Abstract
Objectives. To examine the associations between obesity and multiple aspects of the food environments, at home and in the neighborhood.
Methods. Our study included 38 650 individuals nested in 18 381 households located in 2104 US counties. Our novel home food environment measure, USDAScore, evaluated the adherence of a household’s monthly expenditure shares of 24 aggregated food categories to the recommended values based on US Department of Agriculture food plans. The US Census Bureau’s County Business Patterns (2008), the detailed food purchase information in the IRi Consumer Panel scanner data (2008–2012), and its associated MedProfiler data set (2012) constituted the main sources for neighborhood-, household-, and individual-level data, respectively.
Results. After we controlled for a number of confounders at the individual, household, and neighborhood levels, USDAScore was negatively linked with obesity status, and a census tract–level indicator of food desert status was positively associated with obesity status.
Conclusions. Neighborhood food environment factors, such as food desert status, were associated with obesity status even after we controlled for home food environment factors.
A number of recent studies have uncovered significant associations between the neighborhood food environment and health outcomes, particularly obesity status.1–6 Other studies, however, have found no such statistically significant relationships.7–10 Among those studies finding significant associations, it is most common to find obesity status or weight negatively related to supermarket counts,3–5 less common to find convenience store counts positively related,3 and rarer still to find club stores or supercenters positively related, with Courtemanche and Carden2 being one of the few studies that link supercenters to obesity. Finally, at least 1 study investigated the link between county-level obesity rates and the percentage of the county’s population living in food desert tracts, but it did not find a significant association.11
One explanation for these mixed results centers on data measurement issues, with researchers’ measures of the built environment varying widely. Different measures include the number of food outlets within a predetermined area,12–15 distance to the nearest food outlet,9,16 and densities of food outlets in various forms.8,17–21 Whereas some studies employed only 1 of these measures, others examined multiple measures to investigate the consistency of effects.22–24
A second explanation for the mixed results centers on particular covariates included or missing from the analysis. Although 1 line of research focuses on the home food environment, few studies that focused on the neighborhood food environment also included covariates that described the home food environment. If covariates that accurately describe the home food environment are not accounted for, behavioral choices may possibly mask or confound associations between obesity and neighborhood food environment measures.
Two reviews concluded that commonly used measures of food availability at home (which the reviews discussed in detail) had various limitations.25,26 Although open inventories examined by researchers can capture any type of food available at home, they are labor intensive and constrained by the time points of data collection.25 Other measures, such as predefined inventory checklists, food frequency questionnaires, and self-reported checklists, include a limited number of items, most of which focus on fruits and vegetables.25,26 In addition, a biomarker-based observational study27 indicated that both food frequency questionnaires and 24-hour recalls are subject to considerable measurement errors, and the bias is larger for food frequency questionnaires.
The availability of household-level scanner data in multiple years enabled us to generate a comprehensive home food environment measure with an extended period of time and potentially less bias. This measure indicates households’ compliance with the US Department of Agriculture’s (USDA) recommended food purchase shares by food category, which are designed for households that would like to meet the Dietary Guidelines for Americans for at-home food consumption, even on a limited budget.28 In this sense, it is related to a substantial body of literature that examines the association between overall dietary patterns and various health outcomes. These studies’ findings are summarized in a number of review articles.29–33 A broader review of studies found that there is an inverse relationship between compliance with the Dietary Guidelines for Americans and obesity.34–36
By including a novel home food environment variable, as well as rich measures of the neighborhood food environment, our study addressed some of these confounding issues and other deficiencies in the literature. Following a number of related studies and research recommendations,1,37 our research was premised on the social environmental approach to health and health interventions, which
places emphasis on how the health of individuals is influenced not only by biological and genetic functioning and predisposition, but also by social and familial relationships, environmental contingencies, and broader social and economic trends.38(p150)
Our research, therefore, investigated how obesity and overweight status was influenced by (1) individual-level factors, including age, gender, and several self-reported behavior responses; (2) household-level factors, including race, ethnicity, education, income, and a home food environment measure that indicated the overall healthfulness of a household’s aggregate food-at-home purchases; and (3) neighborhood-level factors, including county-level densities of various food store types, poverty rates, metro status, and a census tract–level indicator of food desert status as defined by the USDA.
METHODS
We compiled a multilevel data set from several sources. Individual- and household-level data came from the IRi Consumer Panel and the IRi MedProfiler data. The Consumer Panel data reflected all food purchases from 2008 to 2012 by a representative set of US households that recorded all their retail food purchases with a home-scanning device. Additionally, the IRi data contained a rich set of household-level demographics. The companion MedProfiler data set for 2012 contained self-reported responses on height, weight, health outcomes, and various behavioral questions for individuals in the IRi households matched by household ID. Neighborhood-level data came from various public sources. From the US Census Bureau’s County Business Patterns, we collected food store and restaurant establishment numbers at the county level. From the Census Bureau’s American Community Survey (2010–2012), we extracted population and poverty rate data. From the USDA, we collected county-level 2013 Rural–Urban Continuum Codes and census tract–level food desert information.
