Abstract
Objectives
This study presents a variant of the Brazilian disk test (BDT) for assessing the bond strength between composite resins and dentin.
Methods
Dentin-composite disks (φ 5 mm × 2 mm) were prepared using either Z100 or Z250 (3M ESPE) in combination with one of three adhesives, Adper Easy Bond (EB), Adper Scotchbond Multi-Purpose (MP) and Adper Single Bond (SB), and tested under diametral compression. Acoustic emission (AE) and digital image correlation (DIC) were used to monitor debonding of the composite from the dentin ring. A finite element (FE) model was created to calculate the bond strengths using the failure loads. Fracture modes were examined by scanning electron microscopy (SEM).
Results
Most specimens fractured along the dentin-resin composite interface. DIC and AE confirmed interfacial debonding immediately before fracture of the dentin ring. Results showed that the mean bond strength with EB (14.9±1.9 MPa) was significantly higher than with MP (13.2±2.4 MPa) or SB (12.9±3.0 MPa) (p<0.05); no significant difference was found between MP and SB (p>0.05). Z100 (14.5±2.3 MPa) showed higher bond strength than Z250 (12.7±2.5 MPa) (p<0.05). Majority of specimens (91.3%) showed an adhesive failure mode. EB failed mostly at the dentin-adhesive interface, whereas MP at the composite-adhesive interface; specimens with SB failed at the composite-adhesive interface and cohesively in the adhesive.
Conclusions
The BDT variant showed to be a suitable alternative for measuring the bond strength between dentin and composite, with zero premature failure, reduced variability in the measurements, and consistent failure at the dentin-composite interface.
Keywords: Adhesive, Dentin, Resin composite, Bond strength, Brazilian disk
INTRODUCTION
An often cited reason for the failure of composite restorations is the breakdown of the tooth-composite interface (1), whereas mechanical forces resulting from composite polymerization shrinkage or mastication are the main reasons for this breakdown (2, 3). The marginal gaps thus formed around the restoration would allow bacterial invasion and biofilm accumulation, leading to secondary caries (4).
Bond strength testing is therefore routinely used to assess the interfacial strength between the tooth and restoration. Different bond strength tests have been developed over the years, with the shear (SBS) and tensile bond strength (TBS) tests being the most popular. However, there are certain drawbacks associated with these tests (5-7). For example, difficulties with machining, handling, aligning and fixing the matchstick specimens are some of the problems encountered in the TBS test (5, 6). Also, when the bond strength is comparable or higher than the fracture strength of the substrates, a high percentage of cohesive fracture in the substrates may result with the TBS test (8).
Similarly, in the SBS test, cohesive failure often occurs within the dental or composite substrate (6, 9, 10). Obviously, for a bond strength test to be valid, failure must initiate from the interface (11). In addition to the above problems, analyses have shown that the stress distribution at the tooth-restoration interface of some of the specimens is highly non-uniform and greatly depends on the material property mismatch, specimen geometry and attachment conditions (12-15). In the SBS test specimen, for example, the dominant stress state is that of tension rather than shear (7, 13, 16).
As an alternative bond strength test, we recently proposed a variant of the Brazilian disk test (BDT), or disk in diametral compression, to assess the interfacial debonding of endodontic posts from root dentin (17). The BDT has been used widely for testing the tensile strength and fracture toughness of brittle materials. It has also been used to test the interfacial fracture toughness of various dissimilar materials (18, 19). During the test, tensile stresses are introduced in the horizontal direction, i.e. transverse to the applied vertical compressive load. The force required to cause failure is used to estimate the tensile strength (20). In the previous work (17), the disk specimen consisted of a slice of root dentin with a section of a circular post cemented in the enlarged concentric root canal. The dentin itself was surrounded by a layer of resin composite to form a disk of 10-mm diameter and 2-mm thick. Using the acoustic emission (AE) and digital image correlation (DIC) techniques, we confirmed that fracture of the disk under diametral compression was initiated by debonding at the post-dentin interface. Compared with some of the other bond tests for endodontic posts, the modified Brazilian disk test had the advantages of simpler specimen preparation and reduced variations in the results. In this paper, we introduce another modification of the BDT specimen that is more suitable for assessing the bond strength of direct composite restorations. Our goal is to determine whether the new test specimen would retain the advantages seen in its previous form for endodontic post testing. Again, DIC and AE were used to validate the test.
METHODS
Sample preparation
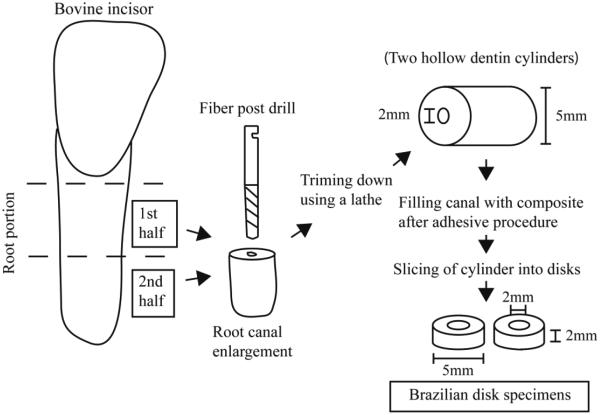
The root portions from approximately 30 bovine incisors were removed and cut into two halves with a diamond saw under water cooling. The cut was made perpendicularly to the long root axis, with each half having an approximate length of 6-7 mm. From these, the halves that had a root canal larger than the intended diameter were rejected. Next, the canal of each selected root segment was enlarged with a 1.9-mm diameter fiber post drill using water as coolant (3M ESPE, Dental products, St. Paul, MN, USA) to obtain a circular hole of ~2-mm diameter. Afterwards, the root segments were trimmed down using a lathe to remove the cementum and the external layer of dentin to produce hollow dentin cylinders of 5±0.05-mm -mm outer diameter and 2.05±0.05-mm inner diameter (Fig. 1).
