Abstract
Background and aims
Research has not studied unique impulsivity dimensions as prospective links between childhood attention deficit hyperactivity disorder (ADHD) and alcohol problems. We examined the association between childhood ADHD, 5 facets of impulsivity and alcohol problems in adulthood, and the indirect effects of childhood ADHD-to-impulsivity-to-alcohol problems.
Design, Setting, and Participants
Participants were from a longitudinal study (N = 289, MAge = 28.67) of individuals with (n = 170) and without (n = 119) childhood ADHD. The ADHD sample, as part of an ADHD summer treatment program, was initially diagnosed in childhood (1987–1996, Pittsburgh, Pennsylvania, USA) via structured parent interview and standardized parent/teacher ratings. The ADHD sample and demographically similar individuals without ADHD (living in the greater Pittsburgh area) were recruited to participate in the Pittsburgh ADHD Longitudinal Study (PALS) between 1999 and 2003.
Measurements
Self-reported impulsivity (UPPS-P) and alcohol-related problems were assessed in adulthood (2011 – 2014).
Findings
Adults with, compared with those without, childhood ADHD had more alcohol problems (β = .34, p < .05) and higher levels of negative urgency, positive urgency, lack of perseverance and lack of planning (β’s = .24–.31, p’s < .001). Impulsivity facets (except sensation seeking) were related to number of alcohol problems (β’s = .34–.61, p’s < .05). Negative (b = .26, p < .01) and positive (b = .27, p < .01) urgency mediated the association between childhood ADHD and number of adult alcohol problems.
Conclusions
Elevated levels of emotional impulsivity (negative/positive urgency) may place children with attention deficit hyperactivity disorder (ADHD) at increased risk for alcohol problems in adulthood.
Keywords: ADHD, alcohol problems, negative urgency, positive urgency
The Indirect Effects of Childhood ADHD on Alcohol Problems in Adulthood through Unique Facets of Impulsivity
A diagnosis of attention deficit hyperactivity disorder (ADHD) in childhood has been shown across studies to increase risk of experiencing an alcohol use disorder by adulthood(e.g.,1,2). Importantly, the association between ADHD and alcohol use (e.g., frequency) has been less consistent(e.g., 1). One reason for these disparate results could be that most studies of the association between ADHD and alcohol use risk have focused on diagnostic comorbidities, such as conduct disorder (CD), rather than dimensional markers of risk. The current study examines the contribution of unique facets of impulsivity to alcohol problems for adults with ADHD histories. Differences in level of impulsivity, across conceptually distinct facets of this construct, may persist for this population into adulthood and may help to explain why those with ADHD experience more problematic alcohol use.
Impulsivity Facets, ADHD, and Alcohol Problems
Impulsivity is a broad personality construct that has been widely studied in relation to alcohol use, alcohol use disorder(e.g., 3,4), and ADHD(5; e.g., see 6 for a review). Despite impulsivity being related to both ADHD and alcohol use, there has been a paucity of research directly testing impulsivity’s contribution to alcohol problems in this population beyond persistence of ADHD diagnostic symptoms(7–9). However, two cross-sectional studies of college students provide tentative support for increased disinhibited personality characteristics (i.e., impulsivity and sensation seeking) being a link to more alcohol problems for individuals with ADHD(10,11).
Increasingly, specific components of impulsivity have been studied in relation to both alcohol use and ADHD. For example, a recent meta-analysis of 96 studies(12) found that multiple facets of impulsivity (UPPS model) were related to alcohol use frequency, but that acting rashly in response to strong negative or positive mood (negative and positive urgency, respectively) was most strongly related to alcohol problems. Similarly, recent cross-sectional findings have shown that disaggregating this construct may be meaningful to understanding ADHD(13,14). Additionally, research has shown that individuals with ADHD may have higher levels of emotion dysregulation and emotional impulsivity(13,15) which underscores the potential importance of emotional impulsivity in this population. Research on the prospective association between childhood ADHD and specific impulsivity facets in adulthood would directly extend this literature and provide critical information about why this population may be at risk for alcohol-related problems.
Current Study
The current study examines associations between childhood ADHD, 5 components of impulsivity (lack of planning, lack of perseverance, negative urgency, positive urgency, and sensation seeking), and alcohol problems in adulthood. The data span an average of 15.25 (SD = 2.5) years from childhood into adulthood. Our first (1) hypothesis, tested with zero-inflated negative binomial regressions, was that individuals with childhood ADHD would have both increased likelihood and number of alcohol problems compared to individuals without childhood ADHD. Secondly (2), based on prior cross-sectional research on children and adults with ADHD(13,14), we hypothesized that childhood ADHD would predict increased impulsivity for four out of five impulsivity facets (all but sensation seeking) in adulthood in structural equation models. Our third (3) hypothesis proposed an indirect effect of childhood ADHD on alcohol problems through the impulsivity facets and was tested with zero-inflated negative binomial models. Given prior findings that emotional impulsivity is strongly related to alcohol use problems and individuals with ADHD may be elevated on this and related constructs (i.e., emotion dysregulation), we hypothesized that the indirect effects would be strongest for positive and negative urgency.
