Abstract
Purpose
Monocytes may be primed towards differentiation into classically activated M1 macrophages or alternatively activated M2 macrophages. M1 macrophages greatly contribute to the inflammation which promotes insulin resistance, whereas M2 macrophages resolve inflammation. We have previously shown that exercise increases M2 marker expression in mixed mononuclear cells, possibly via activation of the nuclear transcription factor PPARγ. However, these effects have not been demonstrated specifically within monocytes. Thus, we aimed to investigate whether moderate-intensity exercise elicited similar effects on monocytic M1/M2 marker expression and PPARγ activity to those reported previously in mononuclear cells, so as to further elucidate the mechanisms by which exercise may alter inflammatory status and, accordingly, prevent insulin resistance.
Methods/results
19 sedentary females completed an 8 week moderate-intensity exercise programme (walking 45 min, thrice weekly). Monocytes were isolated from blood via immunomagnetic separation; monocyte expression of M2 markers (Dectin-1: 2.6 ± 1.9-fold; IL-10: 3.0 ± 2.8-fold) significantly increased, whilst the expression of the M1 marker MCP-1 significantly decreased (0.83 ± 0.2 cf. basal), over the duration of the programme. Serum PPARγ activity levels and PPARγ target-genes (CD36: 1.9 ± 1.5-fold; LXRα: 5.0 ± 4.7-fold) were significantly increased after the 8 week exercise programme. Associated with these effects were significant improvements in systemic insulin sensitivity (McAuley’s ISI: Δ0.98 M/mU/L cf. basal).
Conclusion
Exercise participation suppressed M1 markers and induced M2 markers in monocytes, potentially via PPARγ-triggered signalling, and these effects may contribute (perhaps via priming of monocytes for differentiation into M2 tissue-macrophages) to improved systemic insulin sensitivity in exercising participants. These findings provide an alternative mechanism by which exercise may exert its anti-inflammatory effects in order to prevent insulin resistance and type 2 diabetes.
Electronic supplementary material
The online version of this article (doi:10.1007/s00421-016-3414-y) contains supplementary material, which is available to authorized users.
Keywords: Monocyte, Polarisation, Exercise, PPARγ, Insulin resistance
Introduction
Insulin resistance is a prerequisite for the development of type 2 diabetes (T2D) (Defronzo and Tripathy 2009; Petersen et al. 2007) with its pathogenesis being strongly associated with the development of chronic local and systemic inflammation (Goldfine et al. 2013; Samuel and Shulman 2012). It has previously been shown that individuals with insulin resistance have a chronically elevated inflammatory status (Harford et al. 2011; Olefsky and Glass 2010), with some inflammatory mediators directly impairing insulin signalling by activating protein kinases to induce deleterious alternative phosphorylation of insulin signalling molecules (Olefsky and Glass 2010). Taken together, it is clear that chronic inflammation plays a key role in the development of insulin resistance and T2D.
Physical activity has long been known to aid in the prevention and management of insulin resistance, whereas a sedentary lifestyle is associated with increased risk of metabolic disease (Colberg et al. 2010). Several key studies have demonstrated that exercise training may prevent T2D incidence by approximately 50 %, either as a lone therapy (Pan et al. 1997) or in combination with other lifestyle interventions such as diet counselling or weight loss (Diabetes Prevention Program Research Group 2002; Eriksson et al. 1999). Interestingly, the effects of lifestyle modification appear to be stronger than those achieved with the pharmacological intervention of metformin (Knowler et al. 2002). As such, physical activity can play an important role in the prevention and management of T2D, and understanding the mechanisms by which physical activity improves insulin sensitivity may aid in the optimisation of effective non-pharmacological therapies. One mechanism by which exercise might improve insulin sensitivity may involve its impact on inflammation (Golbidi et al. 2012; Petersen and Pedersen 2005). For example, in response to exercise, muscle-derived IL-6 promotes elevated levels of anti-inflammatory cytokines, such as IL-10 and IL-1 receptor antagonist (IL-1Ra) (Febbraio and Pedersen 2002; Kristiansen and Mandrup-Poulsen 2005; Petersen and Pedersen 2005; Scheller et al. 2011), potentially inhibiting the actions of pro-inflammatory mediators to bring about benefits with regard to chronic inflammatory conditions (Golbidi et al. 2012; Febbraio and Pedersen 2002; Petersen and Pedersen 2005).
Macrophages are immune cells which exist in almost every tissue type (Geissmann et al. 2010). Under certain conditions, such as in acute inflammation, macrophage populations may be replenished by extravasation of circulating monocytes, which then differentiate into mature macrophages within tissues (Ginhoux and Jung 2014; Haldar and Murphy 2014). Macrophages exist in several different phenotypic states, depending on the stimuli to which they are exposed (Mantovani et al. 2004); for example, interferon-γ (IFN-γ; either alone or in combination with microbial ligands or other cytokines e.g., TNFα or MCP-1) gives rise to ‘classically activated’ M1 macrophages, which are characteristically pro-inflammatory, whilst IL-4 and/or IL-13 stimulation promotes the production of ‘alternatively activated’ M2 macrophages, which play regulatory and anti-inflammatory roles (Mantovani et al. 2004; Mosser and Edwards 2008; Sica and Mantovani 2012). It is thought that pro-inflammatory macrophages are major instigators of the inflammation which drives insulin resistance (Huang et al. 2010; Osborn and Olefsky 2012; Romeo et al. 2012). In support of this, macrophage-specific inhibition of the IKKβ or JNK pro-inflammatory pathways was found to protect against insulin resistance (Arkan et al. 2005; Han et al. 2013). Furthermore, it has been found that macrophages in individuals with obesity and/or T2D are skewed towards the M1 phenotype (Chinetti-Gbaguidi and Staels 2011; Lumeng et al. 2007; Pradhan Nabzdyk et al. 2013; You et al. 2013), while deletion of peroxisome proliferator activated receptor gamma (PPARγ), an important regulator of M2 polarisation, in murine macrophage cells promoted diet-induced systemic insulin resistance and/or glucose intolerance (Hevener et al. 2007; Odegaard et al. 2007). Exercise has also been shown to have a beneficial impact on immune cell function within tissues, and on local and systemic inflammation. For example, exercise training in obese individuals reduced systemic inflammation, specifically via decreased macrophage infiltration into adipose tissue (Bruun et al. 2006) whilst others have demonstrated a significant link between the influence of exercise on tissue-macrophages and the pathogenesis of insulin resistance (Ikeda et al. 2013; Kawanishi et al. 2010; Oliveira et al. 2013).
Interestingly, we have previously shown that exercise may upregulate PPARγ expression and activity in mixed peripheral mononuclear cells (PMNCs; cells which include monocytes) (Butcher et al. 2008; Thomas et al. 2012; Yakeu et al. 2010). We, and others, have also found that, following participation in exercise, macrophages and PMNCs appear to adopt a less inflammatory, M2-like phenotype (Ikeda et al. 2013; Oliveira et al. 2013; Yakeu et al. 2010). Since PPARγ has also been deemed ‘critical’ in priming monocytes for the M2 macrophage phenotype (Bouhlel et al. 2007), these findings suggest that the insulin-sensitising, anti-inflammatory effects of exercise may be attributed, in part to its ability to upregulate PPARγ-activity in monocyte/macrophages (Yakeu et al. 2010).
Therefore, the present research aimed to determine the effects of an 8 week, moderate-intensity exercise programme on expression of markers of M1 or M2 polarisation in isolated human monocytes, and to investigate the mechanisms behind any observed changes. We aimed to test the hypotheses that such an exercise programme brings about anti-inflammatory insulin-sensitising systemic effects within participants; that markers of M2 polarisation in primary human monocytes are induced following participation in the exercise programme; and that PPARγ signalling is increased by exercise, supporting a putative role for this signalling molecule in exercise-associated anti-inflammatory M2 macrophage polarisation.
