Abstract
Objectives. We examined the associations of job strain, an indicator of work-related stress, with overall unhealthy and healthy lifestyles.
Methods. We conducted a meta-analysis of individual-level data from 11 European studies (cross-sectional data: n = 118 701; longitudinal data: n = 43 971). We analyzed job strain as a set of binary (job strain vs no job strain) and categorical (high job strain, active job, passive job, and low job strain) variables. Factors used to define healthy and unhealthy lifestyles were body mass index, smoking, alcohol intake, and leisure-time physical activity.
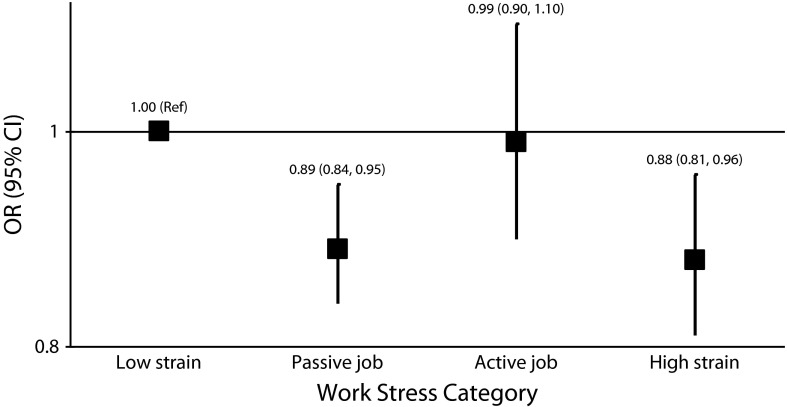
Results. Individuals with job strain were more likely than those with no job strain to have 4 unhealthy lifestyle factors (odds ratio [OR] = 1.25; 95% confidence interval [CI] = 1.12, 1.39) and less likely to have 4 healthy lifestyle factors (OR = 0.89; 95% CI = 0.80, 0.99). The odds of adopting a healthy lifestyle during study follow-up were lower among individuals with high job strain than among those with low job strain (OR = 0.88; 95% CI = 0.81, 0.96).
Conclusions. Work-related stress is associated with unhealthy lifestyles and the absence of stress is associated with healthy lifestyles, but longitudinal analyses suggest no straightforward cause–effect relationship between work-related stress and lifestyle.
Behavior-related modifiable health risk factors, such as smoking and physical inactivity, are major contributors to the noncommunicable disease burden and mortality worldwide.1 These factors tend to cluster at the population level, with some people having multiple health risk factors (an overall unhealthy lifestyle) and others having multiple health-promoting factors (an overall healthy lifestyle)2,3; the causes of this clustering are not well understood, however. Work-related psychosocial stress may be one (possibly modifiable) factor influencing or contributing to adoption or maintenance of a healthy or unhealthy lifestyle. For instance, some people who experience stress may not find time to exercise or eat a healthy diet, or they may attempt to alleviate stress by smoking or drinking excessive amounts of alcohol, whereas others may choose healthy behaviors (e.g., exercise) as a way of coping with stress.4
Work and workplace-related issues are common sources of stress. A better understanding of the association between work-related stress and overall health-related lifestyle is important because there is evidence from studies of cardiovascular diseases and cancer that combinations of lifestyle risk factors may induce larger risks of adverse health outcomes than the sum of the separate effects of the same factors2,5–7; there is also evidence that the co-occurrence of multiple healthy lifestyle factors has a protective effect against many diseases, including stroke and cancer.8–10 Psychosocial stress at work has been shown to be associated with individual unhealthy lifestyle factors such as smoking,11–14 heavy alcohol consumption,15–17 physical inactivity,18–21 and obesity.22–26 However, the relationship between work-related stress and the co-occurrence of healthy and unhealthy lifestyle factors remains poorly understood.
We investigated the associations of work-related psychosocial stress, operationalized as job strain, with overall healthy and unhealthy lifestyles, operationalized as the co-occurrence of unhealthy and healthy lifestyle factors. We hypothesized that the association between job strain and health-related lifestyles would be stronger than the association between job strain and each individual unhealthy lifestyle factor. To examine these issues, we conducted a meta-analysis of data from 11 prospective European cohort studies.
METHODS
We used pooled individual-level data from 11 studies conducted in 6 European countries: Belstress (Belgium)27; the Finnish Public Sector Study (FPS; Finland)28; Gazel (France)29; the Health and Social Support Study (HeSSup; Finland)30; the Heinz Nixdorf Recall Study (HNR; Germany)31; Kooperative Gesundheitsforschung in der Region Augsburg studies 1, 2, and 3 (KORA 1–3; Germany)32; the Whitehall II Study (United Kingdom)33; and Work, Lipids, and Fibrinogen (WOLF) Norrland and Stockholm (Sweden).34,35
Each of these studies was part of the IPD-Work (Individual-Participant Data Meta-analysis of Working Populations) Consortium, a collaborative meta-analysis project established at the Four Centers Initiative meeting (a meeting of stress researchers from University College London, the Institut National de la Santé et de la Recherche in Paris, the University of Dusseldorf in Germany, and Karolinska Institutet in Stockholm) in London in 2008.36 The overall aim of the consortium is to investigate the relationships between work-related psychosocial stress and disease. Details on the design and samples of the individual studies included in our analyses have been published previously (brief descriptions, with references to previous publications, are provided in Appendix A, available as a supplement to the online version of this article at http://www.ajph.org).
