Abstract
Objective
As commonly seen symptoms, headaches are among the most frequently encountered health challenges in emergency rooms by healthcare professionals. Among one of the most commonly seen and primary headaches is migraine. Migraines are mostly accompanied by functional deficits.
Aims
To observe the changes of neutrophil/lymphocyte ratio occurring during migraine attacks.
Method
This is a retrospective study where hospital records of patients previously diagnosed with migraine and admitted to the emergency with the complaints of attacks between May 2014 and January 2015 were investigated. All patients in the study were evaluated as to age, gender and complete blood count. Additionally, a healthy control group was formed with individuals with no disorders. By also evaluating the same features in the controls, the values found in the patients and controls alike were compared.
Results
The values of white blood cell, lymphocyte, neutrophil, hemoglobin, thrombocyte and neutrophil/lymphocyte ratio determined in the patient group (n = 92) were statistically compared with those of the controls (n = 67). Neutrophil/lymphocyte ratio during the attacks was found higher in the patients, compared to the controls.
Conclusion
Neutrophil/lymphocyte ratio is a sign of inflammation, and we consider that this ratio will also increase during migraine attacks, as with other inflammatory and acute processes.
Keywords: Headaches, Migraine, Neutrophil/lymphocyte ratio, Inflammation
Highlights
-
•
A migraine headache is a frequent reason for emergency departments.
-
•
During migraine attacks it is not fully understood that there is an inflammatory process.
-
•
We think that the role of inflamation during attack.
-
•
We think that this inflamation process increases the severity of the pain.
1. Introduction
Headaches are among the most commonly encountered complaints in the emergency. Nearly one million cases are admitted to the emergency rooms with the complaint of headaches in the United States each year, and the admissions due to headaches to the emergency constitute more than 4% of all emergency admissions [1]. As a general approach, headaches can be grouped into two as primary headaches, such as migraines where no underlying cause can be defined, and secondary or organic headaches, like subarachnoid hemorrhagies, led by an underlying reason [2].
The most common of the conditions affecting individuals is headaches. As well as neurological disorders, headache is a symptom accompanied by cardiovascular disorders, hypertension and gastrointestinal system diseases, and systemic diseases, such as otolaryngeal problems, eye defects and psychiatric disorders. Almost all individuals experience headaches during lifetimes. Headache is one of the most frequently seen symptoms in adolescency and adulthood. Most of the patients with headaches are admitted to the emergency rooms due to primary headache syndrome, and become amolierated with rapid and effective treatment modalities. Secondary headaches are seen in 3.8% of all patients admitted to the emergency rooms [3].
The existence of moderate or severe headache affecting routine activities is one of the diagnostic criteria of migraine and observed in nearly 70% of the patients [4]. Migraine is classically seen as throbbing and one-sided headaches; however, it is unlikely to distinguish migraine from other types of headaches through the characteristics and site of the pain. So, accompanying symptoms and signs are required to be known. Such symptoms as photophobia, phonophobia, nausea (90%), anorexia (75%), vomitting (60%) and diarrhea (15%) are common symptoms observed in patients with migraine. Constitutional alterations, such as personal changes before and after the pain, exhausting, fatique, myalgia, bulimia and irritability, and neurological symptoms, like aura or visual phonemena, are also observed in migrane patients. Although less frequently, motor deficits, including hemiparesis, ophtalmoplegia and aphasia, emotional disorders and brainstem findings, such as vertigo and ataxia, may be seen during aura [5].
During attacks, migraine sufferers are known either to give a break to their jobs at work sites or go home. Therefore, migraine leads to a decrease or loss of productivity in organizations. The World Health Organization (WHO) has been defined the condition as a disability restricting or preventing individuals from performing their daily activities [6]. Many different mechanisms are considered to be responsible for the pathogenesis of migraine. Although it is known that an association exists between hematologic disorders such as anemia and polycythemia, and headaches, the number of studies where the relationships between features of headaches such as frequency, severity or duration and hematologic parameters are investigated is limited [7].
