Orthopaedic manual physical therapy (OMPT) practice incorporates an evidence-based practice (EBP) model, including research integration, clinical expertise, and patient values and circumstances. Contemporary EBP focuses on written words in peer-reviewed research manuscripts, frequently de-emphasizing other critical components. While EBP was originally developed to increase use of epidemiology and statistics in clinician practice, it was never intended to de-emphasize the clinician’s expertise or a patient’s biology, beliefs, and values.1
An explosive growth in peer-reviewed evidence has been witnessed, reaching an almost mythical grandeur in terms of perceived importance for shaping future OMPT clinical practice boundaries. Thus, clinicians face the daunting task of accessing, organizing, and understanding evidence, implementing into meaningful practice patterns.2 Clinicians are faced with time barriers, ease of access and clarity, statistical complexity, poor employer support, and insufficient resources when attempting to become EBP practitioners.3,4
In response, EBP proponents have prioritized studies, based on methodology rigor. One such model, the ‘Sackett solution,’ suggests that the ‘highest’ level of research incorporates a systematic review (SR) or meta-analysis (MA), engendering the greatest confidence in the findings, versus clinician’s observations at the ‘lowest’ level.5 However, the Sackett solution appears to be flawed. First, the study order is based on rigor versus relevance. Authentic evidence-based medicine should have individualized patient care as a top priority.6 Most RCTs or SR/MAs do not exhibit this priority due to inadequate methodology and clinical outcomes. Second, the typical conclusions of a SR/MA paper is ‘no conclusions can be drawn until further numbers of quality papers are published,’ making a ‘reflection on action’ more difficult to manifest in practice.7 Third, if RCTs should be accepted as the optimal guide to clinical decisions, then the evidence to support EBP will be partial or incomplete and of potentially reduced quality, possibly slowing professional practice maturation.8
Do these issues suggest that evidence should be abandoned when fashioning a contemporary clinical practice? Absolutely not. Rather, the clinician–patient team can make appropriate care decisions that may or may not match what the ‘best evidence’ may recommend. While the Sackett solution was important for inspiring clinicians to be mindful of evidence when engaging in practice, an alternative model relocates written evidence from the center of practice and replaces it with patient/clinician interactions (the Evidence-Supported Practice Wheel, Figs. 1 and 2). Here, the patient’s concerns are found at the center of practice, surrounded by the clinician’s observations, judgment, and decisions that comprise sound clinical reasoning. The evidence ‘spokes’ encircling the wheel serves as support for appropriate clinical behaviors and decisions. These spokes can represent different forms of evidence, allowing a research medium that best addresses the patient’s condition and includes all relevant science disciplines. Biopsychosocial constructs and practices comprise the wheel’s ‘rim,’ providing a foundation for consistent care. The clinician’s systematic management approach serves as the management ‘tire,’ providing a conduit of care to the patient. This approach can create an opportunity to develop a ‘Knowledge Transfer,’ which will be facilitated by research that clearly states the findings’ potential clinical relevance.9
Figure 1.
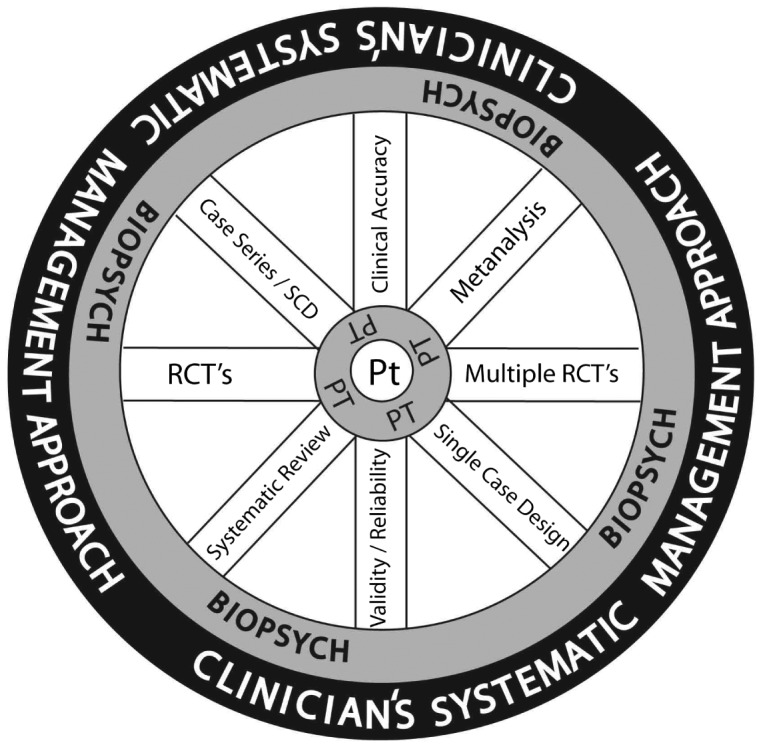
Evidence-supported practice wheel: Pt = patient needs, concerns; PT = clinician’s observations, judgment, and decisions; BIOPSYCH = biopsychosocial constructs; RCT’s = randomized control trials; SCD = single case design.
