Abstract
Background
Electromyography (EMG) and musculoskeletal (MSK) ultrasound (US) are core learning objectives during physical medicine and rehabilitation (PM&R) training. However, there have been no prior studies using MSK US to assess the acquisition of EMG procedural skills during residency training. This study aims to demonstrate the differences in skillful needle placement between junior and senior physiatry residents. The integration of both EMG and MSK US may have tremendous potential for additional learning opportunities related to electrodiagnostic education.
Objective
To determine the accuracy of anatomic landmark–guided EMG needle electrode placement in commonly used muscles by PM&R resident physicians.
Design
Cross-sectional study.
Setting
An academic PM&R residency program.
Participants
Twelve (5 postgraduate year [PGY] −3 and 7 PGY-4) PM&R resident physicians participating in a MSK US training course.
Methods
Twelve PM&R residents in the eighth month of their third and fourth years of postgraduate training performed anatomic landmark–guided needle placement to the extensor indicis proprius (EIP), pronator teres (PT), peroneus longus (PL), and soleus muscles of live subjects. Once the needle electrode was satisfactorily placed, needle localization was verified with US.
Main outcome measures
Accuracy of EMG needle electrode placement.
Results
The overall accuracy of needle electrode placement for all resident participants was 68.8%. The mean accuracy of the 4 selected muscles was 50% by PGY-3 residents and 82.1% for PGY-4 residents (P = .01). EIP was the most commonly missed muscle, with correct placement performed by 20% of PGY-3 and 42.9% of PGY-4 residents. PGY-3 residents demonstrated 60% accuracy with localizing the PT, PL, and soleus muscles. PGY-4 residents demonstrated 85.7% accuracy for PT, and 100% accuracy for both PL and soleus muscles.
Conclusions
Senior residents demonstrated greater accuracy of landmark-guided needle placement than junior residents. EMG procedural skills are important milestones in PM&R training, and MSK US may be a useful tool to enhance resident learning.
Introduction
Electromyography (EMG) is a time-intensive, operator-dependent diagnostic procedure that requires extensive training for the operator to become proficient. It is also a required competency of physical medicine and rehabilitation (PM&R) residency training. EMG training traditionally takes place in the classroom followed by self-study, observation, and eventually hands-on practice under supervision in the clinical setting. Critical to the performance and integrity of an EMG study is the ability of the examiner to quickly and accurately place the needle electrode in the desired muscle. The difficulty of this skill is commonly underestimated by seasoned electromyographers, and it can be one of the more daunting challenges to a trainee. When the electromyographer’s proficiency and accuracy of needle placement is low, the diagnostic integrity of the study suffers, and the study itself can become more painful for patients [1].
Multiple studies have assessed needle placement accuracy in cadavers. Accuracy rates of needle placement by trained electromyographers, confirmed by dissection, ranged from 0%–100% accuracy for each muscle tested, with an overall accuracy of 57% [2]. A similar study using cadavers and placement confirmation by dissection demonstrated correct placement in 45% of upper limb and 52% of lower limb muscles [3]. Ultrasound was used as an adjunct to needle placement in another cadaveric study for EMG needle placement, and demonstrated 96% accuracy compared to 39% accuracy of needle placement when using anatomic landmark guidance alone (P < .0001) [4]. Ultrasound is also being used to confirm placement of needles in living humans. A prior study in children with cerebral palsy demonstrated 78% accuracy of needle placement for botulinum toxin type A injections into the gastrocnemius muscles when using anatomic landmarks and verification with MSK US [5]. Multiple studies have demonstrated excellent precision with US-guided peripheral joint and soft tissue injections [6–11]. In addition, US guidance for EMG needle placement into the diaphragm has been promoted to increase the safety of the study [12–14]. Expanding the use of US in EMG studies is currently a growing area of interest.
The increasing popularity of musculoskeletal (MSK) ultrasound (US) in the last decade has made it more accessible to use in education as well as patient care. MSK US is also being used to provide direct feedback to residents in training when performing other critical competency skills such as the physical examination [15,16]. The real-time feedback for a trainee performing a test is a valuable asset to any educational curriculum, because it is an objective measure of performance. The true potential of using MSK US is not yet fully actualized, and the opportunities for incorporating MSK US with EMG education are great.
