Abstract
Objectives. To quantify inequalities in rates of unintentional injury–related hospitalizations between Australian Aboriginal and non-Aboriginal children.
Methods. We used linked hospital and mortality data to construct a retrospective whole-of-population birth cohort including 1 124 717 children born in the state of New South Wales, Australia, between July 1, 2000 and December 31, 2012. We adjusted hazard ratios (HRs) of first injury hospitalization for geographic clustering and individual- and area-level factors.
Results. Aboriginal children were 1.6 times more likely than were non-Aboriginal children to be hospitalized for an unintentional injury. The largest inequalities were for poisoning (HR = 2.7; 95% CI = 2.4, 3.0) and injuries stemming from exposure to fire, flames, heat, and hot substances (HR = 2.4; 95% CI = 2.1, 2.7). Adjustment reduced the inequality for all unintentional injury overall (HR = 1.4; 95% CI = 1.3, 1.4) and within leading injury mechanisms.
Conclusions. Australian Aboriginal children suffer a disproportionately high burden of unintentional injury.
Australian Aboriginal people, like indigenous people worldwide, experience significant socioeconomic and health disadvantages.1,2 This is reflected in the large gap in life expectancy compared with non-Aboriginal Australians aged 9.7 years for girls and 11.5 years for boys.3 Aboriginal health disadvantage is evident from the early life period onward, with higher rates of hospitalization4 and higher infant and child mortality rates compared with non-Aboriginal children.5 Unintentional injury is a leading cause of morbidity and mortality in childhood and is an important contributor to childhood health inequalities.1 Rates of morbidity and mortality from unintentional injury are up to 5 times higher in Aboriginal than in non-Aboriginal children.6–8
These inequalities might, at least in part, be explained by the socioeconomic disadvantage Aboriginal peoples experience. Past policies of colonization and dispossession have led to a cycle of disadvantage, poor education, high unemployment, low income, separation of families, and overcrowded living conditions in Aboriginal peoples,9 all of which have been associated with an increased risk of child injury.10–12 However, it is not known how much socioeconomic disadvantage and other child injury risk factors contribute to the higher injury burden in Australian Aboriginal children.13 Moreover, a larger proportion of Aboriginal than non-Aboriginal people live in remote and in socioeconomically disadvantaged areas,14 which in turn have higher child injury rates.10,11,15,16 Accordingly, the difference in injury rates between Aboriginal and non-Aboriginal people is also likely to be influenced by the uneven population distribution.
Unintentional injuries in children are highly preventable and therefore present a key opportunity to “close the gap” in health and life expectancy between Aboriginal and non-Aboriginal children. However, there are limited injury prevention programs developed for Aboriginal children,17–19 and there is currently a paucity of data to inform the development of appropriate Aboriginal child injury prevention programs.9 Numerous previous Australian studies have investigated transportation-related injuries in Aboriginal children,7,8,20,21 but few have studied other common childhood injury mechanisms, such as burns, poisoning, and falls.6,7,22 There are no in-depth studies identifying priority areas for injury prevention, and no studies have accounted for geographical clustering and risk factors in the analysis of Aboriginal child injuries.13
Against this background, we explored hospitalization for unintentional injury in a whole-of-population cohort of children in the state of New South Wales (NSW), Australia to address the following questions: (1) What are the leading mechanisms resulting in hospitalized injury in Aboriginal children? (2) Which mechanisms resulting in hospitalized injury have the largest inequalities between Aboriginal and non-Aboriginal children? and (3) How much of the inequality is explained by geographic clustering and individual- and area-level risk factors?
METHODS
NSW is the most populous state in Australia, with an estimated 6 816 087 residents (1 318 990 children aged 0–14 years) in 2006.14 At the 2006 census, 2.2% of NSW residents self-identified as Aboriginal or Torres Strait Islander (7.0% of children aged 0–14 years), referred to henceforward as “Aboriginal” because Torres Strait Islander people make up only 0.1% of the NSW population.14 In 2006, in the whole of Australia, 5.1% of the Aboriginal population lived in remote or very remote areas, 51.6% lived in regional areas, and 43.3% lived in major cities.14 This compares with 0.5%, 26.3%, and 73.2%, respectively, for the non-Aboriginal population.14
Data Sources
We used hospital data from the NSW Admitted Patient Data Collection linked with mortality data from the NSW Register of Births, Deaths and Marriages. The Admitted Patient Data Collection includes records for all separations (discharges, transfers, and deaths) from all NSW public and private sector hospitals and day procedure centers.
Patient demographics and multiple diagnoses and procedures are recorded for each separation and coded according to the Australian modification of the International Statistical Classification of Diseases and Related Problems, 10th revision (ICD-10-AM).23
The Register of Births, Deaths and Marriages captures details of all deaths registered in NSW. The NSW Centre for Health Record Linkage performed probabilistic linkage of the data sets24 and supplied de-identified data sets including linked Admitted Patient Data Collection and Register of Births, Deaths and Marriages records from July 2000 to March 2014.
Participants
We used the linked data to define a cohort of children for our analysis. We included all children living in NSW who were born in a hospital in NSW between July 1, 2000 and December 31, 2012, to allow a minimum of 1 year of follow-up. We identified birth records from the Admitted Patient Data Collection data set using the following criteria: “live born infant” (ICD10-AM code Z38) in any diagnosis field or a date of birth greater than or equal to the admission date and less than or equal to the separation date (1 124 717 children, of which 35 779 were Aboriginal).
We excluded children if their gender was coded as indeterminate or missing or if there were discrepancies in their date of birth, admission, or discharge date on their birth record (293 non-Aboriginal and 30 Aboriginal children). A similar proportion of excluded Aboriginal and non-Aboriginal children were hospitalized for an unintentional injury (7% of non-Aboriginal and 11% of Aboriginal children) compared with the study cohort. The final study cohort consisted of 1 124 717 children (1 088 645 non-Aboriginal and 35 749 Aboriginal).