Method
Design
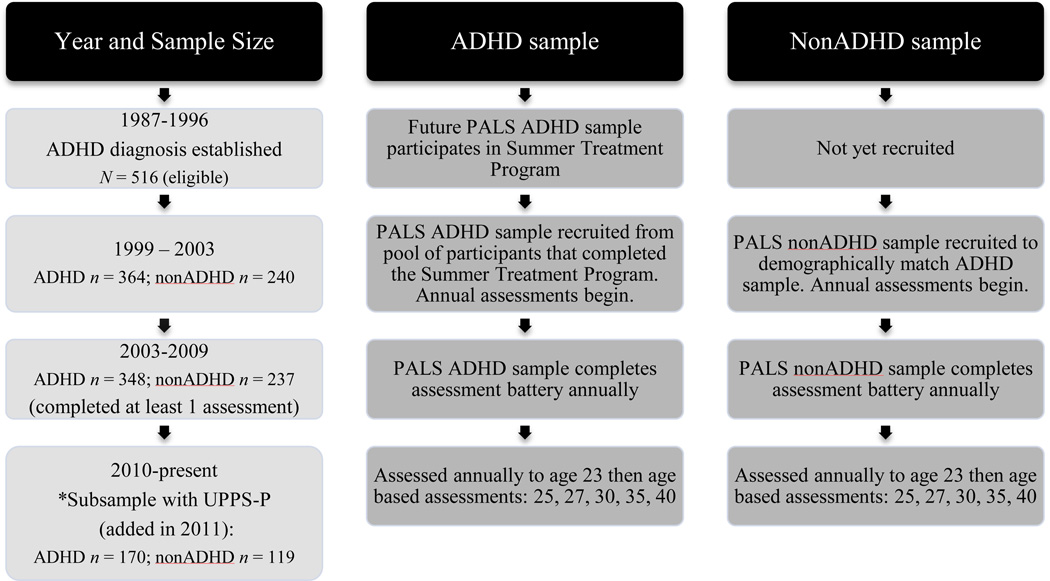
The participants are from a longitudinal study of individuals with and without childhood ADHD (Pittsburgh ADHD Longitudinal Study: PALS). Initial enrollment into this study occurred from 1999–2003; annual interviews occurred through 2009; assessments have since been age-based (annually to 23, and then at ages 25, 27, 30, 35, 40; See Figure 1). Interviews were conducted by post-baccalaureate research staff following informed consent. Participants were assured confidentiality of all disclosed material except in cases of impending danger to self or others (reinforced with a DHHS Certificate of Confidentiality). The UPPS-P was added to the PALS assessment battery in 2011; the current study utilizes the subsample of PALS participants with UPPS-P data. Additional study details may be found in Molina and colleagues(18).
Figure 1.
Flow chart of PALS study over time for ADHD and nonADHD samples
Participants
ADHD sample
Participants were selected for the PALS study due to their diagnosis of ADHD and participation in a summer treatment program (STP) for children with ADHD(16). As part of participating in the STP, childhood ADHD was diagnosed with DSM-III-R or DSM-IV ADHD criteria at the ADD Clinic, Western Psychiatric Institute and Clinic, in Pittsburgh, PA between 1987 and 1996. Participants were initially referred for treatment by schools, physicians, mental health workers or their parents. Average age at this diagnostic evaluation was 9.40 years old (SD = 2.27, range = 5.0–16.92, 90% were ages 5–12).
Diagnostic information for the participants with ADHD was collected using standardized parent and teacher DSM-III-R and DSM-IV symptom rating scales (DBD17) and a standardized semi-structured diagnostic interview administered to parents by a Ph.D. level clinician. It also included queries about other comorbidities (instrument available through co-author W.E.P.). Two Ph.D. level clinicians independently reviewed all ratings and interviews to confirm DSM diagnoses and when disagreement occurred, a third clinician reviewed the file and the majority decision was used. Exclusion criteria for participation in PALS included a full-scale IQ < 80, a history of seizures or other neurological problems, and/or a history of pervasive developmental disorder, schizophrenia, or other psychotic or organic mental disorders.
Of those eligible for enrollment into PALS (n = 516), 70.5% participated (n = 364; MAge = 17.75, SDAge = 3.39, age range 11 – 25). Enrollment into PALS was an average of 8.35 (SD = 2.79) years after childhood diagnosis and STP participation. Enrolled PALS participants were different from non-enrolled on 1 out of 14 childhood demographic and diagnostic variable comparisons. Parent/teacher ratings of CD symptoms were lower (t = 3.09, p < .01) for participants (M = 2.13; SD = 1.93) versus nonparticipants (M = 2.74; SD = 2.19).
