Abstract
Background: Cognitive dysfunction affects approximately 43% to 70% of individuals with multiple sclerosis (MS) and is an important determinant of several functional outcomes in MS and quality of life. Brief neuropsychological test batteries have been developed specifically for use in MS and are widely used to aid clinicians in assessing levels of cognitive impairment in MS. Neuropsychologists and neurologists also frequently use briefer screening measures, such as the Perceived Deficits Questionnaire (PDQ), to assist in determining whether a more extensive neuropsychological evaluation is warranted. However, despite the ease of such measures, the relationship between self-report and objective cognitive impairment has been inconsistent, at best. Moreover, factors such as depression, fatigue, anxiety, and personality have been found to be more related to reports of cognitive difficulties. The purpose of the present study was to clarify the relationship between subjective cognitive concerns and objective cognitive impairment while accounting for related symptoms.
Methods: We examined the association of self-reported cognitive concerns on the PDQ with objective cognitive measures, as well as depression, anxiety, fatigue, and self-efficacy.
Results: There was no relationship between self-reported cognitive concerns and objective performance. Rather, reports on the PDQ were more correlated with reports of depression, anxiety, fatigue, and self-efficacy.
Conclusions: Depression and poor self-efficacy can contribute to reports of cognitive difficulties. Effective treatment to improve these factors seems warranted given the impact of perceived cognitive impairment on outcomes in MS and the potential for more accurate self-reports.
Multiple sclerosis (MS) is a neurologic disorder that affects approximately 2.3 million people worldwide.1 Cognitive and behavioral changes are common following the onset of this most common nontraumatic neurologic disorder of middle adulthood. In particular, cognitive dysfunction affects approximately 43% to 70% of individuals with MS.2 The degree of cognitive impairment varies among individuals, but the most affected domains include information processing speed2 and learning and memory.1–4 To a lesser extent, impairments in executive functioning, attention, and visuospatial abilities have also been reported.5 Due to the high prevalence of cognitive impairment in individuals with MS, and its potential to detrimentally affect individuals' vocational and personal life, identification of cognitive deficits is of paramount concern.
Brief neuropsychological test batteries, such as the Minimal Assessment of Cognitive Functioning in Multiple Sclerosis (MACFIMS)6 and the Brief Repeatable Neuropsychological Battery (BRNB),7 have now been extensively used and can aid clinicians in accurately assessing levels of cognitive impairment in MS. However, these evaluations can be costly and time-consuming, particularly when repeated every few years. Given this, neuropsychologists and neurologists frequently use briefer screening measures, such as the Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS),8 to assist in determining whether a more extensive neuropsychological evaluation is warranted. In addition, self-report questionnaires, such as the Multiple Sclerosis Neuropsychological Screening Questionnaire (MSNQ)9 and the Perceived Deficits Questionnaire (PDQ),10 have been suggested to assess patients' and significant others' perception of cognitive concerns.
The MSNQ was developed to provide clinicians with a neuropsychological impairment screening measure that would be brief, cost-effective, and convenient to administer. Initial findings affirmed the reliability and validity of this tool, demonstrating significant correlations between informants' reports and objective measures of cognitive performance.9 However, in the same study, patients' self-reports did not correlate with objective cognitive performance but were more related to reports of depression. In a larger follow-up study, the investigators found that patients' self-reports were correlated with objective cognitive measures but noted that correlations to depressive measures remained stronger.11 Taken together, these findings suggest that the measure is susceptible to the occurrence of false-positive reports of cognitive deficits in those experiencing concomitant depressive symptoms. This cautionary provision was echoed in a subsequent investigation of the MSNQ, further raising the concern that the self-report of cognitive concerns may be more related to depressive symptoms than to objective cognitive performance, per se.12 Thus, it has been recommended that other screening instruments (eg, depression measures) be administered when using self-report measures of cognitive functioning to determine the contribution of affective symptoms to cognitive concerns.13
The PDQ was also developed specifically for MS to measure self-reported cognitive impairment and is part of the Multiple Sclerosis Quality of Life Inventory. As with the MSNQ, previous investigators have been unable to find a direct and consistent relationship between this measure and objective neuropsychological test performance.14,15 Reports on the PDQ have similarly been found to be related to concomitant reports of depression.15 Moreover, in a recent study examining the PDQ in a population of patients with lupus, who tend to underreport cognitive concerns, Vogel et al.16 observed a high correlation between subjective cognitive concerns as measured by the PDQ and self-rated depressive symptoms. Together, these findings suggest that coexisting depressive symptoms confound self-reports of cognitive dysfunction, which affects the interpretation of these self-report measures and reduces their clinical utility.
