Abstract
Background
In this paper, we report findings regarding the prevalence of expressed distress and depressive conditions among women living in a rural region of Sichuan Province. As well, we know of no data among women in rural China that examine whether “depression,” as categorically defined in classifications such as the DSM, adequately captures the expressed distress and symptomatic complaints of women in rural China.
Methods
A multistage sampling method was employed to recruit the target population. The Center for Epidemiologic Studies Depression Scale (CES-D) was used to measure distress symptoms, and MINI International Neuropsychiatric Interview (MINI) was employed to determine the prevalence of diagnosable depression and other disorders.
Results
Among 1898 rural women, 12.4% (236) scored ≥16 on the CES-D, indicative of distress, and a subset of 7.7% (146) had scores ≥21, highly suggestive of a clinically significant disorder. We found that 49.8% women with ≥16 CES-D score were identified as showing features consistent with a current major depressive episode (MDE) vs. 1.9% in a sample of randomly selected women with <16 CES-D score. Among respondents, 30 of 84 (35.7%) scoring 16–20 and 83 of 143 (58.0%) scoring ≥21 reported symptoms consistent with MDE. 25.1% of women with a positive CES-D score did not describe symptoms consistent with any DSM-IV disorder.
Conclusions
We found a higher portion of women reporting significant distress than previously described. Among them, there was a clear gradient, such that 41.7% of women with moderate distress did not have a psychiatric diagnosis, and even among those with more severe symptoms, 15.4% did not manifest a DSM-specific psychiatric condition.
Introduction
In this paper we report findings regarding the prevalence of expressed distress and depressive conditions among women living is a rural region of Sichuan Province. Women in rural China continue to serve as primary care givers for their families and more often are “left behind” as their spouses seek employment in urban centers and industrial zones. Even as overall suicide rates apparently have been declining during recent years, those of younger and middle aged rural women continue to remain close to those of men [1].
Rural areas in China, especially those distant from major metropolitan centers, remain less modernized and less influenced by western medical concepts. The education level in rural China is lower and it is likely that rural residents are more likely to retain traditional notions of mental health and related interventions. Now that the PRC government has committed the country to modernizing health services across rural regions of China, as well as providing enhanced medical insurance coverage, it essential to better understand the burden of mental distress and clinically definable conditions.
Similar to Western nations [1–11], the reported rate of major depressive disorder in China among women is higher than that found among men (2.60% vs. 1.55%), and the rate of depression in rural regions (2.24%) is higher than that in urban areas [9]. However, we know of no data among women in rural China that examine whether “depression,” as categorically defined in classifications such as the DSM, adequately captures the expressed distress and symptomatic complaints of women in rural China. As well, many people and families are embarrassed by the presence of mental health concerns [12–15], and avoid expressing distress in a clinically meaningful fashion.
In this paper, part of a series arising from this research, we describe the prevalence of symptoms of distress using the Center for Epidemiologic Studies Depression Scale (CES-D) among women, ages 16 years and older, in a rural region of Sichuan Province. We also determine among those “cases,” the prevalence of diagnosable “clinical conditions,” including depressive disorders and other conditions by the MINI International Neuropsychiatric Interview (MINI).
Methods
For this study we focused on the rural region of Guangyuan City, which lies in the northern, mountainous area of Sichuan Province. In China, “cities” stretch beyond central urban areas and often encompass distinctly rural communities. Guangyuan City includes three districts, and four counties, with a population of 2.48 million– 820,000 (33.1%) urban and 1.66 million (66.9%) rural. The average annual net 2010 income for rural residents was ¥5,649 (approximately $911) and the average living expenses were ¥4,406 (approximately $711) [16].
