Abstract
Background
A carotid web can be defined as an endoluminal shelf-like projection often noted at the origin of the internal carotid artery (ICA) just beyond the bifurcation. Diagnosis of a carotid web as an underlying cause of recurrent ischemic stroke is infrequent and easily misdiagnosed as an atheromatous plaque. Surgery has traditionally been used to resect symptomatic lesions while there is no enough evidence supporting medical therapy as the sole management. To our knowledge there is only one report about carotid artery stenting (CAS) as a definite management of carotid web and no previous reports of acute large-vessel occlusions undergoing mechanical thrombectomy in the setting of carotid web as the etiology.
Case report
We report two cases: The first presented with recurrent ischemic stroke in the same arterial territory and the other with an emergent left middle cerebral artery (MCA) occlusion that underwent endovascular mechanical thrombectomy in which initial computed tomographic angiograms (CTA) suggested carotid web etiologies. Following confirmation with digital subtraction angiography (DSA), both patients ultimately underwent endovascular carotid stenting instead of surgical resection for definitive carotid web treatment.
Conclusions
Carotid webs are a rare cause of ischemic stroke in young and middle-aged adults that can readily be identified by CTA. Endovascular management may include emergent mechanical thrombectomy for large-vessel thromboembolic complications, and for definitive treatment with carotid stenting across the carotid web as an alternative to surgical resection and medical management for secondary stroke prevention.
Keywords: Carotid, web, stent, recurrent, stroke
Background
Ischemic stroke in young and middle-aged adults has various etiologies. Carotid web is an underestimated cause of recurrent ischemic stroke and has been described by multiple case reports.1–17 It was first described as a stigma of fibromuscular hyperplasia in 19651 followed by similar reports in 1967 and 1968.2,3 Since then it has been described in the literature using other synonyms such as atypical fibromuscular dysplasia,4,5 atypical fibromuscular hyperplasia,6,7 septal fibromuscular dysplasia,8,9 septa,4,10,11 diaphragms,12,13 pseudo-valvular folds14 and webs.10,15,16,17 In most of the reported cases, the diagnosis of carotid web was based on conventional digital subtraction angiography (DSA) appearance as a translucent linear endoluminal filling defect.
Lenck et al. first reported endovascular stenting as an option for stroke secondary prevention in patients with carotid webs13 while the prior literature suggested management options such as surgical resection1–3,5–9,11,12,14–16 and/or medical treatment including anticoagulation11,13 and antiplatelet therapy.5
Case presentation
Both cases were admitted to our institution in the last two years with history of recurrent stroke confined to a single arterial territory. Both patients had initiated antiplatelet therapy following the initial ischemic event. Ischemic strokes were confirmed by magnetic resonance imaging (MRI) including diffusion-weighted imaging (DWI). Angiographic studies including CTA and contrast-enhanced magnetic resonance angiography (MRA) were conducted. Cervical and intracranial segments of the carotid, vertebral and intracranial arteries were assessed to exclude underlying atherosclerotic disease or vasculopathy. Electrocardiography and transthoracic echocardiography were performed in both cases to exclude a cardioembolic source. Patients’ demographics, clinical presentations, infarction distributions, initial stroke management, and associated comorbidities are summarized in Table 1.
Table 1.
Patients’ demographics, clinical presentations, infarction distributions, initial stroke management, and associated comorbidities.
|
|
Patient 1 |
Patient 2 |
|---|---|---|
| Age / gender | 36/Male | 41/Female |
| Ischemic strokes: | ||
| - Frequency | Twice | Four times |
| - Location | Left parietal lobe | Left basal ganglia and corona radiata |
| - Intracranial occlusion | No | Left MCA mid M1 segment |
| - Management | Medical therapy | Mechanical thrombectomy |
| Associated comorbidities: | ||
| - Cardiovascular disease | Hypertension | No |
| - Atherosclerotic disease | No | No |
| - Vasculopathy | No | No |
| - Others: | No | No |
MCA: middle cerebral artery.
The initial diagnosis of the carotid web in both patients was established by CTA as a noncalcified, shelf-like, hypodense projection at the internal carotid artery (ICA) bulb prior to DSA confirmation, while the contrast-enhanced MRA revealed an irregular noncharacteristic proximal ICA stenosis.