It is assumed that accuracy improves with experience throughout the resident training process. However, obtaining objective evidence that residents improve with increased experience in a procedural setting is difficult. In this study, we sought to evaluate the accuracy of EMG needle electrode placement in 4 specific muscles by physical medicine and rehabilitation (PM&R) residents in their postgraduate year 3 (PGY-3) and postgraduate year 4 (PGY-4) levels of training. To our knowledge, there have been no prior studies specifically assessing the accuracy of EMG needle electrode placement through the course of PM&R residency training using US to confirm correct placement. We hypothesized that the PGY-4 residents with more EMG experience would demonstrate better accuracy of needle placement compared to the PGY-3 residents.
Methods
This study was approved by the Northwestern University Institutional Review Board. PM&R residents in the academic institution receive a 5-hour series of introductory lectures, including hands-on EMG skills training, before performing 2 months of EMG training during their PGY-3 year and then 3 months during the PGY-4 year. As part of routine formal education, residents are taught EMG electrode placement, using anatomic landmarks, on their fellow residents. Eight months into the academic year, the accuracy of needle EMG placement by residents on their peers was assessed by attending physicians using US. Informed consent was obtained to report the de-identified data. Residents were assured that their participation in this study would have no impact on their promotion and status within the residency program. Only PGY-3 and PGY-4 were included in the study to ensure that residents would have a significant level of exposure and experience with EMG. All participants had completed at least 1 EMG rotation.
The primary outcome measure was accuracy of needle placement in each of the 4 selected muscles: extensor indicis proprius (EIP), pronator teres (PT), peroneus longus (PL), and soleus. These muscles were chosen because of their frequency of use during EMG procedures and/or botulinum A toxin injections, as well as their superficial location allowing residents to palpate these muscles for localization. Residents were allowed to palpate anatomic landmarks and to use muscle activation to place the needle into the muscle, as they would typically be allowed to do during an EMG study. They were given no direction other than the name of the muscle that they were to target, and a machine was not provided for electromyographic feedback. The resident acting as the model was not allowed to assist the subject. Monopolar 25-mm, 28-gauge needle electrodes were chosen to minimize discomfort. An MSK attending physician (K.K.) with 3 years of US experience (1 year of US experience as an attending physician) evaluated the placement of the tip of each electrode with a high-frequency linear array transducer (14-6 MHz, Mindray M7, Mahwah, NJ) using in-plane and out-of-plane imaging of the needle (Figures 1–4), as well as real-time “jiggling” of the needle [17]. A sports medicine physiatrist with greater than 5 years of US experience (M.R.) was available to clarify any borderline or unclear needle placements. The residents involved (subjects and models) also participated in the verification process of needle accuracy to take advantage of the critical learning component that was available in this process.
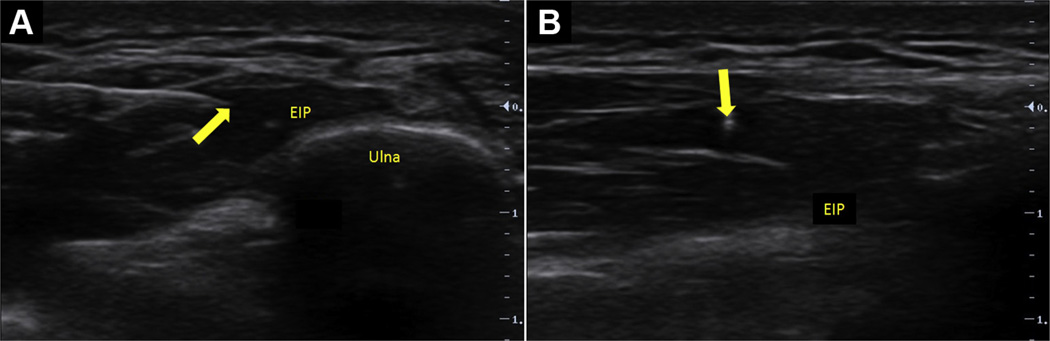
Figure 1.
