Abstract
The spontaneous regression of disk herniation secondary to dehydration is a much-debated topic in medicine. Some physicians wonder whether surgical removal of the extruded nucleus pulposus is really necessary when the spontaneous disappearance of a herniated lumbar disk is a well-known phenomenon. Unfortunately, without spontaneous regression, chronic pain leads to progressive disability for which surgery seems to be the only solution. In recent years, several studies have demonstrated the utility of oxygen–ozone therapy in the treatment of disk herniation, resulting in disk shrinkage. This retrospective study evaluates the outcomes of a series of patients with a history of herniated disks neuroradiologically unchanged in size for over two years, treated with oxygen–ozone therapy at our center over the last 15 years. We treated 96 patients, 84 (87.5%) presenting low back pain complicated or not by chronic sciatica. No drug therapy had yielded significant benefits. A number of specialists had been consulted in two or more years resulting in several neuroradiological scans prior to the decision to undertake oxygen–ozone therapy. Our study documents how ozone therapy for slipped disks “unchanged over time” solved the problem, with disk disruption or a significant reduction in the size of the prolapsed disk material extruded into the spinal canal.
Keywords: Lumbar disk herniation, ozone therapy
Introduction
Symptomatic lumbar disk herniation is a degenerative disease of the intervertebral disk that presents with a clinical picture characterized by back pain, sciatica, or compressive femoral (lumbar) radiculopathy and functional limitations or incapacity. Studies on the natural history of disk herniation show that the herniated intervertebral disk often resorbs completely or in part, and that the associated symptoms frequently subside with conservative therapies.1–10 Herniated disks are often detected in asymptomatic subjects undergoing diagnostic imaging (computed tomography (CT) and/or magnetic resonance imaging (MRI)) for other medical complaints. The herniated disk is therefore a dynamic phenomenon and a relatively common condition with a favorable prognosis in most cases.7,11
The variability of interventions and treatment offered for lumbar disk herniation reflects the uncertainty regarding the indications for surgery. Recent years have seen an increasing number of reports on the use of oxygen–ozone therapy for disk–root conflict caused by disk herniation.4,6,7,9,11–30 The therapeutic efficacy of CT-guided intraforaminal injection of an oxygen–ozone mixture in patients with disk–root pain caused by lumbar disk herniation is well known.7,15,16 This study reports on the outcomes of 84 patients with disk herniation unchanged for one or two years, treated with oxygen–ozone therapy.
Materials and methods
In the period April 2002–July 2015, we treated 84 patients (63 male, 33 female) aged between 42 and 71 (median age 63). All patients presented radiological CT or MR evidence of lumbar herniated disk and had a history of low back pain with or without sciatica. Medical treatment had not yielded significant benefits and repeated neuroradiological examinations were required by different specialists consulted over two or more years.
In these 84 cases we noted that there had been no change in imaging findings of disk herniation in the years before treatment, and all patients presented a similar medical history. In the first instance, all patients had been treated by their physicians who prescribed common analgesic and anti-inflammatory therapies, sometimes associated with muscle relaxants. Because of chronic pain, all patients were enrolled in our study.
We carried out a neuroradiological MRI check on the anatomical situation using a Siemens system (see Table 1). Imaging findings confirmed the unmodified herniated disks.
Table 1.
Siemens Magnetom AERA 1.5 T software SYNGO MR D13.