Ascertainment of Lifestyle Factors
The health-related lifestyle factors assessed in our study were body mass index (BMI), tobacco smoking, alcohol intake, and leisure-time physical activity. BMI (defined as weight in kilograms divided by the square of height in meters) was calculated from participants’ height and weight, which were self-reported in 3 studies (FPS, Gazel, HeSSup) and measured at a medical examination in the other 8 studies (Belstress, HNR, KORA 1–3, Whitehall II, WOLF Stockholm, and WOLF Norrland). We grouped BMIs into 3 categories (according to the World Health Organization’s recommendations37), as follows: underweight (< 18.5 kg/m2), normal weight (18.5–25 kg/m2), and overweight (≥ 25 kg/m2).
We ascertained smoking, alcohol intake, and physical activity status from participant-completed questionnaires in all studies. Participants were classified as nonsmokers (including those who had never smoked and ex-smokers) or current smokers. Alcohol intake was ascertained according to the total number of alcoholic drinks participants consumed in a week (1 drink was defined as approximately equivalent to 10 g of ethanol). Participants were grouped into 3 categories: nondrinkers, moderate drinkers (women: 1–14 drinks/week; men: 1–21 drinks/week), and heavy drinkers (women: ≥ 15 drinks/week; men: ≥ 22 drinks/week). This categorization was based on current public health guidelines and estimated thresholds for harmful alcohol intake.38–40
We categorized leisure-time physical activity according to the World Health Organization’s recommendations on the minimum amount of activity that confers health benefits.41 Individuals were classified as either inactive (no physical activity, < 2.5 hours of moderate activity/week, or < 1.25 hours of vigorous activity/week) or active (≥ 2.5 hours of moderate activity/week or ≥ 1.25 hours of vigorous activity/week).
Definitions of Healthy and Unhealthy Lifestyles
We defined a healthy lifestyle as having 4 healthy lifestyle factors: being normal weight (BMI = 18.5–24.9 kg/m2), being a nonsmoker, drinking moderate amounts of alcohol, and being physically active during leisure time. An unhealthy lifestyle was defined as having 4 unhealthy lifestyle factors: being underweight or overweight (BMI < 18.5 or ≥ 25 kg/m2), being a current smoker, not drinking or drinking more than recommended amounts of alcohol, and being physically inactive during leisure time.
Moderate drinking was defined as healthy and complete abstinence from alcohol as unhealthy because there is evidence that moderate alcohol consumption is associated with decreased cardiovascular disease risk.42 However, this categorization should not be interpreted as advice for individuals abstaining from alcohol to take up drinking for health reasons, and we also conducted a sensitivity analysis in which abstinence from alcohol was excluded from the definition of an unhealthy lifestyle. Participants with missing data on any of the lifestyle factors (BMI, alcohol intake, smoking, or physical activity) were excluded from the analyses (n = 30 214, or 20% of all potential participants).
Ascertainment and Definitions of Work Stress Exposures
Job strain was ascertained in all studies with sets of questions (or items) from the Job Content Questionnaire or the Demand-Control Questionnaire,43,44 which were included in the baseline self-report questionnaire in each study. A detailed description of the questionnaires, the job demands and job control scales, and their harmonization across the IPD-Work Consortium studies has been provided elsewhere.45
Briefly, mean scores for job demands items and job control items were calculated for each participant. Participants with a job demands score higher than the study-specific median score were defined as having high job demands, and those with a job control score lower than the study-specific median score were defined as having low job control. Job strain was analyzed as a set of binary and categorical variables. The job strain categories were as follows: high strain (high demands and low control), active job (high demands and high control), passive job (low demands and low control), and low strain (low demands and high control). The binary variable was defined as job strain (high demands and low control) versus no job strain (all other categories). Participants with missing data on more than half of the job demands or job control items (n = 1927, or 1% of all participants) were excluded from the analyses.
Ascertainment and Definitions of Covariates
Gender and age were ascertained from population registries or from the participants at a medical examination in 5 studies (FPS, Gazel, HNR, WOLF Norrland, WOLF Stockholm) and from participant-completed questionnaires in 6 studies (Belstress, HeSSup, KORA 1–3, Whitehall II). Age in years was modeled as a continuous variable.
Socioeconomic position was defined according to occupational title, which was obtained from employers’ registers in 2 studies (FPS, Gazel) and from participant-completed questionnaires in 8 studies (Belstress, HNR, KORA 1–3, Whitehall II, WOLF Norrland, WOLF Stockholm). In one study, HeSSup, socioeconomic position was defined on the basis of the participant’s self-reported highest level of completed education. We grouped socioeconomic position into 3 categories: low, intermediate, or high. Participants who were self-employed or who had missing data on job title were grouped into the “other” socioeconomic category (n = 2053; 1.7%).
Statistical Analyses
We pooled individual-level data from the studies into a single data set. Our cross-sectional analyses of job strain exposures and lifestyle were based on data from all 11 studies. Longitudinal analyses of changes in job strain exposures and lifestyles during follow-up were undertaken in 4 studies (Belstress, FPS, HeSSup, Whitehall II), each of which included a second assessment of both job strain and lifestyle factors. The cross-sectional and longitudinal analyses were based on the 118 701 and 43 971 individuals, respectively, who had complete data on job strain, age, gender, socioeconomic position, BMI, smoking, alcohol intake, and leisure-time physical activity.