Our full data set contained 38 650 individuals nested in 18 381 households located in 2104 counties of the United States. The actual sample size for analysis was slightly less because of missing observations for some of the variables.
Obesity and Overweight Status Outcomes
We calculated individuals’ body mass indexes (BMIs; defined as weight in kilograms divided by the square of height in meters) on the basis of IRi household members’ self-reported weights and heights ([weight in pounds/(height in inches)2] × 703). On the basis of our BMI calculations, we constructed indicator variables for obesity and overweight status using different criteria for adults and children. For adults aged 18 years and older, overweight status was a binary variable, with 1 indicating overweight status (25 ≤ BMI < 30) and 0 indicating underweight or normal-weight status (BMI < 25). Similarly, obesity status was a binary variable, with 1 indicating obesity (BMI ≥ 30) and 0 indicating underweight or normal-weight status (BMI < 25). For children aged 2 to 17 years, we obtained age- and gender-specific BMI percentile values from the Centers for Disease Control and Prevention.39 We categorized children with BMIs lower than the 85th percentile for their age and gender as being underweight or normal weight, those with BMIs greater than or equal to the 85th percentile but lower than the 95th percentile as overweight, and those with BMIs greater than or equal to the 95th percentile as obese.40
Individual-Level Variables
“Diet feature” was a factor analysis score constructed from 7 MedProfiler questions related to special diets, including high-fiber, high-protein, low-calorie, low-carbohydrate, low-fat, low-salt, and low-sugar diets. All responses to these dietary features were either yes (coded as 1) or no (0). Additional covariates included individuals’ age, gender, whether they ate at a fast-food restaurant on most days of a week (“fast food”), and whether they exercised for at least 20 minutes per day on most days of a week (“exercise”).
Household-Level Variables
Household-level demographic characteristics, including race/ethnicity, household size, income, education, and marital status, were available directly from the IRi Consumer Panel.
One of the main household-level measures in our analysis, USDAScore, reflected the home food environment and was constructed from the detailed food purchase information in the IRi Consumer Panel. Following Volpe and Okrent,28 USDAScore measured adherence of a household’s monthly expenditure shares of 24 aggregated food categories—defined by the USDA’s Center for Nutrition Policy and Promotion (CNPP)—to the recommended values based on USDA food plans. We calculated the USDAScore by a squared-error loss function:
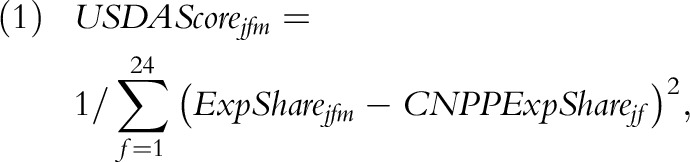 |
where
 is the recommended household-specific food expenditure share
for household j in CNPP food category f and
is the recommended household-specific food expenditure share
for household j in CNPP food category f and
 is household j’s actual expenditure
share in category f in month m. The recommended
shares varied across households depending on household demographics, which included
the age of male household head, age of female household head, and presence and age of
children. Table 1 lists the 24 food
categories and shows how the expenditure shares based on USDA food plan
recommendations for each category compared with observed average expenditures in the
sample. Further explanation of this score can be found in Volpe and Okrent.28 In this study, we used the 5-year
average of the monthly scores (USDAScore) for households that stayed in the IRi panel
from 2008 to 2012, thus emphasizing the long-term impact that the at-home food
environment might have on obesity.
is household j’s actual expenditure
share in category f in month m. The recommended
shares varied across households depending on household demographics, which included
the age of male household head, age of female household head, and presence and age of
children. Table 1 lists the 24 food
categories and shows how the expenditure shares based on USDA food plan
recommendations for each category compared with observed average expenditures in the
sample. Further explanation of this score can be found in Volpe and Okrent.28 In this study, we used the 5-year
average of the monthly scores (USDAScore) for households that stayed in the IRi panel
from 2008 to 2012, thus emphasizing the long-term impact that the at-home food
environment might have on obesity.
