals (CCATH) composite scores by ownership type
| Composite | Government hospitals (n = 32) | Not-for-profit hospitals (n = 65) | For-profit hospitals (n = 26) | F test |
|---|---|---|---|---|
| Leadership and strategic planning | 29.2 | 44.3 | 24.5 | 4.25* |
| Data collection on inpatient population | 88.9 | 92.2 | 72.0 | 4.29* |
| Data collection on service area | 56.5 | 65.3 | 51.4 | 2.15 |
| Performance management systems and QI | 24.0 | 39.3 | 28.2 | 2.45 |
| Human resources practices | 56.6 | 67.5 | 55.3 | 4.66* |
| Diversity training | 42.7 | 61.5 | 47.4 | 3.69* |
| Community representation | 40.3 | 45.3 | 28.9 | 1.20 |
| Availability of interpreter services | 71.9 | 70.9 | 66.9 | 0.30 |
| Interpreter services policies | 61.7 | 68.3 | 45.0 | 4.97** |
| Quality of interpreter services | 53.1 | 68.2 | 37.2 | 6.06** |
| Translation of written materials | 52.7 | 55.0 | 45.5 | 1.60 |
| Clinical cultural competency practices | 83.1 | 82.8 | 75.0 | 1.16 |
Data in bold italics represent statistically significant (p < 0.05) pairwise differences based on Tukey’s post hoc analysis.
p < .05.
p < .01.
Discussion
The national CLAS standards in health care were aimed at providing guidelines on policies and practices for culturally competent systems of care (OMH, 2001). Through a comprehensive and multistage evaluation process, we developed the CCATH, a survey directly targeted at assessing adherence to the CLAS standards for hospital in-patient services. The field test provided support for the reliability and validity of the CCATH.
Several important policy, managerial, and research implications were found in this study. First, results from this study showed that California hospitals have better performance in patient-related cultural competency scales, such as data collection on inpatient populations, interpreter services, and clinical cultural competency practices. However, they tend to lag in integrating cultural competency into management practices, as suggested by their underperformance in the subdomains of leadership and strategic planning, QI, and community representation. These results are similar to those in prior studies examining cultural competency activities of hospitals in Pennsylvania (Weech-Maldonado, Dreachslin, Dansky, De Souza, & Gatto, 2002) and Alabama (Whitman & Davis, 2008). Organizations need a systems approach to cultural competency with strong leadership commitment and integration of cultural competency into management systems, such as human resources, information systems, and QI (NQF, 2008).
Second, this study shows that not-for-profit hospitals outperform for-profit hospitals in California with respect to cultural competency practices. This is not surprising given the different missions of for-profit and not-for-profit hospitals. This suggests the need for further research on the business case for cultural competency, showing how organizational cultural competency activities may relate to patient satisfaction, revenues, and ultimately financial performance. To the extent that cultural competency provides competitive advantage, there is greater likelihood that for-profit hospitals will adopt these practices. Differences between for-profit and not-for-profit hospitals may also be a result of contextual differences, such as differences in competitive pressures and diversity of markets served. Further research is needed on the contextual factors that may explain the differences between for-profit and not-for-profit hospitals in cultural competency.
Finally, organizational assessments such as the CCATH need to be systematically implemented by hospitals so that appropriate benchmark data can be collected. This benchmarking data can provide national and regional norms that can be used as comparative data for QI efforts. On the basis of the focus group feedback, we suggest development of an online version of the CCATH, which would likely contribute to ease of administration and, consequently, encourage more widespread use of the CCATH. An online version of the CCATH could reside on the Web site of a hospital association group and provide feedback in terms of individual hospital scores and include a link to other resources to improve performance. Ideally, the Web site would also provide benchmarking data so that hospitals can compare their results with national and regional averages.
Practice Implications
As the population’s racial and ethnic diversity continues to increase, tools such as the CCATH will be increasingly important to hospital administrators, regulators, and researchers. The CCATH can have multiple field applications. First, managers and policy makers can use the CCATH as a tool to evaluate hospital performance in cultural competency and identify and target improvements in hospital policies and practices that undergird the provision of CLAS. Second, it can be used for research. For example, hospital CCATH scores can be used to examine the relationship between adherence to the CLAS standards and key outcomes hypothesized to be related to effective diversity management or cultural competency. These outcomes can include both human resources, such as employee turnover and absenteeism, and patient outcomes, such as patient assessments of care and clinical outcomes.