We conducted the t test and the χ2 test to compare covariate data for the individuals excluded from and included in the analyses. Although the 2 groups were similar in terms of average age at baseline (44 years), excluded individuals were slightly more likely to be male (55% vs 47%; P < .001).
We used logistic regression models to investigate the associations of job strain with healthy and unhealthy lifestyles and estimated odds ratios (ORs) for rare outcomes (outcomes that occurred among 11% or fewer of the participants, such as job strain at follow-up among those with no strain at baseline). When the outcomes were not rare (those that occurred in > 11% of cases), prevalence ratios (PRs) from modified Poisson regression models were used, because odds ratios would have been likely to overestimate any associations.46 We defined individual studies as clusters in the models and calculated robust standard errors to account for the within-study similarity of the observations. Models adjusted for age and gender and models adjusted for age, gender, and socioeconomic position were run for all exposure–outcome pairs. We used Stata SE version 11.0 (StataCorp LP, College Station, TX) in conducting our analyses.
RESULTS
The characteristics of the participants included in our analyses are presented in Table 1. In the cross-sectional analyses of single lifestyle factors and job strain, individuals who were underweight were slightly more likely to report job strain (OR adjusted for age, gender, and socioeconomic position = 1.17; 95% confidence interval [CI] = 1.07, 1.27), as were smokers (OR = 1.14; 95% CI = 1.05, 1.24) and nondrinkers (OR = 1.16; 95% CI = 1.06, 1.28). Physically inactive individuals were more likely to report job strain (OR = 1.15; 95% CI = 1.04, 1.27) than those who were active. Job strain was not associated with being overweight or drinking more than the recommended amount of alcohol.
TABLE 1—
Characteristics of Participants: 11 IPD-Work Consortium European Studies
| Characteristic | Overall Samplea (n = 118 701), Mean ±SD or No. (%) | No Job Strain (n = 99 404), Mean ±SD or No. (%) | Job Strain (n = 19 297), Mean ±SD or No. (%) | ORb (95% CI) |
| Covariates | ||||
| Age, y | 44.4 ±9.0 | 44.4 ±9.0 | 44.5 ±8.8 | |
| Gender | ||||
| Male | 55 428 (100.0) | 47 949 (86.5) | 7479 (13.5) | 1.00 (Ref) |
| Female | 63 273 (100.0) | 51 455 (81.3) | 11 818 (18.7) | 1.48 (1.31, 1.66) |
| Socioeconomic position | ||||
| Low | 28 831 (100.0) | 22 365 (77.6) | 6466 (22.4) | 1.40 (1.14, 1.73) |
| Intermediate | 58 891 (100.0) | 48 279 (82.0) | 10 612 (18.0) | 1.00 (Ref) |
| High | 28 926 (100.0) | 27 001 (93.3) | 1925 (6.7) | 0.34 (0.28, 0.40) |
| Other | 2053 (100.0) | 1759 (85.7) | 294 (14.3) | 0.78 (0.59, 1.04) |
| Lifestyle factors | ||||
| Body mass index, kg/m2 | ||||
| < 18.5 | 1298 (100.0) | 1051 (81.0) | 247 (19.0) | 1.17 (1.07, 1.27) |
| 18.5–24.9 | 60 581 (100.0) | 50 878 (84.0) | 9703 (16.0) | 1.00 (Ref) |
| ≥ 25 | 56 822 (100.0) | 47 475 (83.6) | 9347 (16.4) | 1.01 (0.96, 1.05) |
| Physical activity status | ||||
| Active | 48 582 (100.0) | 41 211 (84.8) | 7371 (15.2) | 1.00 (Ref) |
| Inactive | 70 119 (100.0) | 58 193 (83.0) | 11 926 (17.0) | 1.15 (1.04, 1.27) |
| Smoking status | ||||
| Nonsmoker | 91 668 (100.0) | 77 419 (84.5) | 14 249 (15.5) | 1.00 (Ref) |
| Smoker | 27 033 (100.0) | 21 985 (81.3) | 5048 (18.7) | 1.14 (1.05, 1.24) |
| Alcohol intake category | ||||
| Nondrinker | 17 502 (100.0) | 14 000 (80.0) | 3502 (20.0) | 1.16 (1.06, 1.28) |
| Moderate drinker | 83 594 (100.0) | 70 440 (84.3) | 13 154 (15.7) | 1.00 (Ref) |
| Heavy drinker | 17 605 (100.0) | 14 964 (85.0) | 2641 (15.0) | 1.02 (0.90, 1.15) |
| Total | 118 701 (100.0) | 99 404 (83.7) | 19 297 (16.3) | |
Note. CI = confidence interval; IPD-Work Consortium = Individual-Participant Data Meta-analysis of Working Populations Consortium; OR = odds ratio.
Participants in the 11 studies assessed with complete data on age, gender, socioeconomic position, smoking status, alcohol intake, body mass index, physical activity status, and job strain.
Odds ratio for job strain, adjusted for age, gender, and socioeconomic position when appropriate.