| T2 SAG 15 × 3 mm3 (Gap 20%, TR 3500, TE 100, Fov 300 mm, Matrix 384 Pd HF) |
| T1 SAG 15 × 3 mm3 (Gap 20%, TR 550, TE 9.7, Fov 300 mm, Matrix 384 Pd HF) |
| T2 AX 4 stacks 20 × 4 mm3 (Gap 10%, TR 4280, TE 100, Fov 220 mm, Matrix 384 Pd AP) |
| T2 SAG pair 15 × 3 mm3 (Gap 20%, TR 3900, TE 100, Fov 300 mm, Matrix 384 Pd HF) |
| T1 COR 15 × 3 mm3 (Gap 15%, TR 420, TE 9.1, Fov 300 mm, Matrix 384 Pd RL) |
| T1 FS SAG 15 × 3 mm3 con MDC (Gap 20%, TR 2500, TE 39, Fov 300 mm, Matrix 384 Pd HF FatSat) |
| T1 FS AX 20 × 3 mm3 con MDC (Gap 20%, TR 3500, TE 39, Fov 220 mm, Matrix 384 Pd AP) |
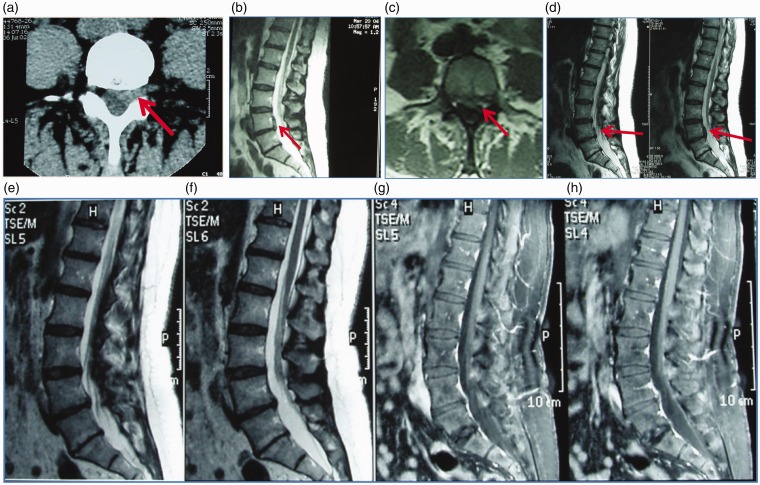
All patients who had been advised to undergo surgery had decided to wait. Persistent pain led them to have a second neuroradiological examination that confirmed the unchanged herniated disk. At this point, after clinical evaluation, we decided to administer oxygen–ozone therapy under CT guidance. All patients treated were then checked by MR scan one month after treatment (Figures 1 to 3).
Figure 1.
(a) CT scan of a 66-year-old woman with L4–L5 left disk herniation (arrow). (b, c) MR follow-up scans after 2 years showing no change in the herniated disk (March 2004) (arrows). (d) MR follow-up scan in Jan 2005, showing no change in the herniated disk (arrows). (e–h) MR follow-up scans (before and after gadolinium injection) in August 2005 one month after oxygen–ozone therapy. The hernia has completed disappeared.
Figure 2.
MR scan of 66-year-old woman on 12 November 2011 showing left herniated disk in L4–L5 (arrows). (c, d) MR follow-up scan on 6 September 2012 showing no change in the herniated disk (arrows). (e, f) MR follow-up scan (22 April 2013) after ozone therapy.
Figure 3.
(a, b) CT scan showing large L5–S1 left herniated disk (arrows). CT scan after one year showing no change in the herniated disk (arrows). (e, f) CT follow-up scan after ozone treatment showing complete resolution of the herniated disk.
CT-guided intraforaminal oxygen–ozone therapy
The treatment was administrated in the day hospital using the same infiltration technique adopted for discographic injections. We usually used a 9 cm 22G needle, but a longer needle was used in some cases depending on the patient’s size. The needle tip must be 4–5 mm from the foraminal region. CT scans were then used to check the correct positioning of the needle (Figure 4) and 3 cm3 of an oxygen–ozone mixture at 25 µg/mL were injected. The needle was then withdrawn for a few mm before injecting 7–8 cm3 of the gas mixture around the intervertebral joint. All treatments were performed using equipment fitted with a photometric detector, monitoring the concentration of ozone in the gas mixture. Another CT scan was then performed to ascertain the correct distribution of the oxygen–ozone mixture. Patients remained clinically monitored for about 30 min before being discharged.
Figure 4.
(a) Intraforaminal injection: correct position of the needle (arrows) and (b) control of the gas mixture (arrows).
All patients were then re-evaluated clinically 10 days after the procedure and if the result was not satisfactory a second treatment was carried out (the procedure can be repeated twice or even more without problems). Out of the 84 patients included in the study, 74 (77.1%) were treated twice, 11 once (11.5%), and 9 (9.4%) three times.