Sampling
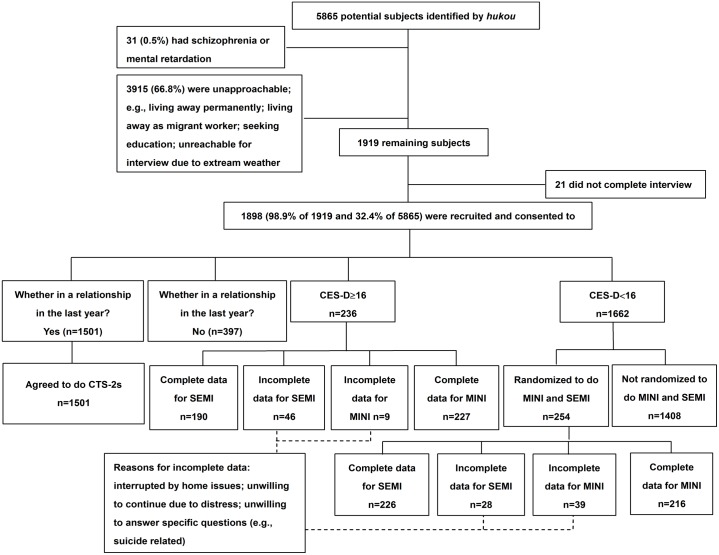
We sought to include a representative sample of women, ages 16 years and older, living in the rural Lizhou district of Guangyuan City. To ensure study participants represented a range of different socio-economic sectors, we used a multistage sampling method: We divided the nine towns in Lizhou District into three levels—low, middle, and high-income. From each income level, one town was randomly selected as our research site, and within each town, three to five villages were selected randomly. We used the method of random number table by SPSS to select the towns and villages. Thirteen villages were recruited in the study. We then used the Chinese household registration system (hukou) to identify eligible women living in the villages. In total, we identified 5865 possible participants. All of the women, ages 16 years and older, currently living in the 13 villages were eligible. We excluded—i.e., did not approach to obtain consent—women if they had a history of severe mental illness or cognitive impairment based on reports from family members or village doctors, or if after providing consent, they chose to discontinue interviews (thus, not completing the stusy protocol).
Recruitment
The study was conducted during the summer of 2012. Local government and health departments played an important role in the recruitment of participants, a necessary aspect of conducting studies in rural areas of China. With the help of the village leaders and village doctors, we first organized public information sessions about the research project. Interviewers were graduate and undergraduate medical students enrolled at Sichuan University who had been trained in survey and semi-structured interviewing techniques. The interviewers spent three to four days in each village. In the villages where there was more population density, we worked with the village leaders, doctors, and seniors to walk door-to-door and conduct our survey; they served the essential role of introducing interviewers to potential participants. In the villages where the population density was lower, local residents with motorcycles drove the interviewers to do survey door-to-door. In one town where the villages perched on a mountainside, we were not able to complete a full door-to-door survey due to heavy summer rains during the study period. All participants were given a token of appreciation for their time consisting of toiletry items (such as toothpaste and soap) worth ¥5 (about $0.80). Interviews lasted 20–70 minutes. When an eligible participant was unavailable or not home, we returned twice before defining them as unavailable.
The protocol including verbal the informed consent was reviewed and approved by the Medical Ethics Committee of Sichuan University (2011004). The University of Rochester Research Subjects Review Broad reviewed and approved analyses of de-identified data. In the study, we recruited women aged 16 years and older—the designated age for adult consent in China. The Medical Ethics Committee of Sichuan University approved the consent procedure for participants younger than 18 years. We asked all participants to provide verbal informed consent, as many of the rural women could not write. The interview process also required affirmative assent to answer our inquires; as seen in Fig 1, 21 participants discontinued the basic interview, which constituted a removal of affirmative consent and the protocol was discontinued with none of their data included in analyses. The study was deemed to pose a low risk for participants, and was conducted in accordance with the Declaration of Helsinki.
Fig 1. Recruitment of subjects.
Interviewer Training and Quality Control
A total of 24 interviewers were selected from undergraduate and postgraduate medical students from West China Medical Center, Sichuan University. All interviewers completed a structured training program. The training program involved: one day training to introduce the topic of affective disorders; two days training on administrating MINI; and two days training on administrating computer based interviews, interview skills, response skills, and research ethics. (Interviewers also participated in training sessions related to other interview tools, which will be discussed in subsequent related publications.) We first demonstrated standardized interviews with two experienced graduate students. Interviewers next paired to conduct mock interviews under supervision. Each interviewer also conducted a practice interview in front of the whole team.