Of the 118 701 people included in our analyses, 18 483 (16%) had a healthy lifestyle (no unhealthy lifestyle factors). The majority of the participants (n = 100 218; 84%) had some combination of unhealthy lifestyle factors: 37 466 (32%) had 1 such factor, 39 258 (33%) had 2, 19 579 (16%) had 3, and 3915 (3%) had 4 (i.e., an unhealthy lifestyle).
Cross-Sectional Analyses
Cross-sectional associations of job strain with unhealthy and healthy lifestyles are shown in Table 2. With unhealthy lifestyle as the outcome, analyses adjusted for age, gender, and socioeconomic position showed that individuals in high-strain jobs and active jobs were, respectively, 34% and 25% more likely than those in low-strain jobs to have an unhealthy lifestyle. There was no clear evidence of an association between having a passive job and having an unhealthy lifestyle. The association between job strain and unhealthy lifestyle was slightly attenuated in the sensitivity analysis, in which abstinence from alcohol was not included in the definition of an unhealthy lifestyle (sensitivity analysis: OR = 1.15; 95% CI = 1.01, 1.30; main analysis: OR = 1.25; 95% CI = 1.12, 1.39).
TABLE 2—
Cross-Sectional Associations of Job Strain and Work Stress Categories With Unhealthy and Healthy Lifestyles: 11 IPD-Work Consortium European Studies
| Type of Work Stress Exposure | Sample, No. (%) | Association Estimate Adjusted for Age and Gender (95% CI) | Association Estimate Adjusted for Age, Gender, and Socioeconomic Position (95% CI) |
| Unhealthy lifestylea | |||
| Binary | |||
| No job strain (n = 99 404) | 3125 (3.1) | 1.00 (Ref) | 1.00 (Ref) |
| Job strain (n = 19 297) | 790 (4.1) | 1.40 (1.25, 1.57) | 1.25 (1.12, 1.39) |
| Categorical | |||
| Low job strain (n = 35 338) | 991 (2.8) | 1.00 (Ref) | 1.00 (Ref) |
| Passive job (n = 32 013) | 1084 (3.4) | 1.27 (1.12, 1.44) | 1.03 (0.85, 1.26) |
| Active job (n = 32 053) | 1050 (3.3) | 1.14 (1.00, 1.31) | 1.25 (1.14, 1.36) |
| High job strain (n = 19 297) | 790 (4.1) | 1.59 (1.38, 1.82) | 1.34 (1.14, 1.58) |
| Healthy lifestyleb | |||
| Binary | |||
| No job strain (n = 99 404) | 15 893 (16.0) | 1.00 (Ref) | 1.00 (Ref) |
| Job strain (n = 19 297) | 2590 (13.4) | 0.80 (0.72, 0.90) | 0.89 (0.80, 0.99) |
| Categorical | |||
| Low job strain (n = 35 338) | 6381 (18.1) | 1.00 (Ref) | 1.00 (Ref) |
| Passive job (n = 32 013) | 4558 (14.2) | 0.76 (0.71, 0.81) | 0.90 (0.87, 0.92) |
| Active job (n = 32 053) | 4954 (15.5) | 0.89 (0.82, 0.97) | 0.86 (0.77, 0.95) |
| High job strain (n = 19 297) | 2590 (13.4) | 0.71 (0.62, 0.82) | 0.82 (0.71, 0.95) |
Note. CI = confidence interval; IPD-Work Consortium = Individual-Participant Data Meta-analysis of Working Populations Consortium.
Having all 4 unhealthy lifestyle factors, that is, being underweight or overweight, being a current smoker, not drinking or drinking more than recommended amounts of alcohol, and being physically inactive during leisure time. Association estimates are odds ratios.
cHaving all 4 healthy lifestyle factors, that is, being normal weight, being a nonsmoker, drinking moderate amounts of alcohol, and being physically active during leisure time. Association estimates are prevalence ratios.
In the converse analyses with healthy lifestyle as the outcome in the model, individuals who reported job strain were 11% less likely to have a healthy lifestyle than individuals who did not report job strain, independent of age, gender, or socioeconomic position. People in active, passive, and high-strain jobs were less likely than those in low-strain jobs to have a healthy lifestyle, but the association estimates for these categories did not markedly differ from one another. When the analysis was restricted to those with unhealthy lifestyles or healthy lifestyles (i.e., those with other combinations of lifestyle factors were excluded), job strain was associated with 1.39 (95% CI = 1.13, 1.71) times the odds of having an unhealthy lifestyle (all 4 unhealthy lifestyle factors). This association was only slightly attenuated in the sensitivity analysis in which alcohol abstinence was not a criterion for defining an unhealthy lifestyle (OR = 1.21; 95% CI = 1.06, 1.38).
Longitudinal Analyses
A total of 43 958 participants in 4 studies had repeated measures data available on job strain and lifestyle factors. The time between baseline and follow-up varied slightly between participants and studies: the follow-up occurred 4 to 8 years after baseline in Belstress, 2 to 4 years after baseline in FPS, 5 years after baseline in HeSSup, and 3 to 9 years after baseline in Whitehall II. Longitudinal associations of job strain at baseline with lifestyle at follow-up, by categories of baseline lifestyle, are shown in Figure 1 (see also Appendix B, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Adjusted odds ratios for having a healthy lifestyle (no risk factors) at follow-up by categories of work stress at baseline: 11 IPD-Work Consortium European studies.