Analysis Variables
The study outcome was first hospitalization for unintentional injury, defined as a principal diagnosis of injury (ICD10-AM code S00-T75 or T79) and an external cause code of unintentional injury (ICD10-AM code V01–X59, Y85–Y86). We analyzed unintentional injuries overall and according to mechanism of injury using the Centers for Disease Control and Prevention injury matrix (Table A, available as a supplement to the online version of this article at http://www.ajph.org).25 The exposure under investigation was Aboriginal status, which we derived from the child’s birth record.
We identified the variables we used in the analysis from the child’s birth record to minimize differential misclassification bias, whereby children who were hospitalized more frequently during the study had more opportunities to update their status than did children who had fewer hospitalizations. Individual-level variables included gender, low birth weight (< 2500 g), prematurity (< 37 wk gestational age), and private health insurance or patient status as a proxy measure for family socioeconomic status (SES). Area-level variables were geographical remoteness and SES of the statistical local area of residence. We classified remoteness of residence using the Accessibility/Remoteness Index of Australia,26 which we grouped into 4 categories: major city, inner regional, outer regional, and remote or very remote areas. We obtained area-level SES from the Australian Bureau of Statistics’ Socio-Economic Index for Areas Index of Relative Social Advantage and Disadvantage,27 which we divided into population tertile groups.
Statistical Analyses
We calculated person-years at risk from the date of birth to the first of the following events: hospitalization for the relevant unintentional injury (all unintentional injuries combined, each specific injury mechanism), death, or end of follow-up (March 31, 2014). We calculated incidence rates by dividing the number of first unintentional injury hospital admissions by the person-years accumulated for Aboriginal and non-Aboriginal children. We calculated confidence intervals (CIs) assuming a Poisson distribution for the first injury hospitalization.
We built Cox regression models to explore the influence of geographical clustering and individual- and area-level covariates on relative risk of unintentional injury for Aboriginal compared with non-Aboriginal children across all years of follow-up. All models used age as the timescale. We adjusted a baseline model (model 1) for gender. Subsequent multilevel models nested children within their statistical local area of residence using a random intercept term (model 2), followed by models adjusting for individual- and area-level variables (models 3 and 4).
We explored possible variations in the effect of Aboriginal status according to remoteness and socioeconomic disadvantage by separately adding the relevant interaction terms to the final model (models 4a and 4b). We assessed the proportional hazards assumption graphically and by Schoenfeld residuals28 in single-level models and by including an interaction term of the covariate and the log of time in the multilevel models.29 We carried out statistical analyses using Stata version 1230 and SAS version 9.3.31 We performed multilevel analysis using SAS version 9.3 with the PHREG procedure.31
The choice of algorithm to identify Aboriginal status from hospital records has been shown to influence risk estimates when comparing Aboriginal and non-Aboriginal peoples.32 We carried out sensitivity analyses using Aboriginal status on the most recent hospital record and Aboriginal status on any hospital record during the study period.
RESULTS
We included 1 124 717 children in the cohort; of these, 35 749 children were Aboriginal. A larger proportion of Aboriginal than non-Aboriginal children were born prematurely (9.5% vs 6.0%) and had low birth weight (6.8% vs 3.7%). A much higher proportion of Aboriginal than non-Aboriginal children lived in remote and very remote areas (11.0% vs 0.7%) and the most disadvantaged areas (67.0% vs 32.0%; Table B, available as a supplement to the online version of this article at http://www.ajph.org).
Of children in the cohort, 75 393 (99.3 per 10 000 person-years) non-Aboriginal and 3412 (157.3 per 10 000 person-years) Aboriginal children were admitted to a NSW hospital for any first unintentional injury from 2000 to 2014. The leading injury mechanisms resulting in hospitalization in Aboriginal children were falls (63.3 per 10 000 person-years), injuries stemming from other specified causes (19.4 per 10 000 person-years), poisonings (15.2 per 10 000 person-years), and transportation-related injuries (14.1 per 10 000 person-years; Table 1). In non-Aboriginal children, the leading mechanisms were falls (48.0 per 10 000 person-years), injuries stemming from causes other specified (11.3 per 10 000 person-years), being struck by or against an object (8.7 per 10 000), and transportation-related injuries (7.6 per 10 000 person-years).
TABLE 1—
First Unintentional Injury Hospitalization by Injury Mechanism in Aboriginal and Non-Aboriginal Children: New South Wales, Australia, 2000–2014
| Aboriginal |
Non-Aboriginal |
||||||
| Injury Type | No. | Person-Years | Rate (95% CI) | No. | Person-Years | Rate (95% CI) | HR (95% CI) |
| All unintentional injury | 3412 | 216 812 | 157.33 (152.1, 162.71) | 75 393 | 7 592 982 | 99.30 (98.59, 100.01) | 1.58 (1.53, 1.64) |
| Fall | 1430 | 225 886 | 63.31 (60.07, 66.67) | 37 320 | 7 783 346 | 47.95 (47.46, 48.44) | 1.33 (1.26, 1.41) |
| Other specified | 446 | 230 134 | 19.38 (17.62, 21.26) | 8901 | 7 906 249 | 11.26 (11.03, 11.49) | 1.68 (1.53, 1.85) |
| Poisoning | 349 | 229 982 | 15.18 (13.62, 16.85) | 4129 | 7 923 084 | 5.21 (5.05, 5.37) | 2.72 (2.44, 3.03) |
| Transportation | 324 | 230 460 | 14.06 (12.57, 15.68) | 6040 | 7 922 924 | 7.62 (7.43, 7.82) | 1.97 (1.76, 2.20) |
| Struck by or against an object | 318 | 230 470 | 13.80 (12.32, 15.40) | 6853 | 7 919 477 | 8.65 (8.45, 8.86) | 1.61 (1.44, 1.80) |
| Fire, flames, heat, and hot substances | 289 | 230 319 | 12.55 (11.14, 14.08) | 3825 | 7 925 689 | 4.83 (4.67, 4.98) | 2.42 (2.15, 2.73) |
| Natural or environmental | 185 | 231 086 | 8.01 (6.89, 9.25) | 3204 | 7 934 282 | 4.04 (3.90, 4.18) | 1.97 (1.70, 2.28) |
| Cutting or piercing | 175 | 231 163 | 7.57 (6.49, 8.78) | 3542 | 7 933 344 | 4.46 (4.32, 4.61) | 1.71 (1.47, 1.99) |
Note. CI = confidence interval; HR = hazard ratio.