During the field study, the 24 interviewers were divided into three groups. Each group was led and supervised by an experienced field researcher. The interviewers checked the participant responses immediately after the interviews were conducted. If any items were missing or inconsistent information was found, the interviewer would reassess the participant regarding these items. At the end of each interview day, the three group supervisors checked all interview protocols. In addition, the team leader conducted quality control meetings for the entire team every evening to discuss any difficulties or challenges encountered, and to develop consensus strategies to address these issues.
Protocol and Measures
All participants completed socio-demographic questions including age, marital status, living situation, education, occupation, ethnic background, religion, and household income. In addition, all participants completed questions regarding self-rated health, diagnosed chronic diseases, and health care utilization, based on items from the National Health Services Survey [17]. For this aspect of the study, all participants completed the CES-D [18]. The CES-D, a self-report inventory, contains 20 items that are scored by respondents to indicate the frequency of symptoms during the previous week, using a scale of 0 –less than a day, 1–1–2 days, 2–2–3 days, and 3–5–7 days. It has a very wide spectrum of noted symptoms, which makes it not simply a depression scale, but also a distress scale. A score of 16 or more is indicating the likely presence of distress. (Of note, past epidemiological research in China has demonstrated the validity and reliability of the CES-D, and similar to other countries, found that a score of 16 was applicable[19–22]).
Those with a CES-D score of ≥16 were further assessed for categorically defined mental disorders using the Mini-International Neuropsychiatric Interview (MINI) and interviewed for their perceptions regarding distress and depression [23, 24]. A sample of lower scoring participants also completed the MINI. The MINI is a short, structured diagnostic interview to explore 17 disorders according to Diagnostic and Statistical Manual (DSM)-III-R diagnostic criteria, designed to allow administration by non-specialized interviewers. The MINI contains 120 questions and screens 17 axis I DSM-III-R disorders for 24 current and lifetime diagnoses. In our results, we reported current diagnoses. Beside, in our study, given that alcohol and drug abuses, anorexia nervosa, and bulimia nervosa in rural women are rare, we did not include them. As well, since women with psychosis were not eligible for the study, psychotic disorders were not investigated.
Analysis
We applied Chi-square test and t-test to analyze differences of demographic factors between people with CES-D score ≥16 and < 16. Furthermore, we employed bivariate logistic regression to define demographic factors associated with depressive symptoms.
We categorized participants into four groups based on age: 16–24 years old, 25–44 years old, 45–64 years old, and ≥ 65 years old. We divided participants into five education groups: lack of formal schooling (no school), primary level of education (≤6 years), junior high school level of education (7–9 years), high school level of education and above (≥10 years). Occupational status was categorized into five groups: agriculture work, non-agriculture work, homemakers, students, and unemployed. In addition, we categorized subjects into three groups based on their annual household income: ≤ 10,000, 10,000–20,000, and >20,000. Living status was categorized into three groups: living alone, living with core family and living with extended family (including living with relatives and friends). We dichotomized marital status into two groups: married and not married, dichotomized ethnic background into Han ethnic and others, and dichotomized religious into two groups: without any religious and with any kind of religious. In our study, statistical significance was established at p < 0.05.
Results
We recruited with verbal consent 1919 women in the study; 1898 of them completed the interview. The CES-D scores ranged from 0 to 57 (average = 7.2±8.4; median = 5). Among the participants, 1662 (87.6% of 1898) respondents scored below 16 (<16), while 236 (12.4%) scored 16 or above (≥16). Of the total sample, 146 (7.7%) had scores ≥ 21, highly suggestive of a clinically significant depressive condition; [18] that is, one that is associated with functional deficits as well as reported symptoms. Table 1 shows the distribution of participants by age, marital status, religion, living situation, education attainment, occupation, and household income. The results of the bivariate logistic regression (Table 2) indicated that women who were poor and unemployed were more likely to have depressive symptoms. Religious impact on depressive symptoms was marginal.