Upon evaluating oxidative stress, the pathophysiology of vessels and inflammation markers in migraine patients, it was concluded that deficient and decreasing antioxidant levels in patients increase oxidative stress, and thus leading to inflammation and changes in the pathophysiology of vessels. Shown among the primary headaches under the criteria defined by the International Headache Association (IHA), migraine is generally described as a neurovascular disorder where neurogenic inflammation, contractile dysfunction of cranial blood vessels and depression mechanisms starting from cerebral cortex and extending other organs play a role. In various studies, it is reported that neurinflammatory conditions, cytokines, different neuropeptides and vasomotor changes are responsible for the pathogenesis of migraine. Vasoactive peptides forming as a result of trigeminal nerve stimulation with the initiation of migraine attacks lead blood flow to increase, protein to leak out of vessels and a neurogenic inloammation to take place. So, sterile inflammation plays a part in the pathogenesis of migraines [8].
The response to stress by leucocytes in circulation causes an increase in the number of neutrophils and a decrease in the number of lymphocytes. Hence, the proportion of these two subgroups to each other is used as a marker of inflammation [9]. Recently started to be used, neutrophil/lymphocyte ratio (NLR) is a cheap and useful marker that can easily be calculated from complete blood count (CBC). As a subclinical inflammatory marker, NLR is associated with the prognosis and mortality of many diseases [10], [11].
In light of literature, we aimed here at observing the changes of NLR, known as a significant inflammatory marker occurring during migraine attacks.
2. Material and method
In this study, 92 patients previously diagnosed with migraine and admitted to the Emergency Department of Konya Training and Research Hospital, Baskent University with the complaint of new headache attacks between May 2014 and January 2015 were retrospectively evaluated. Among our subjects, those using analgesic drugs, exposed to blood transfusion or other blood products, with uncontrolled hypertension, intracranial space-occupying lesion, treated due to anemia or polycythemia within the last one year, and those with the history of hemorrhages or an operation during the last six months, hematologic disorders, chronic kidney or liver diseases, the history of pregnancy or fever in the last one month and any other disorders such as oncologic diseases, iron deficiency anemia, thalasemia, a metabolic disorder and anti-inflammatory bowel disease were excluded out of the study. A total of 45 patients with neurologic deficits, vertigo and any chronic disorder, along with migraine attacks, were also excluded out of the criteria. In short, those with no other complaints rather than migraine-type headaches were included into the study.
In order to investigate complete blood count (CBC), blood samples were drawn from 92 patients admitted to the emergency with the complaints of migraine attacks. The values of white bloodcell count (WBC), neutrophil, lymphocyte, hemoglobin and thrombocyte of all patients were recorded, and patients were referred to the clinic to be treated. Standard symptomatic treatment was commenced as a modality. In addition, for comparisons, a control group was formed from 67 healthy volunteers admitted to the check-up clinic due to their check-ups. By informing all participants on study design, written consent forms were obtained from all participants to investigate CBC samples. Blood samples were drawn with the reference amount defined in routin CBC kit. As well as age and gender, the values of leucocytes (WBC), neutrophil, lymphocyte, hemoglobin, thrombocyte and NLR of all patients were compared. While a group of patients were discharged because their complaints were improved in the emergency, another group was hospitalized and followed-up in the neurology department due to the fact that no reggression was observed in complaints while observing in the emergency room.
3. Laboratory analysis
To perform the investigation of CBC samples, routine electronic CBC device was used (Cell-Dyne 3700, Abbott, Abbott Park, IL, USA).
4. Statistical analysis
Collected data were recorded into previously prepared forms, and the statistical analyses were performed with SPSS 18.0 software package. The analyses of appropriateness for the data showing normal distribution were carried out with the Shapiron Willing Test. For comparisons between both groups, the student's t-test was used. Numeric values were reported as mean ± standartd deviation (SD). p < 0.05 was accepted as significant.
5. Results
The study was performed in the emergency department of Konya Training and Research Hospital of Baskent University between May 2014 and January 2015. A total of 92 patients admited to the emergency room with the complaint of headache with previous migraine complaints were included into the study. While 92 patients in the study were composed of 68 women (73.9%) and 24 men (24.1%), 35 (52.2%) of 67 healthy controls were composed of women. Mean age rates were detected as 41.13 ± 12.9 and 42.07 ± 11.2 in the patient and control groups, and no difference was detected between both groups as to mean age rates (p = 0.05) (Table 1).
Table 1.