Statistical Modeling of Inequalities
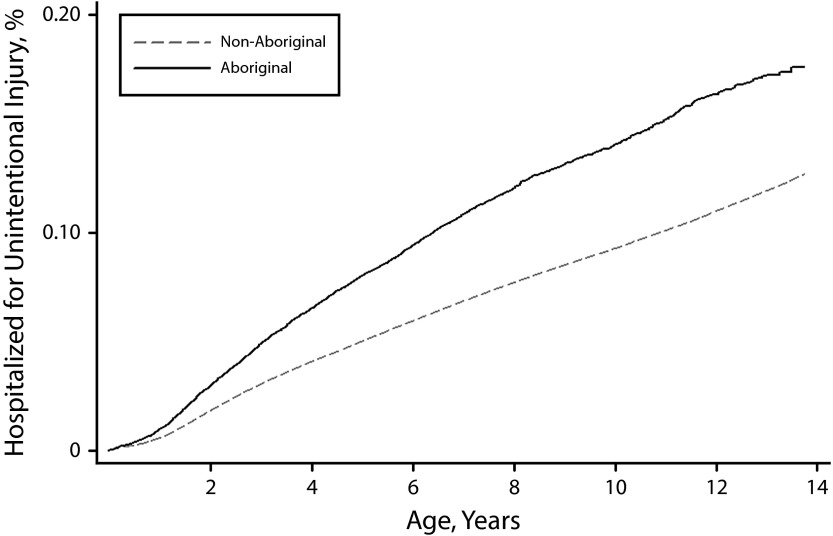
Aboriginal children had an elevated risk of hospitalization for any unintentional injury (HR = 1.58; 95% CI = 1.53, 1.64) compared with non-Aboriginal children. The largest differences were observed for poisoning (HR = 2.72; 95% CI = 2.44, 3.03); exposure to fire, flames, heat, and hot substances (HR = 2.42; 95% CI = 2.15, 2.73); and transportation-related injuries (HR = 1.97; 95% CI = 1.76, 2.20), whereas the smallest difference was for falls (HR = 1.33; 95% CI = 1.26, 1.41; Table 1). For all unintentional injuries combined, Aboriginal children had a higher probability of being admitted to a hospital from birth to age 13 years than did non-Aboriginal children (Figure 1).
FIGURE 1—
Probability of Hospitalization for Unintentional Injury by Age in a Cohort of Aboriginal and Non-Aboriginal Children: New South Wales, Australia, 2000–2014
Adjusting for clustering by area of residence reduced the inequality for all unintentional injuries (HR = 1.42; 95% CI = 1.37, 1.48). For the injury mechanisms with the largest inequalities, after adjusting for area, the Aboriginal to non-Aboriginal hazard ratio (HR) decreased for poisoning to 2.01 (95% CI = 1.79, 2.26); for injuries caused by fire, flames, heat, and hot substances to 2.05 (95% CI = 1.81, 2.32); and for transportation-related injuries to 1.41 (95% CI = 1.25, 1.58; Table 2). Adding individual- and area-level factors to the model further reduced the Aboriginal to non-Aboriginal HR for all unintentional injuries combined to 1.39 (95% CI = 1.34, 1.44); for poisoning to 1.76 (95% CI = 1.57, 1.98); for injuries caused by fire, flames, heat, and hot substances to 1.76 (95% CI = 1.55, 2.00); and for transportation-related injuries to 1.28 (95% CI = 1.13, 1.43; Table 2). The largest relative decreases in Aboriginal to non-Aboriginal HR in the fully adjusted model were for poisoning, transportation-related injuries, and injuries stemming from natural and environmental causes. In comparison, adjusting for clustering by area and covariates had only a small effect on the size of the inequality for injuries stemming from being struck by or against an object, falls, and cutting and piercing.
