Abstract
Introduction:
There are widespread moves to develop risk-stratified approaches to population-based breast screening. The public needs to favour receiving breast cancer risk information, which ideally should produce no detrimental effects. This study investigates risk perception, the proportion wishing to know their 10-year risk and whether subsequent screening attendance is affected.
Methods:
Fifty thousand women attending the NHS Breast Screening Programme completed a risk assessment questionnaire. Ten-year breast cancer risks were estimated using a validated algorithm (Tyrer-Cuzick) adjusted for visually assessed mammographic density. Women at high risk (⩾8%) and low risk (<1%) were invited for face-to-face or telephone risk feedback and counselling.
Results:
Of those invited to receive risk feedback, more high-risk women, 500 out of 673 (74.3%), opted to receive a consultation than low-risk women, 106 out of 193 (54.9%) (P<0.001). Women at high risk were significantly more likely to perceive their risk as high (P<0.001) and to attend their subsequent mammogram (94.4%) compared with low-risk women (84.2% P=0.04) and all attendees (84.3% ⩽0.0001).
Conclusions:
Population-based assessment of breast cancer risk is feasible. The majority of women wished to receive risk information. Perception of general population breast cancer risk is poor. There were no apparent adverse effects on screening attendance for high-risk women whose subsequent screening attendance was increased.
Keywords: breast cancer, mammography, risk feedback, risk perception
UK deaths from breast cancer have declined by 40% in women <70 years. Some of this fall is attributed to mammographic screening, but widespread use of adjuvant systemic therapies and general improvements in care have also contributed (Parkin et al, 2005; Cancer Research UK, 2014). Unlike many national breast screening programmes, which typically use one or two yearly intervals, the interval between mammograms in the UK National Health Service Breast Screening Programme (NHSBSP) is 3 years. There is evidence that women at high risk of breast cancer (30%+ lifetime risk or 8% 10-year risk – NICE guidelines; McIntosh et al, 2004 updated 2006 and 2013) are more likely to develop interval cancers (Nixon et al, 2000) and reducing the screening interval in this poor prognosis group may be indicated (Porter et al, 2007; Bennett et al, 2011). The Swedish two-county study showed women with a positive family history of breast cancer were more likely to develop breast cancer between their two-yearly screens than women with negative family histories (Nixon et al, 2000). High mammographic density also increases the chances of developing breast cancers as well as interval cancers due possibly to masking effects, suggesting density should be incorporated into risk models (Mandelson et al, 2000; Ciatto et al, 2004). Stratification of screening frequency by risk is likely to be cost effective (Schousboe et al, 2011; Pharoah et al, 2013).
Breast cancer risk is generally assessed using models that include breast cancer family history, reproductive and hormonal history (age at first pregnancy, menarche, menopause, HRT use), height and weight (Gail et al, 1989; Costantino et al, 1999; Tyrer et al, 2004; Amir et al, 2010). Models generally perform well for predicting risk in a population (e.g., 1 in 3 lifetime risk) but not for precise individual risk (Amir et al, 2010).
In the USA, the Gail model is widely used. It is based on age, first-degree relatives with breast cancer, number of surgical breast biopsies and reproductive factors as above (Gail et al, 1989; Costantino et al, 1999). In a comparison of models using UK data, we demonstrated that for women with a family history of breast cancer the Tyrer-Cuzick model performed better than the Gail model; similar results were reported with US data (Boyd et al, 2002; Amir et al, 2003). The Tyrer-Cuzick model has a more extensive familial component and includes HRT, height and weight (Tyrer et al, 2004). Nevertheless, many breast cancers arise in women with no commonly assessed risk factors (Amir et al, 2003).
Mammographic density is an assessable risk factor with the largest population attributable risk and is substantially heritable (Pankow et al, 1997; Boyd et al, 2002). The difference in risk between women with extremely dense, as opposed to predominantly fatty breasts, is approximately four- to six-fold (Santen et al, 2007). Incorporating density into models increases their predictive values (Barlow et al, 2006; Chen et al, 2006).
There are international moves to promote risk-stratified screening, particularly for breast cancer (Schousboe et al, 2011; Evans et al, 2012). For this to happen, risk must be estimated in individuals, communicated to them and to organisers of screening programmes. Breast cancer risk may be assessed best in the context of the screening programme. Here we report the feasibility of this approach in a large population of women screened in northwest England. Since previous studies indicated adding an assessment of mammographic density improved a model's discriminatory power, we also assessed the feasibility of obtaining an estimate of visually assessed mammographic density (Gilbert et al, 2006). Public opinion needs to favour receiving breast cancer risk information if it is to be introduced into screening programmes. Finally, there must be no substantial adverse effects, such as decreased subsequent screening uptake. Specific research questions are: is it feasible to deliver risk assessment in the NHSBSP? Do women want to know their 10-year breast cancer risk estimate? And, does knowing one's risk affect screening attendance?
Materials and methods
All women aged 46–73 years (n=187 466) in 15 screening areas across Greater Manchester invited for routine three-yearly mammographic screening were identified through the UK NHSBSP. Recruitment took place between October 2009 and February 2013. Before screening, 131 373 were mailed information about the Predicting Risk of Cancer At Screening (PROCAS) study, a consent form and questionnaire (http://www.uhsm.nhs.uk/research/Documents/PROCAS%20Questionnaire.pdf). The consent process made clear that participants' breast cancer risk would be assessed and that usual breast cancer screening would continue for non-participants.
