Abstract
Although historically the majority of overdose education and naloxone distribution (OEND) programs have targeted opioid users, states are increasingly passing laws that enable third-party prescriptions of naloxone to individuals who may be able to respond to an overdose, including friends and family members of individuals who use opioids. In this report, we discuss the Baltimore Student Harm Reduction Coalition (BSHRC) OEND program, Maryland’s first community-based, state-authorized training program under a new law allowing third-party naloxone prescription. In an 8-month pilot period, 250 free naloxone kits were distributed, and 3 overdose reversals were reported to BSHRC. Trainings were effective in increasing self-efficacy surrounding overdose prevention and response, which appears to persist at up to 12 months following the training.
Naloxone is a Food and Drug Administration–approved medication that reverses opioid overdoses, including those from heroin and prescription opioids. It is easy to administer and has been used by paramedics to reverse opioid overdose for more than 30 years with an excellent safety record.1 In response to increasing overdose rates in the United States, opioid overdose and naloxone distribution (OEND) programs have increased dramatically since they were first established in 1996.2 As of 2014, there were 140 organizations known to provide naloxone kits to laypersons at 644 distinct sites in the United States.2 Current evidence suggests that individuals who may witness an overdose, and who have received appropriate training, can and do use naloxone to reverse opioid overdoses.3,4
Although most OEND programs target individuals who use opioids,2 national medical and pharmacy associations have advocated widening access to naloxone to individuals in close proximity to opioid users.5 As of July 2015, 36 states had legalized third-party prescriptions of naloxone to individuals who may have the ability to respond to an overdose.6
A PILOT OEND PROGRAM
Maryland’s Overdose Response Program bill (SB 610/HB 890) took effect on October 1, 2013, with regulations going into practice in April 2014; it allows for third-party prescriptions of naloxone. To receive a prescription, third parties are required to complete a state-authorized training on how to use naloxone.
The Baltimore Student Harm Reduction Coalition (BSHRC) OEND program was the first community-based, state-authorized training program in Maryland after passage of this bill.
BSHRC is a student-founded and community-based organization that supports harm reduction education, advocacy, and services. It is composed of health- and social justice–oriented Baltimore-area graduate and undergraduate students, recent graduates, and other community members dedicated to improving health among Marylanders made vulnerable by drug use, sex work, overdose, sexual minority status, HIV, or hepatitis. In 2015, it had 30 active members and 1 full-time executive director. It is a program of Fusion Partnerships, Inc, which provides fiscal sponsorship under its 501(c)3 status.
BSHRC’s OEND program is volunteer driven, using group members to administer trainings throughout the state. The training curriculum (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org) was informed by the Maryland state-mandated curriculum and other OEND programs across the country,3 and covers topics including how to recognize and respond to an overdose as well as overdose risk factors. Trainings take place in various locations, including parent- and peer-support groups, churches, and community-based health organizations serving at-risk populations. Those aged 18 years or older who complete the training are eligible to receive a free intramuscular naloxone kit prescribed by a volunteer medical provider present at the trainings.
BSHRC obtained naloxone through contractual agreements, and approximate cost per kit was $15.84, which is similar to other cost estimates of injectable naloxone kits and lower than for intranasal kits.3 Total materials came to $20.01 per kit. Labor costs reflecting the time of 1 part-time staff member overseeing the program were an additional $12.24 per kit.
METHODS
At the start of training sessions, the trainers verbally invited trainees to participate in the program evaluation, which consisted of pretest and posttest written surveys and follow-up telephone surveys after 8 to 12 months. Those who elected to participate provided written consent. Surveys assessed knowledge, attitudes, and self-efficacy surrounding opioid overdose using multiple choice questions and Likert scales. The telephone surveys additionally assessed overdose- and naloxone-related experiences since the training. These surveys included both multiple choice and open-ended questions. Participants were not compensated for the training or evaluation. We entered survey data into Microsoft Excel (Microsoft, Redmond, WA) and analyzed them using the McNemar test for matched pairs in Stata version 12.0 (StataCorp LP, College Station, TX). We qualitatively analyzed open-ended questions in Excel using content analysis.
RESULTS
During our pilot phase, from April through November 2014, 16 OEND trainings were held in Baltimore city and 10 Maryland counties. In total, 1 part-time BSHRC staffer, 14 BSHRC volunteers, and 4 volunteer prescribers trained 285 community members and distributed 250 free naloxone kits.
Of 263 eligible trainees, 50% consented to participate (n = 132) in the evaluation of the program, of whom 86% completed both initial pre- and posttest surveys (n = 113). Most individuals (72%) were at the training because they were concerned about somebody they knew overdosing, such as a family member, friend, or colleague.
We observed significant pretest-to-posttest increases on all knowledge items about overdose (P < .05; Table A, available as a supplement to the online version of this article at http://www.ajph.org). We also observed a significant increase from pretest to posttest in the percentage of participants strongly or somewhat agreeing with positively worded attitudes and self-efficacy items (P < .05; Table 1). There was no shift in the distribution of Likert scale responses for the item “I will get into trouble with law enforcement if I stay with someone who is overdosing.”