TABLE 2—
Sequentially Adjusted Aboriginal to Non-Aboriginal HRs for Hospitalization for an Unintentional Injury: New South Wales, Australia, 2000–2014
| Injury Type | Model 1,a HR (95% CI) | Model 2,b HR (95% CI) | Model 3,c HR (95% CI) | Model 4,d HR (95% CI) |
| All unintentional injury | 1.58 (1.53, 1.64) | 1.42 (1.37, 1.48) | 1.40 (1.35, 1.45) | 1.39 (1.34, 1.44) |
| Poisoning | 2.72 (2.44, 3.03) | 2.01 (1.79, 2.26) | 1.84 (1.64, 2.07) | 1.76 (1.57, 1.98) |
| Fire, flames, heat, and hot substances | 2.42 (2.15, 2.72) | 2.05 (1.81, 2.32) | 1.87 (1.65, 2.12) | 1.76 (1.55, 2.00) |
| Transportation | 1.97 (1.76, 2.20) | 1.41 (1.25, 1.58) | 1.35 (1.20, 1.52) | 1.28 (1.13, 1.43) |
| Natural and environmental | 1.97 (1.70, 2.28) | 1.48 (1.27, 1.73) | 1.40 (1.20, 1.64) | 1.30 (1.11, 1.52) |
| Cutting and piercing | 1.71 (1.47, 1.99) | 1.68 (1.44, 1.96) | 1.60 (1.37, 1.87) | 1.56 (1.33, 1.84) |
| Other specified | 1.68 (1.53, 1.85) | 1.62 (1.47, 1.78) | 1.55 (1.41, 1.71) | 1.50 (1.36, 1.66) |
| Struck by or against an object | 1.61 (1.44, 1.80) | 1.61 (1.43, 1.80) | 1.58 (1.41, 1.78) | 1.55 (1.38, 1.75) |
| Fall | 1.33 (1.27, 1.41) | 1.27 (1.20, 1.34) | 1.26 (1.20, 1.34) | 1.25 (1.19, 1.32) |
Note. CI = confidence interval; HR = hazard ratio.
Sequentially adjusted for gender.
Sequentially adjusted for statistical local area of residence (random intercept).
Sequentially adjusted for individual-level covariates. Low birth weight (< 2500 g), premature birth (< 37 wk gestational age), and private patient or private health insurance.
Sequentially adjusted for area-level covariates. Accessibility/Remoteness Index of Australia and Index of Relative Socio-Economic Advantage and Disadvantage.
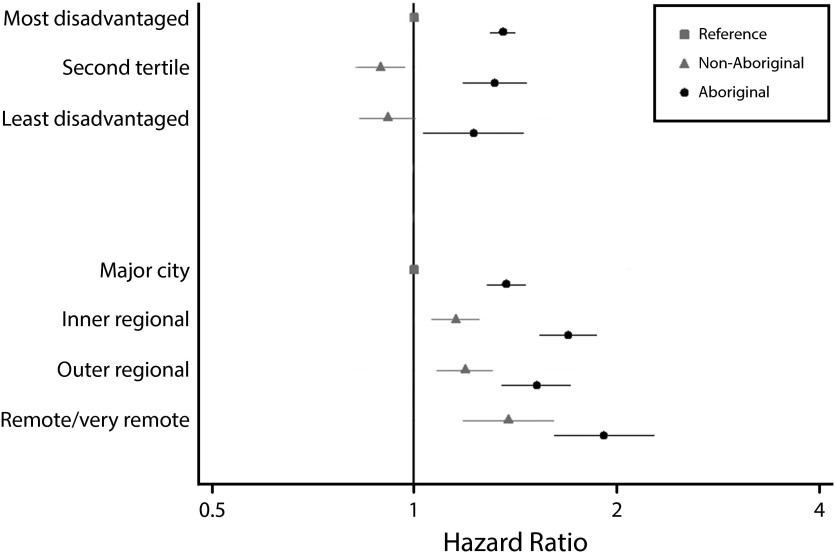
The inclusion of interaction terms of the Accessibility/Remoteness Index of Australia (model 4a) and the Socio-Economic Index for Areas (model 4b) with Aboriginality showed a consistently higher risk of injury hospitalization for Aboriginal children for all categories of area-level SES and remoteness (Figure 2). The size of the inequality varied by geography for the different injury mechanisms; for transportation-related injuries and poisoning, the largest inequalities were observed in major cities, whereas for injuries caused by fire, flames, heat, and hot substances, the largest inequality was in remote and very remote areas (Figure A, available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 2—
Adjusted Hazard Ratios for Hospitalization for Unintentional Injury for Interaction Terms Aboriginality × Area Socioeconomic Status and Aboriginality × Remoteness: New South Wales, Australia, 2000–2014
Note. Adjusted hazard ratios accounted for clustering within statistical local area and other covariates (model 4). Error bars represent 95% confidence intervals. We added interactions separately to the model. The referent groups were non-Aboriginal children living in most disadvantaged areas and non-Aboriginal children living in major cities. SES is from the Index of Relative Socio-Economic Advantage and Disadvantage. We obtained remoteness from the Accessibility/Remoteness Index of Australia.
Sensitivity Analyses
We identified 40 521 children in the cohort as Aboriginal on their most recent hospital record, which increased to 43 734 when we used any of their hospital records to identify their Aboriginal status.
The measure of inequality between Aboriginal and non-Aboriginal children increased using these alternative algorithms, producing unadjusted HRs of 1.9 (95% CI = 1.8, 2.0) using Aboriginal status from the most recent hospital record and 2.0 (95% CI = 1.9, 2.1) using ever recorded as Aboriginal and adjusted HRs (model 4) of 1.7 (95% CI = 1.6, 1.7) and 1.8 (95% 1.7, 1.8), respectively.
DISCUSSION
To our knowledge, this is the first study using a whole-of-population cohort study design to investigate differences in hospitalization for unintentional injury between Aboriginal and non-Aboriginal children in Australia. We observed a significantly higher overall risk of first hospitalization for an unintentional injury in Aboriginal compared with non-Aboriginal children aged 0 to 13 years.
The leading mechanisms for hospitalized injury in Aboriginal children were falls, injuries stemming from other specified causes, and poisoning. The main injury types included in other specified causes were foreign objects getting stuck in the child’s body and being caught between objects. Injury mechanisms with the highest inequalities between Aboriginal and non-Aboriginal children were poisoning; fire, flames, heat, and hot substances; and transportation.
For all unintentional injuries combined, the injury inequalities increased from age 1 year and kept increasing to the maximum of age 13 years. Adjusting for geographical clustering and individual- and area-level covariates in the analysis reduced the inequalities in unintentional injury between Aboriginal and non-Aboriginal children, but substantial differences remained.