Figure 1.
Schematic representation of the technical steps to obtain the modified Brazilian disk.
The machined dentin cylinders were randomly assigned to three bonding systems: Total-etch Adper™ Single Bond Plus (SB), Self-etch Adper™ Easy Bond Adhesive (EB) and total-etch Adper™ Scotchbond™ Multi-Purpose Adhesive (MP); see Table 1. Each bonding system was applied to the inner surface of the hollow dentin cylinders with a disposable brush applicator provided by the manufacturer and subsequently cured according to the manufacturer’s instructions. After this, the canal of each cylinder was restored with either Filtek™ Z250 Universal Restorative or Z100™ Restorative; see also Table 1. The composites were applied incrementally to minimize shrinkage stress, with each layer being less than 2-mm thick. The first increment was placed in the middle section of the cylinder with the aid of a composite condenser and the subsequent increments placed at its ends. The first increment was cured from both ends for 20 s each. The end increments were cured from the respective ends of the cylinder for 40s. Light curing was done with an Elipar Trilight (3M ESPE, Dental Products, St. Paul, MN, USA) curing light operated at 800 mW/cm2.
Table 1.
Compositions of composites and bonding systems used in this study.
| Product | Composition | Batch number |
|---|---|---|
|
Z100™
Restorative |
Silane treated ceramic, triethylene glycol dimethacrylate (TEGDMA), bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-benzotriazolyl-4-methylphenol*. |
N362970 |
|
Filtek™ Z250
Universal Restorative |
Silane treated ceramic, bisphenol a polyethylene glycol diether dimethacrylate (BISEMA6), diurethane dimethacrylate (UDMA), bisphenol a diglycidyl ether dimethacrylate (BISGMA), triethylene glycol dimethacrylate (TEGMA), benzotriazol, ethyl 4-dimethyl aminobenzoate (EDMAB)*. |
N326080 |
|
Adper Single
Bond Plus |
Ethyl alcohol, silane treated silica (nanofiller), bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-hydroxyethyl methacrylate(HEMA), glycerol 1,3-dimethacrylate, copolymer of acrylic and itaconic acids, water, diurethane dimethacrylate (UDMA) diphenyliodonium hexafluorophosphate, ethyl 4- dimethyl aminobenzoate (EDMAB) *. |
N509492 |
|
Adper™ Easy
Bond Self- Etch Adhesive |
Bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2- hydroxyethyl methacrylate, ethanol, water, phosphoric acid-6- methacryloxy-hexylesters, silane treated silica, 1,6-hexanediol dimethacrylate, copolymer of acrylic and itaconic acid, (dimethylamino)ethyl methacrylate camphorquinone, 2,4,6- trimethylbenzoyldiphenylphosphine oxide*. |
N497589 |
|
Adper™
Scotchbond™ |
Primer: Water, 2-hydroxyethyl methacrylate (HEMA), copolymer of acrylic and itaconic acids |
N491015 |
|
Multi-
Purpose Adhesive |
Bond: Bisphenol a diglycidyl ether dimethacrylate (BISGMA), 2-hydroxyethyl methacrylate (hema), triphenylantimony*. |
N494505 |
Obtained from manufacturer’s data sheets (3M ESPE).
The filled dentin cylinders were cut using an Isomet™ (Buehler, Lake Bluff, IL, USA) diamond saw into 2-mm thick dentin-resin composite disks under cooling water; see Fig 1 and inset in Fig. 2. Two or three disk specimens could be obtained from each root segment. The disks were examined for defects under a microscope (Olympus MVX10, Olympus America Inc.) with a magnification of 3.2× Defective samples with pores on the surface, air bubbles that could be clearly seen in the composite, irregularities or cracks were removed from the study. A total of 15 to 17 disks were used for each group and they were stored in 0.1% thymol solution at 4°C overnight before testing.
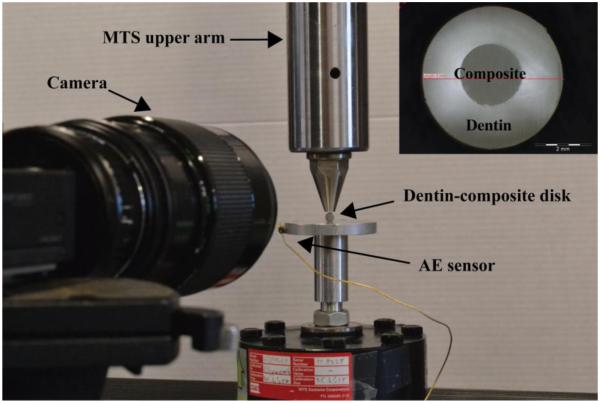
Figure 2.
Experimental setup for diametral compression, digital image correlation and acoustic emission measurement. Inset: Modified Brazilian disk for measuring interfacial bond strength between root dentin and direct composite restoration.