Although depression and its influence on cognitive concerns has received the most attention in MS, other confounding variables are thought to affect a patient's perceived cognition, namely, fatigue, anxiety, personality, and self-efficacy. Fatigue is one of the most frequently reported symptoms in MS,17,18 and it has been shown to be related to self-reported cognitive concerns. Specifically, in a recent investigation, Kinsinger et al.19 found that changes in depression and fatigue after treatment were associated with fewer perceived deficits after treatment. This finding suggests that fatigue, as well as depression, plays a role in patients' perceptions of their cognitive ability.
Another common report among people with MS is elevated levels of anxiety.20 Despite the prevalence of anxiety in the MS community, it remains relatively understudied in this population. As with fatigue, there is growing evidence of a relationship between self-reported cognitive symptoms and anxiety. Lester et al.21 found that anxiety symptoms contributed to one's perceived cognitive impairments, in conjunction with depression. Furthermore, Akbar et al.22 found depression, anxiety, and personality to be associated with cognitive concerns as measured by the MSNQ and not reflective of objective cognitive impairment on the BRNB. Regarding personality specifically, lower levels of conscientiousness and higher levels of neuroticism were correlated with greater reports of cognitive concerns. The finding that neuroticism was correlated with subjective cognitive concerns is not surprising given that high levels of neuroticism are highly associated with anxiety, depression, and somatization. Conscientiousness, or the tendency to be orderly, thorough, and careful, is also likely to be associated with one's perception of their cognition, as they may feel that they are making more errors, which, in fact, may be a result of low levels of conscientiousness. In fact, in a stepwise regression analysis, anxiety and conscientiousness were the most significant predictors of perceived cognitive dysfunction. This research supported previous work demonstrating an association of conscientiousness and neuroticism with self-reported cognitive concerns.23,24
Finally, greater attention has been given to the role of self-efficacy in MS and its influence on perceived functioning and overall quality of life.25,26 By definition, self-efficacy refers to one's own confidence in being able to perform a given behavior and is considered to be a measure of perceived capability rather than actual capability.27 As a result, investigators are beginning to examine this measure in relationship to perceived cognitive deficits and objective performance.28 For instance, Lester et al.'s21 investigation of emotional functioning and perceived cognition found self-efficacy to be related to depression and anxiety, known contributors to cognitive concerns. They suggested that further attention to the role of self-efficacy was warranted as both a direct and mediating effect on perceived functioning.21
The aim of the present study was, thus, to examine the relationship between subjective cognitive concerns on the PDQ and objective neuropsychological performance while taking into account the possible confounding factors of depression, anxiety, fatigue, and self-efficacy. We hypothesized that the correlation between subjective cognitive concerns and objective performance on a neuropsychological test battery would be inconsistent, at best. In contrast, we hypothesized that the relationship between subjective cognitive concerns and factors such as depression, anxiety, fatigue, and one's perceived self-efficacy would yield stronger and more consistent associations.
Methods
Participants
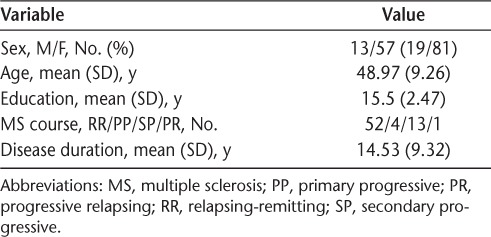
Participants consisted of individuals diagnosed as having clinically definite MS who were enrolled in a randomized clinical trial examining the effectiveness of a memory retraining program in MS. For all the participants, it must have been at least 1 month since their most recent exacerbation and corticosteroid use. Individuals with a history of stroke or neurologic injury/disease, psychiatric illness, or alcohol or drug abuse were excluded. All the study procedures were approved by the institutional review board of the Kessler Foundation. Informed consent was obtained from all the participants at the screening evaluation. Seventy individuals diagnosed as having clinically definite MS were enrolled in the present study and completed a neuropsychological test battery, which is reported herein. The mean (SD) age of the participants was 48.97 (9.26) years, and the mean (SD) amount of education was 15.5 (2.47) years (Table 1).
Table 1.