Table 1. Sociodemographics Characteristics of Women.
| Total | CES-D ≥ 16 | CES-D < 16 | Chi-square | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | T-test | |
| n = 1898 | n = 236 | n = 1662 | ||
| Total | - | |||
| Participant Characteristics | ||||
| Age | 0.010 | |||
| 16–24 | 143(7.5) | 11(4.7) | 132(7.9) | |
| 25–44 | 605(31.9) | 61(25.8) | 544(32.7) | |
| 45–64 | 843(44.4) | 127(53.8) | 716(43.1) | |
| 65- | 307(16.2) | 37(15.7) | 270(16.2) | |
| Marital Status | 0.176 | |||
| Single | 342(18.0) | 50(21.2) | 292(17.6) | |
| Married | 1556(82.0) | 186(78.8) | 1370(82.4) | |
| Ethnic Background | 0.119 | |||
| Han | 1893(99.7) | 234(99.2) | 1659(99.8) | |
| Others | 5(0.3) | 2(0.8) | 3(0.2) | |
| Religion | 0.020 | |||
| Yes | 88(4.6) | 18(7.6) | 70(4.2) | |
| No | 1810(95.4) | 218(92.4) | 1592(95.8) | |
| Living Situation | 0.483 | |||
| Alone | 75(4.0) | 10(4.3) | 65(3.9) | |
| With Core Family | 680(35.9) | 76(32.3) | 604(36.4) | |
| With extended family (including living with relatives and friends) | 1141(60.1) | 149(63.4) | 992(59.7) | |
| Education Attainment | 0.029 | |||
| No School | 724(38.1) | 102(43.2) | 622(37.4) | |
| Less than 6 Years | 706(37.2) | 91(38.6) | 615(37.0) | |
| 7 to 9 Years | 324(17.1) | 35(14.8) | 289(17.4) | |
| 10 and above | 144(7.6) | 8(3.4) | 136(8.2) | |
| Occupation | 0.001 | |||
| Agricultural work | 1117(58.9) | 146(61.9) | 971(58.5) | |
| Non-agricultural work | 234(12.3) | 20(8.5) | 214(12.9) | |
| Homemakers | 326(17.2) | 34(14.4) | 292(17.6) | |
| Students | 43(2.3) | 1(0.4) | 42(2.5) | |
| Unemployed | 177(9.3) | 35(14.8) | 142(8.5) | |
| Household Income | 0.010 | |||
| ≤ 10000 | 685(36.1) | 103(43.6) | 582(35.0) | |
| 10000–20000 | 483(25.4) | 62(26.3) | 421(25.3) | |
| > 20000 | 730(38.5) | 71(30.1) | 659(39.7) |
Table 2. Bivariate logistic regression—demographic factors and depressive symptoms.
| Participants’s Characteristics | OR(95% CI) | P |
|---|---|---|
| Income | 0.82(0.69–0.96) | 0.014 |
| Education | 0.91(0.76–1.08) | 0.27 |
| Occupation | ||
| Agricultural work | — | — |
| Non-agricultural work | 0.74(0.45–1.24) | 0.26 |
| Homemakers | 0.84(0.56–1.25) | 0.38 |
| Students | 0.19(0.03–1.44) | 0.11 |
| Unemployed | 1.66(1.10–2.50) | 0.02 |
| Religious | ||
| No religious | — | — |
| Any religious | 1.74(1.00–3.01) | 0.05 |
Among the women scoring <16 (n = 1662), we randomly selected and consented 254 for further study. Compared to the larger asymptomatic group, there were no significant differences in educational attainment, marital status, and household income, although we did find modest differences in age and occupation distribution. Asymptomatic women who were randomized to do MINI had a lower average age (44.4 vs 48.9 years for “positive” responders) and were more likely to be involved in agricultural work (66.2% vs 57.3%).