Materials and methods
Participant recruitment
Exclusion criteria included; a physically active lifestyle [assessed using a short version International Physical Activity Questionnaire (IPAQ)], a history of cardiovascular disease (CVD) and any individuals on prescribed lipid-lowering or metabolism-altering drugs. A power calculation (Minitab v16) was used to determine that a sample size of at least 11 was required for this study. To account for a 25–30 % attrition rate, it was decided to recruit 19 healthy, yet sedentary participants onto the study (convenience sampling resulted in a female only cohort with a mean age of 42 ± 11 years). Informed consent was obtained from all participants and ethics was granted by the School of Health Sciences’ School Research Ethics Committee (SREC) at Cardiff Metropolitan University, Cardiff, UK.
Pre-study screening/baseline measures
Body mass, height, BMI and waist circumference were measured using standard protocols (Butcher et al. 2008). Participant fitness was estimated using the submaximal Rockport Fitness Walking Test (Kline et al. 1987), where, following a 4 min familiarisation/warm up period, participants were required to walk as fast as possible for 1 mile (1.6 km) on a treadmill (Woodway Desmo, Waukesha, USA). Heart rate (HR) upon completion was measured using a Polar S410 HR monitor (Polar Electro, Finland) and time of completion was taken. VO2max was estimated using the following formula (Kline et al. 1987):
Estimated VO2max and anthropometric measures were taken at baseline and repeated upon completion of the exercise programme, ensuring a 24 h rest period between the final exercise session and the VO2max test, in both cases.
Exercise programme design
The exercise programme consisted of three 45 min walking sessions on a treadmill (Woodway Desmo, Waukesha, USA) per week for 8 weeks, totalling 24 fully supervised walking sessions. Treadmill walking speeds were set to ensure that participants exercised at moderate intensity (55–69 % of HRmax; HRmax = 220-age in years) (Bagchi and Preuss 2012). In subsequent sessions, HR was monitored using a Polar S410 HR monitor (Polar Electro, Finland) once weekly, at rest and then at 5, 15, 30 and 45 min into the exercise session. Throughout programme participation, walking speed was altered according to changes in HR to maintain a constant exercise intensity.
Blood sampling
Participants were fasted for 12 h prior to blood collection by venipuncture of the antecubital vein. Blood was collected at four time points; immediately prior to (baseline; Wk 0, T0) and immediately following the first exercise session (Wk 0, T1) and immediately prior to (Wk 8, T0) and immediately following (Wk 8, T1) the final exercise session (T0 and T1 indicate pre- or post-exercise, respectively). A 24 h rest period was left between the penultimate exercise session and procurement of the ‘Wk 8, T0’ sample.
Serum procurement
Whole blood was collected in plain blood tubes and allowed to clot prior to centrifugation for 10 min at 3000×g. Serum was stored in aliquots at −80 °C.
Blood fractionation and monocyte purification
Whole blood was collected in EDTA and fractionated via density gradient centrifugation using Histopaque®-1077 (Sigma–Aldrich, Dorset, UK). The mononuclear cell layer was collected, washed in isotonic phosphate buffered saline (PBS) solution and centrifuged (300×g/10 min) to pellet mononuclear cells. An additional platelet wash (200×g/10 min) was carried out to remove contaminating platelets. Following this, monocytes were isolated via magnetic cell isolation using CD14 MACS MicroBeads (Miltenyi Biotec, Germany), as per manufacturer’s instructions, and monocyte purity was assessed using flow cytometry (see online resources ESM). Labelled cells were removed from the column and harvested by centrifuged.
Biochemical analysis
Serum cholesterol, HDL, triglyceride and glucose levels were analysed, using an iLab 300 Plus analyser (Instrumentation Laboratories UK ltd, Warrington, UK). Serum LDL was quantified indirectly using the Friedewald (Friedewald et al. 1972) equation ; all values expressed in mmol/l). Serum insulin was measured using the Invitrogen Insulin Assay Kit, as per manufacturer’s instruction (Invitrogen Ltd, Paisley, UK). The Berthold Technologies Centro Plate Luminometer (Herts, UK) was used to measure luminescence, whilst insulin concentrations were determined using MikroWin® software.
Calculation for insulin sensitivity
The McAuley’s score for measuring the insulin sensitivity index (McAuley’s ISI) was used as a surrogate measure of insulin resistance. This calculation has been found to be suitable for estimations of insulin resistance in normoglycaemic individuals, such as the participants within this study (Ascaso et al. 2003; McAuley et al. 2001). McAuley’s ISI was calculated as follows:
where I0 = fasting insulin (mU/l), BMI = body mass index (kg/m2), TG = fasting triglycerides (mmol/l).
RNA isolation/RT-PCR
TRI reagent® (Applied Biosystems, Warrington, UK) was used to obtain RNA from monocyte samples, as per manufacturer’s instructions. RNA quantity and quality were assessed using the NanoDrop® ND-1000 spectrophotometer (Thermo Fisher Scientific, Leicester, UK) and RNA was converted into cDNA using a High Capacity cDNA Reverse Transcription kit (Applied Biosystems, Warrington, UK), as per manufacturer’s instructions. Gene expression was carried out on an Applied Biosystems Fast 7500 Real-Time PCR System (Warrington, UK) using Fast SYBR® Green or TaqMan® Fast Universal (No AmpErase® UNG) methodologies. For Fast SYBR® Green, primers were designed using National Center for Biotechnology Information’s ‘Primer-BLAST’ primer designing tool, and made to order (Sigma–Aldrich, Dorset, UK). The following primer sequences were used:
Dectin-1. Fwd: 5′- GGAAGCAACACATTGGAGAATGG-3′; Rev: 5′- CTTTGGTAGGAGTCACACTGTC-3′
IL-10. Fwd: 5′-ACGGCGCTGTCATCGATT-3′; Rev: 5′-TTGGAGCTTATTAAAGGCATTCTTC-3′
IL-1Ra. Fwd: 5′-GGCCTCCGCAGTCACCTAATCAC-3′; Rev: 5′-GGACAGGCACATCTTCCCTCCAT-3′
TNFα. Fwd: 5′-TGCCTGCTGCACTTTGGAGTGA-3′; Rev: 5′- CTGGGCCAGAGGGCTGATTAGAGA-3′
CD36. Fwd: 5′-GGAAGTGATGATGAACAGCAGC-3′; Rev: 5′- GAGACTGTGTTGTCCTCAGCGT-3′
LXRα. Fwd: 5′-CGCACTACATCTGCCACAGT-3′; Rev: 5′-TGAGGCGGATCTGTTCTTCT-3′
ABCA1. Fwd: 5′-GCACTGAGGAAGATGCTGAAA-3′; Rev: 5′-AGTTCCTGGAAGGTCTTGTTCA-3′
COX-2. Fwd: 5′-TGAAACCCACTCCAAACACA-3′; Rev: 5′-GAGAAGGCTTCCCAGCTTTT-3′
GAPDH. Fwd: 5′-CATTGACCTCAACTACATG-3′; Rev: 5′-TCTCCATGGTGGTGAAGAC-3′.
Alternatively, TaqMan® RT-PCR was used to determine MCP-1, IL-4 receptor α (IL-4Rα) and PPARγ gene expression. For TaqMan® experiments, pre-designed PrimeTime® Assays (Integrated DNA Technologies, Iowa, USA) which detected all genetic variants but not genomic DNA and those in which exon boundaries were consolidated were selected for use (assay configuration: 6-FAM/ZEN/IBFQ, P:P 2.0). A non-template control (NTC; nuclease free water instead of cDNA) was included for each gene analysed. The comparative CT method was used to calculate gene expression relative to the reference sample. Data were only included if plots of log[RNA] versus ΔCT resulted in slopes of between −0.1 and +0.1, meaning that amplicon efficiencies were approximately equal, and if plots of log template versus CT gave slopes of approximately −3.3 (representing 100 % PCR efficiency). Baseline samples, i.e., those taken prior to the 8 week exercise programme, were used as reference samples.