Demographic features of patients and control groups, and laboratory findings.
| Migrain (n = 92) | Control (n = 67) | P value | |
|---|---|---|---|
| Gender (M/F) | 24/68 | 32/35 | |
| Age* | 41,13 ± 1,.9 | 42,07 ± 11,2 | 0.05 |
| WBC (x103/mm3)* | 7,95 ± 2,21 | 7,11 ± 1,71 | 0.008 |
| Neutrophil (x103/mm3)* | 5,10 ± 1,74 | 4,47 ± 1,12 | 0.005 |
| Lymphocyte (x103/mm3)* | 2,21 ± 0,59 | 2,97 ± 0,88 | <0.001 |
| N/L | 2,44 ± 0,86 | 1,55 ± 0,37 | <0.001 |
| Hemoglobin (mg/dL)* | 13,38 ± 1,44 | 13,11 ± 0,88 | 0.16 |
| Platelet (x103/mm3)* | 290,14 ± 70,06 | 220,01 ± 65,38 | 0.028 |
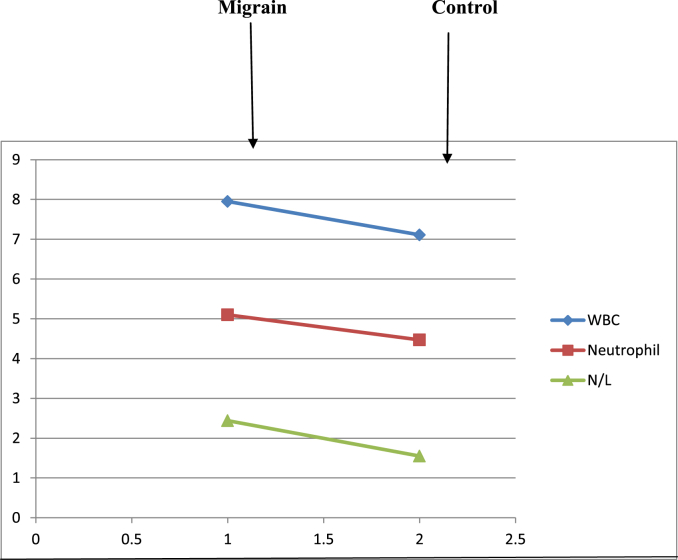
While mean WBC rate was found as 7.95 ± 2.21 in the patients, the rate in the controls was determined as 7.11 ± 1.71. Compared WBC values of both groups, the rate was found higher in the patients, and the difference was accepted as statistically significant (p = 0.008). When compared neutrophil values of two groups, mean number of neutrophils in the patient group was observed to be higher, and the difference was accepted as significant (p = 0.005). When we compared lymphocyte values between two groups, we saw that mean rate of lymphocytes in the controls was higher, and the difference was statistically significant (p < 0.001). NLR was investigated in two groups, and it was detected that while mean N/LR of the patients were 2.44 ± 0.86, the mean rate was found as 1.55 ± 0.37 in the controls. As to N/LR, a statistically significant difference was determined between two groups (p < 0.001). When we compared hemoglobin values between two groups, no statistical difference was detected between two groups (p = 0.16). However, compared thrombocyte values between two groups, the rate was found higher in the patient group, and the difference was accepted as significant (p = 0.028) (Fig. 1).
Fig. 1.
Comparisons of white blood counts, neutrophil and neutrophil/lymphocyte ratio between patient and control groups.
When the correlations between values detected in the patient group were investigated, a strong correlation was seen to be present between the rates of WBC and neutrophils (r = 0.87, p < 0.001). Also, neutrophils were strongly correlated with N/LR (r = 0.56, p < 0.001), as well as the strong correlation detected between WBC and lymphocytes (r = 0.50, p < 0.001). However, a weak correlation was determined between WBC and N/LR (r = 0.34, p = 0.001).
6. Discussion
Migraine is accepted as a neuromuscular control disorder with hereditary transition and paroxismal quality involving cranial vessels [12]. While migraine attacks show no significant gender difference in childhood period, the frequency of encountering migraine increases in women after puberty, and the frequency rate in society is two fold higher among women, compared to men in adulthood. In Turkish society, age segment where migraine is encountered at most was found as 30–39 years of age, as consistent with the findings found in western countries. The gap between both genders rises to three or fourfold higher in women. The fact that migraine attacks are seen more commonly in women may be related to menstrual cycle; however, migraine attacks are known to decrease increasingly as pregnancy advances. That the frequency of migraine alters in some women using oral contraceptives indicates obviously the role of women's sex hormones in the pathophysiology of migraine [13]. In the study investigating the epidemiology of headache in Turkey, the prevalance of migraine was found as 16.4% in individuals between the ages of 15–55, and the rate was defined as 21.8% for women and 10.9% for men [14]. In our study, mean age of patients was 41.13 ± 12.9, and of these, 73.9% were women while 26.1% were men, as consistent with the findings in literature.