Note. CI = confidence interval; IPD-Work Consortium = Individual-Participant Data Meta-analysis of Working Populations Consortium; OR = odds ratio. Odds ratios were adjusted for baseline age, gender, and socioeconomic position.
Of the 34 034 individuals who did not have a healthy lifestyle at baseline (i.e., who had 1–4 unhealthy lifestyle factors), approximately 10% had adopted a healthy lifestyle (no unhealthy lifestyle factors) by follow-up. After adjustment for age, gender, and socioeconomic position, job strain (vs no strain) at baseline was not associated with a healthy lifestyle at follow-up (OR = 0.92; 95% CI = 0.82, 1.03; Appendix B). However, Figure 1 shows that among individuals who did not have a healthy lifestyle at baseline, those with high-strain or passive jobs at baseline were less likely to have adopted a healthy lifestyle by follow-up than individuals in low-strain jobs.
A shift from a healthy lifestyle to an unhealthier one was more common than the other way around. Of the 9937 individuals who had a healthy lifestyle at baseline (i.e., no unhealthy lifestyle factors), 42% had drifted to a less healthy lifestyle (1–4 unhealthy factors) by follow-up (Appendix B). There was no clear evidence in this group of participants of an association between the binary job strain variable or most job strain categories at baseline and having drifted into an unhealthy lifestyle by follow-up (Appendix B). However, those with active jobs at baseline were slightly more likely than those with low-strain jobs at baseline to have drifted into an unhealthy lifestyle by the follow-up (PR = 1.04; 95% CI = 1.02, 1.06).
To investigate possible reverse causality, we modeled the longitudinal associations between baseline lifestyle and job strain at follow-up according to baseline job strain exposure. The results of these analyses, adjusted for age, gender, and socioeconomic position, are shown in Table 3. Among individuals who reported no strain at baseline, those who had a healthy lifestyle at baseline were 10% less likely than those who did not to report job strain at follow-up, independent of age, gender, or socioeconomic position (OR = 0.90; 95% CI = 0.83, 0.96). Among individuals with job strain at baseline, lifestyle at baseline was not associated with job strain at follow-up.
TABLE 3—
Tests of Reverse Causation: Longitudinal Associations Between Baseline Lifestyle and Job Strain at Follow-Up, by Baseline Job Strain Exposure: 11 IPD-Work Consortium European Studies
| Type of Work Stress Exposure and Lifestyle at Baseline | No. of Participantsa | Outcome or No. (%) With Outcome | Association Estimate Adjusted for Age and Gender (95% CI) | Association Estimate Adjusted for Age, Gender, and Socioeconomic Position (95% CI) |
| No job strain at baselineb (n = 37 080) | Job strain at follow-up | |||
| Unhealthy lifestyle | 28 539 | 2989 (10.5) | 1.00 (Ref) | 1.00 (Ref) |
| Healthy lifestyle | 8541 | 764 (9.0) | 0.82 (0.77, 0.88) | 0.90 (0.83, 0.96) |
| Job strain at baselinec (n = 6891) | No job strain at follow-up | |||
| Unhealthy lifestyle | 5495 | 3241 (59.0) | 1.00 (Ref) | 1.00 (Ref) |
| Healthy lifestyle | 1396 | 875 (62.7) | 1.06 (1.01, 1.11) | 1.03 (0.98, 1.09) |
Note. CI = confidence interval; IPD-Work Consortium = Individual-Participant Data Meta-analysis of Working Populations Consortium.
Participants with repeat data on job strain and lifestyle factors (n = 43 958) in 4 studies: Belstress (follow-up = 4–8 years), Finnish Public Sector Study (follow-up = 2–4 years), Health and Social Support Study (follow-up = 5 years), and Whitehall II Study (follow-up = 3–9 years).
Association estimates are odds ratios for job strain at follow-up.
Association estimates are prevalence ratios for no job strain at follow-up.
DISCUSSION
In our cross-sectional analyses, individuals who reported job strain were less likely than those who reported no job strain to have an overall healthy lifestyle (i.e., to have a normal weight, not smoke, drink moderate amounts of alcohol, and be physically active in their leisure time). In our longitudinal analyses, individuals with high-strain jobs or passive jobs at baseline were less likely to have adopted a healthy lifestyle by follow-up than individuals with low-strain jobs at baseline. Also, among individuals who reported no job strain at baseline, those with a healthy lifestyle were slightly less likely than those with other combinations of lifestyle factors to report job strain at follow-up.
We hypothesized that the association between job strain and overall health-related lifestyle would be stronger than the association between job strain and each individual unhealthy lifestyle factor. In our previous analyses based on IPD-Work Consortium data, job strain was associated with individual health behaviors, but the associations were modest in size. In those analyses, job strain was associated with 1.11-fold odds of being a current smoker, and the corresponding odds ratios for heavy alcohol consumption, complete abstinence from alcohol, and physical inactivity were 1.12, 1.10, and 1.17, respectively.47–49 Job strain was also associated with approximately 1.1-fold odds of obesity as well as underweight.50 However, in both this study and our previously published analyses, our estimates of the associations of job strain with overall healthy or unhealthy lifestyles were only marginally larger than the associations of job strain with each individual health behavior.