Patient 1 presented with recurrent small-vessel lacunar infarcts confined to the left parietal lobe (Figure 1) within a two-month interval, initially managed conservatively with medical therapy. Patient 2 presented emergently with an acute left middle cerebral artery (MCA) M1 occlusion and ischemic infarction involving lateral left basal ganglia and corona radiata (Figure 2). Noncontrast computed tomography (CT) and emergent MRI studies also demonstrated findings of a chronic left insular cortex infarction. Additional history of two prior left hemispheric strokes with good recovery and reportedly negative workup at an outside hospital was obtained. CTA demonstrated a mid-left MCA M1 segment occlusion that was managed by emergent mechanical thrombectomy under conscious sedation. The M1 segment was recanalized after two passes of the Solitaire FR stent retriever device (EV3, Plymouth, MN, USA) restoring near-complete distal reperfusion (Thrombolysis in Cerebral Ischemia (TICI) score = 2b). The procedure was complicated by a non-flow-limiting iatrogenic dissection of the mid-cervical left ICA.
Figure 1.
(a) Reformatted left oblique CTA demonstrates a focal stenosis at the origin of the left ICA secondary to a shelf-like hypodense projection (white arrow) arising from the posterior wall, raising the possibility of a carotid web or noncalcified atheroma. (b) Left common carotid (CCA) anterior oblique DSA centered over the neck demonstrates a prominent curved triangular ridge on the postero-lateral aspect of the left ICA causing flow stagnation in the carotid bulb (black arrow) consistent with a carotid web. (c) Lateral CCA DSA demonstrates final results after angioplasty and stent deployment with no residual stenosis at the left ICA origin, and redundant contrast at the distal carotid bulb with expected thrombosis and vessel remodeling. (d) Color Doppler images demonstrate patent stent (arrow heads) across the distal CCA and proximal ICA with full color saturation and no residual/recurrent stenosis. CTA: computed tomographic angiogram; ICA: internal carotid artery; DSA: digital subtraction angiography.
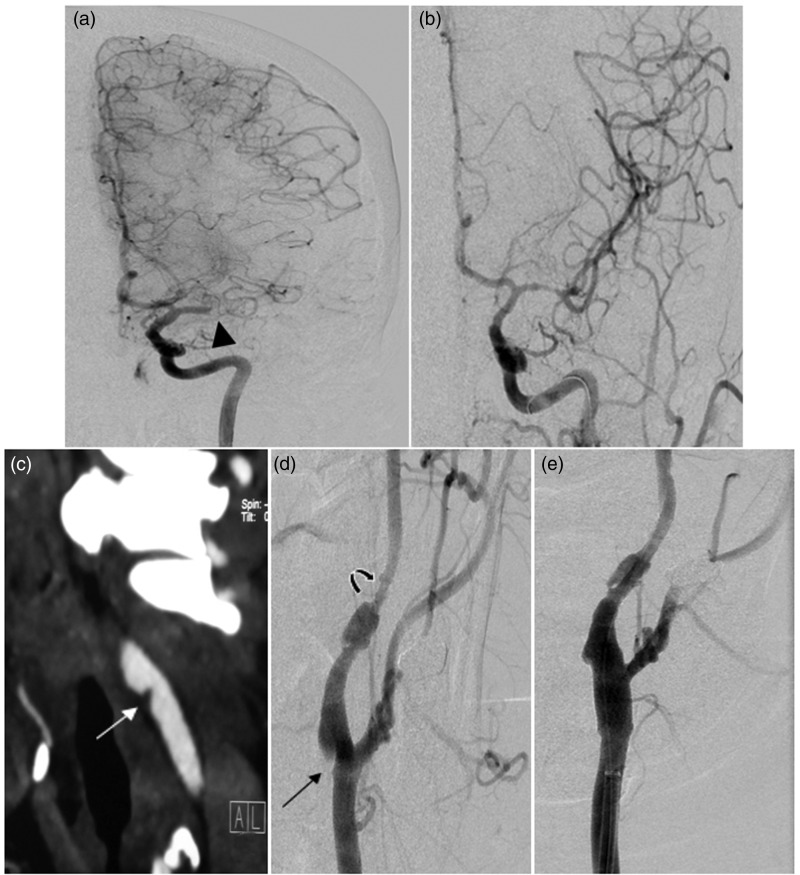
Figure 2.