Two hundred twenty-seven (227) of the 236 participants scoring ≥16 on the CES-D completed the MINI to determine the prevalence of diagnosable depression and other conditions; as well, 216 of 254 of our random sample of participants with a CES-D <16 completed the protocol (Fig 1).
Table 3 shows that 113 of the 227 (49.8%) women with ≥16 CES-D score were identified as showing features consistent with a current major depressive episode (MDE) vs. four of the 216 (1.9%) in the comparison group. Of those individuals with scores of 16–20, 30 of 84 (35.7%) reported symptoms consistent with MDE; of those with CES-D scores ≥21, 83 of 143 (58.0%) also had consistent features. Of those scoring ≥16, 24 of 227 (10.6%) presented with symptoms of dysthymia in contrast to one (0.5%) among the non-distressed women. For those with scores of 16–20, 5 of 84 (6.0%) apparently suffered dysthymia, while for those ≥21, 19 of 143 (13.3%) had a similar presentation. Thus, among women with a positive CES-D score, 57 of 227 (25.1%) did not describe conditions that were diagnosed in a fashion consistent with a DSM-IV disorder, 35 of 84 (41.7%) for those scoring 16–20 and 22 of 143 (15.4%) of those ≥21.
Table 3. MINI Diagnosed Conditions among Participants with Distress.
| CES-D < 16 N (%) n = 216 | CES-D ≥ 16 N (%) n = 227 | ||||
|---|---|---|---|---|---|
| CES-D = 16–20 | CES-D ≥ 21 | CES-D ≥ 16 | |||
| N (%) | N (%) | N (%) | |||
| n = 84 | n = 143 | n = 227 | |||
| Primary Diagnosis | Major Depressive Episode (MDE) | 4 (1.9) | 30(35.7) | 83(58.0) | 113(49.8) |
| Dysthymia | 1(0.5) | 5(6.0) | 19(13.3) | 24(10.6) | |
| Bipolar Disordera | 2(0.9) | 0(0.0) | 4(2.8) | 4(1.8) | |
| Manic/Hypomanic Episode | 3(1.4) | 2(2.4) | 2(1.4) | 4(1.8) | |
| Anxiety Disordersb | 11(5.1) | 12(14.3) | 13(9.1) | 25(11.0) | |
| No Diagnosis | 195(88.9) | 35(41.7) | 22(15.4) | 57(25.1) | |
a. MINI does not have a diagnosis of bipolar disorder. In our sample, if respondent had major depressive episode and manic/hypomanic episode, she was classified as bipolar disorder in our study.
b. Anxiety disorders include panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder, posttraumatic stress, and generalized anxiety disorder. As long as respondents had one of these anxiety disorders, they were counted as having anxiety disorders.
Discussion
We found a higher prevalence than previously reported of personal distress and major depression in these rural communities [9, 25, 26], which are bearing the burden of heavy rural-to-urban migration. Among the unapproachable potential subjects listed in the village hukou, the vast majority were migrant workers who lived at distant locations. Compared to those remaining in the villages, they were younger, and likely healthier and better educated. Our results suggest that, among the women who did remain in rural regions during this period of rapid urbanization in China, there are many who are especially vulnerable to significant clinical conditions. Moreover, we would anticipate that as urbanization accelerates further, there will be an increasing tendency to draw younger, more mobile, economically prepared women to the cities, further concentrating more vulnerable, less educated, older and less employable individuals, posing future challenges. We are mindful, for example, that problems such as suicide among elders have not declined in rural regions in the same fashion as the decline among younger individuals [1], and such rates may tend to increase during years ahead as elders’ children and extended familes continue to migrate away.
