Abstract
Background
The Benchmark (Penumbra, Alameda, CA) is a novel intracranial guide catheter that provides optimized proximal stability combined with a hyperflexible and atraumatic tip. We assessed the use of a biaxial catheter system consistent with the Benchmark and Marksman microcatheter for placement of a Pipeline embolization device (PED) for intracranial aneurysms.
Methods
We reviewed consecutive patients with aneurysms undergoing Pipeline embolization for an aneurysm using the biaxial system from April to October 2015 at a major academic institution in the United States. Benchmark performance was measured by the number of 90° turns the catheter could safely cross. Landing and final positions of the Benchmark were recorded.
Results
A total of 26 procedures were performed in 25 patients (mean age 59.5 ± 10.3 years; male:female = 1:4). In one case (3.8%) the biaxial system had to be substituted for a traditional triaxial system. The Benchmark was able to cross one, two, or three 90° turns in 48%, 40%, and 8% of cases, respectively. There was one (3.8%) thromboembolic event and no arterial dissections. In the period from January 2014 to March 2015 and prior to adopting the biaxial system we encountered three thromboembolic events (6.4%) and one (2.1%) dissection potentially related to the triaxial system in 47 PED procedures.
Conclusion
Preliminary experience shows that a biaxial system using the Benchmark is a safe and efficacious alternative to the traditional triaxial guide catheter system for placement of PED and may reduce the complexity and duration of the procedure.
Keywords: Catheter, flow diverter, aneurysm, dissection, complication
Introduction
Triaxial catheter systems are traditionally used for placement of Pipeline embolization devices for intracranial aneurysms (PED, Covidien-Ev3, Plymouth, MN) and frequently consist of a Flexor Shuttle sheath (Cook Medical, Bloomington, IN) or a Neuron MAX (Penumbra, Alameda, CA), a Navien distal intracranial catheter (Covidien-Ev3), and microcatheters such as the Marksman (Covidien-Ev3) or the XT-27 (Stryker, Kalamazoo, MI).1–4 Triaxial systems, however, add to the complexity and duration of the procedure. Stagnant blood flow in a triaxial system could result in thrombus formation and a higher rate of thromboembolic complications. Thus, we have recently changed our practice and used a biaxial system consistent with a Benchmark intracranial guide catheter (Penumbra) and a Marksman microcatheter for placement of PED. The purpose of this manuscript was to assess the safety and efficacy of this biaxial approach.
Methods
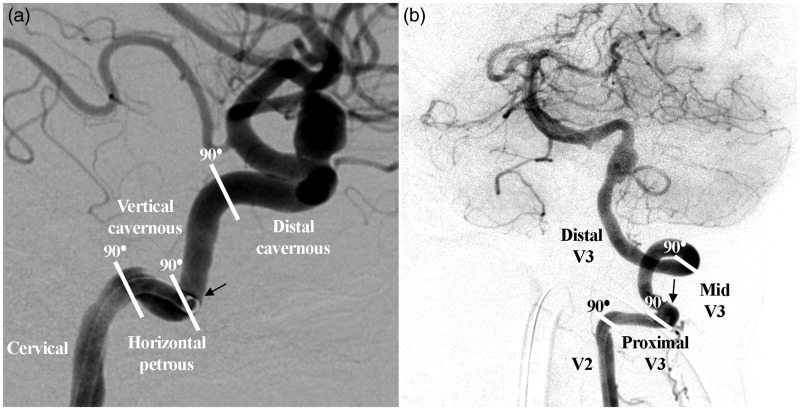
We retrospectively reviewed a prospectively maintained database on consecutive patients with aneurysms undergoing Pipeline embolization for an aneurysm using a biaxial catheter system consistent with a 6F 0.071-inch inner diameter Benchmark intracranial guide catheter and a Marksman microcatheter from April to October 2015 at a major academic institution in the United States. The Benchmark is an advanced polymer construct with 10 material transitions and a hybrid of flat/round metal reinforcement. The design provides optimized proximal stability combined with a hyperflexible and atraumatic tip. Patient demographics, risk factors, aneurysm characteristics, and complications were recorded. Benchmark performance was measured by the number of 90° turns the catheter could safely cross. One point was assigned for each 90° turn the Benchmark crossed in either the cervical or intracranial internal carotid artery (ICA) or vertebral artery (VA) and points were added. Landing and final position of the guide catheter tip in the ICA and VA were graded as following: The ICA was subdivided into cervical, horizontal petrous, vertical cavernous, and distal cavernous segments (Figure 1(a)). The VA was divided into V2, proximal V3, middle V3, and distal V3 segments (Figure 1(b)).5
Figure 1.