There are several studies investigating migraine attacks in periods with and without aura. Many researchers found an increase in thrombocyte activation and thrombocyte aggregation in migraine patients. In a study, Zeller et al. found the increase of thrombocyte activation and the formation of leucocyte-thrombocyte aggregation by measuring P-selectin expression on thrombocytes, especially in migraine patients without aura during non-attack period, compared to healthy controls [15]. Also, in another study, Varol et al. determined that thrombocyte count was lower in migraine patients, compared to healthy controls, but average thrombocyte volume was higher [16]. In our study, however, thrombocyte count was found to be higher in the patients.
Iron in metabolism may increase the frequency of headaches in patients with headache by decreasing the pain threshold via different mechanisms, such as nitric oxide, inflammatory mediators and neurotransmitters. In the study investigating the same entity and performed by Admont et al., the frequency of headaches was detected to decrease in cases with hemoglobin levels lower than 11.5. Interestingly, no association was determined between ferritine levels and the prevalance of headaches [17]. However, hemoglobin levels were within normal limits in the patient group, and no difference was detected between both groups.
In a study, levels of C-reactive protein (CRP) was detected to be higher in patients admitted with the complaint of migraine attacks, compared to the controls [18], [19]. Recurrency of perivascular inflammation during migraine attacks also increases the risk of stroke in migraneurs [20]. In another study, oxidative stress factors and inflammation were determined to be effective on migraine-type headaches [21]. Another study also suggested that meningeal inflammation could play a role in the frequency of migraine attacks and headaches [22].
As a result of a series of experiments, Moskowitz et al. obtained results suggesting that migraine pain is a type of sterile inflammation [23]. In a study by Waeber et al., it was reported that ions, free radicals, complement system, kinines and cytokines are important in the inflammatory process [24]. Turan et al. determined that procalcitonin increases as a marker of inflammation during migraine attacks [25].
For the first time, Zahorec determined an association between neutrophiles and lmyphocytes during the systemic inflammatory response [9]. Neutrophiles, lymphocytes and other white blood cells are the primary sources of proinflammatory and anti-inflammatory cells [26]. Neutrophiles are the most significant cells leading to inflammatory response in acute phase reactions. Lymphocytes are the major components of both humoral and cellular responses [27], [28]. NLR is produced from neutrophiles and lmyphocytes in the circulation and is of a vital importance due to the association with inflammation. NLR has drawn the attention of medical workers in recent times due to its non-invasive measurement, easy determination from peripheric blood and cost-effective features [29].
In migraine models today, presence of neurogenic inflammation is shown and triptans which are effective therapeutic drugs are used to block neurogenic inflammation [30]. Moskowitz and Cutrer's [23] findings suggest that migraine develops as a result of the development of a neurogenic inflammatory reaction. Turan et al. determined that inflammation markers elevate increase as a marker of inflammation during migraine attacks [25].
In our study, which is a marker of inflammation NLR; it was detected high during an attack.
7. Conclusions
Here, we aimed at observing the changes of N/LR occurring during acute pain in migraine patients, and we saw that along with other inflammation markers, NLR is also affected during inflammatory process, especially during migraine attacks with aura. Additionally, we detected NLR to be higher in patients experiencing migraine attacks, compared to the controls. We reached no studies investigating NLR changes during migraine attacks. So, we consider that further studies with larger samples will be useful to enlighten the entity.
8. Limitations
The most important limitation of our study is that it was performed in a short period, and the low number of patients were enrolled. Additionally, the fact that the study was performed in an emergency room was another limitation because of short follow-up period and no follow-up of administered drugs.
Ethical approval
Ethical approval was not received due to This study is retrospective.
Source of funding
None.
Author contribution
Keziban Ucar Karabulut – Study design, study execution, data collation.