To aid hospital administrators, we provide an example of how the CCATH can be used as a benchmarking tool to assess cultural competency practices (Table 4). We divided hospitals in our sample into three performance tiers based on their mean score on the 12 CCATH scales: high (top 25%), medium (middle 50%), and low (bottom 25%). High-performing hospitals had overall scores of greater or equal than 72, whereas low-performing hospitals had scores lower than or equal to 45. Medium-performing hospitals had scores in between the high- and low-performing hospitals. Hospitals can use similar benchmarking data to compare themselves with the industry. For example, a hospital with scores of 20 on leadership and strategic planning, 40 on human resource practices, and 90 on availability of interpreter services would show that it performs relatively well in terms of providing interpreter services but could improve its management practices as it pertains to strategic planning and human resource practices. Using a tool like the CCATH, hospital administrators would be better positioned to assess their cultural competency and identify particular areas that may require particular improvement. This, in turn, facilitates proactive steps to ensure hospital’s cultural competence.
Table 4.
Analysis of variance of CCATH composite scores by performance tiers
| Composite | High (n = 30) | Medium (n = 65) | Low (n = 30) | F test |
|---|---|---|---|---|
| Leadership and strategic planning | 75.7 | 29.5 | 8.6 | 61.0** |
| Data collection on inpatient population | 100.0 | 92.4 | 69.2 | 10.7** |
| Data collection on service area | 88.9 | 61.5 | 35.8 | 26.2** |
| Performance management systems and QI | 61.1 | 29.7 | 8.9 | 30.1** |
| Human resources practices | 85.7 | 64.9 | 49.0 | 34.8** |
| Diversity training | 87.8 | 50.5 | 26.2 | 36.2** |
| Community representation | 69.6 | 43.4 | 8.9 | 15.7** |
| Availability of interpreter services | 84.5 | 71.2 | 51.4 | 15.3** |
| Interpreter services policies | 88.8 | 60.7 | 38.5 | 24.8** |
| Quality of interpreter services | 87.4 | 67.2 | 19.0 | 36.2** |
| Translation of written materials | 67.9 | 51.4 | 37.4 | 17.0** |
| Clinical cultural competency practices | 93.1 | 82.6 | 65.7 | 11.9** |
All pairwise comparisons were statistically different (p < .05) based on Tukey’s post hoc analysis.
p < 0.05.
p < 0.01.
Although tools like the CCATH can be an important aid in identifying the organization’s status with respect to cultural competency, it is important to understand that becoming culturally competent organizations is a process. Organizations striving to become more culturally competent will need to engage in a change process of organizational transformation. This entails an organizational culture change from a monoculture (or a culture that “accepts only one way of doing things and one set of values and beliefs” to a pluralistic environment) or an environment that accepts and integrates people from diverse cultural backgrounds (Daft & Marcic, 2005). This change process has been described as a continuum from early to later stages of development. For example, Dreachslin (1996) proposes a five-stage change model from affirmative action to valuing diversity: discovery, assessment, exploration, transformation, and revitalization.
Furthermore, becoming culturally competent should be viewed as an ongoing process whereby organizations (a) determine cultural competency goals in the context of its strategic plan; (b) assess individual, group, and organizational baseline performance to determine gaps in performance; (c) develop interventions to close the gaps in performance; and (d) reassess performance to determine the effectiveness of the interventions. For example, in designing cultural competency training, the organization should determine goals for its training in the context of its strategic plan, measure current performance against needs, design training to address the gap, implement the training, assess training effectiveness, and strive for continuous improvement (Curtis et al., 2007).