The higher injury rates in Aboriginal children we observed were consistent with findings of previous national and regional Australian studies.6–8,20–22,33,34 Although few of these studies compared different injury mechanisms, some of the largest differences in hospitalization were also reported for poisoning,6,7 transportation,7,8,20,21 and fire, flames, heat, and hot substances.6,7 Compared with a previous cross-sectional study for NSW,7 we found greater inequalities for injuries caused by transportation; poisoning; exposure to fire, flames, heat, and hot substances; and falls.
The greater risk estimates for Aboriginal compared with non-Aboriginal children in our study compared with the previous study7 is likely to be explained by differences in study design. Whereas the previous NSW study7 used census population estimates for denominator data, our study derived person-years at risk from the cohort data, thus using the same method of identification of Aboriginal children in the numerator and denominator for calculation of rates. As a consequence, we avoided the problem of numerator–denominator bias arising from differences in the way that Aboriginal status is recorded in hospital35 and population census data.36 Our results therefore suggest that the inequalities in unintentional injuries between Aboriginal and non-Aboriginal children are even larger than previously reported. This is further supported by the results of our sensitivity analyses using different algorithms for identifying Aboriginal status from hospital records. These yielded greater risk estimates than did those produced using Aboriginal status from the birth record, suggesting that our results may be conservative.
Previously, no Australian studies have considered risk factors in the analysis of unintentional injury in Aboriginal children,13 and only 1 study looked at the effect of geographic clustering in the analysis of road transportation–related injuries in Aboriginal peoples of all ages.37 This study showed a differential impact of adjusting for geographic clustering on injury hospitalization for Aboriginal and non-Aboriginal peoples for different types of transportation-related injury.37
Similarly, multilevel whole-of-population studies from the United Kingdom, Sweden, and Korea38–41 have highlighted the contribution of individual- and area-level factors to child injury. In our study, adjusting for geographical clustering reduced the inequalities for all major injury mechanisms but did not make them disappear, suggesting that contextual area factors contribute to, but do not fully explain, inequalities in injury. This geographical clustering effect is likely to reflect the much larger proportion of Aboriginal children who live in rural and remote areas and in disadvantaged areas, which in turn has been linked with an increased risk of child injury.10,11,15,16,40 High injury rates in more remote areas might be owing to a greater risk of injury from natural and environmental causes and motor vehicle crashes as well as greater exposure to risk factors in farming environments.15,16
Additionally, confounding by socioeconomic factors is likely to contribute to the higher injury rates in remote areas, because those living in remote areas tend to be more socioeconomically disadvantaged.42–44 In our analysis, adjustment for private health insurance and patient status, a proxy measure of family SES, accounted for some of the inequality between Aboriginal and non-Aboriginal children for the major injury mechanisms. This is consistent with previous findings of an association between SES and child injury.10 The underlying causes may be greater exposure to a wider range of hazards in the living environment and a lack of means of protection in families of low SES.10 For example, in poorer households parents may have less time to supervise their children; families may not be able to afford safety equipment, such as smoke alarms, stair gates, window locks, and safety helmets; and families may live in overcrowded houses with a lack of space for safe play and near streets with high traffic volume.11,12,45,46
Previous population-based studies have shown a link between low birth weight and premature birth and child injury.47,48 This association remained after adjusting for SES and has been explained by the fact that children born prematurely or of low birth weight are frailer and have slower cognitive development, which may put them at a higher risk of injury.48 Although higher proportions of Aboriginal than non-Aboriginal children in our cohort were born prematurely and had low birth weight, these factors explained little in the way of inequalities in unintentional injury once we adjusted for other factors.
Limitations
There are limitations to our study, some of which are inherent to the use of routinely collected hospital data. Our study, like others using these data, was restricted to the more severe injuries resulting in hospitalization.7,8 At present, there is no available source of data on injuries treated in the primary care setting in Australia. Potential inaccuracies in the external cause coding in hospital data have been highlighted previously.49–52
Our analysis was limited to the risk factors available in the routinely collected data. In the fully adjusted model we still observed considerable inequalities for injuries stemming from poisoning and fire, flames, heat, and hot substances. Both these injury mechanisms have been shown to be strongly associated with SES.10 We restricted our measures of SES to private health insurance or private patient status, a proxy measure at the family level and an area-level composite measure of socioeconomic disadvantage. More detailed measures of factors at the family level (e.g., parental education and employment and quality of housing) and other structural factors (e.g., availability of quality child care) would assist in identifying modifiable factors that might impinge on parents’ ability to protect their children.
In addition, underreporting indigenous status in routinely collected data is a recognized problem,32,53–56 which can lead to underascertainment of health outcomes, including hospitalization for injury, in Aboriginal children. We used Aboriginal status from the birth record in our analysis to minimize the effect of differential misclassification bias whereby sicker children who are admitted to a hospital more frequently would have had more opportunity to be recorded as Aboriginal. Additionally, the interstate migration of children after birth or admission to hospitals in other Australian states may have further biased our risk estimates in a downward direction. Although population mobility is lower for children than for older individuals, there is greater mobility in the Aboriginal than the non-Aboriginal population.57
Conclusions and Implications for Practice
Despite the national goals to reduce health inequalities between Aboriginal and non-Aboriginal peoples and to reduce childhood injury,58,59 there are substantial inequalities in hospitalizations for unintentional injuries between Aboriginal and non-Aboriginal children in NSW. Previous studies suggest that our findings are in line with those reported for other states in Australia.6,8,20–22,33,34 However, our results also indicate that these inequalities are even larger than previously reported and are not only a result of the greater proportion of Aboriginal people living in rural areas, as has been discussed previously.9,18 Comparing a large range of injury mechanisms, we identified priority targets for injury prevention in terms of injury burden and inequalities.