NonADHD sample
Participants without ADHD were recruited from the greater Pittsburgh area from several sources (e.g., pediatric practices, local schools). A telephone screening with parents gathered basic demographics, history of diagnosis and treatment for ADHD and other behavior problems including CD, presence of exclusionary criteria as previously listed for the ADHD participants, and a checklist of ADHD symptoms. Young adults (18+) also provided self-report of the same information. In addition to the exclusion criteria listed for the ADHD sample, individuals who met DSM-III-R criteria for ADHD (presence of 8 or more symptoms reported by either the parent or young adult), currently or historically, were excluded from the nonADHD sample. Subthreshold ADHD symptoms and other psychiatric disorders were not exclusions. By design, the ADHD and nonADHD samples were demographically similar(18).
Subsample for the current study
Data were selected from the first interview that participants completed the UPPS-P impulsivity questionnaire (N = 289; 30 women, 259 men; MAge = 28.67, SD = 3.38; n = 170 ADHD; n = 119 nonADHD: See Table 1 for demographics presented separately by ADHD group). Participants who completed the UPPS-P did not differ in age, gender, parental education, or race compared to those who were actively participating in PALS but as a result of the age based assessment schedule had not yet completed the UPPS-P. Within the ADHD sample, those who had not yet completed the UPPS-P were more likely to have childhood CD than those who had completed the UPPS-P (40.5% vs 30.6%, X2 = 4.16, p = .04).
Table 1.
Comparison of ADHD and NonADHD participants in the current sample
| ADHD (n = 170) | NonADHD (n = 119) | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | t-test | |
| Continuous Variables | |||
| Current Age | 29.02 (3.39) | 28.15 (3.32) | 2.15* |
| Highest Parental Education | 7.11(1.62) | 7.49 (1.65) | −1.89* |
| Percentage (n) | Percentage (n) | Chi-Square | |
| Dichotomous Variables | |||
| Gender (Male) | 88.7 (152) | 89.7 (107) | .08 |
| Race (White) | 81.18 (138) | 81.51 (97) | .01 |
| Childhood Conduct Disorder Diagnosis | 29.22 (45) | 0 (0) | 41.64*** |
Note:
p < .05,
p < .01,
p < .001.
Highest parental education was measured during the initial PALS interview (1999–2003) using a 1 (elementary school) to 9 (graduate school) scale.
Measures
Alcohol problems
A modified version of the Young Adult Alcohol Problems Screening Test (YAAPST19) was used to assess alcohol problems in adulthood. This 36-item questionnaire (response options: 0 = “none or not in the past year” through 3 = “more than 5 times”) assesses how frequently problems occurred while drinking or as a result of drinking within the past year. The YAAPST has been shown to have good reliability(e.g., 19). For the current study, the number of different problems reported (range 0–28; M = 2.50; SD = 3.97) was the outcome variable to allow for a two-part modeling statistical approach.
Impulsivity
Five impulsivity facets were assessed using the 59-item UPPS-P impulsive behavior scale(20,21): (lack of) planning (11 items: α = .90; e.g., “My thinking is usually careful and purposeful”), sensation seeking (12 items: α = .87; e.g., “I generally seek new and exciting experiences and sensations”), (negative) urgency (12 items: α = .92; e.g., “In the heat of an argument, I will often say things that I later regret”), (positive) urgency (14 items: α = .95; e.g., “When I am really excited, I tend not to think of the consequences of my actions”), and (lack of) perseverance (10 items: α =.85; e.g., “I generally like to see things through to the end”). Response options ranged from 1 (agree strongly) to 4 (disagree strongly). All responses were coded so that higher numbers meant higher impulsivity. In the current sample, a high correlation between negative urgency and positive urgency was found (r = .80, p < .001), which resulted in these two facets being non-significant in analyses when examined simultaneously. Based on this multicollinearity and prior research examining positive and negative urgency separately, we conducted analyses separately for these two facets. The other impulsivity facets were moderately correlated (See Table 2).
Table 2.
Correlations between the five facets of impulsivity measured by the UPPS-P
| facet of impulsivity | lack of planning | sensation seeking | negative urgency | positive urgency | lack of perseverance |
|---|---|---|---|---|---|
| lack of planning | - | ||||
| sensation seeking | −.01 | - | |||
| negative urgency | .46*** | −.20*** | - | ||
| positive urgency | .40*** | −.27*** | .80*** | - | |
| lack of perseverance | .65*** | −.24*** | .49*** | .40*** | - |
Note:
p < .05,
p < .01,
p < .001
Covariates
Gender, age (at adult assessment), race (White vs. nonWhite), frequency of alcohol use in the past year (Substance Use Questionnaire22) and CD diagnosis from childhood (assessed at the same time as childhood ADHD) were included as covariates in the analyses. Past year alcohol frequency was controlled for because we were specifically interested in whether individuals with childhood ADHD experienced more alcohol problems at comparable levels of use compared to those without ADHD histories. CD was based on positive parent and teacher rating scale reports of DSM symptoms(17) and a semi-structured parent interview in childhood for the ADHD participants. None of the nonADHD group participants had childhood CD based on parent retrospective report with the same standardized rating scales used in childhood for the ADHD group.