Demographic characteristics of the 70 study participants
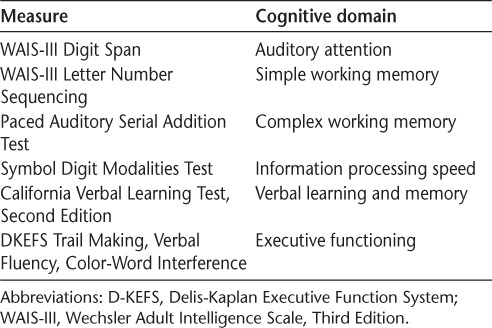
Measures
The PDQ was completed by all the participants. The PDQ consists of 20 items and instructs patients to assess their cognitive functioning within the past 4 weeks. Each item is rated on a 5-point scale ranging from 0 (never) to 5 (almost always). This instrument consists of four subscales identifying domains commonly impaired in MS: attention, retrospective memory, prospective memory, and planning and organization. The combined subscales yield a total score ranging from 0 to 80, with a higher score indicating greater perceived cognitive impairment. Objective measurement of cognitive functioning was obtained through a brief neuropsychological test battery (Table 2).
Table 2.
Neuropsychological test battery
Participants also completed a packet of questionnaires assessing their overall psychological health (depression, anxiety, and self-efficacy) and MS symptoms that can influence cognition (eg, fatigue). In particular, depression was assessed by the Chicago Multiscale Depression Inventory (CMDI), a self-report measure that was specifically designed to assess depression in MS and other medically ill groups. It consists of three subscales: Evaluative, Mood, and Vegetative. Each subscale contains 14 items, and patients are asked to rate on a scale from 1 to 5 the extent to which each word/phrase describes them during the past week, including today, with 1 being “not at all” and 5 being “extremely.”
The State-Trait Anxiety Inventory was used to assess anxiety. This 40-item measure is divided into two 20-item scales to assess present (state) and long-standing (trait) anxiety. Ratings are based on a 4-point Likert scale. Patients are asked to describe how they feel at the present moment (state) as well as how they generally feel (trait).
Fatigue was assessed by the Modified Fatigue Impact Scale (MFIS). The MFIS is a modified form of the Fatigue Impact Scale consisting of items derived from interviews with patients with MS assessing the degree to which fatigue affects their lives. This instrument provides an assessment of the impact of fatigue on physical, cognitive, and psychosocial functioning, with a subscale for each type of fatigue. The full-length MFIS consists of 21 items rated on a 5-point Likert scale.
Self-efficacy was measured using the Multiple Sclerosis Self-Efficacy Scale (MSSES), an 18-item inventory assessing both a functional domain, reflecting a patient's certainty in the ability to function independently, and a control domain, identifying a patient's confidence in the ability to manage and cope with disease. Each item is rated on a scale from 10 (very uncertain) to 100 (very certain), with 10-point intervals in between. The items in each subscale are summed to produce separate scores for self-efficacy function and control and then are combined to produce an MSSES general score, with totals ranging from 180 to 1800. Designed specifically for use in MS, the MSSES has been shown to be a reliable, valid, and stable measure.29
Statistical Analyses
All statistical analyses were conducted using PASW Statistics for Windows, version 18.0 (SPSS Inc, Chicago, IL). Correlational analyses were first conducted to examine the relationship between subjective cognitive concerns and objective cognitive performance. Additional correlations were then performed among the factors presumed to confound reports of cognitive concerns (ie, depression, fatigue, anxiety, and self-efficacy). Finally, to determine which of these factors most contributed to subjective cognitive concerns, a stepwise hierarchical regression was performed, with the total score of the PDQ as the dependent variable.
Results
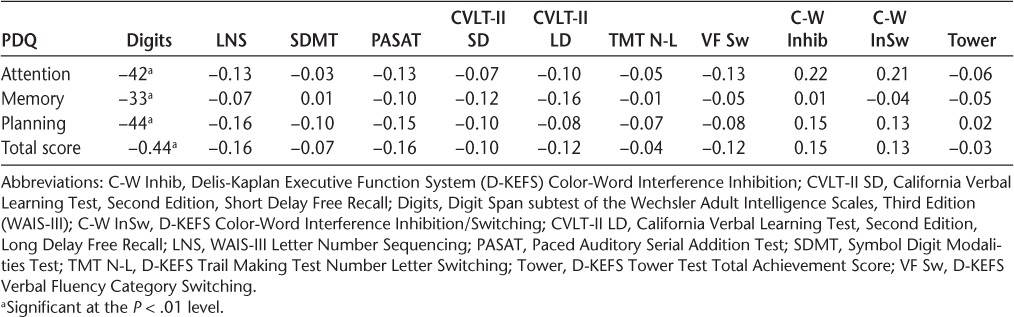
Pearson correlations indicated that individuals' self-reports on the PDQ were related only to performance on a simple measure of attention (Digit Span). More specifically, a significant correlation was noted between Digit Span and all indices of the PDQ (r = −0.33 to −0.44). There were no other significant correlations with the PDQ and any of the other objective neuropsychological measures (Table 3).