Gene reporter assays
Two gene reporter assays were conducted to investigate (1) the PPARγ activating properties of serum (‘PPRE-Luc’) and (2) PPARγ ligand availability (‘PPARγ-LBD’) in serum samples obtained from study participants. Human embryonic kidney (HEK-293T) cells (ATCC, Middlesex, UK) were maintained under standard conditions in DMEM (Invitrogen Ltd, Paisley, UK), supplemented with 10 % US Defined, Irradiated and Heat inactivated Fetal Bovine serum (FBS; Thermo Fisher Scientific, Leicester, UK), 100 U/mL penicillin/100 μg/mL streptomycin mix and 4 mM l-glutamine (Invitrogen Ltd, Paisley, UK). Cells were seeded in opaque 96-well plates at 2 × 105 cells/well and incubated in a 37 °C, 5 % CO2, humidified incubator for 24 h prior to transient transfection.
PPRE-Luc
Cells were transfected with 100 ng of each of the PPRE-luciferase reporter construct and the PPARγ expression vector and 2 ng of the Renilla plasmid, using Lipofectamine® LTX Reagent (Invitrogen Ltd, Paisley, UK) according to manufacturer’s instructions and as previously described (Thomas et al. 2012). Cells were incubated with plasmids in a 37 °C, 5 % CO2, humidified incubator for a further 24 h, following which media was removed and replaced with plasma samples [normalised for protein content and added at 10 % (v/v) to DMEM (minus FBS)]. Alternatively cells were treated with 1 µM rosiglitazone (a known activator of PPARγ) as a positive control. After 24 h, cells were harvested and lysed and luminescence was analysed using the Dual-Luciferase® Reporter Assay System (Promega, Southampton, UK) as per manufacturer’s instructions. Luminescence values were normalised with regard to transfection efficiency by use of a ratio of Luciferase:Renilla luminescence and reported as relative light units (RLU).
PPARγ-LBD
Cells were transfected with 2 μg of a fusion vector carrying the PPARγ-LBD fused with the GAL4 DNA-binding domain (DBD) [PPARγ-LBD/GAL4-DBD; (Tzameli et al. 2004)], 2 μg of an Upstream Activation Sequence (UAS; GAL4 response element)-luciferase reporter construct [UAS; (Collingwood et al. 1997)] and 0.5 μg of β-gal, diluted in 1.5 mL unsupplemented DMEM and mixed with TransFastTM Transfection Reagent (Promega, Southamptom, UK) in a 3:1 charge ratio of TransFast™ (μL) to DNA (μg). The TransFast™-plasmid mix was incubated for 10 min before cells were incubated with the plasmids in a 37 °C, 5 % CO2, humidified incubator for 1 h, before 2.5 mL of supplemented DMEM media (minus antibiotics) was added to cells. Cells were incubated with plasmids for a further 24 h, following which media was removed and replaced with plasma samples [normalised for protein content and added at 10 % (v/v) to DMEM (minus FBS)]. Alternatively cells were treated with 1 µM rosiglitazone (a known activator of PPARγ) as a positive control. After 24 h, cells were harvested and lysed and 40 μL of each lysate was transferred to the wells of an opaque 96 well plate and 50 μL of LAR II was auto-injected into each well and luminescence readings were taken using a Tecan Infinite 200 plate reader. Simultaneously, for internal control (β-gal) readings, 40 μL of each lysate was transferred into wells of a transparent 96-well plate and an equal volume of o-Nitrophynyl-beta-d-galactopyranosidase (ONPG; β-gal substrate) was added to wells, incubating for 30 min, or until a yellow colour developed. Absorbance was read using the Tecan Infinite 200 plate reader, set at 435 nm. The ratio of Luciferase luminescence to β-gal OD was used to normalise values, and values were reported as RLU.
ELISA
Commercially available ELISA kits were used according to manufacturer’s instructions to determine serum cytokine levels; the Human IL-4 High Sensitivity ELISA (eBioscience, Vienna, Austria) was used to quantify IL-4 and The RayBio® Human IL-13 ELISA Kit (Insight Biotechnology Ltd, Middlesex, UK) was used to quantify IL-13 in ‘Wk 0, T0’ and ‘Wk 8, T0’ serum samples, whilst the Quantikine® HS ELISA Human IL-6 Immunoassay (R&D Systems, Abington, UK) was used to quantify serum IL-6 in ‘Wk 0, T0’ and ‘Wk 0, T1’ serum samples. Spectrophotometry was carried out on a Tecan Infinite 200 (Tecan, Reading, UK).
Statistical analysis
All data were expressed as mean ± standard deviation (SD), unless otherwise stated. Where comparisons were made between the means of two samples, t tests or Wilcoxon’s pairwise analysis were used, depending on data distribution (the D’Agostino and Pearson omnibus normality test was used to test for normal distribution of data). Alternatively, one-way analysis of variance (ANOVA) with Tukey’s post hoc analysis was used for multiple comparisons within groups of normally distributed data. Statistical analysis was performed using GraphPad Prism®5 software and results were deemed significant at p < 0.05.
Results
The effect of an 8-week moderate-intensity walking programme on cardio-metabolic risk markers
Nineteen healthy, yet sedentary female participants were recruited onto the study (mean age of 42 ± 11 years; body weight 76.54 ± 12.54 kg; body mass index (BMI) 29.7 ± 5.1 kg/m2; waist circumference 91.74 ± 13.36 cm; systolic blood pressure 126.3 ± 9.9 mmHg; diastolic blood pressure 78.5 ± 8.8 mmHg. As shown in Table 1, mean body mass was significantly reduced following participation in the exercise intervention [p < 0.05 compared to baseline (‘Wk 0, T0’)], as was BMI (p < 0.05) and waist circumference (p < 0.01). Furthermore, systolic blood pressure showed a non-significant decrease (p = 0.059) and diastolic blood pressure was unaltered. Additionally, there was a significant increase in estimated VO2max (p < 0.01).
Table 1.
Physiological and biochemical parameters at baseline (Wk 0, T0) and after 8 weeks (Wk 8, T0) of exercise participation
| Wk 0, T0 | Wk 8, T0 | Δ (95 % CI) | |
|---|---|---|---|
| Weight (kg) | 76.5 ± 12.5 | 75.7 ± 12.4 | −0.9 (−1.63, −0.09)* |
| BMI (kg/m2) | 29.7 ± 5.1 | 29.4 ± 4.9 | −0.4 (−0.67, −0.04)* |
| Waist circumference (cm) | 91.7 ± 13.4 | 86.2 ± 12.0 | −5.6 (−8.09, −3.05)** |
| Systolic BP (mmHg) | 126.3 ± 9.9 | 121.2 ± 12.0 | −5.1 (−10.36, −0.21) |
| Diastolic BP (mmHg) | 78.4 ± 7.8 | 77.8 ± 10.9 | −0.6 (−4.78, 3.52) |
| VO2max (mL/kg/min) | 26.8 ± 8.2 | 34.7 ± 5.3 | −7.9 (4.95, 10.84)** |
| Total cholesterol (mmol/L) | 4.8 ± 0.9 | 5.0 ± 1.1 | −0.2 (−0.17, 0.47) |
| LDL (mmol/L) | 2.6 ± 0.7 | 2.9 ± 0.8 | −0.2 (−0.01, 0.49) |
| HDL (mmol/L) | 1.6 ± 0.4 | 1.6 ± 0.4 | −0.0 (−0.09, 0.07) |
| Triglycerides (mmol/L) | 1.3 ± 0.5 | 1.1 ± 0.5 | −0.2 (−0.34, −0.02)** |
| Fasting glucose (mmol/L) | 4.8 ± 0.5 | 4.7 ± 0.5 | −0.1 (−0.38, 0.15) |
| Fasting insulin (pmol/L) | 49.9 ± 54.0 | 34.2 ± 19.9 | −15.7 (−37.50, 6.12) |
| McAuley’s ISI (M/mU/L) | 8.2 ± 2.2 | 9.1 ± 2.2 | −0.98 (−0.0009, 1.96)* |
Results are shown as mean ± SD with changes from baseline (Δ) presented with 95 % CI of the mean. n = 19 for all the cases except for VO2max, where n = 15 (for n = 4, baseline VO2max levels were below the measurable range) and blood lipids and McAuley’s ISI, where n = 17 (for n = 2, blood lipid levels were undetectable). *p < 0.05, **p < 0.01, paired t test was used for all the analysis other than fasting insulin, glucose, and blood lipids, where Wilcoxon’s paired analysis was used
No significant changes were identified in serum total cholesterol, LDL or HDL. However, median levels of serum triglycerides were significantly reduced post intervention, when compared to baseline (‘Wk 0, T0’) (p < 0.01). Additionally, there was a significant increase in insulin sensitivity, as measured by McAuley’s ISI, when compared to baseline (p < 0.05, see Table 1).