Figure 2.
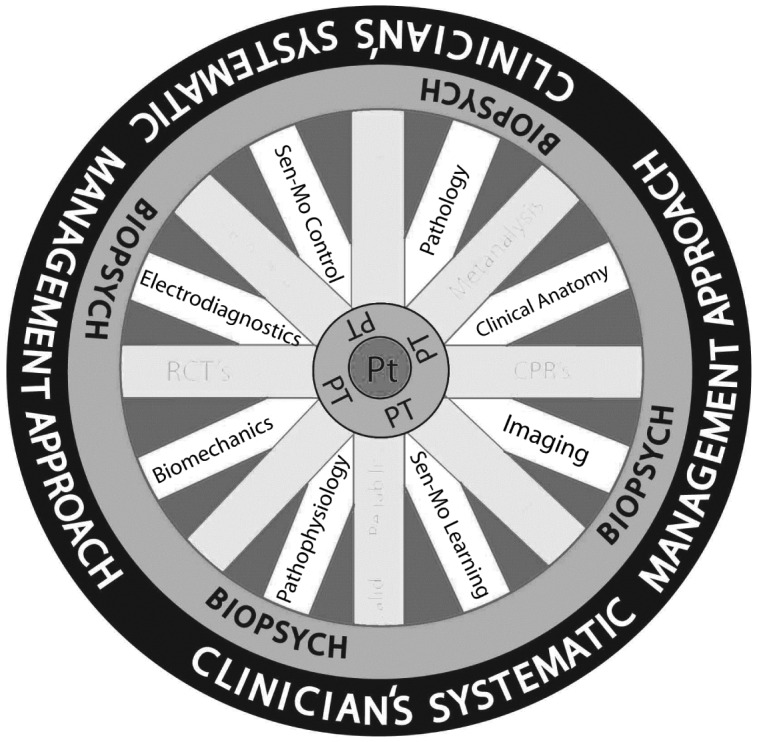
Evidence-supported practice wheel – Considering other diagnostic, basic science and therapeutic evidence as further support to sound clinical reasoning: Pt = patient needs, concerns; PT = clinician’s observations, judgment, and decisions; BIOPSYCH = biopsychosocial constructs.
This Evidence-Supported Practice Wheel addresses several issues. First, the relevance of evidence is addressed, where each study approach (spoke) maintains the highest value at the given time. As the evidence improves in quality, each approach can better support practice patterns. Moreover, each particular approach’s value may vary for each patient, producing diverse values to the clinician during different clinical decisions. For example, the ‘higher rigor’ RCT that supports clinical practice through general inferences could miss the distinction of subject variance. This could preclude a reader’s appreciation for contextually rich clinical descriptions that are commonplace in a case report or single-subject design. These designs, although traditionally considered lower rigor, often reside closest to clinician’s practice realities by: (1) embellishing variance richness; (2) offering consideration to rare conditions or unique clinical combinations; and (3) supporting practice patterns that provide immediate solutions for exploratory processes.
The ‘rim’ (biopsychosocial constructs) that undergirds patient management progress includes emotional (anxiety, frustration, anger),10 cognitive (illogic, distrust, catastrophizing),11 psychological (depression, bipolar tendencies, personality disorders, psychosis),12 contextual (goals, settings, background, circumstances),13 sociocultural (race, culture, gender, ethnicity),14 economic (employment/work status, socioeconomic group),15 and/or communication (observing, listening, perceiving, expressing, responding, reporting)16 influences. Patient care that considers these influences may require effort outside of contemporary evidence, where the patient’s perception of care may be as important as what is actually delivered. This requires a clinician’s adaptation and flexibility, using modifications that maximize patient trust and outcomes. Moreover, the clinician should be encouraged to trust their own clinical judgment, based on systematic and sound practice principles (the ‘tire’) and best available evidence at that time (the ‘spokes’). Doing so can steer the clinician’s self-efficacy regarding their patient management abilities, the patient’s confidence in that clinician’s approach, and the relationship between the patient and clinician that emerges out of a trust contract. The clinician is encouraged to reflect on clinical interaction outcomes and incorporate this new found knowledge into one’s database, where the process can be repeated with each new patient.17
This new model for evidenced-informed practice seeks to return the patient and the clinician’s expertise back to the equation’s epicenter, so to encourage innovative practice. The Sackett evidence hierarchy diagrammatically represented evidence levels based on statistical strength that was proportional to internal validity. Because internal validity can be reciprocal to external validity representing patient generalizability, our proposed patient-centered construct may more accurately demonstrate that different levels of evidence can be applicable, thus informing and supporting the clinician’s practice. In addition, if clinicians find that the patient presentation does not correspond with the current highest available evidence and the observe consistent success in an alternative strategy, then they should be encouraged to utilize that solution in rendering care. Moreover, while a chosen alternative may not be fully supported by presently available evidence and could be considered an outlier, that outlier of today may be the basis for developing future evidence. Thus, choosing that alternative based on sound clinical reasoning places the clinicians in a position to navigate future clinical science discoveries.