Fifty thousand women brought their completed questionnaires to their screening appointment and consented to PROCAS at the time of mammography. A breakdown of participant ages and screening area can be found in Table 1. Questionnaires were entered into the study database, and 10-year breast cancer risk was estimated automatically using the Tyrer-Cuzick model (Tyrer et al, 2004). Participants had at least two opportunities to opt-out of receiving personal breast cancer risk information; first at the time of initial consent (by not ticking a box ‘I wish to know my risk') and later by contacting the study coordinator.
Table 1. Participant ages, ethnicity and screening location.
| Age | Number | Percentage | % of those attended screening |
|---|---|---|---|
| <50 | 3690 | 7.4 | 6.4 |
| 50–54 | 12 909 | 25.8 | 26.2 |
| 55–59 | 10 793 | 21.6 | 21.0 |
| 60–64 | 11 151 | 22.3 | 21.0 |
| 65–69 | 8518 | 17.0 | 17.1 |
| 70+ | 2939 | 5.9 | 8.3 |
| Ethnicity | Percentage GMRa | ||
| White | 45 538 | 91.1 | 82.8 |
| Black or Black British | 516 | 1.0 | 2.76 |
| Asian or Asian British | 679 | 1.4 | 10.15 |
| Mixed | 249 | 0.5 | 2.26 |
| Jewish | 455 | 0.9 | 1.2 |
| Other | 733 | 1.5 | 1 |
| Data not known | 1830 | 3.7 | |
| Area | % of those attended screening | ||
| Manchester | 20 897 | 41.8 | 40.2 |
| Salford | 7914 | 15.8 | 17.1 |
| Trafford | 3723 | 7.5 | 16.5 |
| Tameside | 8695 | 17.4 | 17.4 |
| Oldham | 8758 | 17.5 | 8.8 |
| Other | 13 | 0.0 |
Percentage of the population within the Greater Manchester region (GMR) in each ethnic group. N.B. there are no details held on ethnicity of invitees for screening and it is likely that certain ethnicities, particularly Asian, are under-represented in the older age groups.
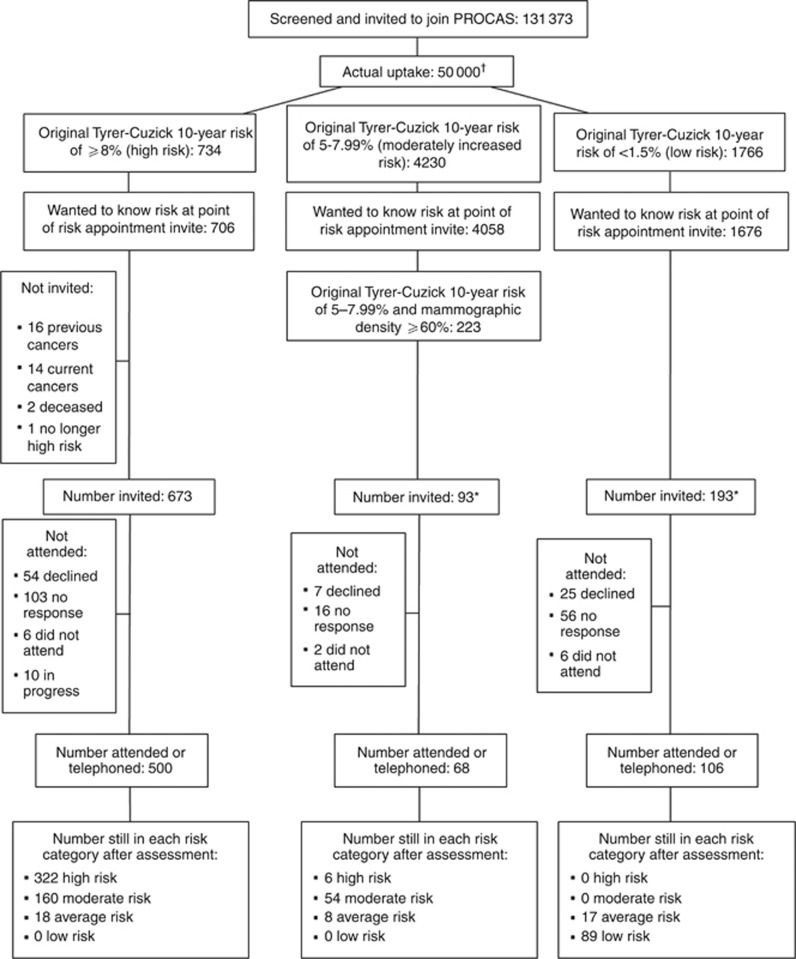
All women with a ⩾8% 10-year risk (Tyrer-Cuzick) of developing breast cancer who were alive and did not have previous or current cancer (673), and a subset (first 93) of those with 5–7.99% 10-year risk and at least 60% mammographic density (high-risk), were invited to receive risk counselling (Figure 1). We were informed by women, their GPs or by checking for updates in the National Breast Screening Service database if women moved out of the screening area. Sixteen women moved out of area and were excluded from further participation. Six did not move out of area but had changed health authority, and therefore screening service. Women were sent a letter explaining the study and were asked to indicate whether they wished to receive risk counselling. Women failing to respond to two invitations were considered as non-responders (Figure 1). In order that participants did not assume their invitation indicated high risk the Patient Information Sheet stated that all women at high risk and a selection of those at low risk would be invited to receive risk counselling. Thus, a subset (first 193) of women screened with a ⩽1.5% 10-year risk (Tyrer-Cuzick) and <10% density were also invited (low-risk), and provided a comparison group. A total of 959 women were given the option of either face-to-face or telephone feedback and risk counselling (see Table 2) by a clinician experienced in risk communication (DGRE and AH). Risk appointments followed a standardised format, based on Leventhal's common sense model of self-regulation of health and illness (Leventhal et al, 2001), with visual representations of the Tyrer-Cuzick risk curve being sent to telephone participants after their appointment. Risk consultations were carried out between March 2010 and August 2014. Women not invited for risk counselling are in the process of receiving their risk by letter. The PROCAS study was approved by Central Manchester Research Ethics Committee (Ref: 09/H1008/81; Evans et al, 2012).