Table 3.
Pearson correlates of the Perceived Deficits Questionnaire (PDQ) and neuropsychological test performance
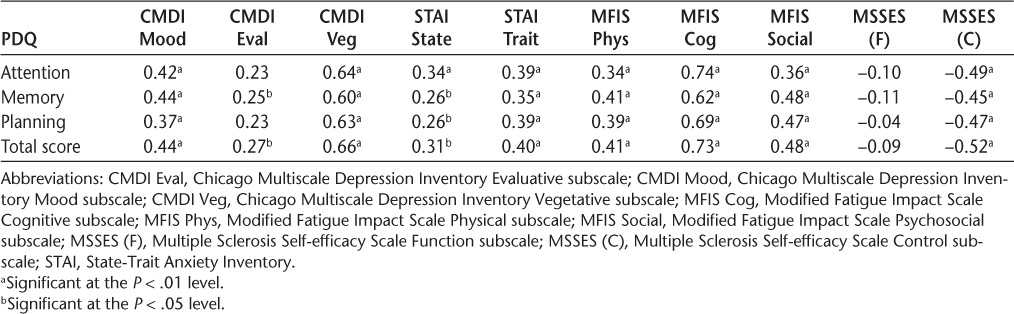
In contrast, cognitive concerns on the PDQ were significantly correlated with all self-report indices. In particular, the total PDQ score was correlated with depression (Mood subscale: r = 0.44, P < .001; Evaluative subscale: r = 0.27, P = .025; Vegetative subscale: r = 0.66, P < .001), anxiety (state: r = 0.31, P = .010; trait: r = 0.40, P = .001), fatigue (physical: r = 0.41, P < .001; cognitive: r = 0.73, P < .001; psychosocial: r = 0.48, P < .001), and self-efficacy (control: r = −0.52, P < .001). In addition, each index of the PDQ (ie, Attention, Memory, and Planning) maintained significant associations with each self-report factor. See Table 4 for the correlations with the specific breakdown of all the subscales of the PDQ.
Table 4.
Pearson correlations of the Perceived Deficits Questionnaire (PDQ) with depression, anxiety, fatigue, and self-efficacy
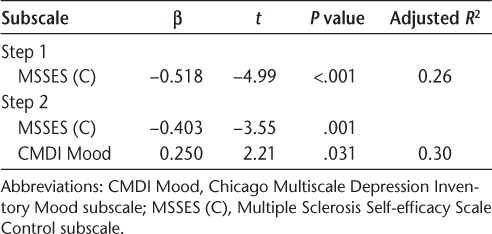
A stepwise regression analysis was performed to determine the most salient predictors of subjective cognitive concerns, as measured by the PDQ. The total PDQ score served as the dependent variable, with depression (Mood subscale), anxiety, fatigue (Physical subscale), and self-efficacy as the predictor variables. As shown in Table 5, the most significant predictors of cognitive concerns as measured by the PDQ were self-efficacy (β = −0.403, P = .001) and depression (β = 0.250, P = .031). Together, these variables accounted for 30% of the variance on the PDQ total score (F2,67 = 15.60, P < .001).
Table 5.
Stepwise hierarchical regression predicting subjective cognitive concerns on the Perceived Deficits Questionnaire
Discussion
Cognitive disturbances are common in MS and are known to have a grave effect on individuals' day-to-day functioning and overall quality of life. Proper identification of individuals' cognitive strengths and weaknesses is imperative to making informed decisions regarding outcomes such as employment and disability, monitoring disease progression, and providing recommendations as to how to best manage day-to-day life activities. Presently, neuropsychological test batteries, such as the MACFIMS and the BRNB, or the even more brief BICAMS battery, are administered to assess cognitive functioning in MS. Self-report questionnaires such as the PDQ and MSNQ are included to further assess one's cognitive concerns and sometimes receive additional input from one's significant others, as is the case with the MSNQ. Unfortunately, previous work documenting the relationship between subjective concerns and objective cognitive performance cite poor or nonexistent findings, generating concern over the clinical utility of self-report measures of cognition.12,22 The current investigation aimed to 1) examine the relationship between subjective cognitive concerns on the PDQ and objective cognitive performance and 2) examine the relationship between reports on the PDQ and reports of depression, fatigue, anxiety, and self-efficacy. Based on the previous findings that noncognitive factors, such as emotional status, disease-related variables, and personality traits, may have a significant effect on one's perception of cognitive functioning, we hypothesized that there would be a stronger and more consistent relationship between cognitive concerns and these factors.