More than three decades ago, Kleinman argued that “depression” in China was manifest in a distinctive, culturally congruent fashion [2, 10], and that the Western notions of psychopathology were inadequate for capturing persons’ presentations. Anthropological and psychiatric research indicated in years past that Chinese people often expressed distress arising from interpersonal or social situations by way of complaints of anxiousness, headaches, insomnia, chest discomfort, and dizziness, rather than using “depression” to characterize their condition. This was captured by the term neurasthenia; except for post-influenza neurasthenia, this concept largely was dropped from the Western diagnostic nosology with the promulgation of DSM-III in 1980[8, 10, 27, 28]. By 2000, the diagnostic use of neurasthenia also had virtually disappeared among Chinese psychiatrists; its replacement, depression, has become the new term for medical professionals, and increasingly, for patients themselves [29]. Studies in Hong Kong [4] and in modern urban centers in China [5, 7] document that the Western construct of depressive disorders now is deeply anchored in those settings and has apparent clinical utility. Moreover, epidemiological studies now undertaken in China use the DSM, Western-based nosology as their frame of reference[9].
Our study found that 137 (60.4%) women with a ≥16 CES-D score reported symptoms indicative of a MINI diagnosed mood disorders—either MDE or dysthymic disorder, while 33 (14.6%) had other primary diagnoses. However, 57 (25.1%) did not report symptoms indicative of any specific diagnosis. Even among women with a CES-D score ≥21, 22 (15.4%) did not have any diagnosis, reinforcing the finding that highly symptomatic persons may not report clinical features consistent with a DSM diagnosis. In the comparison group of women with a CES-D score <16, only five of 216 (2.4%) received a MINI diagnosis of MDE or dysthymic disorder. Overall, 195 (88.9%) had no diagnosis.
These results suggested that there were many moderately and severely distressed women who did not present their complaints in a fashion consistent with DSM categorical conditions. Clearly this dissonance diminished with increasing severity; yet even at higher CES-D levels, we found many who were not coded diagnostically. This is potentially relevant when considering future service needs, and also when planning how best to train village and town doctors to recognize persons in distress.
The CES-D has been used across nations and populations with reported variation in its prediction of diagnosed clinical conditions. A study of evaluating reliability and validity of CES-D in Greek populaion showed that sensitivity and specificity of CES-D were 92.5% and 85.0%, respectively, if 21 was used as the cutoff score [30]. Another involving older Chinese showed that 22 was the optimum threshold in its sample, with sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were 0.75, 0.51, 0.55 and 0.72 [31]. Various studies from the 1990s, using a a CES-D score of 16, found widely varying sensitivity (from 63.3% to 100.0%) and specificity (from 53.0% to 93.9%) [32, 33]. These results are consistent with our finding that there are many significantly distressed individuals whose conditions do not neatly fit into categorical diagnoses.
Our findings point to the presence of meaningful and important levels of personal distress that are not captured in a categorical fashion. At the same time, a majority of the participants’ presentations were consistent with DSM-based patterns of psychopathology. Put another way, we partly confirmed Kleinman’s past observations using other methods—that is, to a modest degree—even as the bulk of our findings at this time point to the potential utility of categorical psychiatric descriptions in these rural villages. Whether the differences in the prevalence of distress versus depression specifically reflect the factors posited by Kleinman remains to be determined.
We caution regarding several potential limitations. The study was conducted in one rural area of Sichuan Province. In light of China’s extraordinary diversity, we must be careful generalizing our results to other rural regions. In addition, we are very aware that because of internal migration in China, we could not approach many women who were registered in study villages, potentially compromising the representativeness of our sample. And women who migrate to city may have different characteristics from those who are left-behind. However, using hukou as a method to identify eligible women living in rural villages such as these remains the best choice currently. Finally, we did not use psychiatrists to administer the MINI, thus requiring caution when considering the accuracy of our psychiatric diagnoses.
Conclusion
Women with clinically significant depressive symptoms were older, less educated, involved in farming or unemployed, and economically disadvantaged. Overall, 25% of women at or above the CES-D threshold had no diagnosis. We saw in our results a clear gradient, such that 41.7% of women with moderate distress did not have a psychiatric diagnosis, and even among those with more severe symptoms, 15.4% did not manifest a DSM-specific psychiatric condition. Distress and depression are relatively common among women residing in these rural communities where many people have left for urban opportunities. These conditions pose significant personal and community challenges, and point to pressing needs in China for developing basic, community-focused mental health services.