Figure 1.
Consort diagram for first 50 000 in PROCAS. †Original Tyrer-Cuzick 10-year risk of 2–4.99% (average risk): 43 270 not included. *The intention was to invite a small proportion of moderately increased risk with a mammographic density of ⩾60% and low-risk participants, which is why we did not invite the full number of participants in these groups for feedback appointments. No response was to two letter invitations.
Table 2. Information discussed at risk assessment appointments.
| All women (high and low) |
| Their 10-year and lifetime risk of breast cancer |
| What factors – hormonal, reproductive, lifestyle, mammographic density and family history – increased or decreased their risk |
| How future breast cancer risk could be reduced by diet and lifestyle changes – reduced alcohol, more exercise, maintaining a healthy weight or losing weight |
| High-risk women |
| Extra mammographic screening if aged <60 years of age |
| Chemoprevention with tamoxifen and more recently raloxifene (there is no guidance on aromatase inhibitors in the UK) |
Assessment of mammographic density
Mammographic density (percent dense area) was assessed using linear visual-analogue scales during film reading by two readers from a pool of 18 readers (nine radiologists, two breast physicians and seven advanced radiography practitioners), working independently as previously described (Gilbert et al, 2006; Duffy et al, 2008). Women with breast density of >60% and a 10-year Tyrer-Cuzick risk of 5–7.99% were considered high risk with an adjusted 10-year estimate of >8%. Women with breast density of <10% and a Tyrer-Cuzick 10-year risk of <1.5% were considered low risk with an adjusted 10-year risk of below 1%. These adjustments take into account that <10% density is in the lowest fifth and >60% density in the highest fifth of mammographic density at all ages and would be expected to reduce or increase risk by at least 60%, respectively.
Risk perception
Women attending face-to-face appointments were asked to complete a previously validated risk perception questionnaire prior to their risk counselling (Evans et al, 1993, 1994; Hopwood et al, 2001). Women were asked to choose a category indicating their risk compared with the population average (comparative risk) and perceived lifetime risk (absolute risk) for themselves and for women in the general population. The categories given for absolute risk ratings were: ‘inevitable', ‘1 in 2', ‘1 in 8 through 1 in 10', to ‘1 in 200' and ‘very unlikely' (see Table 3 for full range of values). Although the main measure of risk in the present study was 10-year risk, we also gave residual lifetime risk figures to women as part of their risk feedback.
Table 3. Risk perception in high- and low-risk women.
| High ⩾8% 10-year risk not seen in FHC previously | High ⩾8% 10-year risk for those previously seen in FHC | Low <1% 10-year risk | |
|---|---|---|---|
| Number | 275 | 53 | 58 |
|
Comparative risk perception | |||
| (a) Above average risk | 156 (57%) | 35 (66%) | 3 (5%) |
| (b) Average risk | 105 (38%) | 17 (32%) | 38 (66%) |
| (c) Below average risk | 10 (4%) | 1 (2%) | 17 (29%) |
| Not filled in | 4 (2%) | 0 | 0 |
| Chi square for trend compared with low-risk group | 71.9 | 45.7 | |
| P-value for chi square for trend compared with low-risk group | P<0.001 | P<0.001 | |
| P-value for above average risk (a) vs below average risk (c) compared with low-risk group | P<0.001 | P<0.001 | |
|
Perception of individual lifetime risk | |||
| (a) >1 in 4 (inevitable, 1 in 2, 1 in 3) (30–100%-high) | 16/264 (6%) | 6/50 (12%) | 1/57 (2%) |
| (b) 1 in 4 1 in 5 or 1 in 6 (18–25% moderate) | 96 (36%) | 26 (51%) | 11 (19%) |
| (c) Between 1 in 8 and 1 in 10 population risk (10–12%) | 68 (26%) | 7 (14%) | 11 (19%) |
| (d) Between >1 in 10 and <1 in 50 Includes 1 in 20 | 32 (12%) | 4 (8%) | 3 (5%) |
| (e) ⩽1 in 50 (1 in 100; 1 in 200, very unlikely) | 52 (20%) | 7 (14%) | 31 (54%) |
| Chi square for trend compared with low-risk group | 22.4 | 20.8 | |
| P-value for chi square for trend compared with low-risk group | P<0.001 | P<0.001 | |
| P-value for >1 in 8 (a+b) vs <1 in 10 (d+e) compared with low-risk group | P<0.001 | P<0.001 | |
|
Perception of population lifetime risk | |||
| (a) >1 in 4 | 2/270 (1%) | 0/50 (0%) | 0/58 (0%) |
| (b) Between 1 in 4 and 1 in 6 | 65 (24%) | 11 (22%) | 12 (21%) |
| (c) Between 1 in 8 and 1 in 10 | 99 (37%) | 26 (52%) | 19 (33%) |
| (d) Between <1 in 10 and >1 in 50 | 32 (12%) | 3 (6%) | 6 (10%) |
| (e) ⩽1 in 50 | 72 (27%) | 10 (20%) | 21 (36%) |
| Chi square for trend compared with low-risk group | 1.7 | 2.3 | |
| P-value for chi square for trend compared with low-risk group | P=0.18 | P=0.13 | |
| P-value for >1 in 8 (a+b) vs <1 in 10 (d+e) compared with low-risk group | P=0.36 | P=0.29 | |
| P-value for population risk (c) vs <1 in 10 (d+e) compared with low-risk group | P=0.41 | P=0.03 | |
Abbreviation: FHC=Family History Clinic.