Tomris Ugur Egercioglu – Data collation, data analysis, manuscript drafting, manuscript editing, manuscript submission, de facto correspondences, Mehmet Uyar – Software design, software programming Yildiz Ucar – Software design, software programming, Study design, study execution.
Conflict of interest
The authors reported no conflict of interest related to this article.
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Research registration unique identifying number (UIN)
Research Registry 1219.
Contributor Information
Keziban Ucar Karabulut, Email: dr_kezi@hotmail.com.
Tomris Ugur Egercioglu, Email: durubatu@gmail.com.
Mehmet Uyar, Email: mehmetuyardr@hotmail.com.
Yildiz Ucar, Email: yildiz-ucar@hotmail.com.
References
- 1.Ang Seng Hock, Chan Yee Cheun, Mahadevan Malcolm. Emergency department headache admissions in an acute care hospital: why do they occur and what can we do about it? Ann. Acad. Med. Singap. 2009;38:1007–1010. [PubMed] [Google Scholar]
- 2.Headache Classification Commitee of the International Headache Society 2003 The international classification of headache disorders. Cephalalgia. 2004;24(1) [Google Scholar]
- 3.Henry G.L. Headache. In: Rosen P., Barkin M.R., editors. Emergency Medicine Consepts and Clinical Practice. fourth ed. Mosby-Year Book; St.Louis: 1998. pp. 2119–2131. [Google Scholar]
- 4.D'Amico D., Usai S., Grazzi L. Disability and migraine: MDAS. J. Headache Pain. 2001;2:25–27. [Google Scholar]
- 5.Rosen P., Barkin R.M., Hayden S.R., Schaider J., editors. Wolfe R.the 5 Minutes Emergency Medicine Consult. Lippincott Williams & Wilkins; Philedelphia: 1999. Headache; pp. 476–477. [Google Scholar]
- 6.Bussone G., Grazzi L., Usai S. Disability in migraine patients Italian experience. J. Headache Pain. 2001;2:29–31. [Google Scholar]
- 7.Welch K.M.A., Nagesh V., Aurora S.K., Gelman N. Periaqueductal gray matter dysfunction in migraine. Cause or burden of illness? Headache. 2001;41:629–637. doi: 10.1046/j.1526-4610.2001.041007629.x. [DOI] [PubMed] [Google Scholar]
- 8.Vanmolkot F.H., de Hoon J.H. Increased C-reactive protein in young adult patients with migraine. Cephalalgia. 2007;27:843–846. doi: 10.1111/j.1468-2982.2007.01324.x. [DOI] [PubMed] [Google Scholar]
- 9.Zahorec R. Ratio of neutrophil to lymphocyte counts—Rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl. Lek. Listy. 2001;102:5–14. [PubMed] [Google Scholar]
- 10.Gomez D., Farid S., Malik H.Z., Young A.L., Lodge J.P., Prasad K.R. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J. Surg. 2008;32(8):1757–1762. doi: 10.1007/s00268-008-9552-6. [DOI] [PubMed] [Google Scholar]
- 11.Azab B., Bhatt V.R., Phookan J., Murukutla S., Kohn N., Widmann W.D. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann. Surg. Oncol. 2012;19(1):217–224. doi: 10.1245/s10434-011-1814-0. [DOI] [PubMed] [Google Scholar]
- 12.Celentano D.P., Stewart W.F., Linet M.S. The relationship of headache symptoms with severety and duration of attacks. J. Clin. Epidemiol. 1990;43:983–999. doi: 10.1016/0895-4356(90)90082-z. [DOI] [PubMed] [Google Scholar]
- 13.Özge A., Buğdaycı R., Şaşmaz T., Kaleağası H., Kurt Ö., Karakelle A., Tezcan H., Siva A. The Sensitivity and specificity of the case definition criteria in diagnosis of headache. Cephalgia. 2002;22:791–798. doi: 10.1046/j.1468-2982.2002.00467.x. [DOI] [PubMed] [Google Scholar]
- 14.Hayran O., Zarifoglu M., Siva A. Başağrısı epidemiyolojisi. In: Erdine S., editor. Ağrı. 2000. pp. 181–183. [Google Scholar]