Extensor indicis proprius (EIP) with needle in view (arrows). (A) Short-axis view of EIP with needle in-plane. (B) Long-axis view of EIP with needle out-of-plane.
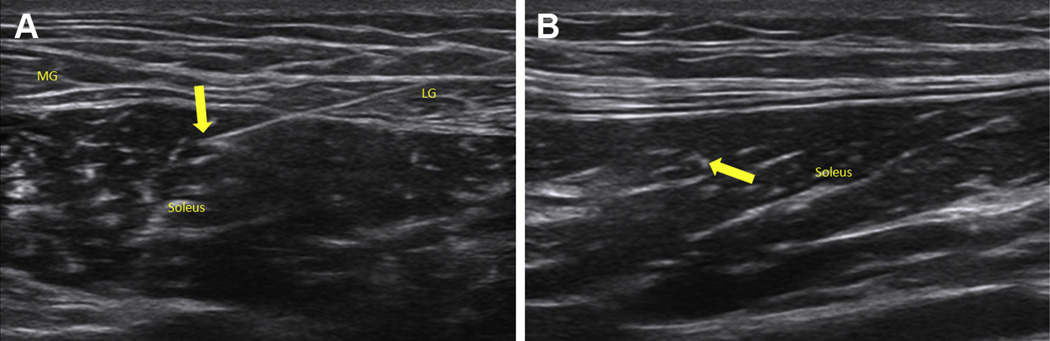
Figure 4.
Soleus with needle in view (arrows). (A) Short-axis view of soleus with needle in-plane. (B) Long-axis view of soleus with needle out-of-plane.
Accuracy of needle placement was recorded for each muscle, and the data were de-identified for analysis. Sample size was determined by the number of upper-level residents participating in this voluntary US education course; therefore a power analysis was not performed. A Student t-test was used to make statistical comparisons between the performances of the 2 groups.
Results
Data were collected from the 12 participating resident electromyographers, including 5 PGY-3 and 7 PGY-4 resident physicians. Accuracy rates were calculated for each muscle by level of residency training. Overall accuracy of needle electrode localization was 68.8% for all of the muscles tested. PGY-4 residents demonstrated superior accuracy compared with PGY-3 residents for all 4 selected muscles (EIP, PT, PL, and soleus). Localization of the EIP was the least accurate, demonstrating correct placement by 20% of PGY-3 and 42.9% of PGY-4 residents. Overall accuracy of all the selected muscles was 50% for PGY-3 and 82.1% for PGY-4 residents (Table 1), demonstrating a statistically significant difference in overall accuracy of needle placement between levels of training (P = .01).
Table 1.
Accuracy of needle placement into targeted muscles, by level of experience
| EIP | PT | PL | Soleus | Overall | |
|---|---|---|---|---|---|
| PGY3 residents (n = 5) | 20.0% | 60.0% | 60.0% | 60.0% | 50.0% |
| PGY4 residents (n = 7) | 42.9% | 85.7% | 100.0% | 100.0% | 82.1% |
| All resident participants (n = 12) | 33.3% | 75.0% | 83.3% | 83.3% | 68.8% |
EIP = extensor indicis proprius; PT = pronator teres; PL = peroneus longus; PGY = postgraduate year.
We also recorded the final locations of the needles that missed the targeted muscles. For the EIP muscle, which was most commonly missed, the final needle locations were the extensor carpi ulnaris (2), extensor digitorum communis (1), extensor pollicis longus (1), extensor carpi radialis longus (1), and subcutaneous tissue (1). For the PT muscle, the final needle locations were the flexor carpi radialis (1), subcutaneous tissue (1), and the lateral forearm rather than the medial forearm (1). For the PL muscle, the final needle locations were extensor digitorum longus (1) and lateral gastrocnemius muscle (1). The final needle location of the missed soleus muscles were the gastrocnemius muscles (2).