Diametral compression
The diametral compression test was carried out using a Universal Test Machine (858 Mini Bionix, MTS, USA), with the specimen located between two flat and parallel steel components (Fig. 2). A loading rate of 0.5 mm/min was applied to fracture the samples. The load and displacement time histories were recorded during the loading process.
Acoustic Emission (AE) measurement
An AE system (Physical Acoustics Corporation, NJ, USA) was used to monitor microcracking of the specimens during loading. The AE sensor was attached to the lower support plate (Fig. 2). Signals detected by the sensor were passed through a preamplifier of 10-dB gain with a band pass of 100 kHz-2MHz and a threshold set at 35 dB. The AE results were used together with the load time histories and DIC data (see below) to identify the point at which interfacial debonding first occurred.
Digital Image Correlation (DIC)
Surface deformation of the disks was measured by using DIC to identify interfacial debonding. This technique utilized a non-contact optical method for tracking movements of surface features. The system consisted of a high-speed CCD camera (Point Grey Grasshopper GRAS-20S4C-C) and propriety software (DaVis 7.2, LaVision-GmbH, Goettingen, Germany) for displacement and strain calculation (Fig. 2b). To allow deformations to be determined, the disk surface facing the CCD camera was first sprayed with a white fixation paint (Krylon products group, Cleveland, OH, USA) followed by a thin layer of charcoal particles (Sigma Aldrich, St. Louis, MO, USA). These created irregular speckles on the surface for local displacement tracking. A reference image was taken before the specimen was loaded. During loading, further images were taken at 10-20 frames per second (fps) for comparison with the reference image. The proprietary software was then used to calculate the full-field strain maps, and interfacial debonding could be identified from the strain concentration developed.
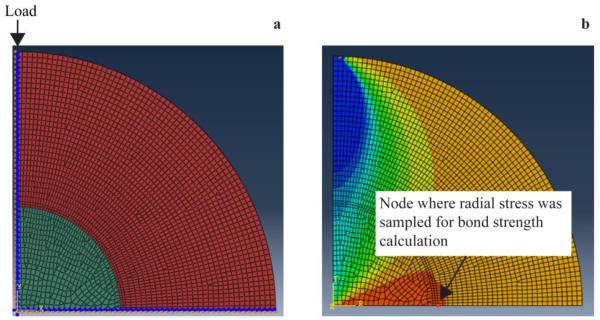
Finite Element (FE) simulation
There is no simple analytical solution for the stress distribution within the dentin-composite disk. The FE method was therefore used to calculate the interfacial bond strength based on the load that caused debonding. Due to symmetry, a 2-D model representing a quadrant of the disc specimen (Fig. 3a) was constructed using Hypermesh 11.0 (HyperWorks, Altair Engineering, Troy, MI, USA). Appropriate boundary conditions were assigned to the vertical and horizontal planes of symmetry of the quadrant model (Fig. 3a). A point load was applied downward at the topmost node of the model to simulate diametral compression. To capture the stress distribution at the dentin-composite interface accurately, the regions around the interface were meshed more finely than other regions. This numerical model was then exported to ABAQUS (version 6.10-EF1; Dassault Systèmes Simulia, Waltham, MA, USA) to solve for the stresses. The model was meshed with the plane-stress elements CPS4I and CPS3 (21). All materials were assumed to be isotropic, homogeneous and behave linear elastically. The material properties for each component are listed in Table 2. Figure 3b shows the radial stress distribution within the disk and the node at the interface (indicated by the arrow) where debonding was observed to initiate.
Figure 3.
a) 2-D quadrant FE model for the dentin-composite disk specimen. Load was applied at the topmost node, indicated by the arrow. b) Radial stress distribution within the disk specimen. The arrow indicates the node where stress was sampled for bond strength calculation.
Table 2.
Material Properties for the Finite Element Models
Scanning electron microscopy (SEM)
To evaluate the mode of interfacial debonding, SEM images of the fracture surfaces of the specimens were obtained using an environmental scanning electron microscope (TM-3000, Hitachi, High-Technologies Corporation, Tokyo, Japan) with the following settings: X50 magnification, compositional mode and 15 kV.
Statistical Analysis
A two-way analysis of variance (ANOVA) was used to explore the effect of the composite and adhesive systems on the bond strength and the interaction between them. To determine whether a significant difference in bond strength existed among the different combinations of composites and adhesives, a one-way ANOVA was carried out using Tukey’s HSD test as the post hoc test. Fisher’s exact test was used to analyze the failure modes and their association with the composite and adhesive systems used. SAS® 9.3 Software (SAS Institute Inc., Cary, NC, USA) was used to perform the statistical analysis.
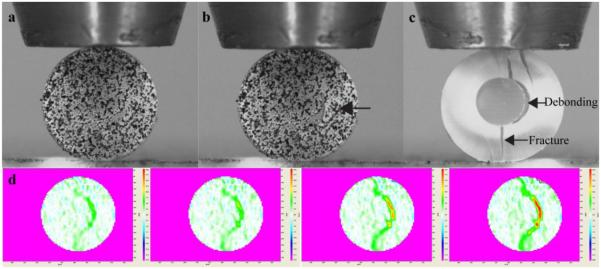
RESULTS
Figs. 4a and 4b show a disk specimen before and after fracture when subjected to diametral compression. Fig. 4c shows a different specimen after fracture with the paint removed from the surface. Most of the specimens (n=84) fractured along part of the dentin-composite interface, with the fracture path extending into the dentin roughly along the vertical diameter, as indicated by the arrows in Fig. 4c. Eight specimens (8.7%) had fracture involving the composite. From the DIC results (Fig. 4d), which showed the emergence and evolution of strain concentrations on the disk surface, it was observed that in the specimens without composite fracture debonding at the interface took place before the fracture extended into the outer dentin ring.