(a) Anteroposterior (AP) left ICA DSA demonstrates occluded left MCA at the mid-M1 segment (arrow head) with occlusion of the lateral lenticulostriate arteries, but robust collaterals from the left ACA. (b) AP left ICA DSA after mechanical thrombectomy with stent retrieval demonstrates successful recanalization of the left MCA and its inferior division, and slow antegrade flow into the superior division (TICI = 2b). (c) Reformatted left oblique CTA reveals a focal stenosis at the origin of the left ICA secondary to a shelf-like hypodense projection (white arrow), raising the possibility of carotid web or noncalcified atheroma. (d) Left CCA anterior oblique DSA confirms a sharp-edged triangular ridge on the posterolateral aspect of the left ICA (black arrow) consistent with a carotid web and a separate downstream segmental stenosis with pseudoaneurysm consistent with an iatrogenic dissection. (e) Left anterior oblique CCA DSA post-treatment demonstrates the Xact stent (black arrow) deployment across the left ICA origin and the Neuroform stent reconstruction and angioplasty across the iatrogenic dissection (arrow heads) with no residual stenosis. ICA: internal carotid artery; DSA: digital subtraction angiography; MCA: middle cerebral artery; ACA: anterior cerebral artery; TICI: Thrombolysis in Cerebral Ischemia score; CCA: common carotid artery.
The decision to proceed with cervical stenting as management for these symptomatic carotid web lesions was discussed and approved by a multidisciplinary cerebrovascular staff. After patient consent, carotid stenting was performed under monitored anesthesia care. Both patients were heparinized with a maximum activated clotting time (ACT) of approximately 250 seconds. Carotid stenting was performed using a self-expandable closed cell stent (Xact stent, both 8 mm × 20 mm, Abbott Vascular). In Patient 1, the procedure was under distal cerebral protection with a filter protection device (Emboshield 7.2 mm, Abbott Vascular) and a post-stenting angioplasty dilatation balloon (Viatrac Plus, Abbott Vascular) was used. In Patient 2, the presence of a downstream ICA dissection prevented the safe deployment of the protection device and no post-stenting angioplasty was performed. In addition, the mid-cervical dissection in Patient 2 also had endovascular treatment with deployment of a self-expanding intracranial stent (Neuroform 4.5 mm × 20 mm, Stryker Neurovascular) with post-stenting angioplasty using Gateway over the wire 4 mm × 15 mm angioplasty balloon at the time of the treatment of the carotid web because of a progressive dissection-related stenosis in the interval since the mechanical thrombectomy procedure. Control angiography was performed at the end of both procedures to confirm the integrity of the cervical and intracranial and cervical arteries. The carotid stenting procedures are summarized in Table 2.
Table 2.
Summary of the carotid stenting procedures.
| Patient 1 | Patient 2 | |
|---|---|---|
| Time interval (Stroke to procedure) | Three days | 10 days |
| Protection devices | Yes | No |
| Stents used | Xact carotid stent | Xact carotid stent for the web |
| Neuroform stent for the dissection | ||
| Post-angioplasty | Viatrac plus balloon | None for the web |
| Gateway balloon for the dissection | ||
| Procedural complications | None | None |
| Clinical and ultrasound follow-up | One year No recurrent TIAs/stroke Patent stent | Three months No recurrent TIAs/stroke Patent stent |
TIA: transient ischemic attack.
Patients were monitored in an intensive care unit for a period of 24 hours after the procedure. Aspirin 81 mg and clopidogrel 75 mg therapy was continued for three months followed by aspirin 81 mg indefinitely. Early clinical follow-up included a neurological examination and a Doppler ultrasound study for at least three months after the procedure. Both patients were independent with a modified Rankin score (mRS) of 0–1 with no recurrent neurological symptoms, transient ischemic attacks (TIAs) or strokes. Doppler ultrasound studies confirmed the patency of the carotid stents with no residual or in-stent stenosis/thrombosis.