TABLE 1—
Attitudes and Self-Efficacy Surrounding Overdose Among Participants of an Overdose Training Program: Baltimore, MD, 2014
| Attitude or Self-Efficacy Item | Pretest (n = 113), No. (%) |
Posttest (n = 113), No. (%) | OR (95% CI)a | 8- to 12-Month Follow-Upb (n = 35), No. (%) |
| Completely or somewhat agree | ||||
| “It is worth it to talk about overdose with my friend or loved one who uses drugs, because overdose can be prevented.” | 100 (94.3) | 103 (97.2) | 4.0 (0.4, 197.0) | 36 (100.0) |
| “I can talk about preventing fatal overdose with someone I think may be at risk.” | 93 (86.9) | 102 (94.4) | 3.7 (1.0, 20.5) | 29 (93.6) |
| “I would be able to deal effectively with an overdose.” | 53 (50.0) | 96 (88.9)* | 20.5 (5.3, 175.0) | 35 (97.2)* |
| “I would be able to perform mouth to mouth resuscitation (‘rescue breathing’) to someone who has overdosed.” | 67 (63.2) | 93 (86.9)* | 9.7 (3.0, 49.6) | 34 (94.4)* |
| “I am able to inject naloxone into someone who has overdosed.” | 61 (57.0) | 98 (91.6)* | 37 (6.2, 1500.4) | 36 (100.0)* |
| Completely or somewhat disagree: “I will get into trouble with law enforcement if I stay with someone who is overdosing.” | 82 (77.4) | 87 (82.9) | 2.8 (0.8, 11.8) | 31 (100.0) |
Note. CI = confidence interval; OR = odds ratio.
OR comparing posttest to pretest (Ref).
OR and CI estimates not generated because of small sample sizes and cell sizes of zero.
*P < .05 using the McNemar test for matched pairs with pretest as the reference group.
Of the 31% of participants who were reached for follow-up at 8 to 12 months (n = 35), more than 90% agreed with the positively worded attitude and self-efficacy items. Most participants had either spoken with others about overdose prevention since the training (86%) or had told others that they had naloxone (83%; Table B, available as a supplement to the online version of this article at http://www.ajph.org). Additionally, most individuals reported keeping their naloxone at home (67%) as opposed to carrying it on them (22%), many citing fears of heat sensitivity during the summer months.
Three participants voluntarily reported overdose reversal after administering naloxone received at the training. Three additional overdoses were reported through follow-up surveys; however, these did not lead to naloxone administration. In 2 cases, a parent found a child who had overdosed in the house. In both of these cases, 911 was called; however, naloxone was not used in either case because the individual had reportedly already died (“stiff” or “cold”).
DISCUSSION
In its first 8 months, BSHRC, a small organization with 1 paid staff member, was able to reach 285 participants and received reports of 3 successful overdose reversals through trainings at various community-based locations. Trainings were effective at increasing self-efficacy surrounding overdose prevention and response, which appears to persist at 8 to 12 months following the survey. It is uniquely run by a coalition of student volunteers, which saves costs and has the additional impact of engaging students in community health. This model may become relevant in other jurisdictions and states as more states legalize third-party prescription of naloxone. Notably, new laws and regulations passed since the pilot period have positively affected Maryland OEND programs. In 2015, two new Maryland laws (SB 654/HB 1009 and SB 516/HB 0745) strengthened existing “Good Samaritan” protections aimed at decreasing fears of calling 911. Indeed, Good Samaritan protections may alleviate the persistent concerns about calling 911 among participants, which has been demonstrated in other studies.7 SB 516/HB 0745 also authorized standing orders for naloxone, obviating the need for medical providers present at the trainings.
Limitations
This study was limited by the low response rate at 8- to 12-month follow-up, because those who could be reached by phone may have differed from those we were unable to reach. Additionally, tracking overdoses and naloxone administration was dependent on participant self-report and follow-up surveys and, thus, probably does not capture all overdoses or reversals that occurred.
Further Discussion
Training third parties differs from training individuals who disclose opioid use in important ways. First, many individuals attending such trainings may not themselves use opioids and may be less familiar with substance use and signs of overdose. Therefore, trainings also offer an opportunity to provide substance use and addiction education to minimize stigma. Additionally, as many third parties are family members of individuals at risk for overdose, trainings that encourage family members to talk about substance use and overdose with loved ones expand the impact of trainings beyond the administration of naloxone. Indeed, our preliminary results suggest that the vast majority of trainees spoke about overdose with others following the training, which, if done in a supportive way, may have benefits.8,9 Finally, although studies among opioid users show that a quarter to 100% of individuals keep their naloxone either on their persons or in the place where they use drugs,4 most individuals in this study reported keeping their naloxone at home, many citing fears of heat sensitivity. Discussions with participants about how to minimize risks of expirations versus maximize probability of use may benefit future trainings.