Markers of M1/M2 polarisation were significantly altered in monocytes following an 8-week moderate-intensity walking programme
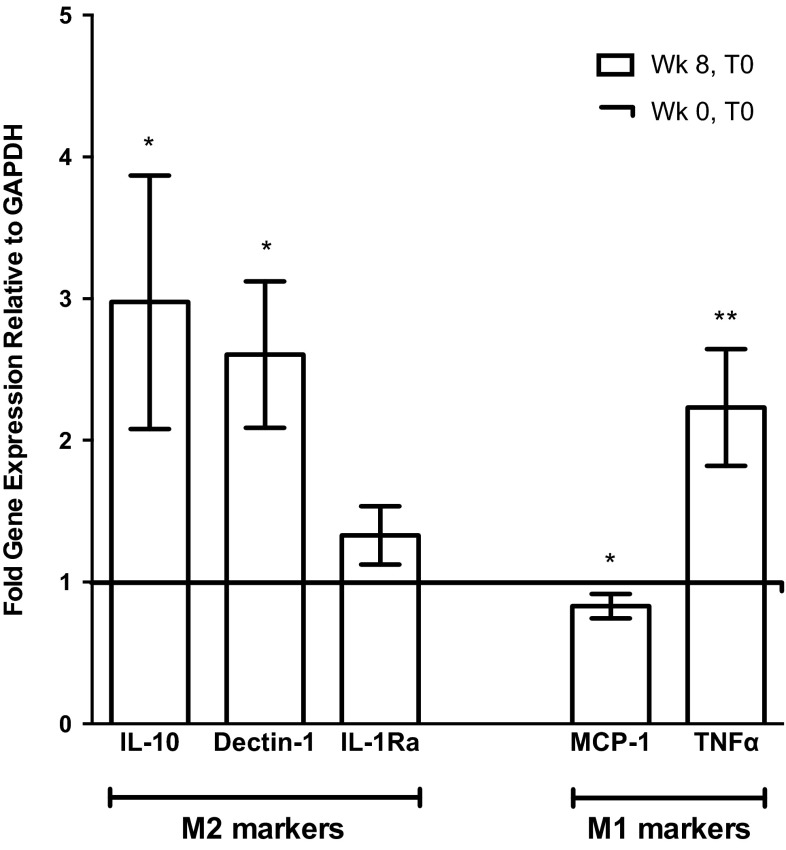
The M2 marker genes Dectin-1 and IL-10 were significantly upregulated by 2.6 ± 1.9-fold (p < 0.01) and 3.0 ± 2.8-fold, respectively (p < 0.05; Fig. 1). mRNA expression of IL-1Ra was also elevated by 1.3 ± 0.7-fold, showing a non-significant trend towards increased expression (p = 0.099). Conversely, the M1 marker, MCP-1, was significantly reduced to approximately 0.83 ± 0.2 (p < 0.05) of baseline (‘Wk 0, T0’) expression, following participation in the exercise intervention [in contrast, TNFα was significantly upregulated by 2.2 ± 1.4-fold (p < 0.01)].
Fig. 1.
Effect of an 8 week, moderate-intensity exercise intervention on gene expression of M2 markers and M1 markers in human monocytes. Isolated human monocytes were obtained at baseline (Wk 0, T0) and prior to the final exercise session (Wk 8, T0) of an 8 week, moderate-intensity walking programme. Where possible, the baseline values for each individual were used as comparators. In some cases, RNA quality or quantity was not sufficient for use in RT-PCR or some genes of interest were expressed at levels below the acceptable range of the assay and so were excluded from analysis (IL-10, n = 10; Dectin-1, n = 14; IL-1Ra, n = 14; MCP-1, n = 8; TNFα, n = 14; values expressed as fold gene expression relative to GAPDH ± SEM; *p < 0.05, **p < 0.01, t test)
PPARγ activity was increased in monocytes following an 8-week moderate-intensity walking programme, potentially due to acute exercise-induced increases in the PPARγ-activating properties of serum
The effects of exercise on PPARγ were investigated to provide a potential mechanism for the increase in M2 marker expression observed in monocytes in response to the exercise intervention. Although PPARγ mRNA expression did not alter significantly in monocytes following exercise training, when compared to baseline (‘Wk 0, T0’) (Fig. 2a), monocytic expression of the PPARγ-regulated downstream target genes, CD36 (1.9 ± 1.5-fold, p < 0.05), Liver X receptor α (LXRα; 5.0 ± 4.7-fold, p < 0.01), and ABCA1 (1.5 ± 1.9-fold, p > 0.05) was increased (Fig. 2a). In addition, the expression of cyclooxygenase-2 (COX-2), an enzyme associated with the generation of intracellular PPARγ ligands (Díaz-Gandarilla et al. 2013), was also significantly upregulated in monocyte samples obtained prior to the final exercise session, when compared to baseline (‘Wk 0, T0’) (3.6 ± 2.7-fold, p < 0.01; Fig. 2a).
Fig. 2.