Findings from the present study demonstrate that subjective cognitive concerns were correlated with only one objective measure of simple attention. There was no relationship between objective performance on the remaining tests of memory, processing speed, working memory, or executive functioning and subjective cognitive concerns on the PDQ. The finding that performance on a simple measure of attention correlated with all the indices of the PDQ may be, in part, attributed to the fact that intact attention underlies all cognitive functions. Nonetheless, the remainder of null findings confirm the weak association between subjective and objective cognitive performance previously described in the literature.12,14,15,22
In contrast, reports of cognitive concerns on the PDQ were highly correlated with concomitant reports of depression, anxiety, fatigue, and self-efficacy, in line with existing literature.15,19,21 Among these variables, reports on the PDQ were most highly correlated with vegetative symptoms of depression (r = 0.60 to 0.66) and cognitive fatigue (r = 0.62 to 0.74). This association may be attributed to the fact that items composing the PDQ and those composing the Vegetative Depression subscale on the CMDI and the Cognitive Fatigue subscale on the MFIS overlap (ie, both contain items pertaining to cognition). However, reports on the PDQ were also highly correlated with the Mood subscale of the CMDI (mean r = 0.42), trait anxiety (mean r = 0.38), physical fatigue (mean r = 0.38), and psychosocial fatigue (mean r = 0.45). These findings are consistent with previous investigations that have demonstrated a significant relationship between perceived cognitive difficulties and depression, anxiety, and fatigue and suggest that approximately 20% of the variance on a measure of perceived cognitive concerns could be explained by any one of these variables.
It has previously been shown that self-efficacy plays an important role in the perception and management of one's illness and has received greater attention in MS most recently. In fact, self-efficacy has been proved to be a predictor of health status,30 adherence to treatment,31 disease management,32 adjustment,33 physical and social functioning,25 and physical activity and health-related quality of life.26 A more recent investigation found self-efficacy to be a significant predictor of physical, social, and cognitive functioning in MS, even when taking into account neurologic impairment and depression.34 Low self-efficacy has also been shown to be related to high levels of depression.25 Depression and low self-efficacy accompanied by increased stress and disability tend to result in a greater chance of developing anxiety in individuals with MS.35 Taken together, it may be proposed that reduced self-efficacy lies at the root of the psychological distress found in MS, which could result in problems with adjustment, perception, and management of one's illness. Such poor adaptation and perception may result in greater reports of cognitive dysfunction, independent of objective impairment.
Thus, self-efficacy was considered a potentially influencing factor that could further explain the lack of a consistent relationship between objective cognitive performance and subjective reports. In fact, the Control subscale of the MSSES was found to have a significant inverse relationship with reports on the PDQ (mean r = −0.48). The Control subscale measures the extent to which individuals feel they can control and/or manage their MS symptoms, avoid allowing their MS to take over their lives, and maintain their overall well-being. This relationship suggests that a low sense of control would be associated with greater cognitive concerns and, again, potentially account for nearly a quarter of the variance. In fact, a subsequent hierarchical regression confirmed that self-efficacy accounted for 26% of the variance of reports on the PDQ, with depression accounting for an additional 4%. Anxiety and fatigue did not contribute significantly beyond self-efficacy and depression, suggesting that of the examined factors, reports of cognitive concerns were most closely related to self-efficacy and depression, together accounting for 30% of the variance.