- 15.Zeller J.A., Lindner V., Frahm K., Baron R., Deuschl G. Platelet activation and platelet-leucocyte interaction in patients with migraine. Subtype differences and influence of triptans. Cephalalgia. 2005;25:536–541. doi: 10.1111/j.1468-2982.2005.00916.x. [DOI] [PubMed] [Google Scholar]
- 16.Varol Sefer, Akıl Esref, Ugur Mehmet. Investigation of mean platelet volume and platelet count in the blood of patients with migraine. Turk. J. Neurol. 2013;19:3. [Google Scholar]
- 17.Admont A.H., Borch-Iohnsen B., Hagen K., Stovner L.J., Asberg A., Zwart J.-A. Headache prevalence related to haemoglobin and ferritin. Cephalalgia. 2004;24:758–762. doi: 10.1111/j.1468-2982.2004.00756.x. [DOI] [PubMed] [Google Scholar]
- 18.Vanmolkot F.H., de Hoon J.H. Increased C-reactive protein in young adult patients with migraine. Cephalalgia. 2007;27:843–846. doi: 10.1111/j.1468-2982.2007.01324.x. [DOI] [PubMed] [Google Scholar]
- 19.Gudmundsson L.S., Aspelund T., Scher A.I. C-reactive protein in migraine sufferers similar to that of non-migraineurs: the Reykjavik Study. Cephalalgia. 2009 Dec;29(12):1301–1310. doi: 10.1111/j.1468-2982.2009.01865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Welch KMWelch K.M. Stroke and migraine the spectrum of cause and effect. Funct. Neurol. 2003;18:121–126. [PubMed] [Google Scholar]
- 21.da Costa S.C., Passos I.C., Réus G.Z., Carvalho A.F., Soares J.C., Quevedo J. The Comorbidity of bipolar disorder and migraine: the role of inflammation and oxidative and nitrosative stress. Curr. Mol. Med. 2016;16(2):179–186. doi: 10.2174/1566524016666160126144440. [DOI] [PubMed] [Google Scholar]
- 22.Levy D. Migraine pain, meningeal inflammation, and mast cells. Curr. Pain Headache Rep. 2009 Jun;13(3):237–240. doi: 10.1007/s11916-009-0040-y. [DOI] [PubMed] [Google Scholar]
- 23.Moskowitz M.A., Cutrer F.M. Sumatriptan: a receptor-targeted for migraine. Annu. Rev. Med. 1993;44:145–154. doi: 10.1146/annurev.me.44.020193.001045. [DOI] [PubMed] [Google Scholar]
- 24.Waeber C., Moskowitz M.A. Migraine as an inflammatory disorder. Neurology. 2005;64:9–15. doi: 10.1212/wnl.64.10_suppl_2.s9. [DOI] [PubMed] [Google Scholar]
- 25.Turan Hale, Horasanli Bahriye, Ugur Murat, Arslan Hande. Procalcitonin levels in migraine patients. Can. J. Neurol. Sci. 2011;38:124–128. doi: 10.1017/s0317167100011161. [DOI] [PubMed] [Google Scholar]
- 26.de Jager C.P., van Wijk P.T., Mathoera R.B. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit. Care. 2010;14(5):R192. doi: 10.1186/cc9309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ear T., McDonald P.P. Cytokine generation, promoter activation, and oxidant-independent NF-kappaB activation in a transfectable human neutrophilic cellular model. BMC Immunol. 2008;9:14. doi: 10.1186/1471-2172-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robertson C.M., Coopersmith C.M. The systemic inflammatory response syndrome. Microbes Infect. 2006;8(5):1382–1389. doi: 10.1016/j.micinf.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Tanrikulu Yusuf, Sen Tanrikulu Ceren, Zafer Sabuncuoglu Mehmet. Is the neutrophil-to-lymphocyte ratio a potential diagnostic marker for peptic ulcer perforation? A retrospective cohort study. Am. J. Emerg. Med. March 2016;34(3):403–406. doi: 10.1016/j.ajem.2015.11.009. pii: S0735–6757(15)00960-2. [DOI] [PubMed] [Google Scholar]
- 30.Buzzi M.G., Moskowitz M.A. The antimigraine drug, sumatriptan (GR43175) selectively blocks neurogenic plasma extravasation from blood vessels in dura mater. Br. J. Pharmacol. 1990;99:202–206. doi: 10.1111/j.1476-5381.1990.tb14679.x. [DOI] [PMC free article] [PubMed] [Google Scholar]