Discussion
Imperative to electrodiagnostic training is learning the appropriate anatomy for muscle localization. Traditionally, at our institution, junior residents learn by first studying in the classroom and then observing senior residents and attending physicians perform EMG studies. Concurrently, residents spend time solidifying their knowledge of muscle innervation and identifying muscle locations based on surface anatomy from a reference EMG anatomy book. Although not required during rotations, many residents practice needle placement into each other as a means to learn both how to maneuver the needles and to better understand the patient experience. They are frequently required to demonstrate basic needle placement proficiency on a supervising physician before performing this diagnostic procedure on patients in the clinical setting. In this traditional method of education, the trainee is given only indirect feedback about accuracy.
Although the use of visual and auditory electromyographic feedback strategies is the standard of care for muscle localization, it may not be 100% accurate, especially considering that this is an acquired skill that also presumably improves with experience. Even when one acquires proficiency with using such feedback, it is important to consider confounding factors that may affect the examination. For example, atrophied muscles may not provide satisfactory auditory feedback due to the loss of motor unit fibers. Another consideration is that adjacent muscles can be co-activated (ie, flexor carpi radialis and PT). Some patients find it difficult to perform isolated contractions of a specific muscle, and, in certain scenarios it may be impossible to differentiate between adjacent muscles based on activation alone. As an example, in poststroke patients with spastic extremities undergoing chemodenervation, EMG guidance will not isolate the targeted muscle if surrounding muscles are also spastic [18]. Direct feedback is possible with US by visualizing the needle electrode in the desired muscle, and this can be used in conjunction with traditional palpation and EMG feedback [4]. This may be particularly important for muscles that are difficult to assess due to either their size or deep location.
A previous study demonstrated that traditional needle placement without US visualization was correct 39% of the time. The authors reported a “slightly better needle placement accuracy” by the seasoned electromyographer when compared with the PM&R resident with 5 months of training (not statistically significant) [4]. Our study supports their finding that accuracy improves with greater experience. Although we were able to achieve statistically significant differences in accuracy based upon level of training, this may be best explained by the exponential learning that occurs during early EMG training. Our study also highlights that the EIP muscle may be difficult to localize using anatomic landmarks, even for PGY-4 residents near the end of their training.
We believe that incorporating US into EMG education would improve the residents’ understanding of anatomy as well as disease processes (eg, muscle appearance in myopathies, denervation atrophy, traumas). Ultrasound allows a qualitative visual assessment of the muscle itself, which can serve to support EMG findings. For example, chronically denervated muscles and muscles affected by neuromuscular disorders may have increased hyperechogenicity on US due to increased adipose tissue and/or may be noticeably atrophied. These qualitative assessments may even be evaluated quantitatively if desired [19].
Prior studies acknowledge that many adjacent muscles share dual innervation and a minimally misplaced needle will not likely change the outcome of most radiculopathy studies. However, there are clinical situations, such as botulinum toxin administration or fine wire electrode placement for physiological studies, in which it is critical for the electrode to be in the correct muscle. In addition, there are disease processes that affect specific muscles, such as the preferential involvement of the flexor digitorum profundus seen in inclusion body myositis [20,21]. Ultrasound is important for avoiding unintended complications such as puncturing nerves or blood vessels. There is also the risk of damaging tendons and other soft tissue structures. A previous study documented that of 263 needle placement attempts, 9.5% struck or nearly struck “undesirable targets” [2]. The patients most at risk for a misdirected needle are patients who are obese, are taking anticoagulants, or have altered anatomy from either trauma or surgery.
The authors of this article want to stress the importance of optimizing the training of residents in anatomy and needle electrode placement. The ideal is to strive to train residents to place needle electrodes in the correct muscle 100% of the time on their first attempt, as this is an invasive study with the results directly affecting diagnosis and management. EMG and neuromuscular US are complementary tools [12], and the integration of these 2 modalities can potentially both improve patient care and optimize the resident education process. It has been shown that US is helpful for learning anatomy and physiology in medical education and in resident/fellow education [15,16,22,23]. Residents deserve an education that is based on objective feedback to help promote optimal understanding of anatomy and physiology, and this can now be accomplished with the use of US.