TABLE 1—
USDA Recommended Expenditure Shares for 24 Aggregated Food Categories, and Average Expenditure Shares in the IRi Consumer Panel (2008–2012): United States
| Food Category | DGA Recommended or Recommended With Limited Consumption | USDA Recommended Expenditure Sharesa | Mean Monthly Expenditure Shares per Householdb |
| Grains | |||
| Whole-grain productsc | Recommended | 10.09 | 2.82 |
| Non–whole-grain productsd | Limited | 6.10 | 20.61 |
| Vegetables | |||
| All potato products | Recommended | 1.77 | 1.85 |
| Dark-green vegetables | Recommended | 5.59 | 0.50 |
| Orange vegetables | Recommended | 2.61 | 0.06 |
| Canned and dry beans, lentils, and peas (legumes) | Recommended | 8.32 | 0.99 |
| Other vegetables | Recommended | 8.66 | 2.71 |
| Fruits | |||
| Whole fruits | Recommended | 16.49 | 1.50 |
| Fruit juices | Recommended | 1.86 | 2.26 |
| Milk products | |||
| Whole-milk productse | Limited | 0.86 | 5.38 |
| Lower fat and skim milk and low-fat yogurt | Recommended | 8.77 | 5.46 |
| All cheese (including cheese soup and sauce) | Limited | 0.60 | 4.85 |
| Meat and beans | |||
| Beef, pork, veal, lamb, and game | Limited | 5.31 | 0.48 |
| Chicken, turkey, and game birds | Recommended | 2.69 | 1.69 |
| Fish and fish products | Recommended | 11.92 | 2.06 |
| Bacon, sausages, and luncheon meats (including spreads) | Limited | 0.91 | 5.29 |
| Nuts, nut butters, and seeds | Recommended | 3.16 | 2.77 |
| Eggs and egg mixtures | Recommended | 0.12 | 1.40 |
| Other foods | |||
| Fats and condimentsf | Limited | 1.79 | 7.86 |
| Coffee and tea | Recommended | 0.02 | 3.71 |
| Soft drinks, sodas, fruit drinks, and ades (including rice beverages) | Limited | 1.33 | 6.46 |
| Sugars, sweets, and candies | Limited | 0.41 | 8.10 |
| Soups (ready-to-serve and condensed soups, dry soups) | Limited | 0.51 | 2.17 |
| Frozen or refrigerated entrees (including pizza, fish sticks, and frozen meals) | Limited | 0.18 | 9.02 |
Note. DGA = Dietary Guidelines for Americans; USDA = US Department of Agriculture.
The USDA recommended shares are based on the recommended dollar costs of feeding a representative family consisting of 1 male and 1 female aged 19–50 years, 1 child aged 9–11 years, and 1 child aged 6–8 years, according to the Liberal Food Plan.28
Average expenditure shares were calculated on the basis of all the households (n = 18 381) included in this study.
Includes whole-grain breads, rice, pasta, and pastries (including whole-grain flours); whole-grain cereals (including hot cereal mixes); and popcorn and other whole-grain snacks.
Includes non–whole-grain breads, cereals, rice, pasta, pies, pastries, snacks, and flours.
Includes whole milk, yogurt, cream, milk drinks, and milk desserts.
Includes table fats, oils, salad dressings, gravies, sauces, condiments, and spices.
Neighborhood-Level Variables
We collected data on the average number of food stores or restaurants per 10 000 county residents. Definitions and specific examples of each category can be found in Morland et al.41 We extracted numbers of establishments from the 2008 County Business Patterns and divided them by county-level population estimates for the corresponding year. Previous studies adopted similar density measures at various geographic levels to investigate their relationship with individual weight outcomes.3,17,21 Note that our 2008 store density measures lagged the obesity and overweight status variables by 4 years; we intended that this lag would lessen any potential endogeneity problems associated with the mutual relationship between consumer preferences and availability of food outlets.42,43
Additional neighborhood-level covariates included county-level poverty rates, metro versus nonmetro classification, and food desert status measured at the census tract level. We included county-level poverty rates as a covariate because studies have shown that disadvantaged communities are especially vulnerable to adverse food environments. Urban and rural areas generally differ in their food landscapes. Important factors that determine store choice and food choice, such as population density or vehicle ownership, also differ along the rural–urban divide. Metro versus nonmetro location was a binary variable, with 1 denoting metropolitan counties and 0 indicating nonmetro counties. According to the 2013 Rural–Urban Continuum Codes, metropolitan counties are divided into 3 subcategories by population: 1 million or more, 250 000 to 1 million, and fewer than 250 000.44
Census tracts referred to as food deserts must meet both low-income and low-access thresholds defined by the USDA.45 Low-income communities are tracts that have “either a poverty rate of 20 percent or greater, or a median family income at or below 80 percent of the area median family income.” Low-access communities, which differed between metro and nonmetro areas, were defined as tracts with “at least 500 persons and/or at least 33% of the census tract’s population live more than one mile (10 miles for non-metro tracts) from a supermarket or large grocery store.”45
Statistical Analysis
We calculated descriptive statistics for the variables at each level. We report means and standard deviations for continuous variables and percentages of observations equal to 1 for binary variables. To account for the multilevel data structure, we based our major analyses on random-intercept logistic models (or multilevel models) with random components at the individual, household, and neighborhood levels. The 2 dependent variables in the models involved 2 comparisons: (1) underweight or normal-weight versus overweight individuals and (2) underweight or normal-weight versus obese individuals. All models employed the variables at the 3 levels discussed earlier in the Methods section as independent variables. We calculated the conditional intraclass correlation coefficient for each model. We performed all statistical analyses using Stata version 13 (StataCorp LP, College Station, TX).