All patients underwent neuroradiological MRI follow-up one month after treatment.
We used a modified version of McNab’s method to define clinical outcome as follows:
Excellent: resolution of pain and a return to normal daily activities performed before the onset of pain.
Good or satisfactory: more than 50% reduction of pain.
Mediocre or poor: partial reduction of pain or no pain resolution.
Results
The neuroradiological follow-up showed that all herniated disks in our patients had persisted unchanged for years. Among the 84 patients, 77 (92.7%) had an alleviation of symptoms: total pain relief in 42 cases (50%) and partial relief in 35 (42.6%). The remaining seven of the 84 patients (8.3%) had no or negligible changes on imaging. The clinical benefit of treatment was immediate. No side-effects were reported.
Discussion
Despite the abundant literature on the topic, the long-term natural history of lumbar disk herniation remains unclear. Radicular pain is a well-recognized symptom of lumbar disk herniation caused by mechanical compression and the resulting vascular and biochemical inflammation generated by contact between disk material and nerve roots. Discogenic back pain is less well understood.
The therapeutic efficacy of oxygen–ozone treatment has been known for over 25 years and many studies have demonstrated the utility of oxygen–ozone administration in the treatment of herniated disks.4,6,7,9,11–39 Although the hernia can cause back pain, radiculopathy, sciatica or crural and functional impairment, disk degeneration can also occur in the absence of symptoms. Herniated disks are commonly encountered in asymptomatic subjects. Symptoms determined by herniated disk may resolve spontaneously: numerous diagnostic imaging studies have shown that the herniated lumbar disk subsides completely or shrinks in a high proportion of cases. The improvement is rapid within the first three months and is due to mechanisms of cell reabsorption mediated by cytokines without a fibroblastic reaction.
In this case series no medication had yielded significant benefits and the repeated neuroradiological documentation was the result of prescriptions from different specialists consulted over two or more years, prior to the decision to administer oxygen–ozone therapy.
This study documents how ozone therapy resolved the problem in this case series. Patients had both a favorable evolution of pain and herniated disk morphology, with disk disruption or significant shrinkage of the prolapsed disk material extruded into the spinal canal.
As CT-guided intraforaminal administration of ozone precisely controls the needle tract and injection, the oxygen–ozone mixture is selectively injected to improve the local circulation with a eutrophication effect on the compressed nerve root and associated muscle spasm. Oxygen–ozone administration normalizes the level of cytokines and prostaglandins with anti-inflammatory and pain relieving effects with an increased production of superoxide dismutase, minimizing oxidizing reagents. Lastly, the close proximity of the ozone mixture to the herniated material accelerates dehydration or destruction of the non-vascularized discal tissue yielding a good end result.4,26,31
Disk herniation is a relatively common dynamic phenomenon with a favorable prognosis in most cases. The vast majority (95%) of patients with back pain are able to return to work within three months from the onset of symptoms, without resorting to surgery.4,26,31
Large or fragmented disk herniations are usually considered clear indications for surgery. However, these lesions frequently regress spontaneously with conservative treatment: the probability of absorption increases with the size of the herniation and the extent of migration from the discal space. Even neurological deficits caused by herniated lumbar disk (with the exception of cauda equina syndrome, and a progressive loss of motor function) have a naturally favorable evolution.