Lateral view of the internal carotid artery (a) and anteroposterior view of the vertebral artery (b) illustrating the system used to assess 90° turns and landing and final position. Panel (a) shows the Benchmark intracranial guide catheter landing position in the horizontal petrous segment of the internal carotid artery during Pipeline embolization of a paraophthalmic internal carotid artery segment aneurysm. Panel (b) shows the landing position of the Benchmark in the proximal V3 segment of the vertebral artery during Pipeline embolization of a fusiform aneurysm involving the origin of the posterior inferior cerebellar artery.
Results
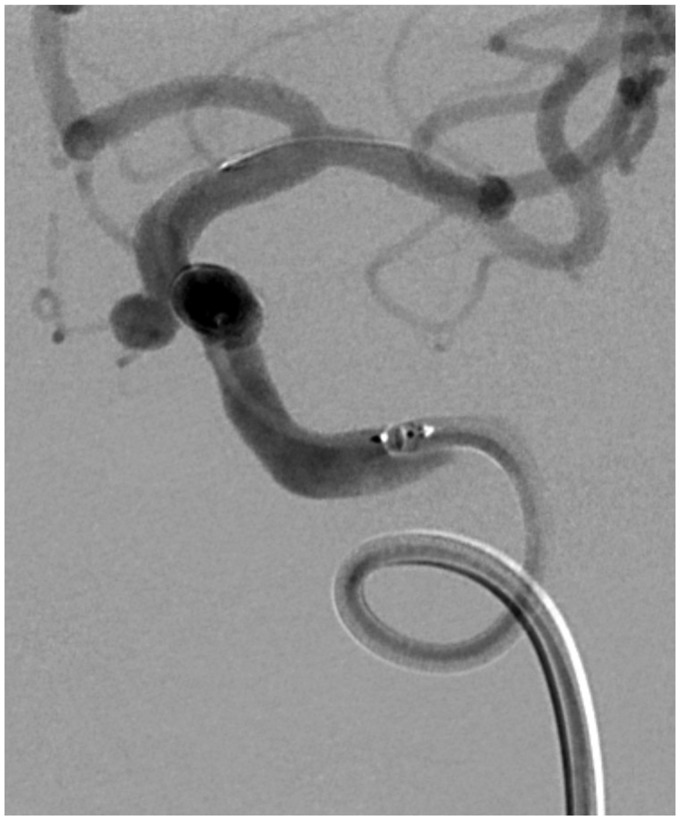
A total of 26 Pipeline embolization procedures were performed in 25 patients (mean age 59.5 ± 10.3 years; male:female = 1:4) between April to October 2015. One (4%) patient had multiple aneurysms. Smoking and hypertension were reported in 32% and 36% of patients, respectively. Eighteen aneurysms (69.2%) were located in the anterior and eight (30.8%) in the posterior circulation. The mean aneurysm size was 7.1 ± 5.6 mm. Morphologically, 80.8% of the aneurysms were saccular with the remainder fusiform or dissecting (Table 1). Adequate PED coverage of the aneurysm neck was achieved in all cases the biaxial catheter system was used. In one case (3.8%) the biaxial system had to be substituted for the traditional triaxial system because of an inability to negotiate the V2 segment of the VA with the Benchmark intracranial guide catheter. The Benchmark was able to cross one 90° turn in 12 (48%) and two 90° turns in 10 (40%) of 25 patients. It crossed three 90° turns in two (8%) patients (Table 2). For interventions in the anterior circulation, the distribution of landing positions in the cervical, horizontal petrous (Figure 2), vertical cavernous, and distal cavernous segments of the ICA was 22.2%, 38.9%, 38.9%, and 0%, respectively. For posterior circulation interventions, distribution landing positions in the V2, proximal V3, middle V3, and distal V3 segments of the VA were 0%, 42.8%, 28.6%, and 28.6%, respectively. Landing and final position of the Benchmark did not change in any of the cases (Table 3). Most Benchmark landing positions were safely achieved over a 0.035 Terumo stiff glidewire (Terumo, Somerset, NJ). When there was severe tortuosity, the Benchmark was parked proximal to the tortuous segment initially. After the Marksman catheter had been passed distal to the tortuous area and sufficient purchase achieved, the Benchmark was guided over the Marksman to its final landing position. There was one (3.8%) thromboembolic event and no arterial dissections. In the period from January 2014 to March 2015 and prior to adopting the biaxial system we encountered three thromboembolic events (6.4%), one (33.3%) clinically symptomatic, and one (2.1%) dissection, potentially related to the triaxial system in 47 PED procedures.
Table 1.