Finally, we should note that there is a potential business case for cultural competency. Patients of culturally competent HCOs may exhibit higher satisfaction with their care and greater customer loyalty, as these organizations would be better placed to serve their varied needs. Literature suggests that higher customer satisfaction leads to superior economic returns for the organization (McKinney & Yoon, 2002) and is key to long-term organizational survival (Aaker & Jacobson, 1994). As such, cultural competency has the potential to improve an organization’s reputation, connections to the local community, and economic profits. Recent public reporting efforts by the Centers for Medicare and Medicaid Services of the Consumer Assessments of Health Care Providers and Systems hospital survey are expected to result in QI initiatives aimed at improving patient experiences with care (Giordano, Elliott, Goldstein, Lehrman, & Spencer, 2010). To the extent that cultural competency practices are associated with better patient experiences, there will be a market incentive for the implementation of such practices.
There are several limitations to the study. First, the study was limited to hospitals in California, which limits generalizability of the findings to other states. However, given the diversity of the State of California, it presents an important barometer of what is happening in other states. Second, the survey had a relatively low response rate. However, we found that respondent hospitals did not differ from nonrespondent hospitals in terms of a large number of organizational and market variables. Respondent hospitals were less likely to be part of a system. Some system hospitals may have not participated, thinking that a system or a coordinated response was necessary. Third, the CCATH was aimed at respondents from top management. Responses may have varied if the survey would have been administered among middle managers and staff. Despite these limitations, we believe this study represents an important contribution to the literature on organizational assessments of cultural competency.
Acknowledgments
The authors acknowledge the assistance of the CCATH Project Advisory Committee (Shelby Dunster, Rupert Evans, Iris A. Garcia, James Plumb, Robert Riney, and Miguel Tirado). This project was supported in part by the Commonwealth Fund Project 20060407 (Project Officer, Anne Beal) and the DHHS OMH Task Order 7 (Contract 282-00-0005; Project Officer, Guadalupe Pacheco). Dr. Weech-Maldonado was supported in part by the UAB Center of Excellence in Comparative Effectiveness for Eliminating Disparities (NIH/NCMHD grant 3P60MD000502-08S1). Dr. Hays was supported in part by the UCLA Older Americans Independence Center (NIH/NIA grant P30-AG028748), the UCLA Resource Center for Minority Aging Research/Center for Health Improvement in Minority Elderly (NIH/NIA grant award P30AG021684), and the UCLA/Drew Project EXPORT (NCMHD 2P20MD000182).
Footnotes
The authors have disclosed that they have no significant relationships with, or financial interest in, any commercial companies pertaining to this article.
Contributor Information
Robert Weech-Maldonado, Email: rweech@uab.edu, Professor and L.R. Jordan Endowed Chair, Department of Health Services Administration, University of Alabama, Birmingham.
Janice L. Dreachslin, Email: jld13@psu.edu, Professor of Health Policy and Administration, Penn State Great Valley School of Graduate Professional Studies, Malvern, Pennsylvania.
Julie Brown, Email: Julie_Brown@rand.org, Director, Survey Research Group, RAND, Santa Monica, California.
Rohit Pradhan, Email: rpradhan@uab.edu, Postdoctoral Fellow, Department of Health Services Administration, University of Alabama, Birmingham.
Kelly L. Rubin, Email: rubink@gao.gov, Senior Social Science Analyst, Center for Design, Methods, and Analysis, U.S. Government Accountability Office, Washington, District of Columbia.
Cameron Schiller, Email: k.cameron.schiller@gmail.com, Health Care Consultant, Gainesville, Florida.
Ron D. Hays, Email: drhays@ucla.edu, Professor of Medicine, Division of General Internal Medicine and Health Services Research, Department of Medicine, University of California-Los Angeles, Los Angeles, California.