Supporting Information
(SAV)
Acknowledgments
We most appreciate the support of Yinghui Zhang, Dean, Guangyuan Mental Health Center, and the the important input of Ma Mei from Guangyuan Mental Health Center, and Chen Shulin from Zhejiang University.
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
Funded by National Institutes of Health, Grant D43 TW009101 and TW009101-01S1 (E.D. Caine, PI). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Wang CW, Chan CL, Yip PS. Suicide rates in China from 2002 to 2011: an update. Soc Psychiatry Psychiatr Epidemiol. 2014. June;49(6):929–41. 10.1007/s00127-013-0789-5 [DOI] [PubMed] [Google Scholar]
- 2.Kleinman AM. Depression, somatization and the “new cross-cultural psychiatry”. Social Science & Medicine (1967). 1977;11(1):3–9. [DOI] [PubMed] [Google Scholar]
- 3.Hu T-w, He Y, Zhang M, Chen N. Economic costs of depression in China. Social psychiatry and psychiatric epidemiology. 2007;42(2):110–6. [DOI] [PubMed] [Google Scholar]
- 4.Chiu H, Yip P, Chi I, Chan S, Tsoh J, Kwan C, et al. Elderly suicide in Hong Kong–a case-controlled psychological autopsy study. Acta Psychiatrica Scandinavica. 2004;109(4):299–305. [DOI] [PubMed] [Google Scholar]
- 5.Lee S, Tsang A, Huang Y, He Y, Liu Z, Zhang M, et al. The epidemiology of depression in metropolitan China. Psychological medicine. 2009;39(5):735 10.1017/S0033291708004091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murray CJL, Lopez A.C. (eds). The Global Burden of Diseases: A Comprehensive Assessment of Mortality and Disability from Disease, 2000. Harvard University Press, Cambridge, MA: 1997. [Google Scholar]
- 7.Lee S, Fung S, Tsang A, Liu Z, Huang Y-Q, He Y, et al. Lifetime prevalence of suicide ideation, plan, and attempt in metropolitan China. Acta Psychiatrica Scandinavica. 2007;116(6):429–37. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Guo W-j, Tsang A, He Y-l, Huang Y-q, Liu Z-r, et al. Perceived barriers to mental health treatment in metropolitan China. Psychiatric Services. 2010;61(12):1260–2. 10.1176/appi.ps.61.12.1260 [DOI] [PubMed] [Google Scholar]
- 9.Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, Pang S, et al. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001–05: an epidemiological survey. The Lancet. 2009;373(9680):2041–53. [DOI] [PubMed] [Google Scholar]
- 10.Kleinman A. Rethinking Psychiatry: From Cultural Category to Personal Experience. New York: Free Press; 1988. [Google Scholar]
- 11.Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2013;380(9859):2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fabrega H Jr. Psychiatric stigma in non-Western societies. Comprehensive psychiatry. 1991;32(6):534–51. [DOI] [PubMed] [Google Scholar]
- 13.Corrigan PW, Shapiro JR. Measuring the impact of programs that challenge the public stigma of mental illness. Clinical Psychology Review. 2010;30(8):907–22. 10.1016/j.cpr.2010.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jones AR, Cook TM, Wang J. Rural–urban differences in stigma against depression and agreement with health professionals about treatment. Journal of affective disorders. 2011;134(1):145–50. [DOI] [PubMed] [Google Scholar]
- 15.Lv Y, Wolf A, Wang X. Experienced stigma and self-stigma in Chinese patients with schizophrenia. General hospital psychiatry. 2013;35(1):83–8. 10.1016/j.genhosppsych.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 16.Intranet GS. Statistical Communique on the 2012 Guangyuan economic and social development. 2012.