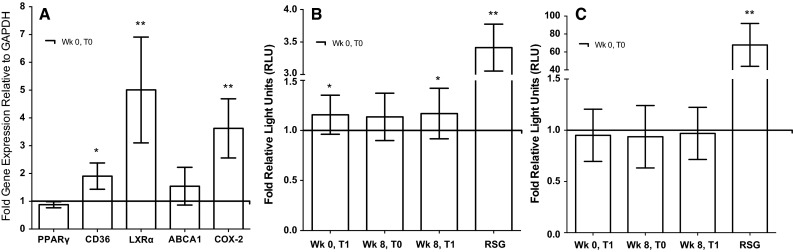
Effect of an 8 week, moderate-intensity exercise intervention on monocyte expression/activity of PPARγ and mechanisms for PPARγ activation. a Monocytes were obtained at baseline (Wk 0, T0) and immediately prior to the final exercise session (Wk 8, T0) of an 8 week, moderate-intensity walking programme and gene expression of PPARγ and PPARγ-associated genes, CD36, LXRα, ABCA1, and COX-2, was analysed. The baseline values for each individual were used as comparators. Gene reporter assays were used to analyse b the PPARγ activating properties of serum and c PPARγ ligand availably in serum obtained at baseline (Wk 0, T0), immediately following the initial exercise bout (Wk 0, T1), immediately prior to the final exercise bout (Wk 8, T0), and immediately following the final exercise bout (Wk 8, T1) of an 8 week, moderate-intensity exercise intervention. Rosiglitazone (RSG) was used as positive control luminescence values that were normalised to an internal control vector to obtain RLU values corresponding to PPARγ activity (RT-PCR: PPARγ, n = 10; LXRα and ABCA1, n = 9; CD36, n = 16; COX-2, n = 12; values expressed as fold gene expression relative to GAPDH ± SEM, *p < 0.05, **p < 0.01, t test. Gene reporter assays: n = 19 for serum, n = 3 for RSG; values expressed as fold RLU ± SD, *p < 0.05, **p < 0.01, one-way ANOVA)
To investigate potential mechanisms for exercise-induced PPARγ activation, gene reporter assays were used to analyse the PPARγ-activating properties of serum and PPARγ ligand generation in serum samples obtained throughout the exercise study. Figure 2b demonstrates that the PPARγ-activating properties of serum (as measured using PPRE-luciferase reporter assay) were significantly increased compared to baseline (‘Wk 0, T0’) immediately following individual exercise bouts (‘Wk 0, T1’: 1.16 ± 0.19-fold RLU; ‘Wk 8, T1’: 1.17 ± 0.25-fold RLU,-fold values relative to baseline (‘Wk 0, T0’), p < 0.05), while the PPARγ activating properties of serum underwent a non-significant increase over the duration of the entire exercise training programme [‘Wk 8, T0’: 1.14 ± 0.24-fold RLU, fold relative to baseline (‘Wk 0, T0’)]. Interestingly, however, neither acute exercise nor exercise training significantly altered ligand generation, as measured by the PPARγ-LBD gene reporter assay, [Fig. 2c; ‘Wk 0, T1’; 1.09 ± 0.26-fold RLU; ‘Wk 8. T0’: 0.94 ± 0.30-fold RLU; ‘Wk 8, T1’: 0.97 ± 0.26-fold RLU, fold values relative to baseline (‘Wk 0, T0’)].
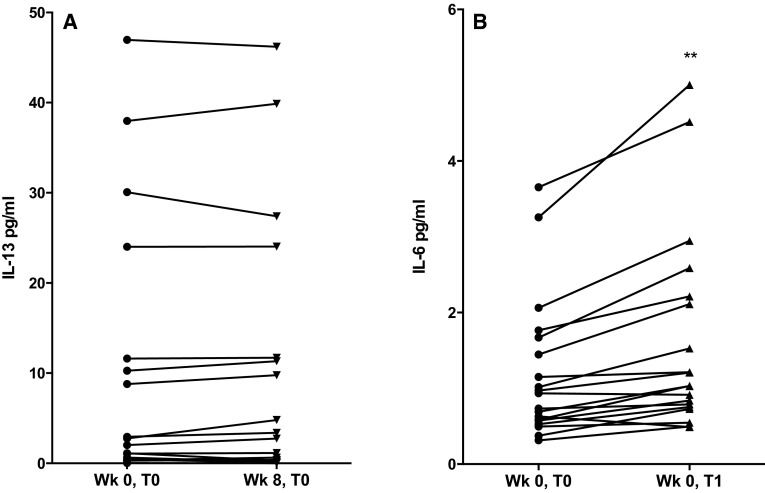
Elevations in IL-6 were observed after individual exercise bouts; however, alterations in IL-4 or IL-13 were not detected over the duration of an 8-week moderate-intensity walking programme
In the present study, levels of the M2-promoting stimulus, IL-4, were non-detectable in serum samples obtained either at baseline (‘Wk 0, T0’) or at the final exercise session (‘Wk 8, T0’) (minimum detection levels of the assay were 0.25 pg/mL; data not shown), whilst serum levels of another M2 stimuli, IL-13, did not alter significantly over the course of the exercise programme (‘Wk 0, T0’: 10.52 ± 3.43 pg/mL; Wk 8, T0: 11.20 ± 3.47 pg/mL; see Fig. 3a). Serum IL-6 concentrations increased significantly immediately after individual exercise bouts (‘Wk 0, T0’: 1.20 ± 0.21 pg/mL vs ‘Wk 0, T1’: 1.63 ± 1.32 pg/mL, p < 0.01, see Fig. 3b); however, baseline (‘Wk 0, T0’) levels of serum IL-6 were not altered over the duration of the 8 week exercise programme (results not shown).
Fig. 3.
Serum IL-13 and IL-6 concentration in response to an 8 week, moderate-intensity brisk walking intervention. a Serum IL-13 and b serum IL-6 were measured via ELISA. Serum IL-13 concentration was measured in samples taken at baseline (Wk 0, T0) and immediately prior to the final bout of an 8 week, moderate-intensity exercise intervention (Wk 8, T0), whereas serum IL-6 was measured in samples taken at baseline (Wk 0, T0) and following an acute bout of moderate-intensity exercise (Wk 0, T1) [IL-13, n = 17 (for n = 2, IL-13 levels were below the detection limit of the assay); IL-6, n = 19; results expressed as individual data points; significance related to mean values; **p < 0.01, paired t test]
Discussion
Previously, our group has demonstrated an increased M2 marker expression in human PMNCs following participation in an 8 week walking intervention (Yakeu et al. 2010). Since monocytes may be ‘primed’ for differentiation into specific M1 or M2 macrophage states (Bouhlel et al. 2007), it was deemed important to determine whether the previously observed effect of exercise on M2 marker expression occurs specifically within monocytes. This study demonstrates that participation in an 8 week, moderate-intensity brisk walking intervention upregulated markers of alternative activation in circulating monocytes and improved systemic insulin sensitivity, and provided evidence for a role for PPARγ as a putative mediator of these exercise-induced effects.
Specifically, the monocyte M2 markers, IL-10, Dectin-1, and IL-1Ra, were found to increase following the exercise intervention (see Fig. 1); mRNA expression of IL-10 and Dectin-1 was significantly elevated, whereas the increase in IL-1Ra expression approached significance. In contrast, the gene expression of the M1 marker, MCP-1, significantly decreased to ~0.8-fold of basal levels, which is in agreement with the previous findings (Kawanishi et al. 2010; Oliveira et al. 2013; Yakeu et al. 2010). However, the expression of the M1 marker, TNFα, was significantly elevated by ~twofold (Fig. 1). Interestingly, the profile of polarisation markers expressed by monocytes following exercise training in the current study is representative of a specific M2 macrophage subtype; the ‘M2b’ macrophage subset, which are said to produce M1-associated cytokines (including TNFα) but also high levels of IL-10, causing M2b cells to be immuno-regulatory (Hao et al. 2012; Kharraz et al. 2013; Mantovani et al. 2004). However, additional research would be required to substantiate the speculation that exercise training drives monocytes into an M2b phenotype. To our knowledge, this study is the first to demonstrate that exercise training increases markers of M2 polarisation specifically within monocytes, in a way which may drive them towards differentiation into the M2 macrophage phenotype, regarded as beneficial in the prevention of insulin resistance and T2D (67). However, at this stage, it should not be assumed that the significant improvement observed in insulin sensitivity (Δ0.98 M/mU/L compared to baseline, p < 0.05) in this study was solely a result of the changes in monocytic expression of M1/M2 markers in the present study (Table 1). Furthermore, it is well known that moderate exercise significantly lowers triglycerides, as was the case in this study, and this may also be an important contributing factor to the observed improvement in insulin sensitivity (Kraus and Slentz 2009).
We have previously shown that both acute and chronic exercise may induce the activation of PPARγ, a transcription factor thought to play an important role in priming monocytes for M2 polarisation (Bouhlel et al. 2007; Butcher et al. 2008; Thomas et al. 2012; Yakeu et al. 2010). However, this has only been demonstrated in mixed mononuclear cells (Butcher et al. 2008; Thomas et al. 2012; Yakeu et al. 2010), and has not yet been investigated within isolated monocytes. The findings from the current study suggest that PPARγ activity was elevated in monocytes in response to exercise training: PPARγ downstream genes, namely, CD36, LXRα and COX-2, were significantly upregulated after the 8 week intervention when compared to baseline, while ABCA1 underwent a non-significant increase (see Fig. 2a). CD36 is also associated with the M2 macrophage phenotype (Bouhlel et al. 2007; Oh et al. 2012) and so its upregulation may be used to further support the impact of exercise on monocyte activation.