Figure 4.
A dentin-composite disk subjected to diametral compression. a) Disk specimen before loading - its surface had been sprayed with white paint and black powder to create speckles for DIC analysis. b) The same specimen after fracture, with debonding between the restorative material and the dentin ring as indicated by the arrow. c) A different specimen with painting removed to reveal the fracture pattern. d) DIC results showing the emergence and spread of strain concentrations during diametral compression.
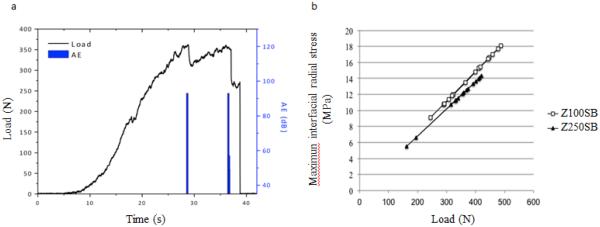
Most of the samples exhibited an approximately linear load-displacement behavior until the first peak was reached (Fig. 5a). Most of the nonlinearity came from the initial development of contact between the disc and the loading plate. The first partial drop in load coincided with the appearance of the strain concentrations at the dentin-composite interface in the DIC images (Fig. 4d) as well as the first major AE signal. Thus, the first load peak was taken to be the load that caused interfacial debonding. The climbing to the second peak and the subsequent complete drop in load showed, respectively, the loading and final separation of the two halves of the debonded disk. It can be seen that both the interfacial and bulk fractures were preceded by the occurrence of AE events (Fig. 5a).
Figure 5.
a) A typical time history of the load and AE events for the dentin-composite disk specimen. b) The maximum interfacial radial stress as a function of load with experimental values superimpossed (□Z100, ▲Z250).
Fig. 5b shows the FE-predicted maximum interfacial radial stress (the one responsible for debonding) as a function of load for the two material systems. The results for bond strength, as derived from using the first peak load (Fig. 5a), are summarized in Fig. 6 and Table 3. From the table, it can be noted that the mean bond strength values for the different bonding systems had the following ranking: EB > MP > SB, irrespective of whether Z100 or Z250 was used. With Z250, the bond strength with EB was significantly greater than those with MP and SB (p<0.05); but no significant differences were detected between SB and MP. Despite showing the same trend, no significant differences were detected amongst the adhesives when Z100 was used.
Figure 6.
Box plot of dentin bond strength values for the different composite and adhesives combinations. Black bar indicates the median value per group and the end of the boxes indicate the interquartile range. EB=Easy bond, MP=Multipurpose and SB=Single Bond.
Table 3.
Mean, ± standard deviation (SD) and coefficient of variation (CV) for dentin bond strength (DBS) of each combination of adhesive and composite.
| Z100 | Z250 | |||
|---|---|---|---|---|
|
| ||||
| Dentin Bond Strength (MPa) |
CV (%) | Dentin Bond Strength (MPa) |
CV (%) | |
| EB | 15.4 (2.1)Aa | 13.6 | 14.3 (1.4)Aa | 9.8 |
| MP | 14.1 (1.7)Aa | 12.1 | 12.2 (2.5)Ba | 20.5 |
| SB | 14.0 (2.8)Aa | 20 | 11.7 (2.5)Ba | 21.4 |
Same upper/lower case letter in a column/row indicates no statistically significant differences at p=0.05 level.
Two-way ANOVA confirmed that there was no interaction between the bonding system and the composite (p >0.05). Considering the effect of composites only, Z100 gave significantly higher bond strength than Z250 (p<0.05). And when only the effect of adhesives was considered, EB gave higher bond strength than SB and MP (p<0.05), but there was no statistically significant difference between SB and MP.
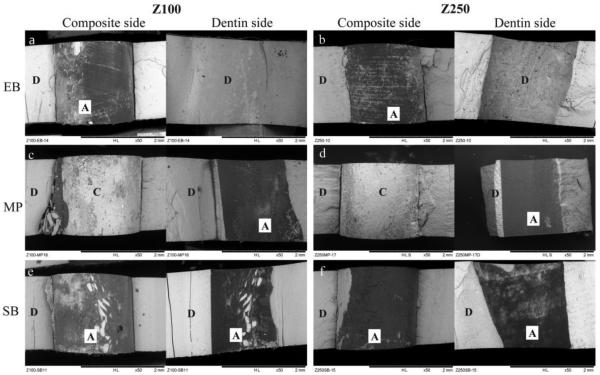
Representative SEM images of the predominant failure mode for each composite/adhesive combination are shown in Fig. 7. The different interfacial failure modes identified from the SEM images of the fracture surfaces were classified and presented in Table 4. The mode of failure was considered as adhesive when it involved the dentin-adhesive interface, the composite-adhesive interface or only the adhesive itself. A cohesive failure was defined as a failure involving only the dentin or the composite. A mixed-mode failure was defined as a combination of adhesive and cohesive failures.
Figure 7.
SEM images of fracture surfaces of specimens from the diametral compression test. A= adhesive, C= composite and D=dentin.
Table 4.