Analytic Overview
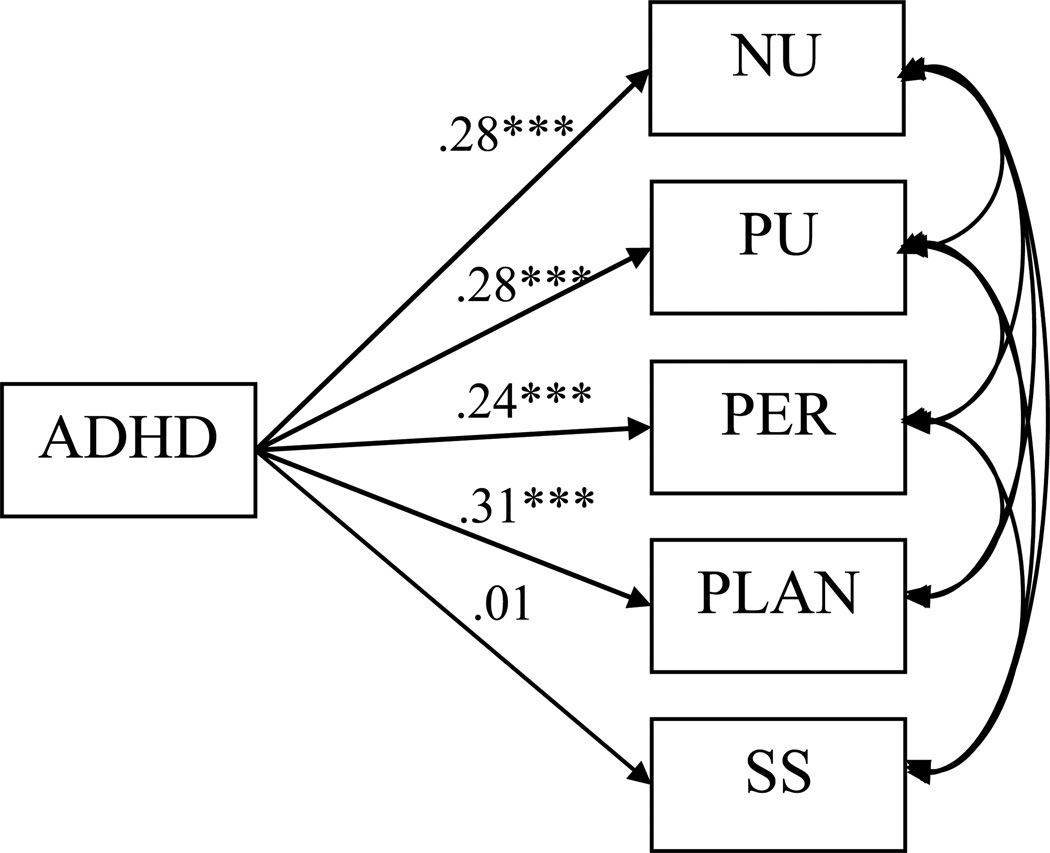
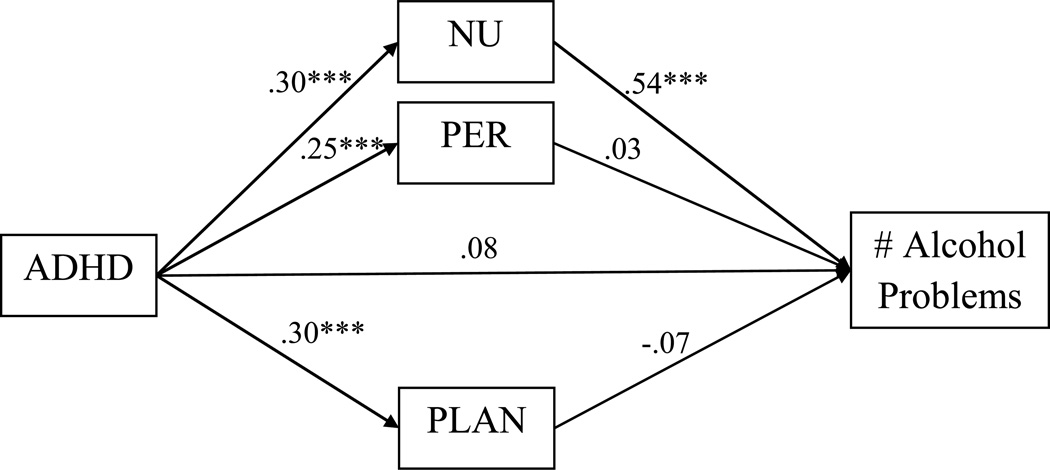
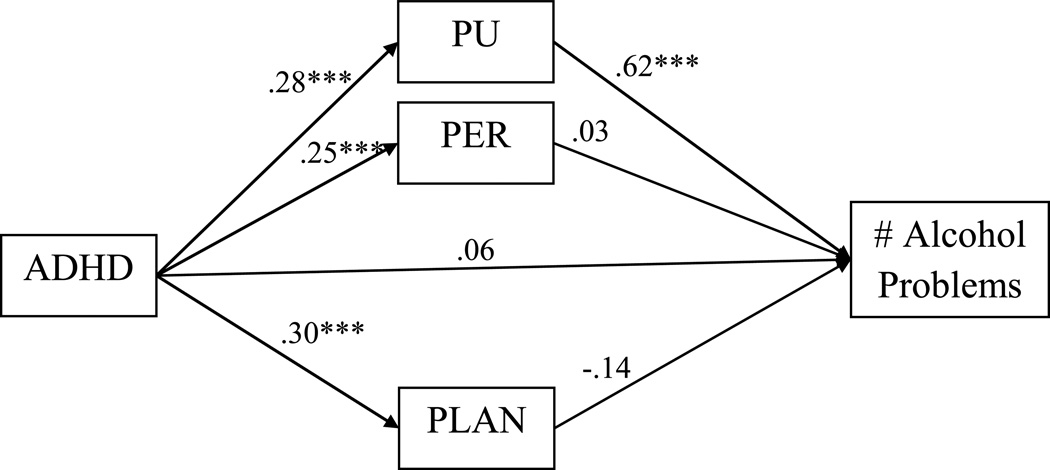
Structural equation models (SEM) utilizing Mplus 7.0(23) were estimated to test our primary hypotheses. First, the associations between ADHD and past year alcohol problems were examined after controlling for demographic covariates (age, gender, and race), past year alcohol use frequency, and CD. Second, the associations between ADHD and the impulsivity facets were examined (Figure 2) with demographic covariates included. Separate models assessed the associations between the impulsivity facets and alcohol problems (same covariates). Finally, mediation models of the indirect associations between ADHD and alcohol problems through the impulsivity facets (same covariates) were tested (Figures 3 and 4). The significance of the indirect effects was tested using MODEL CONSTRAINT in Mplus(24).
Figure 2.
Associations between ADHD and the five UPPS traits. To ease presentation of the results, only significant correlations between the UPPS-P traits are presented using arches. Age, gender, and race were included as covariates. The reported path coefficients are standardized, and bold lines indicate a significant association in the model. NU = negative urgency; PU = positive urgency; PER = lack of perseverance; PLAN = lack of planning; SS = sensation seeking.
Notes: *p < .05, **p < .01, ***p < .001
Figure 3.
Indirect effects of ADHD on alcohol problems through negative urgency, lack of planning, and lack of perseverance. Age, gender, race, past year alcohol use frequency, and diagnosis of conduct disorder were included as covariates. To ease presentation of the results, only the results for the count outcome are reported. The reported path coefficients are standardized, and bold lines indicate a significant association in the model. NU = negative urgency; PER = lack of perseverance; PLAN = lack of planning.