RESULTS
About one third of the total sample was overweight and about one third was obese, which was consistent with statistics based on other nationally representative surveys such as the National Health and Nutrition Examination Survey (NHANES; Table 2). Individuals in our adult sample had an average BMI of 28.50, which was comparable to a calculation by Flegal et al. of 28.7 for US adults based on measured heights and weights in the 2009 to 2010 NHANES.46 More than 85% of the households were non-Hispanic White and more than half had a college-educated household head. The average household size was 2 and the mean household income was estimated to be above $69 000.
TABLE 2—
Descriptive Statistics of Data Compiled From IRi Consumer Panel (2008–2012), Its Associated MedProfiler Data Set (2012), and County Business Patterns (2008): United States
| Variable | % or Mean ±SD |
| Individual level (n = 38 650)a | |
| BMI, kg/m2 | 27.54 ±7.08 |
| Overweight, % | 31.92 |
| Obese, % | 31.54 |
| Age, y | 50.81 ±20.39 |
| Female, % | 53.17 |
| Diet featureb | 0.00 ±1.00 |
| Fast food,c % | 3.29 |
| Exercise,d % | 39.98 |
| Household level (n = 18 381) | |
| USDAScore | 6.06 ±1.54 |
| Race/ethnicity, % | |
| Non-Hispanic White | 85.18 |
| Hispanic | 3.67 |
| Non-Hispanic Black | 8.31 |
| Asian | 2.88 |
| Other race | 2.09 |
| Household size | 2.15 ±1.14 |
| Income, $ | 69 141.68 ±43 366.38 |
| Education, % | |
| ≤ high school | 17.01 |
| Some college | 28.68 |
| College graduate | 35.35 |
| Post-college graduate | 18.96 |
| Married, % | 62.24 |
| Neighborhood levele | |
| Supermarket and other grocery stores (n = 2 103) | 2.20 ±1.24 |
| Clubs and supercenters (n = 2 103) | 0.18 ±0.18 |
| Convenience stores (n = 2 103) | 0.71 ±0.71 |
| Specialty food stores (n = 2 103) | 0.62 ±0.61 |
| Pharmacies and drug stores (n = 2 103) | 1.58 ±0.85 |
| Full-service restaurants (n = 2 103) | 7.45 ±4.12 |
| Limited-service restaurants (n = 2 103) | 6.09 ±2.19 |
| Poverty ratef (n = 1 583) | 16.37 ±5.86 |
| Metro areag (n = 2 104) | 47.34 |
| Food desert tracth (n = 14 511) | 5.66 |
Note. We report means and standard deviations for continuous variables, and percentages of observations equal to 1 for binary variables. BMI = body mass index.
Sample sizes for fast food and exercise are 38 646 and 38 644, respectively.
Diet feature is a factor analysis score constructed from 7 MedProfiler questions related to special diets, including high-fiber, high-protein, low-calorie, low-carbohydrate, low-fat, low-salt, and low-sugar diets. All responses to these dietary features were either yes (coded as 1) or no (0).
“Fast food” indicates whether the person eats at a fast-food restaurant on most days of a week.
“Exercise” indicates whether the person exercises for at least 20 minutes per day on most days of a week.
Food outlets at the neighborhood level are measured as the number of food store or restaurant establishments per 10 000 county residents. All the variables are measured at the county level, with 1 exception: food desert is measured at the census tract level.
“Poverty rate” measures the percentage of people below the federal poverty level in each county.
“Metro area” indicates metropolitan counties according to the 2013 Rural–Urban Continuum Codes from the USDA.
“Food desert tract” indicates census tracts that meet both low-income and low-access thresholds defined by the USDA.
Results from multilevel random intercept logistic models are presented in Table 3. Almost all the individual-level demographics and lifestyle choices were significantly associated with obesity or overweight status. Specifically, age was positively associated with obesity or overweight status, and being female was negatively associated with obesity or overweight status. A higher diet feature score was related to a higher probability of being obese or overweight, which was expected if individuals adopted special diets (low-fat, low-sugar, low-salt, etc.) when concerned about their weight or BMI. Although regular fast-food consumption was positively associated with obesity status, it was not significantly associated with overweight status. Finally, regular exercise was negatively related to the probability of obesity or overweight.