Frequency and percentage of failure mode by composite/adhesive combination
| Failure Type | |||
|---|---|---|---|
|
| |||
| Combination of composite/adhesive |
Adhesive n° (%) |
Mixed n° (%) |
Cohesive n° (%) |
| Z100/EB (n=15) | 13 (86.7) | 1 (6.7) | 1 (6.7) |
| Z100/MP (n=16) | 16 (100.0) | 0 (0.0) | 0 (0.0) |
| Z100/SB (n=15) | 12 (80.0) | 0 (0.0) | 3 (20.0) |
| Z250/EB (n=15) | 12 (80.0) | 2 (13.3) | 1 (6.7) |
| Z250/MP (n=16) | 16 (100.0) | 0 (0.0) | 0 (0.0) |
| Z250/SB (n=15) | 15 (100.0) | 0 (0.0) | 0 (0.0) |
|
| |||
| Total | 84 (91.3) | 3 (3.2) | 5 (5.4) |
Adhesive failure was found to be predominant, accounting for 80 to 100% of all failures (Table 4). In addition, as displayed in Fig. 7, each composite/adhesive combination seemed to present a distinct adhesive failure mode. To explore the association between the composite/adhesive system and the actual mode of adhesive failure, the latter was subdivided according to the exact position of failure, i.e., composite-adhesive interface, adhesive-dentin interface, or within the adhesive layer itself. The results are summarized in Fig. 8, which shows that the mode of adhesive failure was largely determined by the bonding system; the composite did not have much effect. Fig. 7b shows that EB, when combined with either Z100 or Z250, exhibited an adhesive failure involving the adhesive-dentin interface, as one half of the fracture surface showed the adhesive layer (dark) and the other half showed the dentin surface. In the case of MP, fracture mostly involved the composite-adhesive interface regardless of the composite used. SB showed a mixed mode of adhesive failure: in about half of the specimens, the adhesive layer itself failed cohesively (Fig. 7e and f); the rest failed at the composite-adhesive interface. Fisher’s exact test confirmed the association between the type of adhesive and the failure mode (p<0.0001).
Figure 8.
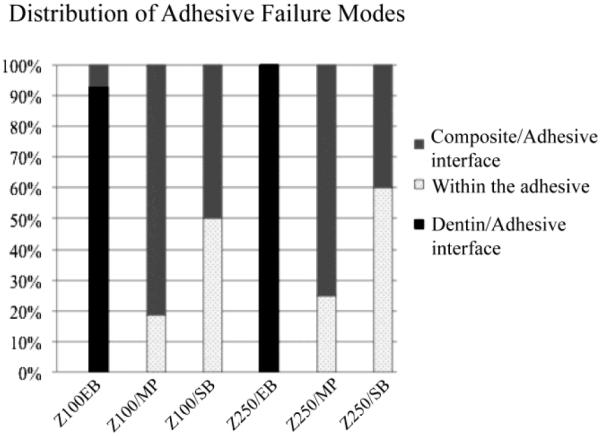
Frequency distribution of the modes of adhesive failure for each composite-adhesive combination.
DISCUSSION
Conventionally, the bond strength at the tooth-resin composite interface is evaluated using direct tensile or shear bond tests. Among these methods, the specimen shape and experimental fixture used vary considerably, so do the bond strength measurements, even for the same system of materials (22). Note that, in a bi-material system, a stress singularity will always exist at the free edges of the interface, the degree of singularity being dependent on the mechanical properties of the substrates (7). It is therefore not surprising to find that the mechanical properties of the composite, in particular the elastic modulus, can affect the results from bond strength testing (7, 16). In fact, finite element analysis demonstrated that the higher the mismatch in mechanical properties between the substrates the higher the stress concentration at the interface, which results in lower bond strengths (6, 7). Further, for some of the specimens, preparation involves extensive machining in the form of sectioning and trimming, which can lead to a high incidence of pre-test failures (5).
The Brazilian disk test has been used widely for testing the fracture strength of brittle materials. Many authors have described this method and its merits and limitations discussed at length (19, 23, 24). The new variant of the Brazilian disk introduced here was prepared using typical steps in adhesive dentistry, and required much less machining than some micro-tensile test specimens (22). For that reason, we observed no pre-test failure. The dentin-restoration interface also formed a closed loop with no abrupt ends in the circular plane, thereby reducing the stress concentration due to the mismatch in material properties. Again, using the DIC and AE techniques, we demonstrated the viability of the test by showing that failure of the disk was initiated by debonding at the dentin-composite interface. The specimen’s shape and size also resembled those of a Class-I restoration, so the measured bond strength should be representative of those of real restorations as correction for the dependence on specimen size (the so-called size effect) would be minimal.
Because the disk specimen resembled a Class-I restoration with a very high level of constraints, the possible effect of shrinkage stress on the measured bond strength cannot be ignored. Care must therefore be taken to minimize the shrinkage stress by using an incremental filling technique. Moreover, since a simple analytical solution is not available, the bond strength has to be calculated using a numerical method such as the Finite Element method used in this study. Consequently, accuracy of the results depends very much on that of the input data, e.g. Young’s modulus of the materials, which have a high degree of uncertainty. Sensitivity studies therefore need to be carried out to quantify the effect of the uncertainty in the input data on the calculated bond strength. Common to all disc in diametral compression tests, high contact stresses exist at the loading and supporting points, leading to the possibility of local damage or even satellite cracking. These may have contributed to the nonlinear load-displacement behavior observed. The high contact stresses can be reduced by using curved loading and supporting plates.