We are aware of only 2 previous studies of the associations between measures of psychosocial work stress and the co-occurrence of health-related lifestyle factors; the data used in both of these investigations were derived from the FPS, also one of the constituent studies in our meta-analysis. In one of these studies, high-strain and passive jobs were associated with 1.3-fold to 1.4-fold odds of having multiple unhealthy lifestyle factors11; in the other, high effort–reward imbalance (another indicator of work-related stress) was also associated with having multiple unhealthy lifestyle factors.51
Our estimates of associations were similar in both direction and magnitude to those reported previously; unlike previous analyses, however, our meta-analysis included participants in a broad range of age groups from multiple sectors of work and several European countries. Taken together, the findings presented here and the results of previous studies lend credibility to the existence of a modest-sized association between job strain and overall healthy and unhealthy lifestyles and to our estimates of associations being generalizable across different fields of work and countries.
Limitations and Strengths
We used a well-recognized and validated measure, job strain, to assess work stress exposures.43 However, data on job strain, as well as smoking, alcohol intake, and physical activity, were self-reported by participants in all of the studies included in our analysis. Also, BMI was based on self-reported weight and height in 3 studies. Thus, it is likely that there was some degree of misclassification of these lifestyle indicators.52–57 Also, although the age and gender distributions of the individuals included in and excluded from our analyses were broadly similar, a relatively large number of potential participants had missing data on 1 or more lifestyle variables, and excluding them may have reduced the precision of our estimates. Furthermore, residual confounding from possible common causes of job strain and health behaviors (e.g., personality and coping styles or stress from other sources such as adverse life events) may have influenced our findings.
An important strength of our analyses is that we used a large set of harmonized individual-level data from 11 European studies, increasing the generalizability of our findings as well as the precision of our association estimates. In some of the individual studies included in our meta-analysis, the associations between job strain and health behaviors had been previously investigated and the findings published; in other studies, our meta-analysis represents the first time these associations have been examined. A major advantage of a meta-analysis such as ours, which was based on individual-participant data from both published and unpublished studies, is that it is less prone to publication bias, which may distort the findings in literature-based meta-analyses.36
Conclusions
Taken together, our findings suggest that psychosocial work stress, operationalized as job strain, is associated with individual lifestyle factors as well as their co-occurrence. Some job characteristics and lifestyle factors may also change simultaneously and predict change in one another over time, but no consistent pattern in such changes was apparent. Therefore, although reducing work-related psychosocial stress would undoubtedly increase the psychological well-being of the working population, it is unlikely to be an important target for any policy or intervention aiming to influence health-related lifestyle factors or overall lifestyle.
Further research is needed into efficient ways at the organizational level for employers to reduce psychosocial stress at work, such as by monitoring staffing levels and reorganizing tasks. Also, employers could encourage and facilitate adoption and maintenance of healthy lifestyles in their workforce by, for example, supporting smoking cessation programs or opportunities for physical activity, including allowing employees to take time off to participate in these initiatives and subsidizing their cost.
Acknowledgments
The IPD-Work (Individual-Participant Data Meta-analysis of Working Populations) Consortium is supported by the European Union NEW OSH ERA research program (funded by the Finnish Work Environment Fund, Swedish Council for Working Life and Social Research, and German Social Accident Insurance), the Academy of Finland (grant 132944), and the BUPA Foundation (grant 22094477). The Heinz Nixdorf Recall Study was funded by the Heinz Nixdorf Foundation (Germany), the German Ministry of Education and Science, and the German Research Foundation. Mika Kivimäki is supported by the Medical Research Council (United Kingdom) and by an Economic and Social Research Council professorial fellowship. At the time of the preparation of this article, G. David Batty was a Wellcome Trust fellow.
Note. The funders had no role in the study design, data collection and analysis, or preparation of the article.
Human Participant Protection
Each IPD-Work Consortium study was approved by the relevant local or national ethics committee (for more details on ethical approval, see Appendix B, available as a supplement to the online version of this article at http://www.ajph.org). All participants provided informed consent.