These findings highlight the importance of individual factors, specifically, self-efficacy and, to a lesser extent, depression, in the perception of cognitive dysfunction in MS and suggest that interventions aimed at enhancing one's self-efficacy and managing depression may be warranted in reducing the impact of perceived cognitive difficulties in individuals with MS. Interventions targeted at improving self-efficacy have also been found to have significant benefits for treated individuals. Improved self-efficacy after a wellness intervention has been shown to result in greater engagement in health-promoting behaviors, which are important for managing one's MS. Improved health-related quality of life (ie, pain and mental health) was noted specifically in women with MS. There were also benefits seen in functional outcomes (ie, employment). In particular, although there were no differences in the rate of employment at baseline, more women in the intervention group were found to be employed at 8-month follow-up.36 These findings suggest that interventions aimed at enhancing self-efficacy are effective at improving overall health as well as functional outcomes in MS. Thus, greater attention should be given to the assessment and treatment of self-efficacy in individuals with MS, particularly given the variability and uncertainty associated with MS. Findings from the present study similarly highlight the importance of self-efficacy in the accurate perception of one's cognitive abilities. Recently, greater attention has been given to the role of self-efficacy in the perception of cognitive functioning in MS. Previous findings suggest that interventions aimed at improving self-efficacy result in more accurate perceptions of cognition in MS, which could inform outcomes and influence one's overall quality of life. Further studies examining the effectiveness, feasibility, and long-term outcomes of such interventions seem warranted at this time.
Regarding depression, reductions in depressive symptoms have also been shown to improve individuals' accuracy in their perception of their cognitive functioning in the absence of significant change in objective cognitive functioning.19 More accurate perceptions of one's cognitive abilities and associated challenges will better inform practitioners and patients as to how to best make decisions and recommendations regarding functional outcomes in MS. This is a main priority of neuropsychological evaluations.
Limitations of the present study include a relatively small sample size and selection and the use of simple zero-order correlations. Further investigations with a larger sample size and perhaps a more representative sample of individuals with MS are warranted. In particular, the sample was derived from a clinical trial aimed at improving memory, which may bias reports somewhat as participants needed to perform 1.5 SD below normative data on a word list memory task to be eligible. However, note that most participants were not found to be impaired cognitively, per se. On the brief neuropsychological test battery, 36% were 1.5 SD below on a measure of processing speed and 43% on a measure of memory. A third or less of the participants were 1.5 SD below on the remaining measures. Participants were also slightly older and more educated than the average MS sample. In addition, the results were exclusively correlational and limited to measures of psychological functioning. Inclusion of other outcome variables (eg, quality of life, employment, and day-to-day functioning) would allow for more advanced modeling of these constructs. Such modeling could further demonstrate the direct and indirect relationships between these constructs, as well as any mediating/moderating factors.
Despite these limitations, the present study offers important contributions to the assessment and recommendation for treatment aspects of clinical work in people with MS. The study findings include insights for better understanding the relative contribution of individual factors, such as self-efficacy and depression, to perceived cognitive ability. Consequently, assessment of perceived cognitive functioning should include measures of these constructs, such as the MSSES and the CMDI. In addition, the results of the present study suggest that for individuals whose perception of cognitive dysfunction is greater than warranted by the objective evaluation, recommendations should include interventions targeted to increase self-efficacy and effectively manage symptoms of depression. This, in turn, may result in improved outcomes, including overall quality of life.
PracticePoints.
Cognitive impairment is common in MS, affecting up to 70% of individuals.
Brief cognitive test batteries and self-report measures are commonly used to assess one's cognitive difficulties. However, the relationship between objective cognitive test performance and subjective reports of cognitive functioning has been found to be inconsistent at best.
Identification of the factors (eg, depression) that may account for these inconsistencies is important for clinical practice because it can inform appropriate interventions.
Footnotes
From the Kessler Foundation, West Orange, NJ, USA (LBS, AB, OMN, NC, JD); and Department of Physical Medicine and Rehabilitation, Rutgers, the State University of New Jersey, New Jersey Medical School (LBS, NC, JD).
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This work was supported by the National Center for Medical Rehabilitation Research, National Institutes of Health (grant R01 HD045798).
References
- 1.Multiple sclerosis FAQs. National Multiple Sclerosis Society website. http://www.nationalmssociety.org/about-multiple-sclerosis/what-we-know-about-ms/faqs-about-ms/index.aspx#howmany. Accessed November 2013.