TABLE 3—
Associations Between Individual Household- and Neighborhood-Level Factors and Overweight or Obesity (Full Sample): United States, 2008–2012
| Variable | Obese vs Underweight or Normal Weighta (n = 25 023), ORb (95% CI) | Overweight vs Underweight or Normal Weighta (n = 25 237), ORb (95% CI) |
| Individual level | ||
| Age | 1.02 (1.02, 1.02) | 1.03 (1.02, 1.03) |
| Gender | ||
| Male (Ref) | 1 | 1 |
| Female | 0.61 (0.57, 0.66) | 0.48 (0.45, 0.51) |
| Diet feature | 1.63 (1.56, 1.70) | 1.18 (1.14, 1.22) |
| Fast food | 1.74 (1.41, 2.14) | 1.16 (0.97, 1.38) |
| Exercise | 0.24 (0.22, 0.26) | 0.64 (0.61, 0.68) |
| Household level | ||
| USDAScore | 0.93 (0.90, 0.96) | 0.99 (0.97, 1.01) |
| Race/ethnicity | ||
| Non-Hispanic White (Ref) | 1 | 1 |
| Hispanic | 1.02 (0.82, 1.27) | 1.04 (0.90, 1.21) |
| Non-Hispanic Black | 1.73 (1.47, 2.04) | 1.32 (1.17, 1.48) |
| Asian | 0.26 (0.20, 0.34) | 0.56 (0.48, 0.65) |
| Other race | 1.08 (0.81, 1.44) | 1.08 (0.88, 1.32) |
| Household size | 1.02 (0.97, 1.06) | 1.00 (0.97, 1.03) |
| Log (income) | 0.93 (0.87, 1.00) | 1.08 (1.03, 1.14) |
| Education | ||
| ≤ high school (Ref) | 1 | 1 |
| Some college | 0.99 (0.87, 1.14) | 1.03 (0.93, 1.14) |
| College graduate | 0.78 (0.68, 0.89) | 0.96 (0.87, 1.06) |
| Post-college graduate | 0.55 (0.47, 0.65) | 0.75 (0.67, 0.84) |
| Married | 0.95 (0.85, 1.07) | 1.05 (0.97, 1.14) |
| Neighborhood level | ||
| Supermarket and other grocery | 0.98 (0.90, 1.08) | 0.98 (0.93, 1.04) |
| Clubs and supercenters | 1.48 (0.87, 2.52) | 1.03 (0.72, 1.47) |
| Convenience stores | 1.04 (0.94, 1.14) | 1.02 (0.96, 1.08) |
| Specialty food stores | 0.92 (0.78, 1.08) | 0.92 (0.83, 1.03) |
| Pharmacies and drug stores | 1.01 (0.89, 1.14) | 1.07 (0.99, 1.16) |
| Full-service restaurants | 0.97 (0.94, 0.99) | 1.00 (0.98, 1.02) |
| Limited-service restaurants | 1.00 (0.96, 1.04) | 0.98 (0.95, 1.01) |
| Poverty rate | 1.00 (0.99, 1.01) | 0.99 (0.99, 1.00) |
| Metro | 0.79 (0.67, 0.92) | 0.91 (0.82, 1.02) |
| Food desert tract | 1.30 (1.06, 1.59) | 1.19 (1.02, 1.38) |
| Constant | 4.24 (1.91, 9.42) | 0.27 (0.15, 0.48) |
| ICC (2nd level) | 0.430 | 0.125 |
| ICC (3rd level) | 0.021 | 0.003 |
Note. CI = confidence interval; ICC = intraclass correlation coefficient; OR = odds ratio. Values reported for ICC in the table are conditional in that they are calculated when all the independent variables are included in the model.
Because of the small number in the underweight population, we combined the underweight and normal-weight population as the reference category.
Random-intercept logit models.
The household-level food environment measure, USDAScore, was negatively associated with the probability of obesity, after we controlled for a number of individual-, household-, and neighborhood-level covariates. However, it was not significantly associated with overweight status. A 1-point increase in average USDAScore would decrease the odds of obesity status by about 7% (odds ratio [OR] = 0.93; 95% confidence interval [CI] = 0.90, 0.96). On the basis of estimates of parameters from this model, we predicted the average probabilities of obesity with increasing levels of USDAScores by gender. The estimated probability of obesity for individuals living in households with the highest USDAScores (USDAScore = 13) was about 0.15 lower than for those in households with the lowest USDAScores (USDAScore = 1). Additional analysis indicated that county-level obesity rates were negatively correlated with average USDAScores at the county level (Pearson correlation coefficient = −0.12; P < .001).