Notes: *p < .05, **p < .01, ***p < .001
Figure 4.
Indirect effects of ADHD on alcohol problems through positive urgency, lack of planning, and lack of perseverance. Age, gender, race, past year alcohol use frequency, and diagnosis of conduct disorder were included as covariates. To ease presentation of the results, only the results for the count outcome are reported. The reported path coefficients are standardized, and bold lines indicate a significant association in the model. PU = positive urgency; PER = lack of perseverance; PLAN = lack of planning.
Notes: *p < .05, **p < .01, ***p < .001
Alcohol problems were modeled using zero-inflated negative binomial (ZINB) regressions. ZINB models account for both the number of zeroes present and the overdispersion of the data for this variable. ZINB models address the excess zeroes in an outcome variable by specifying two forms of the outcome variable: a count variable, adjusted for overdispersion, and a logit variable(25). Thus, the models in the present study assessed the likelihood of experiencing an alcohol problem as well as individual differences in the number of alcohol problems experienced.
Results
ADHD, Alcohol Problems, and Impulsivity Facets
Childhood ADHD significantly predicted more (number of unique) alcohol problems in adulthood (β = .34, p < .05) but not the likelihood of reporting any vs. no alcohol problem (β = .04, p = .76). Descriptive statistics parallel the ZINB models. NonADHD participants reported zero to 18 different alcohol problems in the past year (M = 2.71, SD = 3.30; 35.0% reported 0 alcohol problems). ADHD participants reported zero to 28 different alcohol problems (M = 2.35, SD = 4.38; 51.2% reported 0 alcohol problems). Among participants reporting any alcohol problem, nonADHD participants reported an average of 4.17 problems (SD = 3.27) and ADHD participants reported an average of 4.82 problems (SD = 5.24).