Additionally, our study showed an injury gradient by geographical remoteness for the leading injury mechanisms, and we found that inequalities are largest in major cities and inner regional areas. These findings indicate that injury prevention measures that specifically address injury risks in Aboriginal children and geographically focused interventions that target areas with high rates of child injury have the potential to improve Aboriginal child health and reduce health inequalities. However, broad population-level prevention programs are unlikely to reduce these health inequalities60 or might even increase them through differential uptake of safety measures.61 With the exception of road transportation,62 there are few current prevention activities that specifically target Aboriginal children.17,63,64
Available evidence from Australian and international studies indicates that to be successful, injury prevention programs targeted at Aboriginal communities should be multicomponent and tailored to the community, incorporate Aboriginal views of health, and involve communities in development and implementation.63,65 Moreover, they should consider the local conditions, geographical location, access to services, distinct cultures, and social structures of Aboriginal communities.9,17,63
However, the underlying socioeconomic gradient in injury hospitalization rates suggests that over and above injury prevention programs, there is potential scope to reduce child injury inequalities through policies and programs that address inequities in the broader social determinants of health.
ACKNOWLEDGMENTS
H. Möller and K. Falster were supported by a National Health and Medical Research Council (NHMRC) capacity building grant (573122). K. Falster was also supported by a NHMRC Early Career Fellowship grant (1016475). R. Ivers was supported by fellowship funding from the NHMRC (grant APP1031781).
The authors would like to thank Sanja Lujic of the University of New South Wales for statistical advice. We are grateful to the reviewers for their constructive and helpful comments. We acknowledge the New South Wales (NSW) Ministry of Health and NSW Registry of Births, Deaths, and Marriages for allowing us access to the data and the Center for Health Record Linkage for conducting the probabilistic linkage of records.
HUMAN PARTICIPANT PROTECTION
The study was approved by the New South Wales Research Ethics Committee, the Aboriginal Health and Medical Research Council, and the University of Western Sydney Human Research Ethics Committee.
REFERENCES
- 1.Australian Institute of Health and Welfare. The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander People, an Overview. Canberra, Australia: 2011. [Google Scholar]
- 2.Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65–75. doi: 10.1016/S0140-6736(09)60914-4. [DOI] [PubMed] [Google Scholar]
- 3.Australian Bureau of Statistics. Experimental Life Tables for Aboriginal and Torres Strait Islander Australians, 2005–2007. Canberra, Australia: 2009. [Google Scholar]
- 4.Australian Indigenous HealthInfoNet. Overview of Australian Indigenous Health Status, 2013. Perth, Australia: 2014. [Google Scholar]
- 5.Australian Institute of Health and Welfare. A Picture of Australia’s Children 2012. Canberra, Australia: 2012. [Google Scholar]
- 6.Australian Institute of Health and Welfare. Aboriginal and Torres Strait Islander Child Safety. Canberra, Australia: 2011. [Google Scholar]
- 7.Walter S. Mortality and Hospitilisation Due to Injury in the Aboriginal Population of New South Wales. North Sydney, Australia: New South Wales Department of Health; 2010. [Google Scholar]
- 8.Henley G, Harrison JE. Injury of Aboriginal and Torres Strait Islander People Due to Transport 2005–2006 to 2009–2010. Canberra, Australia: Australian Institute of Health and Welfare; 2013. [Google Scholar]
- 9.Ivers R, Clapham K, Senserrick T, Lyford M, Stevenson M. Injury prevention in Australian Indigenous communities. Injury. 2008;39(suppl 5):S61–S67. doi: 10.1016/S0020-1383(08)70030-5. [DOI] [PubMed] [Google Scholar]
- 10.Laflamme L, Hasselberg M, Burrows S. 20 years of research on socioeconomic inequality and children’s unintentional injuries: understanding the cause-specific evidence at hand. Int J Pediatr. 2010 doi: 10.1155/2010/819687. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearson M, Hewson P, Moxham T, Taylor R. Review 2: A Systematic Review of Risk Factors for Unintentional Injuries Among Children and Young People Aged Under 15 Years. Quantitative Correlates Review of Unintentional Injury in Children. Exeter, PA: Peninsula Technology Assessment Group, Peninsula Medical School; 2009. [Google Scholar]
- 12.Peden MM, Oyegbite K, Ozanne-Smith J, editors. World Report on Child Injury Prevention. Geneva, Switzerland: World Health Organisation; United Nations International Children’s Emergency Fund; 2008. [Google Scholar]
- 13.Möller H, Falster K, Ivers R, Jorm L. Inequalities in unintentional injuries between indigenous and non-indigenous children: a systematic review. Inj Prev. 2015;21(e1):e144–e152. doi: 10.1136/injuryprev-2013-041133. [DOI] [PubMed] [Google Scholar]
- 14.Australian Bureau of Statistics. Experimental Estimates of Aboriginal and Torres Strait Islander Australians, June 2006. Canberra, Australia: 2008. [Google Scholar]
- 15.Kim K, Ozegovic D, Voaklander DC. Differences in incidence of injury between rural and urban children in Canada and the USA: a systematic review. Inj Prev. 2012;18(4):264–271. doi: 10.1136/injuryprev-2011-040306. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell RJ, Chong S. Comparison of injury-related hospitalised morbidity and mortality in urban and rural areas in Australia. Rural Remote Health. 2010;10(1):1326. [PubMed] [Google Scholar]
- 17.Möller J, Thomson N, Brooks J, Clapham K. Injury Prevention Activity Among Aboriginal and Torres Strait Islander Peoples. Canberra, Australia: Australian Department of Health and Ageing; 2003. [Google Scholar]
- 18.Clapham K, Senserrick T, Ivers R, Lyford M, Stevenson M. Understanding the extent and impact of Indigenous road trauma. Injury. 2008;39(suppl 5):S19–S23. doi: 10.1016/S0020-1383(08)70025-1. [DOI] [PubMed] [Google Scholar]
- 19.Azzopardi PS, Kennedy EC, Patton GC et al. The quality of health research for young indigenous Australians: systematic review. Med J Aust. 2013;199(1):57–63. doi: 10.5694/mja12.11141. [DOI] [PubMed] [Google Scholar]
- 20.Cercarelli LR. Road crashes involving Aboriginal people in Western Australia. Accid Anal Prev. 1994;26(3):361–369. doi: 10.1016/0001-4575(94)90009-4. [DOI] [PubMed] [Google Scholar]
- 21.Cercarelli LR, Knuiman MW. Trends in road injury hospitalisation rates for Aboriginal and non-Aboriginal people in Western Australia, 1971–97. Inj Prev. 2002;8(3):211–215. doi: 10.1136/ip.8.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moorin RE, Hendrie D. The epidemiology and cost of falls requiring hospitalisation in children in Western Australia: a study using linked administrative data. Accid Anal Prev. 2008;40(1):216–222. doi: 10.1016/j.aap.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 23.National Centre for Classification in Health. The International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Australian Modification (ICD-10-AM) 6th ed. Sydney, Australia: 2008. [PubMed] [Google Scholar]
- 24.Centre for Health Record Linkage. Available at: http://www.cherel.org.au. Accessed January, 23, 2016.