- 2.Chiaravalloti ND, DeLuca J. Cognitive impairment in multiple sclerosis. Lancet Neurol. 2008;7:1139–1151. doi: 10.1016/S1474-4422(08)70259-X. [DOI] [PubMed] [Google Scholar]
- 3.DeLuca J, Barbieri-Berger S, Johnson SK. The nature of memory impairments in multiple sclerosis: acquisition versus retrieval. J Clin Exp Neuropsychol. 1994;16:183–189. doi: 10.1080/01688639408402629. [DOI] [PubMed] [Google Scholar]
- 4.Rao SM, Grafman J, DiGiulio D et al. Memory dysfunction in multiple sclerosis: its relation to working memory, semantic encoding, and implicit learning. Neuropsychol. 1993;793:364–374. [Google Scholar]
- 5.Zakzanis KK. Distinct neuropsychological profiles in multiple sclerosis subtypes. Arch Clin Neuropsychol. 2013;15:115–136. [PubMed] [Google Scholar]
- 6.Benedict RH, Cookfair D, Gavett R et al. Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) J Int Neuropsychol Soc. 2006;12:549–558. doi: 10.1017/s1355617706060723. [DOI] [PubMed] [Google Scholar]
- 7.Rao S. A Manual for the Brief, Repeatable Battery of Neuropsychological Tests in Multiple Sclerosis. New York, NY: National Multiple Sclerosis Society; 1991. [Google Scholar]
- 8.Langdon DW, Amato MP, Boringa J et al. Recommendation for a Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS) Mult Scler. 2012;18:891–898. doi: 10.1177/1352458511431076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benedict RH, Munschauer F, Linn R et al. Screening for multiple sclerosis using a self-administered 15-item questionnaire. Mult Scler. 2003;9:95–101. doi: 10.1191/1352458503ms861oa. [DOI] [PubMed] [Google Scholar]
- 10.Sullivan M, Edgley K, DeHousx E. A survey of multiple sclerosis, part 1: perceived cognitive problems and compensatory strategy use. Can J Rehabil. 1990;4:99–105. [Google Scholar]
- 11.Benedict RH, Cox D, Thompson LL et al. Reliable screening for neuropsychological impairment in multiple sclerosis. Mult Scler. 2004;10:675–678. doi: 10.1191/1352458504ms1098oa. [DOI] [PubMed] [Google Scholar]
- 12.O'Brien A, Gaudino-Goering E, Shawaryn M et al. Relationship of the Multiple Sclerosis Neuropsychological Questionnaire (MSNQ) to functional, emotional, and neuropsychological outcomes. Arch Clin Neuropsychol. 2007;22:933–948. doi: 10.1016/j.acn.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Benedict RH, Duquin JA, Jurgensen S et al. Repeated assessment of neuropsychological deficits in multiple sclerosis using the Symbol Digit Modalities Test and the MS Neuropsychological Screening Questionnaire. Mult Scler. 2008;14:940–946. doi: 10.1177/1352458508090923. [DOI] [PubMed] [Google Scholar]
- 14.Christodoulou C, Melville P, Scherl WF et al. Perceived cognitive dysfunction and observed neuropsychological performance: longitudinal relation in persons with multiple sclerosis. J Int Neuropsychol Soc. 2005;11:614–619. doi: 10.1017/S1355617705050733. [DOI] [PubMed] [Google Scholar]
- 15.Lovera J, Bagert B, Smoot KH et al. Correlations of Perceived Deficits Questionnaire of Multiple Sclerosis Quality of Life Inventory with Beck Depression Inventory and neuropsychological tests. J Rehabil Res Dev. 2006;43:73–82. doi: 10.1682/jrrd.2004.09.0118. [DOI] [PubMed] [Google Scholar]
- 16.Vogel A, Bhattacharya S, Larsen JL et al. Do subjective cognitive complaints correlate with cognitive impairment in systemic lupus erythematosus? a Danish outpatient study. Lupus. 2011;20:35–43. doi: 10.1177/0961203310382430. [DOI] [PubMed] [Google Scholar]
- 17.Fisk JD, Pontefract A, Ritvo PG et al. The impact of fatigue on patients with multiple sclerosis. Can J Neurol Sci. 1994;21:9–14. [PubMed] [Google Scholar]
- 18.Krupp LB, Alvarez LA, LaRocca NG et al. Fatigue in multiple sclerosis. Arch Neurol. 1988;45:435–437. doi: 10.1001/archneur.1988.00520280085020. [DOI] [PubMed] [Google Scholar]