Statistical analysis of the results showed that both the composite and the adhesive affected the bond strength, but there appeared to be no interaction between the two components. EB showed higher bond strength than SB and MP, but no significant differences were detected between SB and MP. A similar trend was found by da Silva et al. (25) who studied the effect of dentin thickness on the micro-shear bond strength of different bonding systems after 24 hours of water storage. The authors found that the self-etching system EB had the highest median bond strength (21 and 27 MPa) for both of the dentin thicknesses (200 and 500 μm) analyzed, followed by SB (15.6 and 23.4 MPa), and MP (15.2 and 17.9 MPa). Other investigators have also reported that self-etching bonding systems performed better than etch-and-rinse systems (26). Overall, however, results remain contradictory. For example, Dantas et al. (27) found the shear bond strength of two total-etch systems (Single Bond 2 and Multipurpose) to be significantly higher than that of two self-etching systems after 24 hours of water storage. Similar results were found by Mcleod et al. (28) when evaluating the influence of the C-factor on shear bond strength. However, they showed that SB only produced higher bond strength than EB with enamel; no differences in bond strength between the adhesive systems were found with dentin. On the other hand, Perdigao et al. (29) found that MP (65.4 ± 9.5 MPa) resulted in significantly higher micro-tensile dentin bond strength than all the other adhesives tested, including SB and EB, although they did find EB (58.6 ± 6.1 MPa) to perform better than SB (44.7 ± 10.8 MPa). Yet other studies have found no significant differences between the total-etch and self-etch adhesives used in this study (30).
One reason that may explain the better immediate bond strength of self-etch adhesives found in this and other studies (25, 26) is that they reduce the technique sensitivity associated with the application of bonding systems. Self-etch systems simplify the bonding process by eliminating some of the more technique-sensitive steps, such as moisture control, in the use of total-etch systems, which can lead to inadequate infiltration. Self-etch systems contain hydrophilic and acidic monomers, which are able to simultaneously demineralize and penetrate the dentin, thus reducing the risk of incomplete resin infiltration. Moreover, because of their highly hydrophilic component, the level of moisture in the dentin is not a critical factor in bond formation (31). However, also because of their high hydrophilicity, these adhesives are very permeable and prone to water sorption, which ultimately plasticizes the polymers and lowers their mechanical properties over time (32).
The inconsistent results obtained by the different groups studying the same materials may also be explained by the high variability inherent in the tensile and shear bond tests. In a recent review (22), the coefficients of variation of several bond strength tests were retrieved from 147 articles. The adhesives they assessed included two of those studied here (SB and MP). The review showed a high scatter in the data, with the coefficient of variation ranging from 22% to 49% for the micro-tensile test, 20% to 53% for the tensile test, 24% to 45% for the shear test and 9% to 36% for the micro-shear test, although an insufficient number of studies was used for the micro-shear test. Possible sources of this variability, as discussed previously, were: variations in dimensions of the specimen, thickness of the adhesive and alignment of the specimen; imprecisely machined jigs; and random inherent flaws in the adhesive or those generated by the preparation procedure, just to name some of them (22). With the modified BDT specimen, the coefficient of variation of the measured bond strengths found in this study ranged between 10% and 22%, which was much lower than the ones reported in the literature for the other types of bond test.
One of the advantages of the modified BDT which may have contributed to the reduced variability in the results is that no fixation of the specimen is required. This, in particular, allows for quick test setup, which avoids dehydration of the specimen, and the elimination of spurious stresses at the fixation points due to specimen misalignment, thus minimizing technique-related errors.
Another reason proposed for the large variability in most bond strength measurement is the high percentage of cohesive failure involving dentin or composite obtained with the tensile and shear bond tests. For example, with the micro-tensile test, the percentage of such cohesive failures ranged from 20% to 39% (22). In the present study, this was 0% for three of the six groups tested and between 7% and 20% for the other three groups. We therefore had a high incidence of adhesive failures across the groups. As mentioned before, for a bond strength test to be valid, failure must initiate from the interface. Otherwise, the measurement would likely be an underestimate of the true value.
The adhesive failures observed in this study could be subdivided according to which region it occurred in. For example, when MP was used, a higher frequency of composite-adhesive interfacial failure was found; but when EB was used failure mainly occurred at the dentin-adhesive interface; whereas SB showed a combination of cohesive failure in the adhesive and interfacial failure at the composite-adhesive interface. This may explain the higher coefficient of variation seen in the results with SB (Table 3). The cohesive failure seen in the SB adhesive could be attributed to the fact that it was applied in two consecutive coatings, between which a weak interface could have formed. Similar results for SB were found by Salvio et al. (26) and Belli et at. (33), who reported a high frequency of failure involving the adhesive layer. A high percentage (~70%) of adhesive failure involving the dentin-adhesive interface has also been reported by others for EB (29), but the same adhesive was found to produce a high incidence of composite cohesive failure (~40%) in other studies (29). Bouillaguet et al. (34) and Perdigao et al. (29) also found a high frequency of adhesive failure for MP; however, the dentin-adhesive interface was mostly involved, which differed from the current study. The inconsistent results observed in the failure mode might be explained by differences in the testing conditions and a lack of standardization among the studies.
The actual mode of failure at the tooth-restoration interface may determine the likelihood of developing secondary caries following interfacial breakdown. For example, with the dentin still fully covered, teeth restored with systems that fail at the composite-adhesive interface may be less likely to develop secondary caries.