References
- 1.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6(4):e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuit AJ, van Loon AJ, Tijhuis M, Ocke M. Clustering of lifestyle risk factors in a general adult population. Prev Med. 2002;35(3):219–224. doi: 10.1006/pmed.2002.1064. [DOI] [PubMed] [Google Scholar]
- 3.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. J Public Health (Oxf) 2012;34(suppl 1):i3–i10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22(6):638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- 5.Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviours and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12. doi: 10.1371/journal.pmed.0050012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tamakoshi A, Tamakoshi K, Lin Y, Yagyu K, Kikuchi S. Healthy lifestyle and preventable death: findings from the Japan Collaborative Cohort (JACC) Study. Prev Med. 2009;48(5):486–492. doi: 10.1016/j.ypmed.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 7.Kvaavik E, Batty GD, Ursin G, Huxley R, Gale CR. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom Health and Lifestyle Survey. Arch Intern Med. 2010;170(8):711–718. doi: 10.1001/archinternmed.2010.76. [DOI] [PubMed] [Google Scholar]
- 8.Chiuve SE, Rexrode KM, Spiegelman D, Logroscino G, Manson JE, Rimm EB. Primary prevention of stroke by healthy lifestyle. Circulation. 2008;118(9):947–954. doi: 10.1161/CIRCULATIONAHA.108.781062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiseman M. The second World Cancer Research Fund/American Institute for Cancer Research expert report. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Proc Nutr Soc. 2008;67(3):253–256. doi: 10.1017/S002966510800712X. [DOI] [PubMed] [Google Scholar]
- 10.Zhang Y, Tuomilehto J, Jousilahti P, Wang Y, Antikainen R, Hu G. Lifestyle factors on the risks of ischemic and hemorrhagic stroke. Arch Intern Med. 2011;171(20):1811–1818. doi: 10.1001/archinternmed.2011.443. [DOI] [PubMed] [Google Scholar]
- 11.Kouvonen A, Kivimäki M, Vaananen A et al. Job strain and adverse health behaviors: the Finnish Public Sector study. J Occup Environ Med. 2007;49(1):68–74. doi: 10.1097/JOM.0b013e31802db54a. [DOI] [PubMed] [Google Scholar]
- 12.Lallukka T, Lahelma E, Rahkonen O et al. Associations of job strain and working overtime with adverse health behaviors and obesity: evidence from the Whitehall II Study, Helsinki Health Study, and the Japanese Civil Servants Study. Soc Sci Med. 2008;66(8):1681–1698. doi: 10.1016/j.socscimed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 13.Perdikaris P, Kletsiou E, Gymnopoulou E, Matziou V. The relationship between workplace, job stress and nurses’ tobacco use: a review of the literature. Int J Environ Res Public Health. 2010;7(5):2362–2375. doi: 10.3390/ijerph7052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radi S, Ostry A, Lamontagne AD. Job stress and other working conditions: relationships with smoking behaviors in a representative sample of working Australians. Am J Ind Med. 2007;50(8):584–596. doi: 10.1002/ajim.20492. [DOI] [PubMed] [Google Scholar]
- 15.Head J, Stansfeld SA, Siegrist J. The psychosocial work environment and alcohol dependence: a prospective study. Occup Environ Med. 2004;61(3):219–224. doi: 10.1136/oem.2002.005256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kouvonen A, Kivimäki M, Cox SJ, Poikolainen K, Cox T, Vahtera J. Job strain, effort-reward imbalance, and heavy drinking: a study in 40,851 employees. J Occup Environ Med. 2005;47(5):503–513. doi: 10.1097/01.jom.0000161734.81375.25. [DOI] [PubMed] [Google Scholar]
- 17.Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32(6):473–481. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- 18.Choi B, Schnall PL, Yang H et al. Psychosocial working conditions and active leisure-time physical activity in middle-aged US workers. Int J Occup Med Environ Health. 2010;23(3):239–253. doi: 10.2478/v10001-010-0029-0. [DOI] [PubMed] [Google Scholar]
- 19.Kouvonen A, Kivimäki M, Elovainio M, Virtanen M, Linna A, Vahtera J. Job strain and leisure-time physical activity in female and male public sector employees. Prev Med. 2005;41(2):532–539. doi: 10.1016/j.ypmed.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 20.van Loon AJ, Tijhuis M, Surtees PG, Ormel J. Lifestyle risk factors for cancer: the relationship with psychosocial work environment. Int J Epidemiol. 2000;29(5):785–792. doi: 10.1093/ije/29.5.785. [DOI] [PubMed] [Google Scholar]
- 21.Wemme KM, Rosvall M. Work related and non-work related stress in relation to low leisure time physical activity in a Swedish population. J Epidemiol Community Health. 2005;59(5):377–379. doi: 10.1136/jech.2004.031526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brisson C, Larocque B, Moisan J, Vezina M, Dagenais GR. Psychosocial factors at work, smoking, sedentary behavior, and body mass index: a prevalence study among 6995 white collar workers. J Occup Environ Med. 2000;42(1):40–46. doi: 10.1097/00043764-200001000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Kivimäki M, Head J, Ferrie JE et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond) 2006;30(6):982–987. doi: 10.1038/sj.ijo.0803229. [DOI] [PubMed] [Google Scholar]
- 25.Kouvonen A, Kivimäki M, Cox SJ, Cox T, Vahtera J. Relationship between work stress and body mass index among 45,810 female and male employees. Psychosom Med. 2005;67(4):577–583. doi: 10.1097/01.psy.0000170330.08704.62. [DOI] [PubMed] [Google Scholar]
- 26.Ostry AS, Radi S, Louie AM, LaMontagne AD. Psychosocial and other working conditions in relation to body mass index in a representative sample of Australian workers. BMC Public Health. 2006;6:53. doi: 10.1186/1471-2458-6-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Bacquer D, Pelfrene E, Clays E et al. Perceived job stress and incidence of coronary events: 3-year follow-up of the Belgian Job Stress Project cohort. Am J Epidemiol. 2005;161(5):434–441. doi: 10.1093/aje/kwi040. [DOI] [PubMed] [Google Scholar]