To further investigate the mechanism(s) by which exercise may have enhanced monocyte PPARγ activity, both serum PPARγ activating properties and serum PPARγ ligand availability were determined using gene reporter assays. The PPARγ-activating properties of serum were shown to increase acutely upon exercise (Fig. 2b), despite no changes in PPARγ expression (Fig. 2a) or serum PPARγ ligand availability in response to acute or chronic physical activity (Fig. 2c). These results are in accordance with those we obtained previously and provide further evidence that exercise promotes PPARγ activation (Thomas et al. 2012). While the serum ligand availability assays demonstrate that this effect is independent of exogenous ligand production, our data suggest that exercise may instead trigger endogenous PPARγ ligand generation, as exercise-associated elevations in monocyte COX-2 expression (Fig. 2a) may contribute to increased PPARγ activity within monocytes, since COX-2 encodes an inducible enzyme which is responsible for the production of endogenous PPARγ ligands (e.g., 15d-PGJ2) (Díaz-Gandarilla et al. 2013; Heusinkveld et al. 2011; Sica and Mantovani 2012). In addition, exercise participation may trigger ligand-independent post-translational modifications of PPARγ, such as phosphorylation or sumoylation, resulting in PPARγ activation (Harmon et al. 2011; Olefsky and Glass 2010). However, it is a limitation of the current study that the specific PPARγ activating factor(s) responsible for this effect was not identified. In addition, the model system used in these experiments (HEK293-T cells) may not express the relevant ligand uptake/processing machinery, and thus, the in vivo situation may not be accurately reflected by these results. Future work would benefit from using cells which more closely resemble human monocytes.
It is also possible that exercise-induced alterations in systemic cytokine levels may impact upon PPARγ activity and M1/M2 marker expression in monocytes. Despite no observed change in serum levels of the established M2-stimuli IL-4 (data not shown) and IL-13 (Fig. 3a) (Mantovani et al. 2004) following exercise training, IL-6 was found to be significantly elevated in serum immediately following participation in exercise bouts (Fig. 3b). IL-6 is known to be synthesised by contracting muscle during acute exercise (Pan et al. 2012; Dishman et al. 2013); accordingly serum levels of IL-6 are transiently elevated upon exercise participation (Pedersen and Febbraio 2008), rapidly returning to baseline within 1–2 h of exercise cessation (Gleeson et al. 2011; Moldoveanu et al. 2000). Recently, an interesting role for IL-6 in the alternative activation of monocytes has been revealed: Mauer et al. demonstrated that IL-6 is required for IL-4-dependent M2 macrophage polarisation, and that the depletion of the IL-6Rα chain of the IL-6 receptor in myeloid cells induced insulin resistance and impaired glucose homeostasis (Mauer et al. 2014). Moreover, IL-6 was shown to upregulate IL-4 receptor (IL-4Rα) expression in macrophages, making these cells more sensitive to IL-4 stimulation. In addition, Szanto et al. (2010) demonstrated that IL-4/STAT-6 signalling resulted in augmented PPARγ activation in macrophages independent of changes in ligand availability. Thus, it may be speculated that in the present study, exercise IL-6-induced upregulation of IL-4Rα and subsequent increased sensitivity to IL-4 may contribute to the observed exercise-associated monocyte PPARγ activation (Fig. 2c), independent of changes in PPARγ ligand availability.
We acknowledge that a major limitation of this research is its reliance on the assumption that the M2 monocyte phenotype is retained upon extravasation and differentiation into tissue macrophages, whereas the possibility of intra-tissue ‘switching’ of macrophage phenotype has been previously reported (Dalmas et al. 2011; Lee et al. 2013). Thus, further investigations are required to elucidate the effects of similar exercise interventions on M1:M2 ratio in various tissue environments. Nevertheless, it should be noted that, if a link can be made between the classification of monocytes and that of macrophages, the current research may facilitate the use of monocytes (which are easily accessible cells) as biomarkers for macrophage-associated diseases, such as T2D.
Importantly, regardless of the specific PPARγ-activating process/es, exercise-associated increases in PPARγ-activating properties of serum may contribute to the systemic beneficial effects of the current exercise programme with regard to insulin sensitivity (Table 1). We propose that, in a similar way to PPARγ-targeting anti-diabetic agents, exercise participation may increase levels of blood-borne PPARγ-activating factors, allowing for sustained systemic PPARγ activation in a range of cells and tissues, and this may, together with many other contributing factors, impact upon glucose metabolism, lipid homeostasis, and inflammation within these tissues (Harmon et al. 2011; Wahli and Michalik 2012). In addition, we would contend that these findings further support the use of exercise prescription as an alternative to currently available pharmacological therapies with regard to the management and treatment of T2D and its cardiovascular complications.
Conclusions
In conclusion, participation in an 8 week, moderate-intensity exercise programme induces M2 marker expression and PPARγ activation in monocytes (potentially priming them for differentiation into M2-polarised tissue macrophage) and exerts beneficial systemic effects with regard to insulin resistance. In addition to the observed beneficial alterations in key predictors of cardio-metabolic risk, including body weight, BMI, waist circumference, triglycerides, aerobic capacity, and insulin sensitivity, the current study provides further evidence that the prescription of a moderate-intensity walking programme may be beneficial to the prevention of T2D and its cardiovascular complications in at risk populations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
The technical support of Laura Watkeys, Gareth Walters, Paul Jones and Steve Potter is greatly appreciated. In addition, the biochemical analysis carried out by Dr Stephen Luzio and Gareth Dunseath at Diabetic Research Network Cymru (Swansea University, UK) is gratefully acknowledged. JSR and NAD were recipients of the Welsh Government through Health and Care Research Wales studentships. Gratitude is also extended to Dr M. van Bilsen (Maastricht University, Belgium) for the kind donation of PPARγ and PPRE-Luciferase vectors, Professor V. K. Chatterjee (University of Cambridge, UK), for the UAS construct and Dr J. S. Flier (Harvard Medical School, USA) for the PPARγ-LBD/GAL4-DBD construct used within this research.