Patient characteristics.
| Number of patients | 25 |
|---|---|
| Number of aneurysms | 26 |
| Patients with multiple aneurysms | |
| Two aneurysms | 1 (4%) |
| Gender | |
| Male | 5 (20%) |
| Female | 20 (80%) |
| Age | 59.5 ± 10.3 years |
| Smoking | 8 (32%) |
| Hypertension | 58 (36%) |
| Size of aneurysm (mm) | 7.1 ± 5.6 |
| Side | |
| Right | 14 (53.8%) |
| Left | 12 (46.2%) |
| Location | |
| PCOM | 4 (15.4%) |
| PO | 14 (53.9%) |
| Cavernous | 1 (3.8%) |
| BA | 3 (11.5%) |
| PICA | 4 (15.4%) |
| Morphology | |
| Saccular | 21 (80.8%) |
| Fusiform/dissecting | 5 (19.2%) |
| Complications of treated aneurysms | |
| Thromboembolic complications | 1 (3.8%) |
| Arterial dissection | 0 (0.0%) |
PCOM: posterior communicating artery; PO: paraophthalmic segment of the internal carotid artery; BA: basilar artery; PICA: posterior inferior cerebellar artery.
Table 2.
Number of 90° turns negotiated by the Benchmark guide catheter.
| Cases | Number | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|---|
| ICA | 18 | 1 (5.6%) | 9 (50%) | 8 (44.4%) | 0 |
| Vertebral | 7 | 0 | 3 (42.8%) | 2 (28.6%) | 2 (28.6%) |
| Total | 25 | 1 (4%) | 12 (48%) | 10 (40%) | 2 (8%) |
ICA: internal carotid artery.
Figure 2.
Anteroposterior view of the internal carotid artery with the Benchmark intracranial guide catheter negotiating 90° turns in the cervical internal carotid artery in a patient undergoing Pipeline embolization of a paraophthalmic internal carotid artery segment aneurysm.
Table 3.
Landing and final position of the Benchmark guide catheter.
| Cervical ICA | Horizontal petrous | Vertical cavernous | Distal cavernous | |
|---|---|---|---|---|
| Anterior circulation (18 cases) | ||||
| Landing position | 4 (22.2%) | 7 (38.9%) | 7 (38.9%) | 0 |
| Final position | 4 (22.2%) | 7 (38.9%) | 7 (38.9%) | 0 |
| V2 segment |
Proximal V3 | Middle V3 | Distal-V3 | |
| Posterior circulation (seven cases) | ||||
| Landing position | 0 | 3 (42.8%) | 2 (28.6%) | 2 (28.6%) |
| Final position | 0 | 3 (42.8%) | 2 (28.6%) | 2 (28.6%) |
ICA: internal carotid artery.
Discussion
Pipeline embolization of intracranial aneurysms is traditionally achieved using a triaxial catheter system.1–4 In an effort to decrease the complexity and duration of the procedure, we have recently changed our practice and preferred a biaxial system consistent with a Benchmark intracranial guide catheter and a Marksman microcatheter for Pipeline embolization of aneurysms. This approach proved to be safe and efficacious in 96.1% of patients. Adequate PED coverage of the aneurysm neck was achieved in all cases the biaxial system was used. In only one case did (3.8%) the biaxial system have to be substituted for a traditional triaxial system because of significant tortuosity of the VA origin and inability to negotiate the V2 segment of the VA with the Benchmark. There were no arterial dissections and only one thromboembolic event (3.8%) thought to be unrelated to the use of the biaxial system. In the period from January 2014 to March 2015 and prior to adopting the biaxial system we encountered three thromboembolic events (6.4%), one (33.3%) clinically symptomatic, and one (2.1%) dissection, potentially related to the triaxial system. To our knowledge this is the first report on the use of a biaxial system for Pipeline embolization of aneurysms.