References
- 1.Groah SL, Libin A, Lauderdale M, Kroll T, DeJong G, Hsieh J. Beyond the evidence-based practice paradigm to achieve best practice in rehabilitation medicine: a clinical review. PM&R. 2009;1:941–50. 10.1016/j.pmrj.2009.06.001 [DOI] [PubMed] [Google Scholar]
- 2.Rivett DA. Improving clinical reasoning in manual therapy In: Jones MA, Rivett DA, editors. Clinical reasoning for manual therapists. 1st ed Butterworth Heinemann; Philadelphia (PA) 2004. p. 403– 19. [Google Scholar]
- 3.Mota da Silva T, da Cunha Menezes Costa L, Garcia AN, Costa LOP. What do physical therapists think about evidence-based practice? A systematic review. Man Ther. 2015;20:388–401. 10.1016/j.math.2014.10.009 [DOI] [PubMed] [Google Scholar]
- 4.Rosenberg W, Donald A. Evidence based medicine: an approach to clinical problem-solving. BMJ. 1995;310:1122–26. 10.1136/bmj.310.6987.1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sackett DL. Evidence-based medicine. The Lancet. 1995;346:1171–2. 10.1016/S0140-6736(95)91850-7 [DOI] [Google Scholar]
- 6.Greenhalgh T, Howick J, Maskrey N. Evidence based medicine: a movement in crisis? BMJ. 2014;348:g3725.doi: 10.1136/bmj.g3725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wainwright SF, Shepard KF, Harman LB, Stephens J. Novice and experienced physical therapist clinicians: a comparison of how reflection is used to inform the clinical decision-making process. Phys Ther. 2010;90:75–88. 10.2522/ptj.20090077 [DOI] [PubMed] [Google Scholar]
- 8.Dijkers MP, Murphy SL, Krellman J. Evidence-based practice for rehabilitation professionals: concepts and controversies. Arch Phys Med Rehabil. 2012;93(8):S164–S176. 10.1016/j.apmr.2011.12.014 [DOI] [PubMed] [Google Scholar]
- 9.Manns PJ, Darrah J. Linking research and clinical practice in physical therapy: strategies for integration. Physiotherapy. 2006;92:88–94. 10.1016/j.physio.2005.09.006 [DOI] [Google Scholar]
- 10.Esteves JE, Wheatley L, Mayall C, Abbey H. Emotional processing and its relationship to chronic low back pain: results from a case-control study. Man Ther. 2013;18:541–6. 10.1016/j.math.2013.05.008 [DOI] [PubMed] [Google Scholar]
- 11.Thorn BE, Day MA, Burns J, Kuhajda MC, Gaskins SW, Sweeney K, et al. Randomized trial of group cognitive behavioral therapy compared with a pain education control for low-literacy rural people with chronic pain. Pain. 2011;152:2710–20. 10.1016/j.pain.2011.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain. 2014;15(3):221–34. 10.1016/j.jpain.2013.10.014 [DOI] [PubMed] [Google Scholar]
- 13.McCracken LM, Yang S. The role of values in a contextual cognitive-behavioral approach to chronic pain. Pain. 2006;123:137–45. 10.1016/j.pain.2006.02.021 [DOI] [PubMed] [Google Scholar]
- 14.Clara Vélez MC, Palacio C, Isabel Moreno AI, Krikorian A. Psychological and family-related facts of suffering in patients with chronic diseases. Tech Reg Anesth Pain Manag. 2013;17(1):7–10. 10.1053/j.trap.2013.09.002 [DOI] [Google Scholar]
- 15.Groenewald CB, Essner BS, Wright D, Fesinmeyer MD, Palermo TM. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J Pain. 2014;15(9):925–33. 10.1016/j.jpain.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rowbotham S, Holler J, Lloyd D, Wearden A. Handling pain: the semantic interplay of speech and co-speech hand gestures in the description of pain sensations. Speech Commun. 2014;57:244–56. 10.1016/j.specom.2013.04.002 [DOI] [Google Scholar]
- 17.Cohen S. Social relationships and health. Am Psychol. 2004;14(1):482–91. [DOI] [PubMed] [Google Scholar]