Abbreviations
- ABCA1
ATP-binding cassette transporter
- COX2
Cyclooxygenase 2
- CD36
Cluster of differentiation 36
- GAPDH
Glyceraldehyde 3-phosphate dehydrogenase
- IL
Interleukin
- ISI
Insulin sensitivity index
- LXRα
Liver x receptor alpha
- MCP-1
Macrophage chemotactic protein-1
- PPARγ
Peroxisome proliferator activated receptor gamma
- RLU
Relative light units
- TNFα
Tumour necrosis factor alpha
- T2D
Type 2 diabetes
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Arkan MC, Hevener AL, Greten FR, Maeda S, Li ZW, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M. IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med. 2005;11(2):191–198. doi: 10.1038/nm1185. [DOI] [PubMed] [Google Scholar]
- Ascaso JF, Pardo S, Real JT, Lorente RI, Priego A, Carmena R. Diagnosing insulin resistance by simple quantitative methods in subjects with normal glucose metabolism. Diabetes Care. 2003;26(12):3320–3325. doi: 10.2337/diacare.26.12.3320. [DOI] [PubMed] [Google Scholar]
- Bagchi D, Preuss HG. Obesity: epidemiology, pathophysiology, and prevention. 2. London: CRC Press; 2012. [Google Scholar]
- Bouhlel MA, Derudas B, Rigamonti E, Dievart R, Brozek J, Haulon S, Zawadzki C, Jude B, Torpier G, Marx N, Staels B, Chinetti-Gbaguidi G. PPARgamma activation primes human monocytes into alternative M2 macrophages with anti-inflammatory properties. Cell Metab. 2007;6(2):137–143. doi: 10.1016/j.cmet.2007.06.010. [DOI] [PubMed] [Google Scholar]
- Bruun JM, Helge JW, Richelsen B, Stallknecht B. Diet and exercise reduce low-grade inflammation and macrophage infiltration in adipose tissue but not in skeletal muscle in severely obese subjects. Am J Physiol Endocrinol Metab. 2006;290(5):E961–E967. doi: 10.1152/ajpendo.00506.2005. [DOI] [PubMed] [Google Scholar]
- Butcher LR, Thomas A, Backx K, Roberts A, Webb R, Morris K. Low-intensity exercise exerts beneficial effects on plasma lipids via PPARgamma. Med Sci Sports Exerc. 2008;40(7):1263–1270. doi: 10.1249/MSS.0b013e31816c091d. [DOI] [PubMed] [Google Scholar]
- Chinetti-Gbaguidi G, Staels B. Macrophage polarization in metabolic disorders: functions and regulation. Curr Opin Lipidol. 2011;22(5):365–372. doi: 10.1097/MOL.0b013e32834a77b4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B, American College of Sports Medicine. American Diabetes Association Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–e167. doi: 10.2337/dc10-9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collingwood TN, Butler A, Tone Y, Clifton-Bligh RJ, Parker MG, Chatterjee VK. Thyroid hormone-mediated enhancement of heterodimer formation between thyroid hormone receptor beta and retinoid X receptor. J Biol Chem. 1997;272(20):13060–13065. doi: 10.1074/jbc.272.20.13060. [DOI] [PubMed] [Google Scholar]
- Dalmas E, Clement K, Guerre-Millo M. Defining macrophage phenotype and function in adipose tissue. Trends Immunol. 2011;32(7):307–314. doi: 10.1016/j.it.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Defronzo RA, Tripathy D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S157–S163. doi: 10.2337/dc09-S302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diabetes Prevention Program Research Group The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Díaz-Gandarilla JA, Osorio-Trujillo C, Hernandez-Ramirez VI, Talamas-Rohana P. PPAR activation induces M1 macrophage polarization via cPLA(2)-COX-2 inhibition, activating ROS production against Leishmania mexicana. BioMed Res Int. 2013;2013:215283. doi: 10.1155/2013/215283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishman RK, Heath G, Lee IM. Physical activity epidemiology. 2. Leeds: Human Kinetics; 2013. [Google Scholar]
- Eriksson J, Lindström J, Valle T, Aunola S, Hämäläinen H, Ilanne-Parikka P, Keinänen-Kiukaanniemi S, Laakso M, Lauhkonen M, Lehto P, Lehtonen A, Louheranta A, Mannelin M, Martikkala V, Rastas M, Sundvall J, Turpeinen A, Viljanen T, Uusitupa M, Tuomilehto J. Prevention of Type II diabetes in subjects with impaired glucose tolerance: the Diabetes Prevention Study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia. 1999;42(7):793–801. doi: 10.1007/s001250051229. [DOI] [PubMed] [Google Scholar]
- Febbraio MA, Pedersen BK. Muscle-derived interleukin-6: mechanisms for activation and possible biological roles. FASEB J. 2002;16(11):1335–1347. doi: 10.1096/fj.01-0876rev. [DOI] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327(5966):656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginhoux F, Jung S. Monocytes and macrophages: developmental pathways and tissue homeostasis. Nat Rev Immunol. 2014;14(6):392–404. doi: 10.1038/nri3671. [DOI] [PubMed] [Google Scholar]
- Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–615. doi: 10.1038/nri3041. [DOI] [PubMed] [Google Scholar]
- Golbidi S, Badran M, Laher I (2012) Antioxidant and anti-inflammatory effects of exercise in diabetic patients. Exp Diabetes Res (Article ID 941868) [DOI] [PMC free article] [PubMed]
- Goldfine AB, Conlin PR, Halperin F, Koska J, Permana P, Schwenke D, Shoelson SE, Reaven PD. A randomised trial of salsalate for insulin resistance and cardiovascular risk factors in persons with abnormal glucose tolerance. Diabetologia. 2013;56(4):714–723. doi: 10.1007/s00125-012-2819-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haldar M, Murphy KM. Origin, development, and homeostasis of tissue-resident macrophages. Immunol Rev. 2014;262(1):25–35. doi: 10.1111/imr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han MS, Jung DY, Morel C, Lakhani SA, Kim JK, Flavell RA, Davis RJ. JNK expression by macrophages promotes obesity-induced insulin resistance and inflammation. Science. 2013;339(6116):218–222. doi: 10.1126/science.1227568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao NB, Lu MH, Fan YH, Cao YL, Zhang ZR, Yang SM. Macrophages in tumor microenvironments and the progression of tumors. Clin Dev Immunol. 2012;2012:948098. doi: 10.1155/2012/948098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harford KA, Reynolds CM, McGillicuddy FC, Roche HM. Fats, inflammation and insulin resistance: insights to the role of macrophage and T-cell accumulation in adipose tissue. Proc Nutr Soc. 2011;70(4):408–417. doi: 10.1017/S0029665111000565. [DOI] [PubMed] [Google Scholar]
- Harmon GS, Lam MT, Glass CK. PPARs and lipid ligands in inflammation and metabolism. Chem Rev. 2011;111(10):6321–6340. doi: 10.1021/cr2001355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heusinkveld M, de Vos van Steenwijk PJ, Goedemans R, Ramwadhdoebe TH, Gorter A, Welters MJ, van Hall T, van der Burg SH. M2 macrophages induced by prostaglandin E2 and IL-6 from cervical carcinoma are switched to activated M1 macrophages by CD4 + Th1 cells. J Immunol. 2011;187(3):1157–1165. doi: 10.4049/jimmunol.1100889. [DOI] [PubMed] [Google Scholar]
- Hevener AL, Olefsky JM, Reichart D, Nguyen MT, Bandyopadyhay G, Leung HY, Watt MJ, Benner C, Febbraio MA, Nguyen AK, Folian B, Subramaniam S, Gonzalez FJ, Glass CK, Ricote M. Macrophage PPAR gamma is required for normal skeletal muscle and hepatic insulin sensitivity and full antidiabetic effects of thiazolidinediones. J Clin Invest. 2007;117(6):1658–1669. doi: 10.1172/JCI31561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang W, Metlakunta A, Dedousis N, Zhang P, Sipula I, Dube JJ, Scott DK, O’Doherty RM. Depletion of liver Kupffer cells prevents the development of diet-induced hepatic steatosis and insulin resistance. Diabetes. 2010;59(2):347–357. doi: 10.2337/db09-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda S, Tamura Y, Kakehi S, Takeno K, Kawaguchi M, Watanabe T, Sato F, Ogihara T, Kanazawa A, Fujitani Y, Kawamori R, Watada H. Exercise-induced enhancement of insulin sensitivity is associated with accumulation of M2-polarized macrophages in mouse skeletal muscle. Biochem Biophys Res Commun. 2013;441(1):36–41. doi: 10.1016/j.bbrc.2013.10.005. [DOI] [PubMed] [Google Scholar]
