Abstract
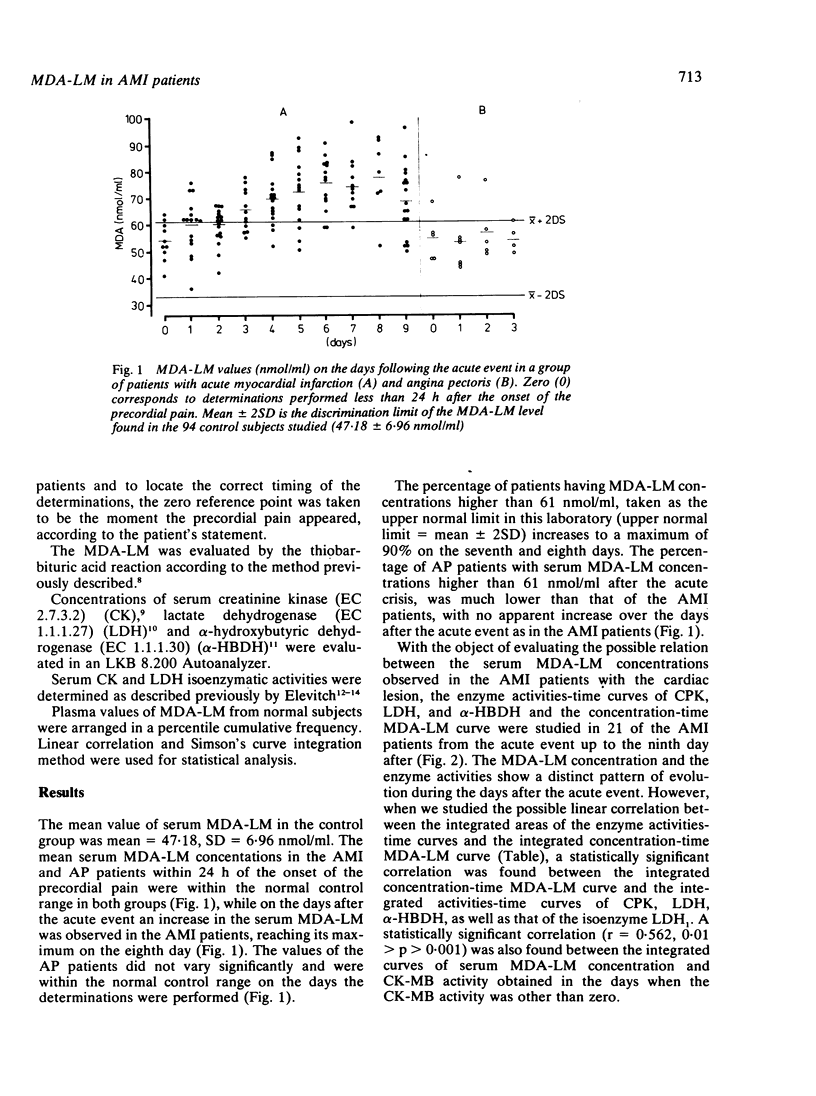
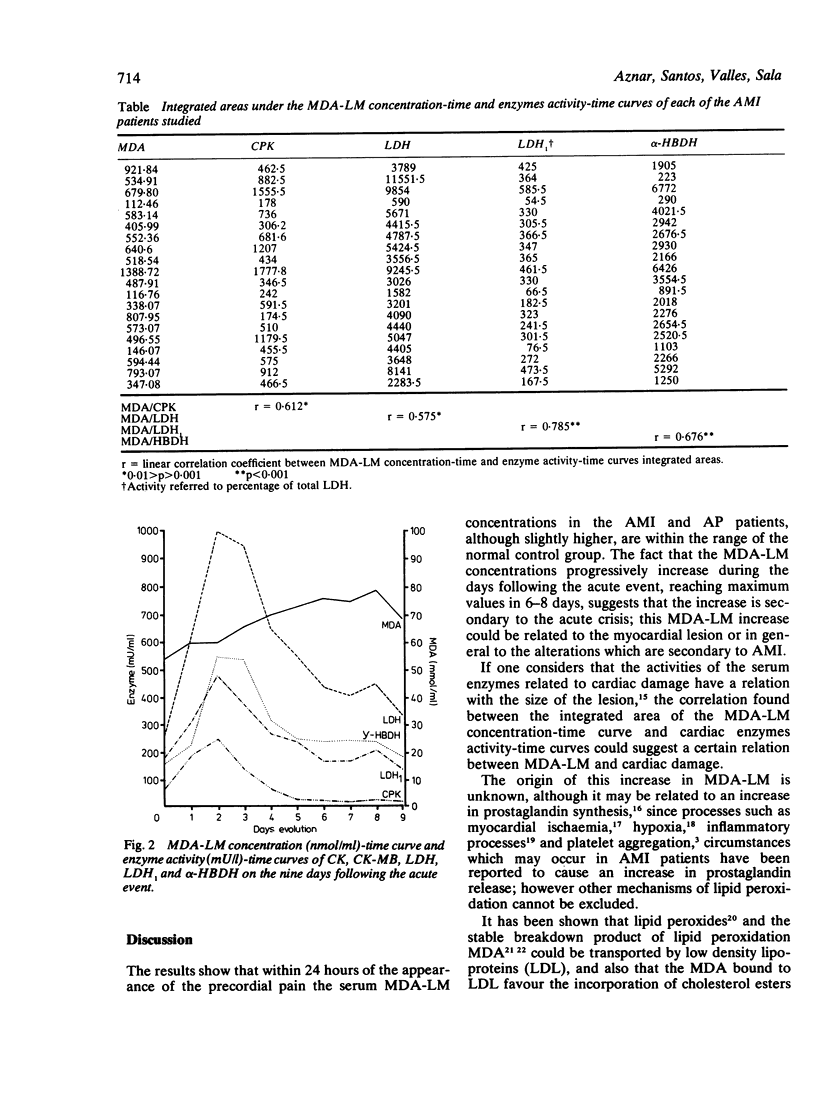
Serum malondialdehyde-like material (MDA-LM), as an index of lipid peroxidation, and the serum enzymes CK, CK-MB, LDH, LDH1 and, alpha-HBDH were evaluated in a group of 26 patients with acute myocardial infarction (AMI), seven with angina pectoris (AP), and in a normal control group of 94 subjects. MDA-LM values were within the normal range in AP patients, while in AMI patients a significant increase in serum MDA-LM was observed in the days following the acute event, reaching a maximum 6-8 days later, when 90% of the patients had values higher than the upper normal limit (mean +/- 2SD) of the control group. A significant correlation was found between the integrated concentration-time MDA-LM curve and the integrated serum enzymes activity curves reached during the nine days after the acute event. The "in vivo" relevance of the increased serum MDA-LM in the post-infarct period is unknown at the present, but as lipid peroxides are known to harm cellular structures and to inhibit prostacyclin synthesis, it may be of interest with regard to the long term secondary effects in AMI patients.