Results from other household-level measures indicated significant socioeconomic disparities in obesity or overweight status. Compared with Whites, Non-Hispanic Blacks were more likely to be obese or overweight, whereas Asians had significantly lower probabilities of being obese or overweight. Although higher income was associated with lower odds of obesity, it was related to higher odds of being overweight. Individuals living in families with college- or post-college-educated household heads were less likely to be obese than those whose household heads had a high school education or less. Household size and marital status were not significantly associated with obesity or overweight status.
After adjustment for individual- and household-level characteristics, most store count measures of the neighborhood food environment were not significantly associated with obesity or overweight status. One exception was that densities of full-service restaurants were negatively associated with obesity status (OR = 0.97; 95% CI = 0.94, 0.99). County-level poverty rates were not significantly associated with obesity or overweight status. Living in metropolitan counties was significantly associated with lower odds of being obese. The tract-level food desert indicator was positively associated with obesity or overweight. With other factors remaining constant, a census tract–level switch from a non–food desert to a food desert increased an individual’s odds of being obese by about 30% (OR = 1.30; 95% CI = 1.06, 1.59) and of being overweight by about 19% (OR = 1.19; 95% CI = 1.02, 1.38).
DISCUSSION
Our study is among the first to encompass the roles of both food at home and the neighborhood food environment, along with a host of important controls, in studying obesity and overweight status prevalence. Our main food-at-home measure, USDAScore, largely performed in a manner consistent with dietary-quality indices used by other studies, in that higher compliance with the Dietary Guidelines for Americans was associated with lower risk of obesity status.34,35 Additional models, with USDAScore quartiles in place of the continuous USDAScores, showed that only high compliance or higher quartiles of USDAScores were associated with lower odds of being obese (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Overall, the food environment at the neighborhood level generally had less significant impact on overweight and obesity than individual- or household-level characteristics. Similar to what was reported by Mehta and Chang,21 higher densities of full-service restaurants were found to be associated with lower odds of being obese in this study. In contrast to most store format density measures, living in food desert tracts posed relatively strong risks for getting overweight or obese. Additionally, households in metro areas had a lower probability of being obese, which concurred with findings based on data from the 2005 to 2008 NHANES.47
We checked the robustness of our findings by estimating models applied to metro and nonmetro subsamples. Although descriptive statistics for the metro subsample differed significantly from those for the nonmetro subsample (Table B, available as a supplement to the online version of this article at http://www.ajph.org), estimation results from the subsamples were generally consistent throughout and similar to those from the full sample, with a few exceptions (Tables C and D, available as supplements to the online version of this article at http://www.ajph.org). Mixed results were found for the relationships between neighborhood food environment variables and obesity or overweight status. On the one hand, a food desert indicator was positively related to obesity or overweight status in the metro subsample. On the other hand, relationships between densities of various store types and obesity status had no strong or consistent pattern. Nonetheless, some of our mixed results were similar to those of other research. Consistent with the findings of Courtemanche and Carden2 and of Volpe et al.48 that increased expenditure shares from supercenters could reduce the healthfulness of households’ shopping basket, our study found that higher densities of club stores and supercenters were associated with higher odds of overweight or obesity status in our nonmetro subsample.
Although our study addressed some gaps in current research, several measurement issues are worth noting. First, rather than using traditional retrospective approaches employing food frequency questionnaires or 24-hour recalls, our study used scanner data to provide potentially more accurate information about the home food environment. However, the scanner data reflected purchases rather than consumption. Additionally, the scanner data and our USDAScore measure accounted only for food-at-home purchases, not food away from home. However, by controlling for fast-food consumption via responses in the MedProfiler data set, we sought to mitigate the effects of potentially omitted food-away-from-home variables. Our diet feature variable also accounted for individuals’ food choices and dietary restrictions.
Second, our study relied on self-reported information found in IRi’s MedProfiler data and might be subject to various measurement errors. A systematic review of previous studies comparing self-reported with measured heights and weights concluded that, in general, heights tend to be overreported and weights are underreported, leading to underestimated BMIs.49 However, this bias has been shown to be small and stable in the past 3 decades in the United States.50 If it was true for our sample, then the overweight and obesity prevalence might be slightly higher than what our data suggest.
Third, the number of food stores or restaurants per capita basically identified a “supply ratio,” but it did not take into consideration geographic distance and mobility obstacles to access the food outlets that might be measured if data were geocoded.18 However, the density measures were supplemented by the food desert indicator variable, which measured access to a supermarket or large grocery store within a predetermined distance, and which was significantly associated with obesity and overweight status in this study.
ACKNOWLEDGMENTS
This research was partially funded by the US Department of Agriculture’s Economic Research Service.