- 28.Kivimäki M, Lawlor DA, Smith GD et al. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart disease: the Finnish Public Sector study. Am J Public Health. 2007;97(5):874–879. doi: 10.2105/AJPH.2005.078691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldberg M, Leclerc A, Bonenfant S et al. Cohort profile: the GAZEL Cohort Study. Int J Epidemiol. 2007;36(1):32–39. doi: 10.1093/ije/dyl247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Korkeila K, Suominen S, Ahvenainen J et al. Non-response and related factors in a nationwide health survey. Eur J Epidemiol. 2001;17(11):991–999. doi: 10.1023/a:1020016922473. [DOI] [PubMed] [Google Scholar]
- 31.Stang A, Moebus S, Dragano N et al. Baseline recruitment and analyses of nonresponse of the Heinz Nixdorf Recall Study: identifiability of phone numbers as the major determinant of response. Eur J Epidemiol. 2005;20(6):489–496. doi: 10.1007/s10654-005-5529-z. [DOI] [PubMed] [Google Scholar]
- 32.Holle R, Happich M, Lowel H, Wichmann HE. KORA—a research platform for population based health research. Gesundheitswesen. 2005;67(suppl 1):S19–S25. doi: 10.1055/s-2005-858235. [DOI] [PubMed] [Google Scholar]
- 33.Marmot MG, Smith GD, Stansfeld S et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 34.Alfredsson L, Hammar N, Fransson E et al. Job strain and major risk factors for coronary heart disease among employed males and females in a Swedish study on work, lipids and fibrinogen. Scand J Work Environ Health. 2002;28(4):238–248. doi: 10.5271/sjweh.671. [DOI] [PubMed] [Google Scholar]
- 35.Peter R, Alfredsson L, Hammar N, Siegrist J, Theorell TPW. High effort, low reward, and cardiovascular risk factors in employed Swedish men and women: baseline results from the WOLF study. J Epidemiol Community Health. 1998;52:540–547. doi: 10.1136/jech.52.9.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kivimäki M, Nyberg ST, Batty GD et al. Job strain as a risk factor for future coronary heart disease: a collaborative meta-analysis of 2358 events in 197,473 men and women. Lancet. 2012;380(9852):1491–1497. doi: 10.1016/S0140-6736(12)60994-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. , 1–253. [PubMed] [Google Scholar]
- 38.National Health Service, United Kingdom. The risks of drinking too much. Available at: http://www.nhs.uk/Livewell/alcohol/Pages/Effectsofalcohol.aspx. Accessed January 4, 2013.
- 39.Alcohol, Wine and Cardiovascular Disease. Dallas, TX: American Heart Association; 2011. [Google Scholar]
- 40.Substance Abuse Facts: Alcohol. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 41.Global strategy on diet, physical activity and health. World Health Organization. Available at: http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_english_web.pdf. Accessed January 4, 2013.
- 42.Yusuf S, Hawken S, Ounpuu S et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 43.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 44.Karasek R, Theorell T. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life. New York, NY: Basic Books; 1990. [Google Scholar]
- 45.Fransson EI, Nyberg ST, Heikkilä K et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health. 2012;12:62. doi: 10.1186/1471-2458-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 47.Fransson EI, Heikkilä K, Nyberg ST et al. Job strain as a risk factor for leisure-time physical inactivity: an individual-participant meta-analysis of up to 170,000 men and women: the IPD-Work Consortium. Am J Epidemiol. 2012;176(12):1078–1089. doi: 10.1093/aje/kws336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heikkilä K, Nyberg ST, Fransson EI et al. Job strain and tobacco smoking: an individual-participant data meta-analysis of 166,130 adults in 15 European studies. PLoS One. 2012;7(7):e35463. doi: 10.1371/journal.pone.0035463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Heikkilä K, Nyberg ST, Fransson EI et al. Job strain and alcohol intake: a collaborative meta-analysis of individual-participant data from 140,000 men and women. PLoS One. 2012;7(7):e40101. doi: 10.1371/journal.pone.0040101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nyberg ST, Heikkilä K, Fransson EI et al. Job strain in relation to body mass index: pooled analysis of 160 000 adults from 13 cohort studies. J Intern Med. 2012;272(1):65–73. doi: 10.1111/j.1365-2796.2011.02482.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kouvonen A, Kivimäki M, Virtanen M et al. Effort-reward imbalance at work and the co-occurrence of lifestyle risk factors: cross-sectional survey in a sample of 36,127 public sector employees. BMC Public Health. 2006;6:24. doi: 10.1186/1471-2458-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vartiainen E, Seppala T, Lillsunde P, Puska P. Validation of self reported smoking by serum cotinine measurement in a community-based study. J Epidemiol Community Health. 2002;56(3):167–170. doi: 10.1136/jech.56.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simpura J, Karlsson T.Trends in Drinking Patterns in 15 European Countries, 1950 to 2000 Helsinki, Finland: National Research and Development Centre for Welfare and Health; 2001 [Google Scholar]
- 54.Stockwell T, Donath S, Cooper-Stanbury M, Chikritzhs T, Catalano P, Mateo C. Under-reporting of alcohol consumption in household surveys: a comparison of quantity-frequency, graduated-frequency and recent recall. Addiction. 2004;99(8):1024–1033. doi: 10.1111/j.1360-0443.2004.00815.x. [DOI] [PubMed] [Google Scholar]
- 55.Merrill RM, Richardson JS. Validity of self-reported height, weight, and body mass index: findings from the National Health and Nutrition Examination Survey, 2001–2006. Prev Chronic Dis. 2009;6(4):A121. [PMC free article] [PubMed] [Google Scholar]
- 56.Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC-Oxford participants. Public Health Nutr. 2002;5(4):561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- 57.van Poppel MN, Chinapaw MJ, Mokkink LB, van Mechelen W, Terwee CB. Physical Activity Questionnaires for Adults: a systematic review of measurement properties. Sports Med. 2010;40(7):565–600. doi: 10.2165/11531930-000000000-00000. [DOI] [PubMed] [Google Scholar]