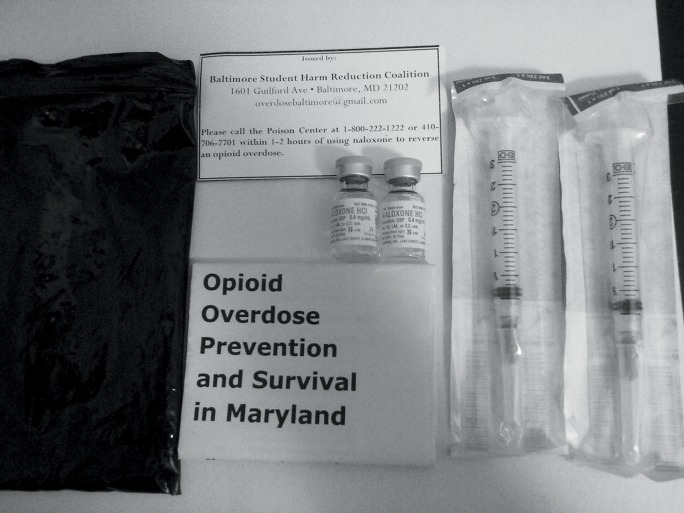
Contents of overdose education and naloxone distribution (OEND) kits include two single-dose 1-mL vials of naloxone (0.4 mg/mL), two 3-mL intramuscular syringes (23 gauge, 1½ inches), a certificate of training completion, and an instructional brochure enclosed in a black zippered bag with a prescription label.
ACKNOWLEDGMENTS
The Baltimore Student Harm Reduction Coalition is funded by grants from Open Society Institute–Baltimore and the Abell Foundation.
We acknowledge Jennifer H. Kirschner, Demetrius D. Marcoulides, Natanya Robinowitz, Alex Niculescu, and training participants for making this program and study possible.
HUMAN PARTICIPANT PROTECTION
Written consent was obtained and all study procedures were confidential. The study was approved by the Johns Hopkins Bloomberg School of Public Health institutional review board.
REFERENCES
- 1.Kim D, Irwin KS, Khoshnood K. Expanded access to naloxone: options for critical response to the epidemic of opioid overdose mortality. Am J Public Health. 2009;99(3):402–407. doi: 10.2105/AJPH.2008.136937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wheeler E, Jones TS, Gilbert MK, Davidson PJ. Opioid overdose prevention programs providing naloxone to laypersons —United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64(23):631–635. [PMC free article] [PubMed] [Google Scholar]
- 3.Clark AK, Wilder CM, Winstanley EL. A systematic review of community opioid overdose prevention and naloxone distribution programs. J Addict Med. 2014;8(3):153–163. doi: 10.1097/ADM.0000000000000034. [DOI] [PubMed] [Google Scholar]
- 4.Strike C, Hopkins S, Watson TM . Best Practice Recommendations for Canadian Harm Reduction Programs That Provide Service to People Who Use Drugs and Are at Risk for HIV, HCV, and Other Harms: Part 1. Toronto, Ontario: Working Group on Best Practice for Harm Reduction Programs in Canada; 2013. [Google Scholar]
- 5.Doyon S, Aks SE, Schaeffer S. Expanding access to naloxone in the United States. Clin Toxicol (Phila) 2014;52(10):989–992. doi: 10.3109/15563650.2014.968657. [DOI] [PubMed] [Google Scholar]
- 6.Network for Public Health Law. Legal interventions to reduce overdose mortality: naloxone access and overdose Good Samaritan laws. Updated July 2014. Available at: https://www.networkforphl.org/_asset/qz5pvn/network-naloxone-10-4.pdf. Accessed September 12, 2015.
- 7.Banta-Green CJ, Kuszler PC, Coffin PO, Schoeppe JA. Washington’s 911 Good Samaritan Drug Overdose Law—initial evaluation results. Alcohol & Drug Abuse Institute, University of Washington, November 2011. Available at: http://adai.uw.edu/pubs/infobriefs/ADAI-IB-2011-05.pdf. Accessed September 12, 2015. [DOI] [PMC free article] [PubMed]
- 8.Cavaiola AA, Fulmer BA, Stout D. The impact of social support and attachment style on quality of life and readiness to change in a sample of individuals receiving medication-assisted treatment for opioid dependence. Subst Abus. 2015;36(2):183–191. doi: 10.1080/08897077.2015.1019662. [DOI] [PubMed] [Google Scholar]
- 9.Lee CH, Wang TJ, Tang HP, Liu YH, Bell J. Familial expressed emotion among heroin addicts in methadone maintenance treatment: does it matter? Addict Behav. 2015;45:39–44. doi: 10.1016/j.addbeh.2015.01.014. [DOI] [PubMed] [Google Scholar]