Future studies could simulate the clinical setting when assessing resident accuracy rates and the usefulness of US. Residents could be given the opportunities to use EMG anatomy atlases, muscle palpation during activation, and EMG auditory feedback of motor unit activity while comparing the outcomes with and without US guidance.
Limitations of this study include a small sample size and a single-center study design. In addition, subjects were not given the opportunity to use auditory feedback of motor unit activity to help guide their needle placement. However, as mentioned previously, using auditory feedback is an acquired skill that develops over time. A prior study accounted for this by taking needle trajectory into account, noting that a needle tip that was found to be located in an incorrect muscle but along the correct trajectory to the targeted muscle would likely have been placed correctly if the physician had received auditory feedback [4]. Our study did not take trajectory into account, which may have led to an increased miss rate. In addition, residents were not given the opportunity to use a standard EMG anatomical reference textbook during the study as they would have available in the clinical setting. That being said, the muscles chosen for this study are frequently tested in routine EMG evaluations and in chemodenervation procedures, which highlights the discrepancy in the results between PGY-3 and PGY-4 residents.
Limitations of the study related to the use of the US machine for accuracy confirmation are directly related to the fact that most subjects in the study inserted needles perpendicular or near perpendicular to the surface of the skin. Needles under US are best visualized if they are parallel to the transducer surface. This made visualization of the needle tip difficult in certain situations. A gel standoff strategy was used to attempt to adjust for this difficulty. However, in some cases, confirmation of the location of the electrode required other strategies such as the “jiggling” technique [17] of the needle in the muscle and/or activation of the muscle while monitoring for needle motion in the way that one confirms needle location in a tendon sheath injection.
Conclusion
PM&R residents at our institution improve their anatomic landmark–guided accuracy of electromyography needle placement through the course of their training. We believe that the addition of US use during PM&R residency can further enhance the educational process in the performance of electrodiagnostic studies and chemodenervation procedures by providing real-time, objective feedback on needle accuracy in targeted muscles.
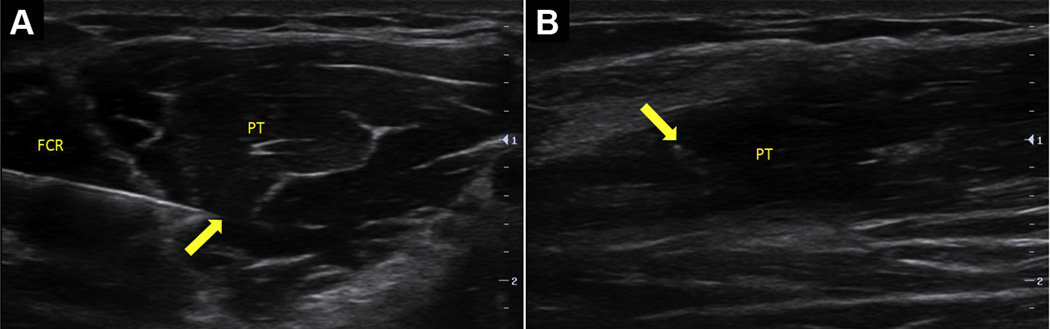
Figure 2.
Pronator teres (PT) with needle in view (arrows). (A) Short-axis view of PT with needle in-plane. (B) Long-axis view of PT with needle out-of-plane.
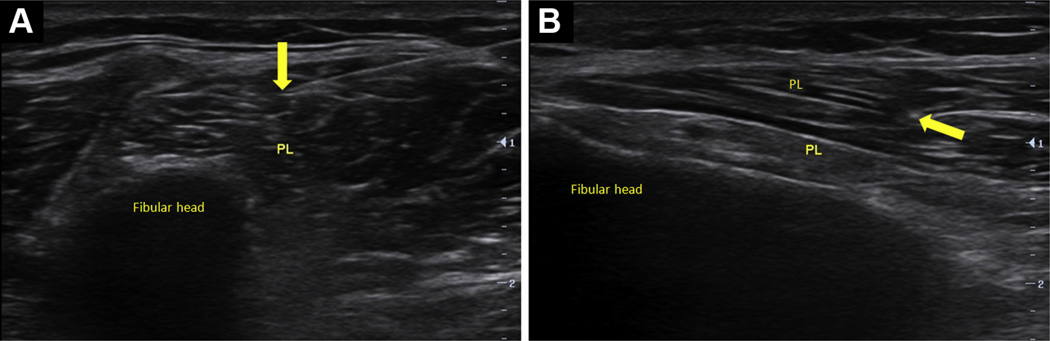
Figure 3.