Conclusions
The rapid resolution of low back pain with no complications, combined with an easy-to-perform treatment under CT guidance make intraforaminal oxygen–ozone therapy a viable alternative to surgery in the management of disk herniation. When surgery is not deemed essential, oxygen–ozone administration is the method of choice among mini-invasive percutaneous therapies.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Bozzao A, Gallucci M, Masciocchi C, et al. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology 1992; 185: 135–141. [DOI] [PubMed] [Google Scholar]
- 2.Bozzao A, Gallucci M, Aprile I, et al. Evoluzione spontanea dell'ernia discale nei pazienti trattati con terapia non chirurgica. Riv Neuroradiol 1993; 6: 267–273. [Google Scholar]
- 3.Davis RA. A long-term outcome analysis of 984 surgically treated herniated lumbar discs. J Neurosurg 1994; 80: 415–421. [DOI] [PubMed] [Google Scholar]
- 4.Iliakis E, Valadakis V, Vynios DH, et al. Rationalization of the activity of medical ozone on intervertebral disc and histological and biochemical study. Riv Neuroradiol 2001; 14(Suppl. 1): 25–30. [Google Scholar]
- 5.Kim KD, Kim ES. Spontaneous regression of herniated disc. Spine 2013; 38: 368. [DOI] [PubMed] [Google Scholar]
- 6.Magalhaes FN, Dotta L, Sasse A, et al. Ozone therapy as a treatment for low back pain secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain Physician 2012; 15: E115–E129. [PubMed] [Google Scholar]
- 7.Niu XK, Bhetuwal A, Yang HF. Diffusion-weighted imaging for pretreatment evaluation and prediction of treatment effect in patients undergoing CT-guided injection for lumbar disc herniation. Korean J Radiol 2015; 16: 874–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahimi-Movaghar V, Eslami V. The major efficient mechanisms of ozone therapy are obtained in intradiscal procedures. Pain Physician 2012; 15: E1007–1008. [PubMed] [Google Scholar]
- 9.Ribeiro RP, Matos RM, Vieira A, et al. Spontaneous regression of symptomatic lumbar disc herniation. Acta Reumatol Port 2011; 36: 396–398. [PubMed] [Google Scholar]
- 10.Saal JA, Saal JS, Herzog RJ. The natural history of lumbar intervertebral disc extrusions treated nonoperatively. Spine 1990; 15: 683–686. [DOI] [PubMed] [Google Scholar]
- 11.Perri M, Grattacaso G, Di Tunno V, et al. MRI DWI/ADC signal predicts shrinkage of lumbar disc herniation after O2–O3 discolysis. Neuroradiol J 2015; 28: 198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andreula CF, Simonetti L, De Santis F, et al. Minimally invasive oxygen–ozone therapy for lumbar disk herniation. Am J Neuroradiol 2000; 24: 996–1000. [PMC free article] [PubMed] [Google Scholar]
- 13.Andreula CF, Muto M, Leonardi M. Interventional spinal procedures. Eur J Radiol 2004; 50: 112–119. [DOI] [PubMed] [Google Scholar]
- 14.Barbara C, Simonetti L, Giatti S, et al. Trattamento percutaneo dell'ernia discale con iniezione intradiscale di miscela di ozono. Risultati preliminari. Riv Neuroradiol 1999; 12(Suppl. 4): 39. [Google Scholar]
- 15.Bonetti M, Fontana A, Cotticelli B, et al. Intraforaminal O2–O3 versus periradicular steroidal infiltrations in lower back pain: randomized controlled study. Am J Neuroradiol 2005; 26: 996–1000. [PMC free article] [PubMed] [Google Scholar]
- 16.Bonetti M, Cotticelli B, Raimondi D, et al. Ossigeno–ozonoterapia vs infiltrazioni epidurali cortisoniche. Riv Neuroradiol 2000; 13: 203–206. [Google Scholar]
- 17.Dall’Olio M, Princiotta C, Cirillo L, et al. Oxygen–ozone therapy for herniated lumbar disc in patients with subacute partial motor weakness due to nerve root compression. Interv Neuroradiol 2014; 20: 547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Santis F, Leonardi M, Simonetti L, et al. Ossigeno–ozonoterapia: la tecnica intradiscale. Int J Ozone Ther 2009; 8: 138–146. [Google Scholar]