Full text
PDF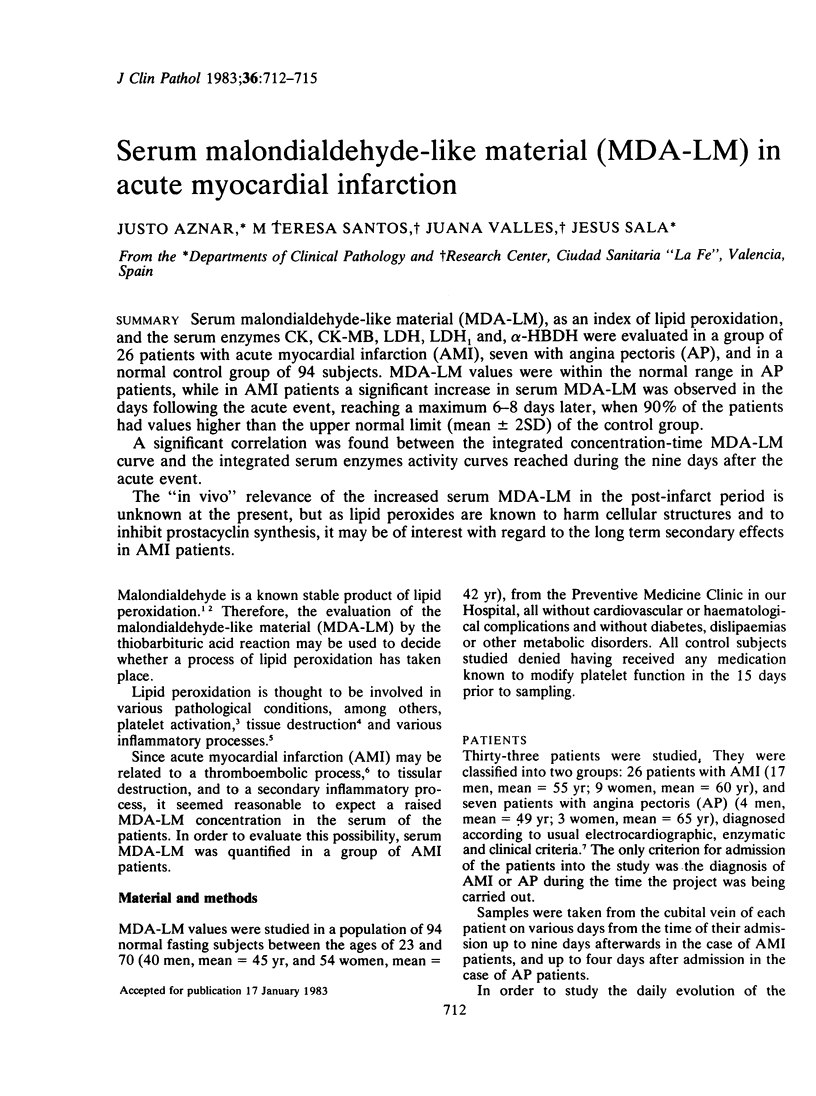
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berger H. J., Zaret B. L., Speroff L., Cohen L. S., Wolfson S. Cardiac prostaglandin release during myocardial ischemia induced by atrial pacing in patients with coronary artery disease. Am J Cardiol. 1977 Apr;39(4):481–486. doi: 10.1016/s0002-9149(77)80154-9. [DOI] [PubMed] [Google Scholar]
- Bragt P. C., Bansberg J. I., Bonta I. L. Antiinflammatory effects of free radical scavengers and antioxidants: further support for proinflammatory roles of endogenous hydrogen peroxide and lipid peroxides. Inflammation. 1980 Sep;4(3):289–299. doi: 10.1007/BF00915030. [DOI] [PubMed] [Google Scholar]
- Brown M. S., Basu S. K., Falck J. R., Ho Y. K., Goldstein J. L. The scavenger cell pathway for lipoprotein degradation: specificity of the binding site that mediates the uptake of negatively-charged LDL by macrophages. J Supramol Struct. 1980;13(1):67–81. doi: 10.1002/jss.400130107. [DOI] [PubMed] [Google Scholar]
- Flamm E. S., Demopoulos H. B., Seligman M. L., Poser R. G., Ransohoff J. Free radicals in cerebral ischemia. Stroke. 1978 Sep-Oct;9(5):445–447. doi: 10.1161/01.str.9.5.445. [DOI] [PubMed] [Google Scholar]
- Fogelman A. M., Shechter I., Seager J., Hokom M., Child J. S., Edwards P. A. Malondialdehyde alteration of low density lipoproteins leads to cholesteryl ester accumulation in human monocyte-macrophages. Proc Natl Acad Sci U S A. 1980 Apr;77(4):2214–2218. doi: 10.1073/pnas.77.4.2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryglewski R. J. Prostaglandins, platelets, and atherosclerosis. CRC Crit Rev Biochem. 1980;7(4):291–338. doi: 10.3109/10409238009105464. [DOI] [PubMed] [Google Scholar]
- Kontos H. A., Wei E. P., Povlishock J. T., Dietrich W. D., Magiera C. J., Ellis E. F. Cerebral arteriolar damage by arachidonic acid and prostaglandin G2. Science. 1980 Sep 12;209(4462):1242–1245. doi: 10.1126/science.7403881. [DOI] [PubMed] [Google Scholar]
- Kuehl F. A., Jr, Humes J. L., Egan R. W., Ham E. A., Beveridge G. C., Van Arman C. G. Role of prostaglandin endoperoxide PGG2 in inflammatory processes. Nature. 1977 Jan 13;265(5590):170–173. doi: 10.1038/265170a0. [DOI] [PubMed] [Google Scholar]