- 17.Center TMoHSI. An Analysis Report of National Health Services Survey in China, 2008. Beijing: Peking Union Medical College Press; 2009. [Google Scholar]
- 18.Sheehan TJ, Fifield J, Reisine S, Tennen H. The measurement structure of the Center for Epidemiologic Studies Depression scale. Journal of personality assessment. 1995;64(3):507–21. [DOI] [PubMed] [Google Scholar]
- 19.Zhang J, Sun W, Kong Y, Wang C. Reliability and validity of the Center for Epidemiological Studies Depression Scale in 2 special adult samples from rural China. Comprehensive psychiatry. 2012. November;53(8):1243–51. 10.1016/j.comppsych.2012.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang L, Jia CX, Qin P. Reliability and validity of the Center for Epidemiologic Studies Depression Scale (CES-D) among suicide attempters and comparison residents in rural China. BMC psychiatry. 2015;15:76 10.1186/s12888-015-0458-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ZHANG J, WU Z, FANG G, LI J, HAN B, CHEN Z. Development of the Chinese age norms of CES-D in urban area. Chinese Mental Health Journal. 2010;24:139–43. [Google Scholar]
- 22.Chin WY, Choi EP, Chan KT, Wong CK. The Psychometric Properties of the Center for Epidemiologic Studies Depression Scale in Chinese Primary Care Patients: Factor Structure, Construct Validity, Reliability, Sensitivity and Responsiveness. PloS one. 2015;10(8):e0135131 10.1371/journal.pone.0135131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Si T, Shu L, Dang W, Su Y, Chen J, Dong W, et al. Evaluation of the reliability and validity of Chinese version of the Mini-International Neuropsychiatric Interview in patients with mental disorders. Chinese Mental Health Journal. 2009;23(7):493–7, 503. [Google Scholar]
- 24.Sheehan D, Lecrubier Y, Harnett Sheehan K, Janavs J, Weiller E, Keskiner A, et al. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12(5):232–41. [Google Scholar]
- 25.Gu L, Xie J, Long J, Chen Q, Chen Q, Pan R, et al. Epidemiology of Major Depressive Disorder in Mainland China: A Systematic Review. PloS one. 2013;8(6):e65356 10.1371/journal.pone.0065356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu J, Ruan Y, Huang Y, Yao J, Dang W, Gao C. Major depression in Kunming: prevalence, correlates and co-morbidity in a south-western city of China. Journal of affective disorders. 2008;111(2):221–6. [DOI] [PubMed] [Google Scholar]
- 27.Jackson SW. Melancholia and depression: From hippocratic times to modern times: Yale University Press; 1986. [Google Scholar]
- 28.Lee DT, Kleinman J, Kleinman A. Rethinking depression: an ethnographic study of the experiences of depression among Chinese. Harvard Review of Psychiatry. 2007;15(1):1–8. [DOI] [PubMed] [Google Scholar]
- 29.Kleinman A. Deep China: The moral life of the person: What anthropology and psychiatry tell us about China today: Univ of California Press; 2011. [Google Scholar]
- 30.Fountoulakis K, Iacovides A, Kleanthous S, Samolis S, Kaprinis S, Sitzoglou K, et al. Reliability, validity and psychometric properties of the Greek translation of the Center for Epidemiological Studies-Depression (CES-D) Scale. BMC psychiatry. 2001;1(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng ST, Chan A. The center for epidemiologic studies depression scale in older Chinese: Thresholds for long and short forms. International journal of geriatric psychiatry. 2005;20(5):465–70. [DOI] [PubMed] [Google Scholar]
- 32.O'Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening for depression in adult patients in primary care settings: a systematic evidence review. Annals of Internal Medicine. 2009;151(11):793–803. 10.7326/0003-4819-151-11-200912010-00007 [DOI] [PubMed] [Google Scholar]
- 33.Pignone MP, Gaynes BN, Rushton JL, Burchell CM, Orleans CT, Mulrow CD, et al. Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine. 2002;136(10):765–76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.