- 25.Centers for Disease Control and Prvention. ICD framework: external cause of injury mortality matrix. 2002. Available at: http://www.cdc.gov/nchs/injury/ice/matrix10.htm. Accessed June 12, 2015.
- 26.Australian Bureau of Statistics. Australian Standard Geographical Classification (ASGC) Remoteness Classification: Purpose and Use. Canberra, Australia: 2003. [Google Scholar]
- 27.Australian Bureau of Statistics. Socio-Economic Indexes for Area (SEIFA)—Technical Paper 2006. Canberra, Australia: 2008. [Google Scholar]
- 28.Schoenfeld D. Partial residuals for the proportional hazards regression model. Biometrika. 1982;69(1):239–241. [Google Scholar]
- 29.Yang M, Goldstein H. Modelling Survival Data in MLwiN 1.20. London, UK: Institute of Education, University of London; 2003. [Google Scholar]
- 30. Stata Statistical Software, Release 12. [computer program]. College Station, TX: StataCorp LP; 2011.
- 31. SAS/STAT, Version 9.2. [computer program]. Cary, NC: SAS Institute; 2011.
- 32.Randall DA, Lujic S, Leyland AH, Jorm LR. Statistical methods to enhance reporting of Aboriginal Australians in routine hospital records using data linkage affect estimates of health disparities. Aust N Z J Public Health. 2013;37(5):442–449. doi: 10.1111/1753-6405.12114. [DOI] [PubMed] [Google Scholar]
- 33.Vimpani G, Doudle M, Harris R. Child accident-mortality in the Northern Territory, 1978–1985. Med J Aust. 1988;148(8):392–395. doi: 10.5694/j.1326-5377.1988.tb115963.x. [DOI] [PubMed] [Google Scholar]
- 34.Silva DT, Ruben AR, Wronski I, Stronach P, Woods M. Excessive rates of childhood mortality in the Northern Territory, 1985–94. J Paediatr Child Health. 1998;34(1):63–68. doi: 10.1046/j.1440-1754.1998.00156.x. [DOI] [PubMed] [Google Scholar]
- 35.Australian Institute of Health and Welfare. National Best Practice Guidelines for Collecting Indigenous Status in Health Data Sets. Canberra, Australia: 2010. [Google Scholar]
- 36.Australian Bureau of Statistics. Estimates of Aboriginal and Torres Strait Islander Australians, June 2011. Canberra, Australia: 2013. [Google Scholar]
- 37.Falster MO, Randall DA, Lujic S, Ivers R, Leylandd AH, Jorma LR. Disentangling the impacts of geography and Aboriginality on serious road transport injuries in New South Wales. Accid Anal Prev. 2013;54:32–38. doi: 10.1016/j.aap.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 38.Laflamme L, Hasselberg M, Reimers AM, Cavalini LT, Ponce de Leon A. Social determinants of child and adolescent traffic-related and intentional injuries: a multilevel study in Stockholm County. Soc Sci Med. 2009;68(10):1826–1834. doi: 10.1016/j.socscimed.2009.02.050. [DOI] [PubMed] [Google Scholar]
- 39.Haynes R, Reading R, Gale S. Household and neighbourhood risks for injury to 5–14 year old children. Soc Sci Med. 2003;57(4):625–636. doi: 10.1016/s0277-9536(02)00446-x. [DOI] [PubMed] [Google Scholar]
- 40.Kim MH, Subramanian SV, Kawachi I, Kim CY. Association between childhood fatal injuries and socioeconomic position at individual and area levels: a multilevel study. J Epidemiol Community Health. 2007;61(2):135–140. doi: 10.1136/jech.2006.047738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reading R, Jones A, Haynes R, Daras K, Emond A. Individual factors explain neighbourhood variations in accidents to children under 5 years of age. Soc Sci Med. 2008;67(6):915–927. doi: 10.1016/j.socscimed.2008.05.018. [DOI] [PubMed] [Google Scholar]
- 42.National Rural Health Alliance. Income Inequality Experienced by the People of Rural and Remote Australia. Deakin, Australia: 2014. [Google Scholar]
- 43.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94(10):1695–1703. doi: 10.2105/ajph.94.10.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith KB, Humphreys JS, Wilson MG. Addressing the health disadvantage of rural populations: how does epidemiological evidence inform rural health policies and research? Aust J Rural Health. 2008;16(2):56–66. doi: 10.1111/j.1440-1584.2008.00953.x. [DOI] [PubMed] [Google Scholar]
- 45.Schwebel DC, Gaines J. Pediatric unintentional injury: behavioral risk factors and implications for prevention. J Dev Behav Pediatr. 2007;28(3):245–254. doi: 10.1097/01.DBP.0000268561.80204.2a. [DOI] [PubMed] [Google Scholar]
- 46.Morrongiello BA, McArthur BA. Parent supervision to prevent injuries. In: Rivara F, editor. Injury Prevention. Encyclopedia of Early Childhood Development. Montreal, Canada: Centre of Excellence for Early Childhood Development and Strategic Knowledge Cluster on Early Child Development; 2010. pp. 16–21. [Google Scholar]