Breast cancers
We are automatically informed of breast cancers in subjects identified on screening. Interval cancers are notified to us by subjects and also from regular checks on the North West Cancer Intelligence Service.
Statistics
Fisher's exact test was used to make two-by-two comparisons (e.g., below average vs above average, >1 in 8 vs <1 in 10). A chi-square test for linear trend was used to compare ordered categorical data. Differences in independent proportions with approximate binomial confidence intervals uptake of risk counselling and subsequent screening, compared with the high risk group (Miettinen and Nurminen, 1985). All statistical tests were two-sided and a P-value of <0.05 considered as statistically significant. StatsDirect version 3 (StatsDirect Ltd, www.statsdirect.com) was used for statistical analysis. A sample size of 176 participants in each group was required to detect a 15% difference in uptake to counselling between the high- and low-risk groups based on a 70% response rate in the high-risk group, with 80% power and a confidence level of 95%.
Results
Of 187 466 women invited for mammography between October 2009 and February 2013, 131 373 attended their screening appointment and were invited to join the PROCAS study. Fifty thousand women consented (38% of screening attendees) (Figure 1). Their ages ranged from 46 to 84 years (a small number aged >73 opted into screening/PROCAS), with a median age at entry of 58 years. Of those consenting 11 852 (23.7%) were attending their first screen and the remainder (76.7%) attending an incident screen.
Identification and counselling of high- and low-risk women
Two groups of women were identified as having high breast cancer risk; those with a Tyrer-Cuzick 10 year risk of ⩾8%, and those with a Tyrer-Cuzick risk of 5–7.99% plus mammographic density ⩾60%. There were 734 (1.5%) with a Tyrer-Cuzick 10 year risk ⩾8% and 223 (0.45%) with a Tyrer-Cuzick risk of 5–7.99% plus mammographic density ⩾60%, 957 in total. Of these 957, 766 were invited to discuss their risk with a clinician (DGRE/AH; Figure 1). A further 193 women from the low-risk group were invited to discuss their risk and to give reasonable power to differentiate uptake between the high- and low-risk groups. We halted inviting those with a Tyrer-Cuzick risk of 5–7.99% plus mammographic density ⩾60% at 93 as there were no differences between this group and the high-risk group.
Women were give the option of receiving their risk by telephone or face-to-face appointment. Of women with a Tyrer-Cuzick 10-year risk ⩾8%, 271 chose telephone vs 229 face-to-face consultations. Of women with a Tyrer-Cuzick score of 5–7.99% and ⩾60% density, 37 chose telephone vs 31 face-to-face consultations. Of women with a Tyrer-Cuzick score of <1.5% and <10% density, 70 chose telephone vs 36 face-to-face consultations. There was no significant difference in method of risk delivery between the three groups (chi square=5.06, P=0.08).
High-risk women
Of women with Tyrer-Cuzick 10-year risk ⩾8%, 706 out of 734 (96.2%) originally indicated that they wanted risk feedback, 33 were ineligible and thus 673 were invited for counselling (Table 4; Figure 1). Of these, 163 (24.2%) declined or did not attend their risk appointment. The remainder attended or had telephone risk counselling, with 10 still in progress. Twenty-eight non-attenders had previously attended our Family History Clinic (FHC). A similar proportion with Tyrer-Cuzick score of 5–7.99% and ⩾60% density originally wanted to know their risk (95.9%), and 68 out of 93 (73.1%) attended.
Table 4. Uptake of risk counselling and next round screening in attendees of risk counselling.
| Number | Number invited | Uptake of risk counselling, compared with high risk | Uptake of next screening round, compared with high risk attendeda | All breast cancers since entry | Percentage with breast cancer | |
|---|---|---|---|---|---|---|
| High risk 8%+ | 734 | 673 | 500 (74.3%)* | 271/287 (94.4%)** | 26/673 | 3.9 |
| Moderate risk | 223 | 93 | 68 (73.1%) | 56/58(96.5%) | 6/223 | 2.7 |
| 5–7·9% ⩾60% density | Difference: 1.2% (95% CI −8% to 11%)* | Difference: −2.1% (95% CI −6% to 6%)** | ||||
| P=0.8 | P=0.54 | |||||
| Low risk <1% (<1·5% with <10% density) | 271 | 193 | 106 (54.9%) | 64/76 (84.2%) | 2/271 | 0.7 |
| Difference: 19.4% (95% CI 12–27%)* | Difference: 10.2% (95% CI 3–20%)** | |||||
| P<0.001 | P=0.004 | |||||
| High-risk non-attenders (i.e., those invited to a risk appointment but did not attend) | 173 | — | 0 | 89/115 (77.4%) Difference: 17.0% (95% CI 9% to 26%)** P<0.0001 | — | |
| Low-risk non-attenders (i.e., those invited to a risk appointment but did not attend) | 87 | — | 0 | 55/69 (79.7%) Difference: 14.7% (95% CI 6% to 26%)** | — | |
| P=0.0002 | ||||||
| All women in Greater Manchester who attended previous round 2012–2013 | 39 058 | — | — | 32 925 (84.3%) Difference: 10.1% (95% CI 7% to 12%)** P<0.0001 | — |
Key: comparisons of the difference between independent proportions with 95% confidence interval and P-value.