Childhood ADHD significantly predicted higher levels of four of the five impulsivity facets in adulthood (Figure 2): lack of planning (β = .31, p < .001), lack of perseverance (β = .24, p < .001), negative urgency (β = .28, p < .001), and positive urgency (β = .28, p < .001). Childhood ADHD did not significantly predict sensation seeking (β = .01, p = .82).
Impulsivity Facets and Alcohol Problems
When examined separately, four of the five impulsivity facets were significantly associated with a higher number of alcohol problems: lack of planning (β = .34, p < .05), lack of perseverance (β = .36, p < .05), negative urgency (β = .55, p < .001), and positive urgency (β = .61, p < .001). In analyses examining lack of planning, lack of perseverance, and negative urgency simultaneously, only negative urgency remained significantly associated with number of alcohol problems (β = .56, p < .001). Similarly, only positive urgency remained significantly associated with number of different alcohol problems (β = .64, p < .001) in analyses examining lack of planning, lack of perseverance, and positive urgency simultaneously. None of the impulsivity facets were associated with the likelihood of having an alcohol problem. As sensation seeking was not significantly related to number of alcohol problems (β = .18, p = .39), or to ADHD, it was eliminated as a potential mediator of the association between ADHD and alcohol problems.
Indirect Effect of ADHD on Alcohol Problems through Impulsivity Facets
Negative (b = .26, p < .001), and positive (b = .24, p < .01), urgency significantly mediated the association between ADHD and number of alcohol problems when examined separately. Lack of perseverance marginally mediated the association between ADHD and number of alcohol problems (b = .10, p = .05). Lack of planning did not (b = .09, p = .11). In analyses examining lack of planning, lack of perseverance, and negative urgency simultaneously, only negative urgency remained as a significant mediator of the association between ADHD and number of alcohol problems (b = .26, p < .01; Figure 3). In parallel analyses examining lack of planning, lack of perseverance, and positive urgency, only positive urgency remained as a significant mediator (b = .27, p < .01; Figure 4).
Discussion
While individuals with ADHD have been shown to be at increased long-term risk for experiencing an alcohol use disorder, research on the underlying pathways linking these two disorders is only just emerging. The current study addressed an important gap in the literature by examining specific impulsivity facets that may link childhood ADHD with later alcohol problems. Specifically, we found that having a diagnosis of childhood ADHD was prospectively related to a higher number of different alcohol problems and higher levels of four facets of impulsivity (lack of planning, lack of perseverance, positive urgency, and negative urgency) in adulthood. Additionally, we found support for an emotional impulsivity risk pathway whereby negative and positive urgency accounted for the association between childhood ADHD and adult alcohol problems. To our knowledge, this study is the first to demonstrate that impulsive tendencies, in the context of strong positive or negative mood, are significantly related to alcohol problems in adulthood for individuals who had ADHD in childhood.
Our findings underscore the importance of examining impulsivity in a disaggregated fashion to identify why individuals with childhood ADHD may be at increased risk for ultimately developing an alcohol use disorder. Research on children with ADHD has shown an increased tendency for many of them to be emotionally dysregulated(e.g., 15). Further, impulsivity may play a critical role in this emotion dysregulation(26,27), which highlights the potential importance of the domain of emotional impulsivity for those with ADHD. Our findings are directly in line with this prior work, showing that not only is having a childhood diagnosis of ADHD related to higher levels of positive and negative urgency in adulthood but that these domains of impulsivity explain the association between ADHD and alcohol problems.
Much has been written about the negative emotions associated with heavy drinking in adulthood, and it is often assumed that children with ADHD should be at risk for this co-occurrence(for review, see 28). Although we found support for this idea in the link with negative urgency, our findings suggest that a combination of positive mood and poor behavioral control may also lead to more negative alcohol-related consequences for these individuals. This is a particularly interesting finding because it suggests that some risky decisions made while drinking may occur during celebratory events or in other contexts connected to happiness or excitement.
Prior research has shown differential prediction of risk taking behavior from positive versus negative urgency(for review, see 29) and only modest relations between these facets (e.g., r = .37)20. However, in our sample they were highly related (r = .80) which resulted in multicollinearity and precluded the simultaneous examination of these facets. Future research parsing out positive and negative urgency in real time through ecological momentary assessment techniques may increase understanding of why and in what situations individuals with ADHD are likely to make risky decisions while drinking. For example, examining risky decisions made while someone is intoxicated and in a positive mood may differ from those made while in a negative mood. Examination of fluctuations in emotional impulsivity may provide proximal points of intervention (e.g., emotion regulation skills prior to drinking) in this at risk population.