Discussion
Carotid web was first described and histologically proven as a fibromuscular hyperplasia by Connett and Lansche in 1965.1 Following this observation, 50 additional carotid web cases2–17 (25 cases in a single report5) and two cases of vertebral artery web14 were subsequently described. Histopathologic examinations of surgical specimens showed an abnormal intimal layer that was affected by fibrosis,1–3,5,8,9,11,16 hyperplasia,5–7 folding14,15 or atherosclerosis.15 The web can be defined angiographically as a shelf- or triangular-like projection with stagnation and turbulences of the blood flow distal to it, which explains the proposed embolic mechanism of the ischemic stroke in these cases. Six studies noted the presence of a thrombus attached to the diaphragm.5–9,11,13,15 Both patients from our study had recurrent ischemic infarcts confined to a single arterial territory downstream from the web including one case presenting with a thromboembolic MCA occlusion.
The mean presenting age of stroke associated with a carotid web is 42 years, being equally prevalent in men and women.13 Apart from a single report of ICA web near the level of the first two cervical vertebrae,10 all other reported cases involved the carotid bulb or ICA origin. Carotid webs have previously been reported manifesting as a rare form of fibromuscular dysplasia (FMD)2–11,14–16 based on the non-atheromatous and noninflammatory (NANI) renal artery stenosis classification.18 Medial FMD of the carotid artery is rarely symptomatic and is often incidentally discovered during evaluation of dizziness, headache or a cervical bruit whereas carotid webs appear to confer a high risk of recurrent thromboembolic stroke despite aspirin therapy.13 The difference between the clinical features, prognosis and management of carotid webs and medial FMD necessitates their distinction as two independent radiological entities.
The definition of a web on CTA includes two descriptors: (1) an endoluminal shelf-like projection arising from the posterior/posterolateral wall of the ICA at the level of the carotid bifurcation in the neck best demonstrated on oblique sagittal reformats (as illustrated in Figures 1 and 2); and (2) a septum evident of axial section CTA.19 In our study, CTA successfully identified the web while MRA failed to detect these lesions. Most of the carotid webs reported in the literature were initially diagnosed on conventional angiography. DSA remains the angiographic gold standard with superior spatial and temporal resolution demonstrating both the intraluminal filling defect and distal turbulent flow resulting in delayed contrast washout from the carotid bulb. Several authors have reported the high recurrence rate for ischemic stroke secondary to carotid webs, presumably due to turbulent hemodynamics.2,3,5–9,11–13,16 Therefore, CTA findings suspicious for carotid webs with no significant atherosclerotic disease in a patient with recurrent ischemic stroke, confined to the same territory despite medical therapy, should be followed by DSA to confirm the diagnosis.
Carotid endarterectomy (CEA) is the standard management of carotid webs and most frequently reported interventional treatment in the literature.1–3,5–9,11,12,14–16 The evaluation of medical management for carotid web is limited with anticoagulation reported as a therapeutic option in only two patients11,13 and a 30% recurrence rate reported in a group of 20 Afro-Caribbean patients treated with antiplatelet therapy for atypical FMD;5 however, several patients in this study had overt thrombus at the site of the FMD, so such antiplatelet therapy wouldn’t be expected to work. Carotid stenting has been reported for carotid web management in two cases with satisfactory clinical results.13 To the best of the authors’ knowledge there are no larger randomized series of carotid web patients testing the CEA or carotid artery stenting (CAS) versus medical management.
The multidisciplinary decisions in favor of CAS as definite management for the two patients were made based on the availability of CAS at our institution and to limit the periprocedural risks of CEA especially in Patient 2. Apart from ICA dissection during an earlier mechanical thrombectomy intervention in Patient 2, the carotid webs in our study were treated successfully with carotid stenting with no intra- or post-procedural complications. One of our cases is unique in describing stenting of a carotid web shortly after mechanical thrombectomy for an acute intracranial large-vessel occlusion. Furthermore, follow-up neurological examinations and carotid Doppler ultrasound studies were normal for up to one year in Patient 1 and three months in Patient 2. The relative short-term follow-up of the cases may be considered as a limitation; in such cases long-term follow-up is needed to determine whether future in-stent stenosis is an issue.