- Placer Z. A., Cushman L. L., Johnson B. C. Estimation of product of lipid peroxidation (malonyl dialdehyde) in biochemical systems. Anal Biochem. 1966 Aug;16(2):359–364. doi: 10.1016/0003-2697(66)90167-9. [DOI] [PubMed] [Google Scholar]
- ROSALKI S. B., WILKINSON J. H. Reduction of alpha-ketobutyrate by human serum. Nature. 1960 Dec 24;188:1110–1111. doi: 10.1038/1881110a0. [DOI] [PubMed] [Google Scholar]
- Santos M. T., Valles J., Aznar J., Vilches J. Determination of plasma malondialdehyde-like material and its clinical application in stroke patients. J Clin Pathol. 1980 Oct;33(10):973–976. doi: 10.1136/jcp.33.10.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu T., Kondo K., Hayaishi O. Role of prostaglandin endoperoxides in the serum thiobarbituric acid reaction. Arch Biochem Biophys. 1981 Feb;206(2):271–276. doi: 10.1016/0003-9861(81)90091-6. [DOI] [PubMed] [Google Scholar]
- Smith J. B., Ingerman C. M., Silver M. J. Malondialdehyde formation as an indicator of prostaglandin production by human platelets. J Lab Clin Med. 1976 Jul;88(1):167–172. [PubMed] [Google Scholar]
- Szczeklik A., Gryglewski R. J., Domagała B., Zmuda A., Hartwich J., Woźny E., Grzywacz M., Madej J., Gryglewska T. Serum lipoproteins, lipid peroxides and prostacyclin biosynthesis in patients with coronary heart disease. Prostaglandins. 1981 Nov;22(5):795–807. doi: 10.1016/0090-6980(81)90219-7. [DOI] [PubMed] [Google Scholar]
- Tappel A. L. Lipid peroxidation damage to cell components. Fed Proc. 1973 Aug;32(8):1870–1874. [PubMed] [Google Scholar]
- WROBLEWSKI F., LADUE J. S. Lactic dehydrogenase activity in blood. Proc Soc Exp Biol Med. 1955 Oct;90(1):210–213. doi: 10.3181/00379727-90-21985. [DOI] [PubMed] [Google Scholar]
- Wennmalm A., Pham-Huu-Chanh, Junstad S. Hypoxia causes prostaglandin release from perfused rabbit hearts. Acta Physiol Scand. 1974 May;91(1):133–135. doi: 10.1111/j.1748-1716.1974.tb05666.x. [DOI] [PubMed] [Google Scholar]
- Witteveen S. A., Hemker H. C., Hollaar L., Hermens W. T. Quantitation of infarct size in man by means of plasma enzyme levels. Br Heart J. 1975 Aug;37(8):795–803. doi: 10.1136/hrt.37.8.795. [DOI] [PMC free article] [PubMed] [Google Scholar]