CONCLUSIONS
The new variant of the BDT specimen provides several advantages for testing dentin-composite bond strength. These include zero premature failure, simpler testing procedures, a consistent failure mode involving the adhesive interface, and reduced variation in the measurements.
Clinical significance.
The new test could help to predict the clinical performance of adhesive systems more effectively and consistently by reducing the coefficient of variation in the measured bond strength.
ACKNOWLEDGMENT
This study was partially supported by the National Institute of Dental and Craniofacial Research (NIDCR), USA through Grant No. 1 R01 DE021366 and the CONICYT Becas Chile Scholarship Program, Chilean Government. The authors of this manuscript declare that no benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Dennison JB, Sarrett DC. Prediction and diagnosis of clinical outcomes affecting restoration margins. J Oral Rehabil. 2012;39(4):301–18. doi: 10.1111/j.1365-2842.2011.02267.x. [DOI] [PubMed] [Google Scholar]
- 2.Drummond JL. Degradation, fatigue, and failure of resin dental composite materials. J Dent Res. 2008;87(8):710–9. doi: 10.1177/154405910808700802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim RJ, Kim YJ, Choi NS, Lee IB. Polymerization shrinkage, modulus, and shrinkage stress related to tooth-restoration interfacial debonding in bulk-fill composites. J Dent. 2015;43(4):430–9. doi: 10.1016/j.jdent.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Cenci MS, Pereira-Cenci T, Cury JA, Ten Cate JM. Relationship between gap size and dentine secondary caries formation assessed in a microcosm biofilm model. Caries Res. 2009;43(2):97–102. doi: 10.1159/000209341. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong S, Geraldeli S, Maia R, Raposo LH, Soares CJ, Yamagawa J. Adhesion to tooth structure: a critical review of "micro" bond strength test methods. Dent Mater. 2010;26(2):e50–62. doi: 10.1016/j.dental.2009.11.155. [DOI] [PubMed] [Google Scholar]
- 6.Braga RR, Meira JB, Boaro LC, Xavier TA. Adhesion to tooth structure: a critical review of "macro" test methods. Dent Mater. 2010;26(2):e38–49. doi: 10.1016/j.dental.2009.11.150. [DOI] [PubMed] [Google Scholar]
- 7.Van Noort R, Noroozi S, Howard IC, Cardew G. A critique of bond strength measurements. J Dent. 1989;17(2):61–7. doi: 10.1016/0300-5712(89)90131-0. [DOI] [PubMed] [Google Scholar]
- 8.Pashley DH, Sano H, Ciucchi B, Yoshiyama M, Carvalho RM. Adhesion testing of dentin bonding agents: a review. Dent Mater. 1995;11(2):117–25. doi: 10.1016/0109-5641(95)80046-8. [DOI] [PubMed] [Google Scholar]
- 9.Perinka L, Sano H, Hosoda H. Dentin thickness, hardness, and Ca-concentration vs bond strength of dentin adhesives. Dent Mater. 1992;8(4):229–33. doi: 10.1016/0109-5641(92)90090-y. [DOI] [PubMed] [Google Scholar]
- 10.Schreiner RF, Chappell RP, Glaros AG, Eick JD. Microtensile testing of dentin adhesives. Dent Mater. 1998;14(3):194–201. doi: 10.1016/s0109-5641(98)00030-x. [DOI] [PubMed] [Google Scholar]
- 11.Li J, Li H, Yun X, Fok AS. A comparison of bond strengths measured using cantilever bending and micro-tensile methods. Dent Mater. 2011;27(12):1246–51. doi: 10.1016/j.dental.2011.08.593. [DOI] [PubMed] [Google Scholar]
- 12.Campillo-Funollet M, Dargush GF, VanSlooten RA, Mollendorf JC, Kim H, Makowka SR. Size-dependent strength of dental adhesive systems. Dent Mater. 2014;30(8):e216–28. doi: 10.1016/j.dental.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Rasmussen ST. Analysis of dental shear bond strength tests, sheer or tensile? International Journal of Adhesion and Adhesives. 1996;16(3):147–54. [Google Scholar]
- 14.Soderholm KJ, Geraldeli S, Shen C. What do microtensile bond strength values of adhesives mean? J Adhes Dent. 2012;14(4):307–14. doi: 10.3290/j.jad.a22767. [DOI] [PubMed] [Google Scholar]
- 15.Van Noort R, Cardew GE, Howard IC, Noroozi S. The effect of local interfacial geometry on the measurement of the tensile bond strength to dentin. J Dent Res. 1991;70(5):889–93. doi: 10.1177/00220345910700050501. [DOI] [PubMed] [Google Scholar]
- 16.Placido E, Meira JB, Lima RG, Muench A, de Souza RM, Ballester RY. Shear versus micro-shear bond strength test: a finite element stress analysis. Dent Mater. 2007;23(9):1086–92. doi: 10.1016/j.dental.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Huang SH, Lin LS, Rudney J, Jones R, Aparicio C, Lin CP, et al. A novel dentin bond strength measurement technique using a composite disk in diametral compression. Acta Biomater. 2012;8(4):1597–602. doi: 10.1016/j.actbio.2011.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tong J, Wong KY, Lupton C. Determination of interfcial fracture toughness of bone-cement interface using sandwich Brazilian disks. Engineering Fracture Mechanics. 2007;74(12):1904–16. doi: 10.1016/j.engfracmech.2006.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang JS. Experimental determination of interfcail toughness curves using Brazil-Nut-Sandwiches. Acta Metall Mater. 1989;38(7):1279–90. [Google Scholar]