Note. The views expressed herein are those of the authors and do not necessarily reflect the views of the US Department of Agriculture.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because data were obtained from secondary sources.
Footnotes
See also Galea and Vaughan, p. 783.
REFERENCES
- 1.Dubowitz T, Ghosh-Dastidar M, Eibner C et al. The Women’s Health Initiative: the food environment, neighborhood socioeconomic status, BMI, and blood pressure. Obesity (Silver Spring) 2012;20(4):862–871. doi: 10.1038/oby.2011.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Courtemanche C, Carden A. Supersizing supercenters? The impact of Walmart Supercenters on body mass index and obesity. J Urban Econ. 2011;69(2):165–181. [Google Scholar]
- 3.Powell LM, Auld MC, Chaloupka FJ, O’Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4):S301–S307. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–495. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morland K, Roux AVD, Wing S. Supermarkets, other food stores, and obesity: The Atherosclerosis Risk in Communities Study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Prince SA, Kristjansson EA, Russell K et al. Relationships between neighborhoods, physical activity, and obesity: a multilevel analysis of a large Canadian city. Obesity (Silver Spring) 2012;20(10):2093–2100. doi: 10.1038/oby.2011.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ford PB, Dzewaltowski DA. Limited supermarket availability is not associated with obesity risk among participants in the Kansas WIC program. Obesity (Silver Spring) 2010;18(10):1944–1951. doi: 10.1038/oby.2009.487. [DOI] [PubMed] [Google Scholar]
- 8.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- 10.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3(1):2. doi: 10.1186/1479-5868-3-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of US adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring) 2014;22(3):868–874. doi: 10.1002/oby.20502. [DOI] [PubMed] [Google Scholar]
- 12.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J Urban Health. 2010;87(5):771–781. doi: 10.1007/s11524-010-9460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Galvez MP, Hong L, Choi E, Liao L, Godbold J, Brenner B. Childhood obesity and neighborhood food-store availability in an inner-city community. Acad Pediatr. 2009;9(5):339–343. doi: 10.1016/j.acap.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hickson DA, Diez Roux AV, Smith AE et al. Associations of fast food restaurant availability with dietary intake and weight among African Americans in the Jackson Heart Study, 2000–2004. Am J Public Health. 2011;101(suppl 1):S301–S309. doi: 10.2105/AJPH.2010.300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard PH, Fitzpatrick M, Fulfrost B. Proximity of food retailers to schools and rates of overweight ninth grade students: an ecological study in California. BMC Public Health. 2011;11(1):68. doi: 10.1186/1471-2458-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: differences by population density. Am J Health Promot. 2007;21(4 suppl):317–325. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- 17.Chou S-Y, Grossman M, Saffer H. An economic analysis of adult obesity: results from the Behavioral Risk Factor Surveillance System. J Health Econ. 2004;23(3):565–587. doi: 10.1016/j.jhealeco.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Inagami S, Cohen DA, Brown AF, Asch SM. Body mass index, neighborhood fast food and restaurant concentration, and car ownership. J Urban Health. 2009;86(5):683–695. doi: 10.1007/s11524-009-9379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li F, Harmer P, Cardinal BJ, Bosworth M, Johnson-Shelton D. Obesity and the built environment: does the density of neighborhood fast-food outlets matter? Am J Health Promot. 2009;23(3):203–209. doi: 10.4278/ajhp.071214133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19(2):137–143. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 21.Mehta NK, Chang VW. Weight status and restaurant availability: a multilevel analysis. Am J Prev Med. 2008;34(2):127–133. doi: 10.1016/j.amepre.2007.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crawford DA, Timperio AF, Salmon JA et al. Neighbourhood fast food outlets and obesity in children and adults: the CLAN Study. Int J Pediatr Obes. 2008;3(4):249–256. doi: 10.1080/17477160802113225. [DOI] [PubMed] [Google Scholar]
- 23.Davis B, Carpenter C. Proximity of fast-food restaurants to schools and adolescent obesity. Am J Public Health. 2009;99(3):505–510. doi: 10.2105/AJPH.2008.137638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reitzel LR, Regan SD, Nguyen N et al. Density and proximity of fast food restaurants and body mass index among African Americans. Am J Public Health. 2014;104(1):110–116. doi: 10.2105/AJPH.2012.301140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bryant M, Stevens J. Measurement of food availability in the home. Nutr Rev. 2006;64(2 pt 1):67–76. doi: 10.1301/nr.2006.feb.67-76. [DOI] [PubMed] [Google Scholar]