- Kawanishi N, Yano H, Yokogawa Y, Suzuki K. Exercise training inhibits inflammation in adipose tissue via both suppression of macrophage infiltration and acceleration of phenotypic switching from M1 to M2 macrophages in high-fat-diet-induced obese mice. Exerc Immunol Rev. 2010;16:105–118. [PubMed] [Google Scholar]
- Kharraz Y, Guerra J, Mann CJ, Serrano AL, Munoz-Canoves P (2013) Macrophage plasticity and the role of inflammation in skeletal muscle repair. Mediat Inflamm (Article ID 491497) [DOI] [PMC free article] [PubMed]
- Kline GM, Porcari JP, Hintermeister R, Freedson PS, Ward A, McCarron RF, Ross J, Rippe JM. Estimation of VO2max from a one-mile track walk, gender, age, and body weight. Med Sci Sports Exerc. 1987;19(3):253–259. doi: 10.1249/00005768-198706000-00012. [DOI] [PubMed] [Google Scholar]
- Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM, Group DPPR Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus WE, Slentz CA. Exercise training, lipid regulation, and insulin action: a tangled web of cause and effect. Obesity. 2009;17(Suppl 3):S21–S26. doi: 10.1038/oby.2009.384. [DOI] [PubMed] [Google Scholar]
- Kristiansen OP, Mandrup-Poulsen T. Interleukin-6 and diabetes: the good, the bad, or the indifferent? Diabetes. 2005;54(Suppl 2):S114–S124. doi: 10.2337/diabetes.54.suppl_2.S114. [DOI] [PubMed] [Google Scholar]
- Lee HW, Choi HJ, Ha SJ, Lee KT, Kwon YG. Recruitment of monocytes/macrophages in different tumor microenvironments. Biochim Biophys Acta. 2013;1835(2):170–179. doi: 10.1016/j.bbcan.2012.12.007. [DOI] [PubMed] [Google Scholar]
- Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117(1):175–184. doi: 10.1172/JCI29881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25(12):677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- Mauer J, Chaurasia B, Goldau J, Vogt MC, Ruud J, Nguyen KD, Theurich S, Hausen AC, Schmitz J, Bronneke HS, Estevez E, Allen TL, Mesaros A, Partridge L, Febbraio MA, Chawla A, Wunderlich FT, Bruning JC. Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol. 2014;15(5):423–430. doi: 10.1038/ni.2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, Duncan AW. Diagnosing insulin resistance in the general population. Diabetes Care. 2001;24(3):460–464. doi: 10.2337/diacare.24.3.460. [DOI] [PubMed] [Google Scholar]
- Moldoveanu AI, Shephard RJ, Shek PN. Exercise elevates plasma levels but not gene expression of IL-1beta, IL-6, and TNF-alpha in blood mononuclear cells. J Appl Physiol. 2000;89(4):1499–1504. doi: 10.1152/jappl.2000.89.4.1499. [DOI] [PubMed] [Google Scholar]
- Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8(12):958–969. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odegaard JI, Ricardo-Gonzalez RR, Goforth MH, Morel CR, Subramanian V, Mukundan L, Red Eagle A, Vats D, Brombacher F, Ferrante AW, Chawla A. Macrophage-specific PPARgamma controls alternative activation and improves insulin resistance. Nature. 2007;447(7148):1116–1120. doi: 10.1038/nature05894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh J, Riek AE, Weng S, Petty M, Kim D, Colonna M, Cella M, Bernal-Mizrachi C. Endoplasmic reticulum stress controls M2 macrophage differentiation and foam cell formation. J Biol Chem. 2012;287(15):11629–11641. doi: 10.1074/jbc.M111.338673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol. 2010;72:219–246. doi: 10.1146/annurev-physiol-021909-135846. [DOI] [PubMed] [Google Scholar]
- Oliveira AG, Araujo TG, Carvalho BM, Guadagnini D, Rocha GZ, Bagarolli RA, Carvalheira JB, Saad MJ. Acute exercise induces a phenotypic switch in adipose tissue macrophage polarization in diet-induced obese rats. Obesity (Silver Spring) 2013;21(12):2545–2556. doi: 10.1002/oby.20402. [DOI] [PubMed] [Google Scholar]
- Osborn O, Olefsky JM. The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med. 2012;18(3):363–374. doi: 10.1038/nm.2627. [DOI] [PubMed] [Google Scholar]
- Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance: the Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20(4):537–544. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- Pan H, Xu X, Hao X, Chen Y. Changes of myogenic reactive oxygen species and interleukin-6 in contracting skeletal muscle cells. Oxid Med Cell Longev. 2012;2012:145418. doi: 10.1155/2012/145418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen BK, Febbraio MA. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev. 2008;88(4):1379–1406. doi: 10.1152/physrev.90100.2007. [DOI] [PubMed] [Google Scholar]
- Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98(4):1154–1162. doi: 10.1152/japplphysiol.00164.2004. [DOI] [PubMed] [Google Scholar]
- Petersen KF, Dufour S, Savage DB, Bilz S, Solomon G, Yonemitsu S, Cline GW, Befroy D, Zemany L, Kahn BB, Papademetris X, Rothman DL, Shulman GI. The role of skeletal muscle insulin resistance in the pathogenesis of the metabolic syndrome. Proc Natl Acad Sci USA. 2007;104(31):12587–12594. doi: 10.1073/pnas.0705408104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan Nabzdyk L, Kuchibhotla S, Guthrie P, Chun M, Auster ME, Nabzdyk C, Deso S, Andersen N, Gnardellis C, LoGerfo FW, Veves A. Expression of neuropeptides and cytokines in a rabbit model of diabetic neuroischemic wound healing. J Vasc Surg. 2013;58(3):766–775. doi: 10.1016/j.jvs.2012.11.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romeo GR, Lee J, Shoelson SE. Metabolic syndrome, insulin resistance, and roles of inflammation—mechanisms and therapeutic targets. Arterioscler Thromb Vasc Biol. 2012;32(8):1771–1776. doi: 10.1161/ATVBAHA.111.241869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel VT, Shulman GI. Mechanisms for insulin resistance: common threads and missing links. Cell. 2012;148(5):852–871. doi: 10.1016/j.cell.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta. 2011;1813(5):878–888. doi: 10.1016/j.bbamcr.2011.01.034. [DOI] [PubMed] [Google Scholar]
- Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest. 2012;122(3):787–795. doi: 10.1172/JCI59643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szanto A, Balint BL, Nagy ZS, Barta E, Dezso B, Pap A, Szeles L, Poliska S, Oros M, Evans RM, Barak Y, Schwabe J, Nagy L. STAT6 transcription factor is a facilitator of the nuclear receptor PPARgamma-regulated gene expression in macrophages and dendritic cells. Immunity. 2010;33(5):699–712. doi: 10.1016/j.immuni.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas AW, Davies NA, Moir H, Watkeys L, Ruffino JS, Isa SA, Butcher LR, Hughes MG, Morris K, Webb R. Exercise-associated generation of PPARgamma ligands activates PPARgamma signaling events and upregulates genes related to lipid metabolism. J Appl Physiol. 2012;112(5):806–815. doi: 10.1152/japplphysiol.00864.2011. [DOI] [PubMed] [Google Scholar]
- Tzameli I, Fang H, Ollero M, Shi H, Hamm JK, Kievit P, Hollenberg AN, Flier JS. Regulated production of a peroxisome proliferator-activated receptor-gamma ligand during an early phase of adipocyte differentiation in 3T3-L1 adipocytes. J Biol Chem. 2004;279(34):36093–36102. doi: 10.1074/jbc.M405346200. [DOI] [PubMed] [Google Scholar]
- Wahli W, Michalik L. PPARs at the crossroads of lipid signaling and inflammation. Trends Endocrinol Metab. 2012;23(7):351–363. doi: 10.1016/j.tem.2012.05.001. [DOI] [PubMed] [Google Scholar]
- Yakeu G, Butcher L, Isa S, Webb R, Roberts AW, Thomas AW, Backx K, James PE, Morris K. Low-intensity exercise enhances expression of markers of alternative activation in circulating leukocytes: roles of PPARgamma and Th2 cytokines. Atherosclerosis. 2010;212(2):668–673. doi: 10.1016/j.atherosclerosis.2010.07.002. [DOI] [PubMed] [Google Scholar]
- You H, Gao T, Cooper TK, Brian Reeves W, Awad AS. Macrophages directly mediate diabetic renal injury. Am J Physiol Renal Physiol. 2013;305(12):1719–1727. doi: 10.1152/ajprenal.00141.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.