* and ** Comparison for P value with high-risk attendees.
Denominator is based on the number of women who have been invited and are eligible for their next three-yearly screen.
Thus far, 568 high risk women have received risk counselling during which questionnaire details (family history, individual hormonal and lifestyle factors) were confirmed. Consequently, a number of women (160 out of 500, 32%) originally identified as high-risk (Tyrer-Cuzick score >8%) were re-assessed as moderately increased risk (Tyrer-Cuzick score 5–7.99%) and 18 out of 500 (3.6%) as average risk, based on Tyrer-Cuzick risk program v6. For the original 500 with ⩾8% 10-year risk there was a mean reduction in 10-year risk of 1.3% after addition of further unaffected female relatives and adjustment of other risk factors. Of those seen with (5–7.99%) risk and >60% density, 8 out of 68 (12%) fell below the 5% 10-year risk on re-evaluation and thus dropped out of the high-risk group (Figure 1).
Referral for additional 12–18-monthly screening as indicated in NICE guidelines (only eligible aged <60 years) was offered to 383 eligible women in both high-risk categories of which 4 declined, and 298 (77.8%) have taken up the offer. Forty were already receiving screening through the FHC. Thus 338 of 383 (88.2%) are having additional screening. In this group, four small breast cancers were detected on the interval 18-month breast screen (Table 5).
Table 5. Breast cancers identified on interval screening.
| Individual | Age (years) | Cancer |
|---|---|---|
| 1 | 54 | 7 mm grade 1 node-negative invasive ductal carcinoma (IDC) |
| 2 | 63 | 28 mm grade 3 node-positive IDC with ductal carcinoma in situ (DCIS) |
| 3 | 58 | 25 mm focus and 7 mm focus of grade 2 node-negative invasive lobular carcinoma with lobular carcinoma in situ (LCIS) |
| 4 | 51 | Grade 2 IDC 10 mm and a separate 4.5 mm focus of grade 1 node-negative invasive tubular carcinoma with DCIS |
Low-risk women
Of those at low-risk (Tyrer-Cuzick score of <1.5% and <10% density), 94.9% originally wished to know their risk. A total of 193 were offered risk consultation and 106 out of 193 (54.9%) attended a risk appointment. Women at high risk were significantly more likely to attend a risk appointment/telephone call than women at low risk (Table 4; P<0.0001).
Cancers
Overall, 26 cancers (3.9%) occurred in the 673 eligible women with an original Tyrer-Cuzick ⩾8% 10-year risk (Table 4). Thirteen were identified on a mammogram at study entry, four on an interval mammogram and nine on their subsequent follow-up mammogram after 3 years. There were 87 cancers (2.1%) in the 4230 women with a Tyrer-Cuzick 5–7.99% 10-year risk, of which 41 were identified at study entry, 20 between screens and 26 on their subsequent three yearly mammogram. Six occurred in women with increased mammographic density (⩾60%) (Table 4). There were only 18 breast cancers (1.0%) in the 1766 women with <1.5% 10-year risk of which 8 were identified at study entry, 4 between screens and 6 on their subsequent screening mammogram, and only 2 cancers occurred in those with mammographic density <10%.
Re-attendance at screening
Figures from the 2012–2013 Greater Manchester NHSBSP showed that among women who attended their previous mammogram and whose last screen was within the last 5 years, 39 058 were invited and 32 925 (84.3%) attended.
For women confirmed as high risk (Tyrer-Cuzick ⩾8%) at their risk feedback (n=328–322 originally high risk and 6 originally moderate risk; Figure 1), the re-attendance rate at the next 3-year screening was 94.4% (271 out of 287). Re-attendance for those who were originally high risk (Tyrer-Cuzick ⩾8%) and who did not attend their risk appointment was significantly lower at 77.4% (89 of 115) (P<0.0001; Table 4).
For women confirmed as low risk (Tyrer-Cuzick<1.5%) at their risk feedback (n=89), the re-attendance rate at the next 3-year screening was lower for the 76 called (84.2%) compared with high-risk attenders (95% P=0.004).
Overall re-attendance at the next three-yearly screen for women who attended their risk appointments for all three risk categories was 92.9% (391 out of 421). Re-attendance was significantly higher for high-risk women invited for feedback (P<0.0001) than usual re-attendance rates in Greater Manchester, but was not significantly lower for low-risk attenders and non-counselled women.
Risk perception
Three-hundred and twenty-eight of 568 (58%) high-risk and 58 of 106 (55%) low-risk women completed risk perception questionnaires. Fifty-three high-risk women had previously attended the FHC for risk assessment between 1990 and 2010 (median=1996) some 4–24 years (median=15) prior to their risk assessment in PROCAS. High-risk women ascribed higher comparative risk categories to themselves than low-risk women (Table 3; P<0.001) and previously counselled women had more accurate risk perceptions for themselves and for the general population than low-risk women's perceptions. When asked to estimate the risk for the general population, only a minority (37% high, 33% low) gave the ‘correct' current lifetime risk range of 10–12%. Meanwhile 52% of women who had previously received risk counselling gave the correct current lifetime risk of breast cancer for the general population. Receipt of risk information did not significantly change low-risk women's intentions to attend subsequent mammograms, with only one expressing a desire to cease screening.