References
- Aaker D, Jacobson R. The financial information content of perceived quality. Journal of Marketing Research. 1994;31(2):191–201. [Google Scholar]
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent health care systems. A systematic review. American Journal of Preventive Medicine. 2003;24(Suppl 3):68–79. doi: 10.1016/s0749-3797(02)00657-8. [DOI] [PubMed] [Google Scholar]
- Beatty PC, Willis GB. Research synthesis: The practice of cognitive interviewing. Public Opinion Quarterly. 2007;71(2):287. [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE. Cultural competence in health care: Emerging frameworks and practical approaches. New York, NY: The Commonwealth Fund; 2002. [Google Scholar]
- Brach C, Paez K, Fraser I. Cultural competence california style. Rockville, MD: Agency for Health Care Research and Quality; 2006. (working paper) [Google Scholar]
- Chait R, Ryan WP, Taylor BE. Governance as Leadership: Reframing the Work of Nonprofit Boards. Hoboken, NJ: Wiley; 1995. [Google Scholar]
- Cooper LA, Roter DL. Institute of Medicine, editor. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: The National Academic Press; 2003. Patient–provider communication: The effect of race and ethnicity on process and outcomes of health care. [Google Scholar]
- Curtis EF, Dreachslin JL, Sinioris M. Diversity and cultural competency training in health care organizations: Hallmarks of success. The Health Care Manager. 2007;26(3):255–262. doi: 10.1097/01.HCM.0000285018.18773.ed. [DOI] [PubMed] [Google Scholar]
- Daft LR, Marcic D. Understanding management. Chula Vista, CA: South-Western College Publication; 2005. [Google Scholar]
- Dansky KH, Weech-Maldonado R, De Souza G, Dreachslin JL. Organizational strategy and diversity management: Diversity sensitive orientations as a moderating influence. Health Care Management Review. 2003;28(3):243–253. doi: 10.1097/00004010-200307000-00005. [DOI] [PubMed] [Google Scholar]
- Dillman DA. Mail and telephone surveys: The total design method. New York, NY: Wiley; 1978. [Google Scholar]
- Dreachslin JL. Diversity leadership. Chicago, IL: Health Administration Press; 1996. [Google Scholar]
- Dreachslin JL, Curtis EF. Study of factors affecting the career advancement of women and racially/ethnically diverse individuals in health care management. The Journal of Health Administration Education. 2004;21(4):441. [PubMed] [Google Scholar]
- Dreachslin JL, Hobby F. Racial and ethnic disparities: Why diversity leadership matters. Journal of Health Care Management. 2008;53(1):8–13. [PubMed] [Google Scholar]
- Dreachslin JL, Weech-Maldonado R, Dansky KH. Racial and ethnic diversity and organizational behavior: A focused research agenda for health services management. Social Science & Medicine. 2004;59(5):961–971. doi: 10.1016/j.socscimed.2003.12.007. [DOI] [PubMed] [Google Scholar]
- Enguidanos ER, Rosen P. Language as a factor affecting follow-up compliance from the emergency department. Journal of Emergency Medicine. 1997;15(1):9–12. doi: 10.1016/s0736-4679(96)00260-0. [DOI] [PubMed] [Google Scholar]
- Giordano LA, Elliott MN, Goldstein E, Lehrman WG, Spencer PA. Development, implementation, and public reporting of the HCAHPS survey. Medical Care Research and Review. 2010;67(1):27–37. doi: 10.1177/1077558709341065. [DOI] [PubMed] [Google Scholar]
- Grant Makers in Health. In the right words: Addressing language and culture in providing health care. San Francisco, CA: Grant Makers in Health; 2003. [PubMed] [Google Scholar]
- Harris DR, Andrews R, Elixhauser A. Racial and gender differences in use of procedures for Black and White hospitalized adults. Ethnicity & Disease. 1997;7(2):91–105. [PubMed] [Google Scholar]
- Hays R, Weech-Maldonado R, Brown J, Sand K, Dreachslin J, Dansky K. Cultural Competency Assessment Tool for Hospitals (CCATH). Final Report for Contract Number 282-00-0005, Task Order # 7. Washington, DC: Office of Minority Health, Department of Health and Human Services; 2006. [Google Scholar]