Although the current study has many strengths (e.g., longitudinal design, clinic referred sample) several limitations warrant acknowledgement. First, as a result of when the UPPS-P impulsivity questionnaire was added into this ongoing study, we are currently unable to examine impulsivity facets and alcohol problems at different time points. While ADHD diagnosis occurred on average over 15 years prior to the adult assessment, we recognize the literature that has shown a bi-directional transaction between heavy alcohol use and impulsivity over time. We conceptualized impulsivity facets as the mediators in the models tested based on a large body of literature identifying these personality characteristics as preceding heavy alcohol use(e.g., 3).
Contrary to our hypothesis, childhood ADHD and impulsivity were not associated with the past year experience of any, versus zero, alcohol problems. While surprising, a dichotomous alcohol problem outcome may be more meaningful in other populations. For example, the likelihood of experiencing any alcohol problem is lower in adolescence so in this age group ADHD and impulsivity may be more strongly related to a likelihood outcome as opposed to the number of different problems. Additionally, our sample was predominantly male and a sample with more females could alter results as women, on average, experience fewer alcohol problems. Lastly, extending this research to the examination of other substances is particularly important given that ADHD has been shown to be more strongly associated with other substances relative to alcohol(e.g., 30,31). Future work with different ages, in samples with more women, and focused on the examination other drugs (e.g., marijuana) is critical and may help explain these unexpected null findings for ADHD and impulsivity relating to likelihood of experiencing an alcohol problem.
Additionally, while we controlled for CD, we did not have the ability to examine a group of individuals who met criteria for CD but not ADHD. Research has shown that CD and novelty seeking may be stronger prospective predictors of substance use than ADHD(e.g., 32). Future research with broad representation of these externalizing behaviors is needed to determine if the pathways that we identified are specific to ADHD or represent a broader pathway from childhood externalizing disorders to later alcohol problems. In addition, examining persistence of ADHD symptoms over time, conjointly with measurements of the impulsivity facets, is an important next step to understand the distinctiveness of these potential influences on alcohol problems.
Our study relied solely on self-report and may under-estimate the degree to which impulsivity contributes to alcohol problem risk. Research has shown that children with ADHD tend to under-report their symptoms and impairment and that this may also exist in adulthood(33,34). Longitudinal research that includes behavioral components of impulsivity assessed via task performance, which have been shown to relate to alcohol consumption and differ for those with compared to without ADHD(e.g., 35), could prove to be a fruitful next step in this line of research. Additionally, incorporating collateral reports (e.g., romantic partner) may further mitigate this potential issue of under-reporting.
Despite the limitations noted above, the current study addresses several existing gaps in the literature that have been identified in recent theoretical reviews(e.g., 28) and have several implications for understanding and ultimately reducing ADHD risk of alcohol problems. Specifically, adults with a history of ADHD had elevated levels of multiple impulsivity traits compared to those without childhood ADHD. Of particular importance were the findings for negative and positive urgency that support an emotional impulsivity risk pathway for this population. A subset of children with ADHD may have elevated levels of urgency that continues into adulthood and may be particularly at risk for experiencing alcohol problems and alcohol use disorder. These results suggest that future treatment targets for this population may need to include strategies that specifically focus on impulsive decision making in the context of strong positive and negative emotions.
Acknowledgments
This research was principally supported by grants from the National Institute on Alcohol Abuse and Alcoholism: AA011873, AA007453, and AA00202. Additional support was provided by DA12414, MH50467, MH12010, ESO5015, AA12342, DA016631, MH065899, KAI-118-S1, DA85553, MH077676, MH069614, MH62946, MH065899, MH53554, MH069434, IES LO3000665A, IESR324B060045, & NS39087. Dr. Pedersen was supported by K01 AA021135.