Discussion
This is the first study to show it is possible to collect and feedback risk information to women at both high and low risk of breast cancer, in the context of a population-based mammographic screening programme. Women at high risk were more likely, than those at low-risk, to perceive their risk as elevated prior to counselling. This is most likely due to the presence of a family history of breast cancer. Accordingly, both attendance at risk counselling (74% in high risk vs 55% in low risk, P⩽0.0001) and re-attendance at the subsequent mammography screen (92% vs 84%, respectively, P=0.05) were higher in women counselled at high risk compared with those with low risk. Indeed, high-risk women were more likely to re-attend subsequent mammography than women in the general screening population. Low-risk women were reluctant to discontinue screening. It is reassuring to screening programmes, which are judged by the re-attendance rate, there was not a significant drop in attendance at the subsequent screen after risk assessment is introduced.
Women at high lifetime risk of breast cancer are now recommended annual mammography screening between 40 and 60 years in the UK (McIntosh et al, 2004 updated 2006 and 2013). There was a high uptake of additional screening in high-risk women in PROCAS, and the 11% not referred by their GP may be the GP's decision rather than the woman's. It is reassuring that not only does Tyrer-Cuzick reliably identify women at high risk (the 3% detection rate can be considered to represent a 3-year period including lead time – thus 1% annually or 10% over 10 years), but that >1% of those detected on additional screening have extremely good prognosis stage-1 cancers. While these numbers are small, for cancers detected on interval screens they represent an extremely high rate (4 of 280 extra screens). Since all occurred in women <63 even the grade 1 cancer would likely have presented in the woman's lifetime and might not be considered an ‘over-diagnosis'.
This study has also assessed risk perception. Unlike previous studies that were based mainly on women with concerns about their breast cancer risk due to family history (Evans et al, 1993, 1994; Hopwood et al, 2001), the present study addresses risk perceptions of women at either end of the spectrum from the general population, the majority of whom had not been assessed previously. Risk perception was, as reported previously not overly accurate (Evans et al, 1993; McCaul and O'Donnell, 1998; Hopwood et al, 2001), with 66% of low-risk women rating themselves at ‘average' risk. High-risk women were more likely to assess their risk as above average compared with low-risk women, in both comparative and absolute terms. Perception of population risk was not statistically significantly different between the two previously uncounselled groups. However, those seen previously in the FHC had more accurate overall risk perception as previously reported (Evans et al, 1994). This finding supports the efficacy of counselling in a health-care setting at producing accurate risk perceptions, in contrast to the mere provision of risk in settings outside of the health-care system (Dillard et al, 2006; Paci et al, 2013). Being informed of one's risk did not impact on intentions to change screening behaviour. This is in opposition to the weight of cross-sectional studies (McCaul et al, 1996) but in line with evidence from prospective studies where the more affective construct of cancer worry is a more consistent predictor of mammography attendance (Hay et al, 2006; Walker et al, 2014).
There are limitations to the present study. The 38% uptake may have biased the population to women with higher risks. A survey alongside our FHC did not suggest this was the case (Evans et al, 2014). The drop-off from ∼95% wishing to receive risk information and who then declined is disappointing, and from women's comments is largely down to inconvenience. It is likely uptake would have been much higher if a letter giving feedback had been offered. Our original report on the first 10 000 women noted that uptake to PROCAS was lower in areas with higher deprivation as was uptake to screening (Evans et al, 2012). This trend has continued and there were no other biases we could detect, with uptake similar across age groups, except a slightly higher uptake in women attending their first screening appointment (Evans et al, 2012). The present report adds data on risk perception, follow-up and re-attendance and accuracy of risk prediction (risk perception was based on a validated questionnaire that used lifetime risk as opposed to 10-year risk). Although uptake to PROCAS is relatively low, it rises to 60% when dedicated study staff are present at the time of screening, and would likely rise further if it became a routine part of screening rather than a ‘study'. We have not conducted a formal assessment of the impact of risk information on anxiety and intention to change behaviour although this is planned in a new prospective arm to the study. There were some inaccuracies in completion of the questionnaires, particularly in relation to bilateral disease and timing of the menopause. In future, an online version of the questionnaire with prompts and pop up questions is likely to improve accuracy. Certainly if only a paper questionnaire is used, confirming details in those whose management may change is important as risk category may change substantially. We believe an online questionnaire with prompts and an inbuilt risk algorithm, such as Tyrer-Cuzick, which could also incorporate automatic measurement of mammographic density, is likely to be the most feasible way forward to provide accurate risk provision. This would be an absolute requirement if risk stratified screening were to be implemented.
In conclusion, the present study has shown it is feasible to obtain risk information in the context of a national breast screening programme. It is also feasible to feedback risk information to women taking part in population-based breast screening. For practical deployment at-scale, automation of processes will be necessary, ideally with interactive online data-capture and error-correction. Further research is necessary to find the safest and most effective means to feedback risk information, especially to high-risk women and, in particular, who should be responsible for their management. For example, what accompanying information about risk reduction strategies is required? Is an accompanying leaflet sufficient? Overall it is encouraging that reattendance rates are extremely high in those fed-back high-risks. It seems likely that interval cancer rates could be reduced and overall outcome after diagnosis improved, but this requires further investigation. Further breast cancer risk could be reduced by the offer of preventive therapy in women detected to be at moderate/high risk (McIntosh et al, 2004 updated 2006 and 2013).