Peroneus longus (PL) with needle in view (arrows). (A) Short-axis view of PL with needle in-plane. (B) Long-axis view of PL with needle out-of-plane.
Acknowledgments
We thank James Sliwa, DO, for allowing this study to be conducted within his residency program and for allowing us to report the data publicly.
M.E.R. Disclosure: grant, NIH (K12HD001097-16)
Footnotes
Disclosure
K.K. Disclosure: nothing to disclose
C.Z. Disclosure: nothing to disclose
Abstract accepted for presentation at the AAPM&R 2015 Annual Assembly in Boston, MA, October 1–4, 2015.
Contributor Information
Kristopher Karvelas, Department of Physical Medicine and Rehabilitation, Wake Forest Baptist Medical Center, Winston-Salem, NC.
Craig Ziegler, Department of Physical Medicine and Rehabilitation, Rehabilitation Institute of Chicago/McGaw Medical Center of Northwestern University, 345 E. Superior St, Suite 1600, Chicago, IL 60611.
Monica E. Rho, Department of Physical Medicine and Rehabilitation, Rehabilitation Institute of Chicago/McGaw Medical Center of Northwestern University, Chicago, IL.
References
- 1.London ZN, Burke JF, Hazan R, Hastings MM, Callaghan BC. Electromyography-related pain: Muscle selection is the key modifiable study characteristic. Muscle Nerve. 2014;49:570–574. doi: 10.1002/mus.23974. [DOI] [PubMed] [Google Scholar]
- 2.Haig AJ, Goodmurphy CW, Harris AR, Ruiz AP, Etemad J. The accuracy of needle placement in lower-limb muscles: A blinded study. Arch Phys Med Rehabil. 2003;84:877–882. doi: 10.1016/s0003-9993(03)00014-5. [DOI] [PubMed] [Google Scholar]
- 3.Goodmurphy C, Chiodo A, Haig A. The accuracy of needle placement in extremity muscles: A blinded study. J Clin Neurophysiol. 2007;24:366–378. doi: 10.1097/WNP.0b013e3180ca9724. [DOI] [PubMed] [Google Scholar]
- 4.Boon AJ, Oney-Marlow TM, Murthy NS, Harper CM, McNamara TR, Smith J. Accuracy of electromyography needle placement in cadavers: Non-guided vs. ultrasound guided. Muscle Nerve. 2011;44:45–49. doi: 10.1002/mus.22008. [DOI] [PubMed] [Google Scholar]
- 5.Yang EJ, Rha DW, Yoo JK, Park ES. Accuracy of manual needle placement for gastrocnemius muscle in children with cerebral palsy checked against ultrasonography. Arch Phys Med Rehabil. 2009;90:741–744. doi: 10.1016/j.apmr.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 6.Finnoff JT, Hurdle MF, Smith J. Accuracy of ultrasound-guided versus fluoroscopically guided contrast-controlled piriformis injections: A cadaveric study. J Ultrasound Med. 2008;27:1157–1163. doi: 10.7863/jum.2008.27.8.1157. [DOI] [PubMed] [Google Scholar]
- 7.Finnoff JT, Nutz DJ, Henning PT, Hollman JH, Smith J. Accuracy of ultrasound-guided versus unguided pes anserinus bursa injections. PM R. 2010;2:732–739. doi: 10.1016/j.pmrj.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 8.Peck E, Lai JK, Pawlina W, Smith J. Accuracy of ultrasound-guided versus palpation-guided acromioclavicular joint injections: A cadaveric study. PM R. 2010;2:817–821. doi: 10.1016/j.pmrj.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Wisniewski SJ, Smith J, Patterson DG, Carmichael SW, Pawlina W. Ultrasound-guided versus nonguided tibiotalar joint and sinus tarsi injections: A cadaveric study. PM R. 2010;2:277–281. doi: 10.1016/j.pmrj.