- 19.Gallucci M, Limbucci N, Zugaro L, et al. Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology 2007; 242: 907–913. [DOI] [PubMed] [Google Scholar]
- 20.Gualandi G, Bonetti M. Ossigeno–ozonoterapia nel trattamento della patologia dolorosa del rachide lombare: esperienza preliminare. Acta Toxicol Ther 1996; 17: 261–264. [Google Scholar]
- 21.Iliakis E. Ozone treatment in low back pain. Orthopaedics 1995; 1: 29–33. [Google Scholar]
- 22.Lehnert T, Naguib NN, Wutzler S, et al. Analysis of disk volume before and after CT-guided intradiscal and periganglionic ozone–oxygen injection for the treatment of lumbar disk herniation. J Vasc Interv Radiol 2012; 23: 1430–1436. [DOI] [PubMed] [Google Scholar]
- 23.Leonardi M, Albini Riccioli L, Battaglia S, et al. Oxygen–ozone chemonucleolysis for herniated disc with sciatica. A comparison of treatments in patients with subacute and chronic symptoms. Rivi Ital Ossigeno Ozonoter 2006; 5: 33–36. [Google Scholar]
- 24.Leonardi M, Barbara C, Agati R, et al. Trattamento percutaneo dell'ernia discale lombare con iniezione intradiscale di miscela di ozono. Riv Neuroradiol 2001; 14(Suppl. 1): 51–53. [Google Scholar]
- 25.Leonardi M, Simonetti L, Raffi L, et al. Mini-invasive treatment of herniated disc by oxygen–ozone injection. Interv Neuroradiol 2003; 9(Suppl. 2): 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leonardi M, Simonetti L, Barbara C. Effetti dell'ozono sul nucleo polposo: reperti anatomo-patologici su un caso operato. Riv Neuroradiol 2001; 14(Suppl. 1): 57–59. [Google Scholar]
- 27.Matsubara Y, Kato F, Mimatsu K, et al. Serial changes on MRI in lumbar disc herniations treated conservatively. Neuroradiology 1995; 37: 378–383. [DOI] [PubMed] [Google Scholar]
- 28.Splendiani A, Perri M, Conchiglia A, et al. MR assessment of lumbar disk herniation treated with oxygen-ozone diskolysis: the role of DWI and related ADC versus intervertebral disk volumetric analysis for detecting treatment response. Neuroradiol J 2013; 26: 347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Steppan J, Meaders T, Muto M, et al. A meta-analysis of the effectiveness and safety of ozone treatments for herniated lumbar discs. J Vasc Interv Radiol 2010; 21: 534–548. [DOI] [PubMed] [Google Scholar]
- 30.Zhang Y, Ma Y, Jiang J, et al. Treatment of the lumbar disc herniation with intradiscal and intraforaminal injection of oxygen–ozone. J Back Musculoskelet Rehabil 2013; 26: 317–322. [DOI] [PubMed] [Google Scholar]
- 31.Leonardi M, Simonetti L, Barbara C. The effects of the ozone on the nucleus pulposus: pathological data on one surgical specimen. Riv Neuroradiol 2001; 14: 57–61. [Google Scholar]
- 32.Komori H, Shinomiya K, Nakai O, et al. The natural history of herniated nucleous polposus with radiculopathy. Spine 1996; 21: 225–229. [DOI] [PubMed] [Google Scholar]
- 33.Leonardi M, Andreula C, Simonetti L. Percutaneous techniques for treating disc disease. Funct Neurol 2003; 18: 242–244. [Google Scholar]
- 34.Leonardi M, Simonetti L, Agati R, et al. Recent CT advances in spine imaging. Riv Neuroradiol 2001; 14: 207–212. [Google Scholar]
- 35.Leonardi M, Simonetti L, Agati R. Neuroradiology of spine degenerative disease. Best Pract Res Clin Rheumatol 2002; 16: 59–88. [DOI] [PubMed] [Google Scholar]
- 36.Muto M, Andreula C, Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen–ozone (O2–O3) injection. J Neuroradiol 2004; 31: 183–189. [DOI] [PubMed] [Google Scholar]
- 37.Orief T, Orz Y, Attia W, et al. Spontaneous resorption of sequestrated intervertebral disc herniation. Acta Reumatol 2011; 36: 396–398. [DOI] [PubMed] [Google Scholar]
- 38.Pellicanò F, Martinetti F, Tavanti V, et al. The Italian Oxygen–Ozone Therapy Federation (FIO) study on oxygen–ozone treatment of herniated disc. Int J Ozone Ther 2007; 6: 7–15. [Google Scholar]
- 39.Saal JA. Natural history and nonoperative treatment of lumbar disc herniation. Spine 1996; 21(24 Suppl.): 2S–9S. [DOI] [PubMed] [Google Scholar]