Acknowledgments
We thank the study radiologists: Dr Anthony Maxwell, Professor Caroline Boggis, Dr Emma Hurley, Dr Megan Bydder, Dr Mary Wilson, Dr Nicky Barr, Prof Anil Jain, Dr Sara Bundred, Dr Soujanya Gadde, Dr Ursula Beetles, Dr Yit Yoong Lim, Dr Rumana Rahim and advanced radiography practitioners: Amanda Bath, Valerie Reece, Miriam Griffiths, Elizabeth Lord, Rita Borgen and Jill Johnson for mammography reporting. This work was supported by the National Institute for Health Research (NIHR) and Genesis Breast Cancer Prevention Appeal (reference: GA10-033 and GA13-006). This paper presents independent research funded by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research (grant reference number RP-PG-0707-10031). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. We also acknowledge the support of MRC grant HeRC MR/K006665/1.
Author contributions
DGRE, SMA, MW, JC and AH conceived and designed the study. DGRE and AH are the responsible clinicians giving risk feedback to women. MW and UB are the consultant radiologists who led the reviews of mammograms. PS and SD organised the conduct of the study. PS, SD and LF carried out the study (including acquiring the study data). DGRE and EFH analysed and interpreted the data. DGRE, LSD, SMA, PS, SD, EFH, JCS, MNH, IB, ARB, DPF, JC, MW, SI, UB and AH contributed towards writing and review of the manuscript. All authors have read and approved the final version of the manuscript.
The authors declare no conflict of interest.
Footnotes
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
References
- Amir E, Evans DG, Shenton A, Lalloo F, Moran A, Boggis C, Wilson M, Howell A (2003) Evaluation of breast cancer risk assessment packages in the family history evaluation and screening programme. J Med Genet 40: 807–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir E, Freedman OC, Seruga B, Evans DG (2010) Assessing women at high-risk of breast cancer: a review of risk assessment models. J Natl Cancer Inst 102: 680–691. [DOI] [PubMed] [Google Scholar]
- Barlow WE, White E, Ballard-Barbash R, Vacek PM, Titus-Ernstoff L, Carney PA, Tice JA, Buist DS, Geller BM, Rosenberg R, Yankaskas BC, Kerlikowske K (2006) Prospective breast cancer risk prediction model for women undergoing screening mammography. J Natl Cancer Inst 98: 1204–1214. [DOI] [PubMed] [Google Scholar]
- Bennett RL, Sellars SJ, Moss SM (2011) Interval cancers in the NHS breast cancer screening programme in England, Wales and Northern Ireland. Br J Cancer 104(4): 571–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd NF, Dite GS, Stone J, Gunasekara A, English DR, McCredie MR, Giles GG, Tritchler D, Chiarelli A, Yaffe MJ, Hopper JL (2002) Heritability of mammographic density, a risk factor for breast cancer. NEngl J Med 347: 886–894. [DOI] [PubMed] [Google Scholar]
- Cancer Research UK (2014) http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer/mortality#ref-2 (accessed July 2015).
- Chen J, Pee D, Ayyagari R, Graubard B, Schairer C, Byrne C, Benichou J, Gail MH (2006) Projecting absolute invasive breast cancer risk in white women with a model that includes mammographic density. J Natl Cancer Inst 98: 1215–1226. [DOI] [PubMed] [Google Scholar]
- Ciatto S, Visioli C, Paci E, Zappa M (2004) Breast density as a determinant of interval cancer at mammographic screening. Br J Cancer 90: 393–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantino JP, Gail MH, Pee D, Anderson S, Redmond CK, Benichou J, Wieand HS (1999) Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst 91: 1541–1548. [DOI] [PubMed] [Google Scholar]
- Dillard AJ, McCaul KD, Kelso PD, Klein WM (2006) Resisting good news: reactions to breast cancer risk communication. Health Commun 19: 115–123. [DOI] [PubMed] [Google Scholar]
- Duffy SW, Nagtegaal ID, Astley SM, Gillan MG, McGee MA, Boggis CR, Wilson M, Beetles UM, Griffiths MA, Jain AK, Johnson J, Roberts R, Deans H, Duncan KA, Iyengar G, Griffiths PM, Warwick J, Cuzick J, Gilbert FJ (2008) Visually assessed breast density, breast cancer risk and the importance of the craniocaudal view. Breast Cancer Res 10: R64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DGR, Burnell LD, Hopwood P, Howell A (1993) Perception of risk in women with a family history of breast cancer. Br J Cancer 67: 612–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DGR, Blair V, Greenhalgh R, Hopwood P, Howell A (1994) The impact of genetic counselling on risk perception in women with a family history of breast cancer. Br J Cancer 70: 934–938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DG, Warwick J, Astley SM, Stavrinos P, Sahin S, Ingham S, McBurney H, Eckersley B, Harvie M, Wilson M, Beetles U, Warren R, Hufton A, Sergeant JC, Newman WG, Buchan I, Cuzick J, Howell A (2012) Assessing individual breast cancer risk within the UK National Health Service Breast Screening Programme: a new paradigm for cancer prevention. Cancer Prev Res (Phila) 5(7): 943–951. [DOI] [PubMed] [Google Scholar]