- 19.Kinsinger SW, Lattie E, Mohr DC. Relationship between depression, fatigue, subjective cognitive impairment, and objective neuropsychological functioning in patients with multiple sclerosis. Neuropsychology. 2010;24:573–580. doi: 10.1037/a0019222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marrie R, Horwitz R, Cutter G et al. The burden of mental comorbidity in multiple sclerosis: frequent, underdiagnosed, and undertreated. Mult Scler. 2009;15:385–392. doi: 10.1177/1352458508099477. [DOI] [PubMed] [Google Scholar]
- 21.Lester K, Stepleman L, Hughes M. The association of illness severity, self-reported cognitive impairment, and perceived illness management with depression and anxiety in a multiple sclerosis clinic population. J Behav Med. 2007;30:177–186. doi: 10.1007/s10865-007-9095-6. [DOI] [PubMed] [Google Scholar]
- 22.Akbar N, Honarmand K, Feinstein A. Self-assessment of cognition in multiple sclerosis: the role of personality and anxiety. Cogn Behav Neurol. 2011;24:115–121. doi: 10.1097/WNN.0b013e31822a20ae. [DOI] [PubMed] [Google Scholar]
- 23.Carone DA, Benedict RH, Munschauer FE et al. Interpreting patient/informant discrepancies of reported cognitive symptoms in MS. J Int Neuropsychol Soc. 2005;11:574–583. doi: 10.1017/S135561770505068X. [DOI] [PubMed] [Google Scholar]
- 24.Bruce JM, Bruce AS, Hancock L et al. Self-reported memory problems in multiple sclerosis: influence of psychiatric status and normative dissociative experiences. Arch Clin Neuropsychol. 2010;25:39–48. doi: 10.1093/arclin/acp092. [DOI] [PubMed] [Google Scholar]
- 25.Amtmann D, Bamer AM, Cook CF et al. University of Washington self-efficacy scale: a new self-efficacy scale for people with disabilities. Arch Phys Med Rehabil. 2012;93:1757–1765. doi: 10.1016/j.apmr.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Motl DC, McAuley E, Snook EM. Physical activity and quality of life in multiple sclerosis: possible roles of social support, self-efficacy, and functional limitations. Rehabil Psychol. 2007;52:143–151. [Google Scholar]
- 27.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 28.Sinnakaruppan I, Macdonald K, McCafferty A et al. An exploration of the relationship between perception of control, physical disability, optimism, self-efficacy and hopelessness in multiple sclerosis. Int J Rehabil Res. 2010;33:26–33. doi: 10.1097/MRR.0b013e32832e6b16. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz CE, Coulthard-Morris L, Zeng Q, Retzlaff P. Measuring self-efficacy in people with multiple sclerosis: a validation study. Arch Phys Med Rehabil. 1996;77:394–398. doi: 10.1016/s0003-9993(96)90091-x. [DOI] [PubMed] [Google Scholar]
- 30.Riazi A, Thompson AJ, Hobart JC. Self-efficacy predicts self-reported health status in multiple sclerosis. Mult Scler. 2004;9:73–81. doi: 10.1191/1352458504ms986oa. [DOI] [PubMed] [Google Scholar]
- 31.Mohr DC, Boudewyn AC, Likosky W et al. Injectable medication for the treatment of multiple sclerosis: the influence of self-efficacy expectations and injection anxiety on adherence and ability to self-inject. Ann Behav Med. 2001;23:125–132. doi: 10.1207/S15324796ABM2302_7. [DOI] [PubMed] [Google Scholar]
- 32.Eccles FJ, Simpson J. A review of the demographic, clinical and psychosocial correlates of perceived control in three chronic motor illnesses. Disabil Rehabil. 2011;33:1065–1088. doi: 10.3109/09638288.2010.525287. [DOI] [PubMed] [Google Scholar]
- 33.Waseem R. Self-efficacy as a predictor of adjustment to multiple sclerosis. J Neurosci Nurs. 1992;24:224–229. doi: 10.1097/01376517-199208000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Schmitt MM, Goverover Y, DeLuca J et al. Self-efficacy as a predictor of self-reported physical, cognitive, and social functioning in multiple sclerosis. Rehabil Psychol. 2014;59:27–34. doi: 10.1037/a0035288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garfield AC, Lincoln NB. Factors influencing anxiety in multiple sclerosis. Disabil Rehabil. 2012;34:2047–2052. doi: 10.3109/09638288.2012.667503. [DOI] [PubMed] [Google Scholar]
- 36.Stuifbergen AK, Becker H, Blozis S et al. A randomized clinical trial of wellness intervention for women with multiple sclerosis. Arch Phys Med Rehabil. 2003;84:467–476. doi: 10.1053/apmr.2003.50028. [DOI] [PubMed] [Google Scholar]