- 47.Jain A, Khoshnood B, Lee KS, Concato J. Injury related infant death: the impact of race and birth weight. Inj Prev. 2001;7(2):135–140. doi: 10.1136/ip.7.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sun Y, Hsu P, Vestergaard M, Christensen J, Li J, Olsenb J. Gestational age, birth weight, and risk for injuries in childhood. Epidemiology. 2010;21(5):650–657. doi: 10.1097/EDE.0b013e3181e94253. [DOI] [PubMed] [Google Scholar]
- 49.Bowman SM, Aitken ME. Assessing external cause of injury coding accuracy for transport injury hospitalizations. Perspect Health Inf Manag. 2011 Epub ahead of print. [PMC free article] [PubMed] [Google Scholar]
- 50.McKenzie K, Enraght-Moony EL, Walker SM, McClure RJ, Harrison JE. Accuracy of external cause-of-injury coding in hospital records. Inj Prev. 2009;15(1):60–64. doi: 10.1136/ip.2008.019935. [DOI] [PubMed] [Google Scholar]
- 51.LeMier M, Cummings P, West TA. Accuracy of external cause of injury codes reported in Washington State hospital discharge records. Inj Prev. 2001;7(4):334–338. doi: 10.1136/ip.7.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Davie G, Langley J, Samaranayaka A, Wetherspoon ME. Accuracy of injury coding under ICD-10-AM for New Zealand public hospital discharges. Inj Prev. 2008;14(5):319–323. doi: 10.1136/ip.2007.017954. [DOI] [PubMed] [Google Scholar]
- 53.Briffa TG, Sanfilippo FM, Hobbs MS et al. Under-ascertainment of Aboriginality in records of cardiovascular disease in hospital morbidity and mortality data in Western Australia: a record linkage study. BMC Med Res Methodol. 2010;10:111. doi: 10.1186/1471-2288-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Freemantle J, Ring I, Arambula Solomon TG et al. Indigenous mortality (revealed): the invisible illuminated. Am J Public Health. 2015;105(4):644–652. doi: 10.2105/AJPH.2014.301994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peiris D, Mohsin M, Jenkins A, Hughes C, Cass A. Robust data to close the gap: current vascular and maternal/newborn indicators as measures of progress in Aboriginal health in New South Wales. Aust N Z J Public Health. 2010;34(6):563–571. doi: 10.1111/j.1753-6405.2010.00629.x. [DOI] [PubMed] [Google Scholar]
- 56.Australian Institute of Health and Welfare. Improving the Quality of Indigenous Identification in Hospital Separations Data. Canberra, Australia: 2005. [Google Scholar]
- 57.Biddle N, Markham F. CAEPR Indigenous Population Project 2011 Census Papers. Canberra, Australia: Australian National University; 2013. [Google Scholar]
- 58. Australian Government. The Australian National Aboriginal and Torres Strait Islander Health Plan 2013–2023. Commonwealth of Australia, 2013.
- 59. National Public Health Partnership (NPHP). 2004. The National Injury Prevention and Safety Promotion Plan: 2004–2014. Canberra: NPHP.
- 60.Kendrick D, Marsh P. Inequalities in receipt of injury prevention in primary care. Health Educ J. 2000;59(2):150–156. [Google Scholar]
- 61.Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190–193. doi: 10.1136/jech-2012-201257. [DOI] [PubMed] [Google Scholar]
- 62.Hunter K, Keay L, Clapham K et al. Buckle up safely (Shoalhaven): a process and impact evaluation of a pragmatic, multifaceted preschool-based pilot program to increase correct use of age-appropriate child restraints. Traffic Inj Prev. 2014;15(5):483–490. doi: 10.1080/15389588.2013.833328. [DOI] [PubMed] [Google Scholar]
- 63.Senserrick T, Hinchcliff R, Ivers R, Boufous S, Martiniuk A, Clapham K. Aboriginal Injury Prevention Projects: A Rapid Review. Ultimo, Australia: Sax Institute for NSW Health and the George Institute; 2010. [Google Scholar]
- 64.Clapham K, Khavarpour F, Bolt R, Stevenson M, Su S. Researching the safety of indigenous children and youth: an urban perspective. In: McCoy BF, Stewart P, Poroch N, editors. Urban Health: Strengthening Our Voice, Culture and Partnership. Canberra, Australia: Australian Institute of Aboriginal and Torres Strait Islanders; 2012. pp. 47–57. [Google Scholar]
- 65.Ishikawa T, Oudie E, Desapriya E, Turcotte K, Pike I. A systematic review of community interventions to improve Aboriginal child passenger safety. Am J Public Health. 2014;104(suppl 3):e1–e8. doi: 10.2105/AJPH.2013.301683. [DOI] [PMC free article] [PubMed] [Google Scholar]