- Evans DGR, Brentnall AR, Harvie M, Dawe S, Sergeant JC, Stavrinos P, Astley S, Wilson M, Ainsworth J, Cuzick J, Buchan I, Donnelly LS, Howell A (2014) Breast cancer risk in young women in the National Breast Screening Programme: implications for applying NICE guidelines for additional screening and chemoprevention. Cancer Prev Res (Phila) 7(10): 993–1001. [DOI] [PubMed] [Google Scholar]
- Gail MH, Brinton LA, Byar DP, Corle DK, Green SB, Schairer C, Mulvihill JJ (1989) Projecting individulized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst 81: 1879–1886. [DOI] [PubMed] [Google Scholar]
- Gilbert FJ, Astley SM, McGee MA, Gillan MG, Boggis CR, Griffiths PM, Duffy SW (2006) Single reading with computer aided detection and double reading of screening mammograms in the United Kingdom National Breast Screening Program. Radiology 241: 47–53. [DOI] [PubMed] [Google Scholar]
- Hay JL, McCaul KD, Magnan RE (2006) Does worry about breast cancer predict screening behaviors? A meta-analysis of the prospective evidence. Prev Med 42: 401–408. [DOI] [PubMed] [Google Scholar]
- Hopwood P, Shenton A, Lalloo F, Evans DG, Howell A (2001) Risk perception and cancer worry: an exploratory study of the impact of genetic risk counselling in women with a family history of breast cancer. J Med Genet 38: 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal H, Leventhal EA, Cameron L (2001) Representations, procedures and affect in illness self-regulation: a perceptual-cognitive model. In A Baum, TA Revenson, JE Singer, (eds) Handbook of Health Psychology pp 19–47. Lawrence Erlbaum Associates: Mahwah, NJ, USA. [Google Scholar]
- Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, White E (2000) Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst 92: 1081–1087. [DOI] [PubMed] [Google Scholar]
- McCaul KD, Branstetter AD, Schroeder DM, Glasgow RE (1996) What is the relationship between breast cancer risk and mammography screening? A meta-analytic review. Health Psychol 15: 423–429. [DOI] [PubMed] [Google Scholar]
- McCaul DF, O'Donnell SM (1998) Naïve beliefs about breast cancer risk. Seomen's Health Res Gender Behav Policy 4: 93–101. [PubMed] [Google Scholar]
- McIntosh A, Shaw C, Evans G, Turnbull N, Bahar N, Barclay M, Easton D, Emery J, Gray J, Halpin J, Hopwood P, McKay J, Sheppard C, Sibbering M, Watson W, Wailoo A, Hutchinson A (2004 updated 2006 and 2013) Clinical Guidelines and Evidence Review for The Classification and Care of Women at Risk of Familial Breast Cancer. National Collaborating Centre for Primary Care/University of Sheffield: London, NICE guideline CG041/CG164 www.nice.org.uk. [Google Scholar]
- Miettinen OS, Nurminen M (1985) Comparative analysis of two rates. Stat Med 4: 213–226. [DOI] [PubMed] [Google Scholar]
- Nixon RM, Pharoah P, Tabar L, Krusemo UB, Duffy SW, Prevost TC, Chen HH (2000) Mammographic screening in women with a family history of breast cancer: some results from the Swedish two-county trial. Rev Epidémiol Santé Publique 48: 325–331. [PubMed] [Google Scholar]
- Paci E, Mantellini P, Giorgi Rossi P, Falini P, Pulido D TBST Working Group (2013) Tailored Breast Screening Trial (TBST). Epidemiol Prev 37: 317–327. [PubMed] [Google Scholar]
- Pankow JS, Vachon CM, Kuni CC, King RA, Arnett DK, Grabrick DM, Rich SS, Anderson VE, Sellers TA (1997) Genetic analysis of mammographic breast density in adult women: evidence of a gene effect. J Natl Cancer Inst 89: 549–556. [DOI] [PubMed] [Google Scholar]
- Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55: 74–108. [DOI] [PubMed] [Google Scholar]
- Pharoah PD, Sewell B, Fitzsimmons D, Bennett HS, Pashayan N (2013) Cost effectiveness of the NHS breast screening programme: life table model. BMJ 346: f2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter GJ, Evans AJ, Burrell HC, Lee AH, Chakrabarti J (2007) NHSBSP type 1 interval cancers: a scientifically valid grouping? ClinRadiol 62(3): 262–267. [DOI] [PubMed] [Google Scholar]
- Santen R, Boyd N, Chlebowski RT, Cummings S, Cuzick J, Dowsett M, Easton D, Forbes JF, Key T, Hankinson SE, Howell A, Ingle J Breast Cancer Prevention Collaborative Group (2007) Critical assessment of new risk factors for breast cancer: considerations for development of an improved risk prediction model. Endocr Relat Cancer 14: 169–187. [DOI] [PubMed] [Google Scholar]
- Schousboe JT, Kerlokowske K, Loh A, Cummings SR (2011) Personalizing mammography by breast density and other risk factors for breast cancer: analysis of health benefits and cost-effectiveness. Ann Intern Med 155: 10–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer J, Duffy SW, Cuzick J (2004) A breast cancer prediction model incorporating familial and personal risk factors. Stat Med 23: 1111–1130. [DOI] [PubMed] [Google Scholar]
- Walker MJ, Mirea L, Glendon G, Ritvo P, Andrulis IL, Knight JA, Chiarelli AM (2014) Does perceived risk predict breast cancer screening use? Findings from a prospective cohort study of female relatives from the Ontario site of the Breast Cancer Family Registry. Breast 23: 482–488. [DOI] [PMC free article] [PubMed] [Google Scholar]