- 20.Procopio AT, Zavalangios A, Cunningham J. Analysis of the diametrical compression test and the applicability to plastically deforming materials. JOURNAL OF MATERIALS SCIENCE. 2003;36(17):3629–39. [Google Scholar]
- 21.Corp. DSS, editor. ABAQUS 6.11 documentation. Providence, RI, USA: 2011. [Google Scholar]
- 22.Scherrer SS, Cesar PF, Swain MV. Direct comparison of the bond strength results of the different test methods: a critical literature review. Dent Mater. 2010;26(2):e78–93. doi: 10.1016/j.dental.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Soares JB. Bimaterial Brazilian Specimen for determining interfacial fracture toughness. Engineering Fracture Mechanics. 1998;59(1):57–71. [Google Scholar]
- 24.Atkinson C. Combined mode fracture via the cracked Brazilian disk test. International Journal of Fracture. 1982;18(4):279–91. [Google Scholar]
- 25.da Silva JM, Rodrigues JR, Camargo CH, Fernandes VV, Jr., Hiller KA, Schweikl H, et al. Effectiveness and biological compatibility of different generations of dentin adhesives. Clin Oral Investig. 2014;18(2):607–13. doi: 10.1007/s00784-013-1000-9. [DOI] [PubMed] [Google Scholar]
- 26.Salvio LA, Hipolito VD, Martins AL, de Goes MF. Hybridization quality and bond strength of adhesive systems according to interaction with dentin. Eur J Dent. 2013;7(3):315–26. doi: 10.4103/1305-7456.115416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dantas DC, Ribeiro AI, Lima LH, de Lima MG, Guenes GM, Braz AK, et al. Influence of water storage time on the bond strength of etch-and-rinse and self-etching adhesive systems. Braz Dent J. 2008;19(3):219–23. doi: 10.1590/s0103-64402008000300008. [DOI] [PubMed] [Google Scholar]
- 28.McLeod ME, Price RB, Felix CM. Effect of configuration factor on shear bond strengths of self-etch adhesive systems to ground enamel and dentin. Oper Dent. 2010;35(1):84–93. doi: 10.2341/09-075-L. [DOI] [PubMed] [Google Scholar]
- 29.Perdigao J, Sezinando A, Monteiro PC. Effect of substrate age and adhesive composition on dentin bonding. Oper Dent. 2013;38(3):267–74. doi: 10.2341/12-307-L. [DOI] [PubMed] [Google Scholar]
- 30.Carvalho AO, Carrilho MRO, Rueggeberg FA, Ambrosaho GMB, Giannini M. Bond strength, biaxial flexural strength and flexural modulus of dentin bonding systems exposed to water. International Journal of Adhesion and Adhesives. 2014;49:109–14. [Google Scholar]
- 31.Manuja N, Nagpal R, Pandit IK. Dental adhesion: mechanism, techniques and durability. J Clin Pediatr Dent. 2012;36(3):223–34. [PubMed] [Google Scholar]
- 32.Delaviz Y, Finer Y, Santerre JP. Biodegradation of resin composites and adhesives by oral bacteria and saliva: a rationale for new material designs that consider the clinical environment and treatment challenges. Dent Mater. 2014;30(1):16–32. doi: 10.1016/j.dental.2013.08.201. [DOI] [PubMed] [Google Scholar]
- 33.Belli R, Sartori N, Peruchi LD, Guimaraes JC, Araujo E, Monteiro S, Jr., et al. Slow progression of dentin bond degradation during one-year water storage under simulated pulpal pressure. J Dent. 2010;38(10):802–10. doi: 10.1016/j.jdent.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 34.Bouillaguet S, Gysi P, Wataha JC, Ciucchi B, Cattani M, Godin C, et al. Bond strength of composite to dentin using conventional, one-step, and self-etching adhesive systems. J Dent. 2001;29(1):55–61. doi: 10.1016/s0300-5712(00)00049-x. [DOI] [PubMed] [Google Scholar]
- 35.Sideridou I, Tserki V, Papanastasiou G. Study of water sorption, solubility and modulus of elasticity of light-cured dimethacrylate-based dental resins. Biomaterials. 2003;24(4):655–65. doi: 10.1016/s0142-9612(02)00380-0. [DOI] [PubMed] [Google Scholar]
- 36.Chung SM, Yap AU, Tsai KT, Yap FL. Elastic modulus of resin-based dental restorative materials: a microindentation approach. J Biomed Mater Res B Appl Biomater. 2005;72(2):246–53. doi: 10.1002/jbm.b.30145. [DOI] [PubMed] [Google Scholar]
- 37.Emami N, Soderholm KJ, Berglund LA. Effect of light power density variations on bulk curing properties of dental composites. J Dent. 2003;31(3):189–96. doi: 10.1016/s0300-5712(03)00015-0. [DOI] [PubMed] [Google Scholar]
- 38.Craig RG, Peyton FA. Elastic and mechanical properties of human dentin. J Dent Res. 1958;37(4):710–8. doi: 10.1177/00220345580370041801. [DOI] [PubMed] [Google Scholar]
- 39.Marshall GW, Jr., Marshall SJ, Kinney JH, Balooch M. The dentin substrate: structure and properties related to bonding. J Dent. 1997;25(6):441–58. doi: 10.1016/s0300-5712(96)00065-6. [DOI] [PubMed] [Google Scholar]