- Hicks LS, Ayanian JZ, Orav EJ, Soukup J, McWilliams JM, Choi SS, Johnson PA. Is hospital service associated with racial and ethnic disparities in experiences with hospital care? American Journal of Medicine. 2005;118(5):529–535. doi: 10.1016/j.amjmed.2005.02.012. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Lauderdale DS, Meltzer D, Shorey JM, Levinson W, Thisted RA. Impact of interpreter services on delivery of health care to limited English-proficient patients. Journal of General Internal Medicine. 2001;16(7):468–474. doi: 10.1046/j.1525-1497.2001.016007468.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jared BJ, David JM. Cognition and survey measurement: History and overview. Applied Cognitive Psychology. 1991;5(3):175–192. [Google Scholar]
- LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Medical Care Research and Review. 2000;57(Suppl 1):146–161. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- Longest BB, Rakich SJ, Darr K. Managing health services organizations and systems. Baltimore, MD: Health Professions Press; 2000. [Google Scholar]
- McKinney V, Yoon K. The measurement of Web-customer satisfaction: An expectation and disconfirmation approach. Information Systems Research. 2002;13(3):296–315. [Google Scholar]
- Morgan DL. Focus groups. Annual Review of Sociology. 1996;22:129–152. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 2010. [Google Scholar]
- National Quality Forum. A comprehensive framework and preferred practices for measuring and reporting cultural competency. Washington, DC: National Quality Forum; 2008. [Google Scholar]
- Ngo-Metzger Q, Telfair J, Sorkin DL, Weidmer B, Weech Maldonado R, Hurtado M, Hays RD. Cultural competency and quality of care: Obtaining the patient’s perspective. New York: The Commonwealth Fund; 2006. [Google Scholar]
- Office of Minority Health. National standards for culturally and linguistically appropriate services in health care: Final report. Washington, DC: U.S. Department of Health and Human Services Office of Minority Health; 2001. [Google Scholar]
- Office of Minority Health. Cultural Competency Assessment Tool for Hospitals (CCATH) Washington, DC: U.S. Department of Health and Human Services Office of Minority Health; 2011. Retrieved from http://www.minorityhealth.hhs.gov/ [Google Scholar]
- Petersen LA, Wright SM, Peterson ED, Daley J. Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Medical Care. 2002;40(1):I86–I96. doi: 10.1097/00005650-200201001-00010. [DOI] [PubMed] [Google Scholar]
- Scott WR, Davis GF. Organizations and organizing: Rational, natural, and open systems perspectives. Upper Saddle River, NJ: Pearson College Div; 2007. [Google Scholar]
- The Lewin Group. Indicators of cultural competence in health care delivery organizations: An organizational cultural competence: Assessment profile. Falls Church, VA: The Lewin Group; 2002. [Google Scholar]
- Ware JE, Allyson RD, Robert HB. Conceptualization and measurement of health for adults in the health insurance study: Vol. 1. Model of health and methodology. Santa Monica, CA: Rand Corporation; 1980. [Google Scholar]
- Weech-Maldonado R, Al-Amin M, Nishimi RY, Salam F. Enhancing the cultural competency of health care organizations. In: Wolf AJ, Hanson H, Moir JM, Friedman L, Savage GT, editors. Organization development in health care: Conversations on research and strategies (advances in health care management) Vol. 10. Bingley, UK: Emerald Publishing Group Limited; 2011. [DOI] [PubMed] [Google Scholar]
- Weech-Maldonado R, Dreachslin JL, Dansky KH, De Souza G, Gatto M. Racial/ethnic diversity management and cultural competency: The case of Pennsylvania hospitals. Journal of Health Care Management. 2002;47(2):111–124. discussion 124–116. [PubMed] [Google Scholar]
- Weech-Maldonado R, Weidmer BO, Morales LS, Hays RD. Cross-cultural adaptation of survey instruments: The CAHPS experience. In: Cynamon M, Kulka R, editors. Seventh Conference on Health Survey Research Methods. Hyattsville, MD: Department of Health and Human Services; 2001. Retrieved May 31, 2011, from http://www.cdc.gov/nchs/data/conf/conf07.pdf. [Google Scholar]
- Whitman M, Davis J. Cultural and linguistic competence in health care: The case of Alabama general hospitals. Journal of Health Care Management. 2008;53(1):26–39. [PubMed] [Google Scholar]
- Wilson-Stronks A, Galvez E. Hospitals, language and culture: A snapshot of the nation. Exploring cultural and linguistic services in the nation’s hospitals. Washington, DC: Joint Commission on Accreditation of Health Care Organizations; 2007. [Google Scholar]