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Curtiss HM, Finnoff JT, Peck E, Hollman J, Muir J, Smith J. Accuracy of ultrasound-guided and palpation-guided knee injections by an experienced and less-experienced injector using a superolateral approach: A cadaveric study. PM R. 2011;3:507–515. doi: 10.1016/j.pmrj.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 11.Muir JJ, Curtiss HM, Hollman J, Smith J, Finnoff JT. The accuracy of ultrasound-guided and palpation-guided peroneal tendon sheath injections. Am J Phys Med Rehabil. 2011;90:564–571. doi: 10.1097/PHM.0b013e31821f6e63. [DOI] [PubMed] [Google Scholar]
- 12.Boon A. Ultrasonography and electrodiagnosis: Are they complementary techniques? PM R. 2013;5:S100–S106. doi: 10.1016/j.pmrj.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 13.Boon AJ, Alsharif KI, Harper CM, Smith J. Ultrasound-guided needle EMG of the diaphragm: Technique description and case report. Muscle Nerve. 2008;38:1623–1626. doi: 10.1002/mus.21187. [DOI] [PubMed] [Google Scholar]
- 14.Sarwal A, Cartwright MS, Mitchell E, Williams K, Walker FO, Childers MK. Guiding intramuscular diaphragm injections using real-time ultrasound and electromyography. Muscle Nerve. 2015;51:287–289. doi: 10.1002/mus.24493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gazzillo GP, Finnoff JT, Hall MM, Sayeed YA, Smith J. Accuracy of palpating the long head of the biceps tendon: An ultrasonographic study. PM R. 2011;3:1035–1040. doi: 10.1016/j.pmrj.2011.02.022. [DOI] [PubMed] [Google Scholar]
- 16.Rho ME, Chu SK, Yang A, Hameed F, Lin CY, Hurh PJ. Resident accuracy of joint line palpation using ultrasound verification. PM R. 2014;6:920–925. doi: 10.1016/j.pmrj.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Smith J, Finnoff JT. Diagnostic and interventional musculoskeletal ultrasound: Part 1. Fundamentals PM R. 2009;1:64–75. doi: 10.1016/j.pmrj.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Henzel MK, Munin MC, Niyonkuru C, Skidmore ER, Weber DJ, Zafonte RD. Comparison of surface and ultrasound localization to identify forearm flexor muscles for botulinum toxin injections. PM R. 2010;2:642–646. doi: 10.1016/j.pmrj.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pillen S, Arts IM, Zwarts MJ. Muscle ultrasound in neuromuscular disorders. Muscle Nerve. 2008;37:679–693. doi: 10.1002/mus.21015. [DOI] [PubMed] [Google Scholar]
- 20.Engel WK, Askanas V. Inclusion-body myositis: Clinical, diagnostic, and pathologic aspects. Neurology. 2006;66:S20–S29. doi: 10.1212/01.wnl.0000192260.33106.bb. [DOI] [PubMed] [Google Scholar]
- 21.Noto Y, Shiga K, Tsuji Y, et al. Contrasting echogenicity in flexor digitorum profundus-flexor carpi ulnaris: A diagnostic ultrasound pattern in sporadic inclusion body myositis. Muscle Nerve. 2014;49:745–748. doi: 10.1002/mus.24056. [DOI] [PubMed] [Google Scholar]
- 22.Hammoudi N, Arangalage D, Boubrit L, et al. Ultrasound-based teaching of cardiac anatomy and physiology to undergraduate medical students. Arch Cardiovasc Dis. 2013;106:487–491. doi: 10.1016/j.acvd.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Dreher SM, DePhilip R, Bahner D. Ultrasound exposure during gross anatomy. J Emerg Med. 2014;46:231–240. doi: 10.1016/j.jemermed.2013.08.028. [DOI] [PubMed] [Google Scholar]