- 26.Pinard CA, Yaroch AL, Hart MH, Serrano EL, McFerren MM, Estabrooks PA. Measures of the home environment related to childhood obesity: a systematic review. Public Health Nutr. 2012;15(1):97–109. doi: 10.1017/S1368980011002059. [DOI] [PubMed] [Google Scholar]
- 27.Schatzkin A, Kipnis V, Carroll RJ et al. A comparison of a food frequency questionnaire with a 24-hour recall for use in an epidemiological cohort study: results from the biomarker-based Observing Protein and Energy Nutrition (OPEN) study. Int J Epidemiol. 2003;32(6):1054–1062. doi: 10.1093/ije/dyg264. [DOI] [PubMed] [Google Scholar]
- 28.Volpe R, Okrent A. Assessing the Healthfulness of Consumers’ Grocery Purchases. Washington, DC: USDA Economic Research Service; 2012. Report no. EIB-102. [Google Scholar]
- 29.Albuquerque RCR, Baltar VT, Marchioni DML. Breast cancer and dietary patterns: a systematic review. Nutr Rev. 2014;72(1):1–17. doi: 10.1111/nure.12083. [DOI] [PubMed] [Google Scholar]
- 30.Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104(4):615–635. doi: 10.1016/j.jada.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 31.Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. 2014;99(1):181–197. doi: 10.3945/ajcn.113.069880. [DOI] [PubMed] [Google Scholar]
- 32.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169(7):659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 33.Waijers PM, Feskens EJ, Ocké MC. A critical review of predefined diet quality scores. Br J Nutr. 2007;97(2):219–231. doi: 10.1017/S0007114507250421. [DOI] [PubMed] [Google Scholar]
- 34.Gao SK, Beresford SA, Frank LL, Schreiner PJ, Burke GL, Fitzpatrick AL. Modifications to the Healthy Eating Index and its ability to predict obesity: the Multi-Ethnic Study of Atherosclerosis. Am J Clin Nutr. 2008;88(1):64–69. doi: 10.1093/ajcn/88.1.64. [DOI] [PubMed] [Google Scholar]
- 35.Guo X, Warden B, Paeratakul S, Bray G. Healthy eating index and obesity. Eur J Clin Nutr. 2004;58(12):1580–1586. doi: 10.1038/sj.ejcn.1601989. [DOI] [PubMed] [Google Scholar]
- 36.Zamora D, Gordon-Larsen P, Jacobs DR, Popkin BM. Diet quality and weight gain among black and white young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study (1985–2005) Am J Clin Nutr. 2010;92(4):784–793. doi: 10.3945/ajcn.2010.29161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumanyika SK, Obarzanek E. Pathways to obesity prevention: report of a National Institutes of Health workshop. Obes Res. 2003;11(10):1263–1274. doi: 10.1038/oby.2003.172. [DOI] [PubMed] [Google Scholar]
- 38.Smedley BD, Syme SL. Promoting health: intervention strategies from social and behavioral research. Am J Health Promot. 2001;15(3):149–166. doi: 10.4278/0890-1171-15.3.149. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Percentile data files with LMS values. Available at: http://www.cdc.gov/growthcharts/percentile_data_files.htm. Accessed December 10, 2014.
- 40.Centers for Disease Control and Prevention. Defining childhood obesity. Available at: http://www.cdc.gov/obesity/childhood/defining.html. Accessed December 10, 2014.
- 41.Morland K, Wing S, Roux AD, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22(1):23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 42.Alviola PA, Nayga RM, Thomsen MR, Danforth D, Smartt J. The effect of fast-food restaurants on childhood obesity: a school level analysis. Econ Hum Biol. 2014;12:110–119. doi: 10.1016/j.ehb.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 43.Chen SE, Florax RJ, Snyder SD. Obesity and fast food in urban markets: a new approach using geo-referenced micro data. Health Econ. 2013;22(7):835–856. doi: 10.1002/hec.2863. [DOI] [PubMed] [Google Scholar]
- 44.US Dept of Agriculture. Economic Research Service. Rural–Urban Continuum Codes. Available at: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx. Accessed December 10, 2014.
- 45.US Dept of Agriculture, Agricultural Marketing Service. Food deserts. Available at: http://apps.ams.usda.gov/fooddeserts/fooddeserts.aspx. Accessed December 10, 2014.
- 46.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 47.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the united states: findings from NHANES (2005–2008) J Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Volpe R, Okrent A, Leibtag E. The effect of supercenter-format stores on the healthfulness of consumers’ grocery purchases. Am J Agric Econ. 2013;95(3):568–589. [Google Scholar]
- 49.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 50.Connor Gorber S, Tremblay MS. The bias in self-reported obesity from 1976 to 2005: a Canada–US comparison. Obesity (Silver Spring) 2010;18(2):354–361. doi: 10.1038/oby.2009.206. [DOI] [PubMed] [Google Scholar]