Conclusion
Carotid artery webs may be an underestimated though rare cause of recurrent thromboembolic stroke in young and middle-aged adults despite antiplatelet therapy. CTA may assist in identification, but DSA remains the gold standard for diagnosis of a carotid web. Carotid stenting appears to be a viable alternative to open surgical management for secondary stroke prevention.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Connett MC, Lansche JM. Fibromuscular hyperplasia of the internal carotid artery: Report of a case. Ann Surg 1965; 162: 59–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ehrenfeld WK, Stoney RJ, Wylie EJ. Fibromuscular hyperplasia of the internal carotid artery. Arch Surg 1967; 95: 284–287. [DOI] [PubMed] [Google Scholar]
- 3.Rainer WG, Cramer GG, Newby JP, et al. Fibromuscular hyperplasia of the carotid artery causing positional cerebral ischemia. Ann Surg 1968; 167: 444–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Houser OW, Baker HL, Jr, Sandok BA, et al. Cephalic arterial fibromuscular dysplasia. Radiology 1971; 101: 605–611. [DOI] [PubMed] [Google Scholar]
- 5.Joux J, Chausson N, Jeannin S, et al. Carotid-bulb atypical fibromuscular dysplasia in young Afro-Caribbean patients with stroke. Stroke 2014; 45: 3711–3713. [DOI] [PubMed] [Google Scholar]
- 6.Gee W, Burton R, Stoney RJ. Atypical fibromuscular hyperplasia involving the carotid artery. Ann Surg 1974; 180: 136–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wirth FP, Miller WA, Russell AP. Atypical fibromuscular hyperplasia. Report of two cases. J Neurosurg 1981; 54: 685–689. [DOI] [PubMed] [Google Scholar]
- 8.Osborn AG, Anderson RE. Angiographic spectrum of cervical and intracranial fibromuscular dysplasia. Stroke 1977; 8: 617–626. [DOI] [PubMed] [Google Scholar]
- 9.So EL, Toole JF, Moody DM, et al. Cerebral embolism from septal fibromuscular dysplasia of the common carotid artery. Ann Neurol 1979; 6: 75–78. [DOI] [PubMed] [Google Scholar]
- 10.So EL, Toole JF, Dalal P, et al. Cephalic fibromuscular dysplasia in 32 patients: Clinical findings and radiologic features. Arch Neurol 1981; 38: 619–622. [DOI] [PubMed] [Google Scholar]
- 11.Kubis N, Von Langsdorff D, Petitjean C, et al. Thrombotic carotid megabulb: Fibromuscular dysplasia, septae, and ischemic stroke. Neurology 1999; 52: 883–886. [DOI] [PubMed] [Google Scholar]
- 12.Lipchik EO, DeWeese JA, Schenk EA, et al. Diaphragm-like obstructions of the human arterial tree. Radiology 1974; 113: 43–46. [DOI] [PubMed] [Google Scholar]
- 13.Lenck S, Labeyrie MA, Saint-Maurice JP, et al. Diaphragms of the carotid and vertebral arteries: An under-diagnosed cause of ischaemic stroke. Eur J Neurol 2014; 21: 586–593. [DOI] [PubMed] [Google Scholar]
- 14.Gironell A, Martí-Fàbregas J, de Juan-Delago M, et al. Carotid pseudo-valvular fold: A probable cause of ischaemic stroke. J Neurol 1995; 242: 351–353. [DOI] [PubMed] [Google Scholar]
- 15.Kliewer MA, Carroll BA. Ultrasound case of the day. Internal carotid artery web (atypical fibromuscular dysplasia). Radiographics 1991; 11: 504–505. [DOI] [PubMed] [Google Scholar]
- 16.Morgenlander JC, Goldstein LB. Recurrent transient ischemic attacks and stroke in association with an internal carotid artery web. Stroke 1991; 22: 94–98. [DOI] [PubMed] [Google Scholar]
- 17.McNamara MF. The carotid web: A developmental anomaly of the brachiocephalic system. Ann Vasc Surg 1987; 1: 595–597. [DOI] [PubMed] [Google Scholar]
- 18.Kincaid OW, Davis GD, Hallermann FJ, et al. Fibromuscular dysplasia of the renal arteries. Arteriographic features, classification, and observations on natural history of the disease. Am J Roentgenol Radium Ther Nucl Med 1968; 104: 271–282. [PubMed] [Google Scholar]
- 19.Choi PM, Singh D, Trivedi A, et al. Carotid webs and recurrent ischemic strokes in the era of CT angiography. AJNR Am J Neuroradiol 2015; 36: 2134–2139. [DOI] [PMC free article] [PubMed] [Google Scholar]