Safety and efficacy of neuroendovascular procedures are based on the foundation of catheter stability and guide catheter positioning in close proximity to the target. In cases of tortuous and redundant anatomy of the aortic arch and proximal extracranial carotid and vertebral systems and tortuous intracranial anatomy, triaxial systems have proven helpful in achieving that foundation.6 Procedures in which triaxial systems are commonly used aside from aneurysm embolization include embolization of remote pedicles of arteriovenous malformations, thrombectomy for acute ischemic stroke, treatment of intracranial arteriosclerosic stenosis or vasospasm, and aspiration of intracranial venous sinus thrombosis.6,7 Triaxial systems, however, add to the complexity of the procedure and may be associated with embolic complications due to stagnation of blood flow.8 The advent of novel guide catheters designed to provide stability proximally and navigability distally has significantly improved guide catheter access.8–10 In the current study we were able to substitute the triaxial system traditionally used for Pipeline embolization for a biaxial system using the Benchmark. The Benchmark has been shown to provide safe access for a variety of neuroendovascular procedures.5 Chandran et al. showed that the Benchmark safely crossed one, two, and three 90° turns in 19%, 45%, and 21% of cases. No thromboembolic event or arterial dissection occurred related to the Benchmark. We argue that the vertical petrous segment in Chandran et al.’s classification is a misnomer as the vertical segment of the ICA distal to the horizontal petrous segment is a portion of the cavernous ICA. Thus, we used the terms vertical cavernous and distal cavernous instead (Figure 1, Panel (a)). Distal landing positions in the vertical cavernous and distal cavernous ICA, corresponding to vertical petrous and cavernous according to Chandran et al.,5 were reported more frequently than in our experience, presumably due to a need for more distal access in some of the conditions treated in the series reported by Chandran et al.5 As all aneurysms treated with PED in our series were located proximal to the ICA bifurcation or in the proximal vertebrobasilar system, positioning of the guide catheter in the horizontal petrous or vertical cavernous ICA or V3 segment of the VA was sufficient. We also did not encounter any significant catheter reversal regardless of the landing position. In cases in which there was any indication of reversal of the Benchmark with advancement of the microcatheter, gentle forward pressure was applied to stabilize the Benchmark position.
Some limitations include the retrospective design and lack of a true comparison group matched for aneurysm characteristics and access difficulty due to tortuosity. To definitively prove superiority of the biaxial system is challenging. In the period prior to adopting the biaxial system, we encountered a slightly higher rate of thromboembolic events and dissections, potentially related to the traditional triaxial system. Nevertheless, a biaxial system using the Benchmark is a safe and efficacious alternative to the conventional triaxial system used for PED placement.
Conclusion
Preliminary experience shows that a biaxial system using the Benchmark is a safe and efficacious alternative to the traditional triaxial guide catheter system for placement of PED and may reduce the complexity of the procedure.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Rouchaud A, Leclerc O, Benayoun Y, et al. Visual outcomes with flow-diverter stents covering the ophthalmic artery for treatment of internal carotid artery aneurysms. AJNR Am J Neuroradiol 2015; 36: 330–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chalouhi N, Zanaty M, Whiting A, et al. Safety and efficacy of the Pipeline Embolization Device in 100 small intracranial aneurysms. J Neurosurg 2015; 122: 1498–1502. [DOI] [PubMed] [Google Scholar]
- 3.Colby GP, Lin LM, Huang J, et al. Utilization of the Navien distal intracranial catheter in 78 cases of anterior circulation aneurysm treatment with the Pipeline embolization device. J Neurointerventional Surg 2013; 5(Suppl. 3): iii16–iii21. [DOI] [PubMed] [Google Scholar]
- 4.Zanaty M, Chalouhi N, Barros G, et al. Flow-diversion for ophthalmic segment aneurysms. Neurosurgery 2015; 76: 286–289. discussion 289–290. [DOI] [PubMed] [Google Scholar]
- 5.Chandran A, Puthuran M, Eldridge PR, et al. Distal access using hyperflexible atraumatic distal tip with optimized proximal stability of the Benchmark intracranial guide catheter for the treatment of cerebral vascular diseases: A technical note. J Neurointerventional Surg. Epub ahead of print 12 June 2015. DOI: 10.1136/neurintsurg-2015-011788. [DOI] [PMC free article] [PubMed]
- 6.Harrigan M, Deveikis J. General considerations for neurointerventional procedures. In: Harrigan M, Deveikis J. (eds). Handbook of cerebrovascular disease and neurointerventional technique, 2nd ed New York: Humana Press, Springer, 2013, pp. 153. [Google Scholar]
- 7.Spiotta AM, Hussain MS, Sivapatham T, et al. The versatile distal access catheter: The Cleveland Clinic experience. Neurosurgery 2011; 68: 1677–1686. discussion 1686. [DOI] [PubMed] [Google Scholar]
- 8.Turk A, Manzoor MU, Nyberg EM, et al. Initial experience with distal guide catheter placement in the treatment of cerebrovascular disease: Clinical safety and efficacy. J NeuroInterventional Surg 2013; 5: 247–252. [DOI] [PubMed] [Google Scholar]
- 9.Lin LM, Colby GP, Huang J, et al. Ultra-distal large-bore intracranial access using the hyperflexible Navien distal intracranial catheter for the treatment of cerebrovascular pathologies: A technical note. J NeuroInterventional Surg 2014; 6: 301–307. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhary N, Pandey AS, Thompson BG, et al. Utilization of the Neuron 6 French 0.053 inch inner luminal diameter guide catheter for treatment of cerebral vascular pathology: Continued experience with ultra distal access into the cerebral vasculature. J NeuroInterventional Surg 2012; 4: 301–306. [DOI] [PubMed] [Google Scholar]