References
- 1.Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin Psychol Rev. 2011;31(3):328–341. doi: 10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: Comparative meta-analyses. J Am Acad Child Adolescent Psychiatry. 2011;50(1):9–21. doi: 10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 3.Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O'Malley SS, et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict Biol. 2010;15(2):217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol. 2009;14(1):22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- 6.Winstanley CA, Eagle DM, Robbins TW. Behavioral models of impulsivity in relation to ADHD: translation between clinical and preclinical studies. Clin Psychol Rev. 2006;26(4):379–395. doi: 10.1016/j.cpr.2006.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howard AL, Molina BS, Swanson JM, Hinshaw SP, Belendiuk KA, Harty SC, et al. Developmental progression to early adult binge drinking and marijuana use from worsening versus stable trajectories of adolescent ADHD and delinquency. Addiction. 2015;110(5):784–795. doi: 10.1111/add.12880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64(10):1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- 9.Molina BS, Pelham WE, Cheong J, Marshal MP, Gnagy EM, Curran PJ. Childhood attention-deficit/hyperactivity disorder (ADHD) and growth in adolescent alcohol use: the roles of functional impairments, ADHD symptom persistence, and parental knowledge. J Abnorm Psychol. 2012;121(7):988–935. doi: 10.1037/a0028260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roberts W, Peters JR, Adams ZW, Lynam DR, Milich R. Identifying the facets of impulsivity that explain the relation between ADHD symptoms and substance use in a nonclinical sample. Addict Behav. 2014;39(8):1272–1277. doi: 10.1016/j.addbeh.2014.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rooney M, Chronis-Tuscano A, Huggins S. Disinhibition mediates the relationship between ADHD and problematic alcohol use in college students. J Atten Disord. 2015;19(4):313–327. doi: 10.1177/1087054712459885. [DOI] [PubMed] [Google Scholar]
- 12.Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res. 2013;37(9):1441–1450. doi: 10.1111/acer.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez R, Dauvilliers Y, Jaussent I, Billieux J, Bayard S. A multidimensional approach of impulsivity in adult attention deficit hyperactivity disorder. Psychiatry Res. 2015;227(2):290–295. doi: 10.1016/j.psychres.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 14.Miller DJ, Derefinko KJ, Lynam DR, Milich R, Fillmore MT. Impulsivity and attention deficit-hyperactivity disorder: subtype classification using the UPPS impulsive behavior scale. J Psychopathol Behav. 2010;32(3):323–332. doi: 10.1007/s10862-009-9155-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shaw P, Stringaris A, Nigg J, Leibenluft E. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 2014;171(3):276–293. doi: 10.1176/appi.ajp.2013.13070966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pelham WE, Hoza B. Psychosocial treatments for child and adolescent disorders: Empirically based strategies for clinical practice. New York: APA Press; 1996. Intensive treatment: A summer treatment program for children with ADHD; pp. 311–340. [Google Scholar]
- 17.Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1992;31(2):210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Molina BS, Pelham WE, Gnagy EM, Thompson AL, Marshal MP. Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcohol Clin Exp Res. 2007;31(4):643–654. doi: 10.1111/j.1530-0277.2007.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurlburt SC, Sher KJ. Assessing alcohol problems in college students. J Am Coll Health. 1992;41(2):49–58. doi: 10.1080/07448481.1992.10392818. [DOI] [PubMed] [Google Scholar]
- 20.Cyders MA, Smith GT, Spillane NS, Fischer S, Annus AM, Peterson C. Integration of impulsivity and positive mood to predict risky behavior: development and validation of a measure of positive urgency. Psychol Assess. 2007;19(1):107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- 21.Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Pers Individ Dif. 2001;30(4):669–689. [Google Scholar]
- 22.Molina BS, Pelham WE., Jr Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol. 2003;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- 23.Muthén L, Muthén B. Mplus User's Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 24.Muthén BO. Applications of Causally Defined Direct and Indirect Effects in Mediation Analysis using SEM in MPlus. 2011 [Google Scholar]
- 25.Group USC, editor. Mplus Data Analysis Examples: Zero-Inflated Negative Binomial Regression. [Google Scholar]
- 26.Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull. 1997;121(1):65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- 27.Walcott CM, Landau S. The relation between disinhibition and emotion regulation in boys with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol. 2004;33(4):772–782. doi: 10.1207/s15374424jccp3304_12. [DOI] [PubMed] [Google Scholar]
- 28.Molina BS, Pelham WE. Attention-deficit/hyperactivity disorder and risk of substance use disorder: developmental considerations, potential pathways, and opportunities for research. Annu Rev Clin Psychol. 2014;10:607–639. doi: 10.1146/annurev-clinpsy-032813-153722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull. 2008;134(6):807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nigg JT. Attention-deficit/hyperactivity disorder and adverse health outcomes. Clin Psychol Rev. 2013;33(2):215–228. doi: 10.1016/j.cpr.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sibley MH, Pelham WE, Jr, Molina BS, Coxe S, Kipp H, Gnagy EM, Meinzer M, Ross JM, Lahey BB. The role of early childhood ADHD and subsequent CD in the initiation and escalation of adolescent cigarette, alcohol, and marijuana use. Journal of abnormal psychology. 2014;123(2):362–374. doi: 10.1037/a0036585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Palmer RH, Knopik VS, Rhee SH, Hopfer CJ, Corley RC, Young SE, Stallings MC, Hewitt JK. Prospective effects of adolescent indicators of behavioral disinhibition on DSM-IV alcohol, tobacco, and illicit drug dependence in young adulthood. Addictive behaviors. 2013 Sep 30;38(9):2415–2421. doi: 10.1016/j.addbeh.2013.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol. 2002;111(2):279–289. [PubMed] [Google Scholar]
- 34.Sibley MH, Pelham WE, Molina BS, Gnagy EM, Waxmonsky JG, Waschbusch DA, et al. When diagnosing ADHD in young adults emphasize informant reports, DSM items, and impairment. J Consult Clin Psychol. 2012;80(6):1052–1061. doi: 10.1037/a0029098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weafer J, Milich R, Fillmore MT. Behavioral components of impulsivity predict alcohol consumption in adults with ADHD and healthy controls. Drug Alcohol Depend. 2011;113:139–148. doi: 10.1016/j.drugalcdep.2010.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]