Abstract
Objectives:
To review the radiation doses received by women attending the UK breast-screening programme between 2010 and 2012. To compare doses with previous years and to quantify the impact on dose of changing from analogue to digital imaging and to analyse doses by type of imaging system.
Methods:
Measurements of doses to samples of about 50–100 women attending for screening were collected across the whole of the UK breast-screening programme.
Results:
Data were collected for 87,122 exposures, using 449 X-ray sets, for 25,408 women. The average mean glandular dose (MGD) was 1.79 mGy for mediolateral oblique images and 1.58 mGy for craniocaudal images. The average MGD per two-view examination was 4.01 mGy for film-screen imaging and 3.03 mGy for direct digital radiography (DR) and 4.69 mGy for computed radiography.
Conclusion:
The MGD to women attending breast screening has been reduced on average by about 25% where DR systems have replaced film-screen systems. The dose reduction was greatest for breasts with the largest compressed thickness. There are large variations in dose between the different models of DR system provided by different manufacturers. There should be further work to ensure that all DR systems are operated at the optimal dose level to ensure the best cancer detection while balancing the detriment caused by using radiation.
Advances in knowledge:
Changes in the radiation dose in breast screening over time have been determined. Specifically, the impact on radiation dose of introducing different types of DR and computed radiography system into breast screening has been quantified.
INTRODUCTION
The National Health Service Breast Screening Programme (NHSBSP) in the UK invites all women aged 50–70 years to attend for X-ray mammography every 3 years. Older women can be screened on request, and some younger (aged 47–49 years) and older (aged 70–73 years) women are also invited as part of an age-extension trial. In 2011–12, the programme in England screened 1.94 million women.1 As for all medical X-ray procedures, the principles of radiation protection require that the radiation exposure be justified and optimized. In order to ensure the justification and optimization, accurate dose information is required. The two main methods used in the UK for the assessment of patient dose in mammography are described in Report 89 of the Institute for Physics and Engineering in Medicine.2 In the “standard breast method”, the mean glandular dose (MGD) for the standard breast model is estimated from measurements with a range of thicknesses of poly (methyl methacrylate) (PMMA) i.e. Perspex® or Lucite® (Lucite International, Darwen, UK). The MGD for the standard breast allows comparison of the doses for different mammography systems that eliminates variations due to the characteristics of individual breasts. A quality control (QC) objective of the NHSBSP is that “the MGD to the 53 mm-thick standard breast simulated with a 45-mm thickness of PMMA is ≤2.5 mGy”.2 The doses to real breasts in screening also depend on other factors, including the breast composition, compressed breast thickness, beam quality and number of exposures. The radiation doses for individual women can be estimated by using the post-exposure tube current–exposure time (mAs) to determine incident air kerma and using conversion factors proposed by Dance et al and tabulated in IPEM Report 89 and European Guidelines.2–4 The method assumes an average variation in breast composition with compressed thickness that was determined experimentally. One factor adjusts for the use of different target/filter combinations, and tables of factors for new target/filter combinations have been published by Dance et al.5,6
Measurements of doses to samples of 50–100 women attending for screening on a specific mammography system are measured routinely at screening centres, and dose data collected from screening centres have been published previously.7–10 This article reviews data collected across the NHSBSP between 2010 and 2012 using a similar methodology. The aims of this study were
to compare doses with previous years
to assess the impact of changing from film-screen to digital mammography
to investigate the effect of various technical features (e.g. model of X-ray set)
to investigate the effect of breast thickness
to compare doses with the national diagnostic reference level (NDRL)
to compare the dose with the standard breast with doses to real breasts.
METHODS AND MATERIALS
For each unit that participated in the study, the following data were collected:
date of survey
models of X-ray set (and processor, films, screens and computed radiography (CR) equipment where relevant)
MGD to standard breast
age of women screened (where available)
compressed breast thickness and projection for each image in sample
exposure factors (mAs, kV, target and filter) for each image
output data for each X-ray set
mode of automatic beam quality selection (if more than one).
The survey was restricted to the basic screening situation, and so, more complicated procedures such as magnification mammography were excluded.
All the mammography systems (digital or analogue) display the exposure factors and compressed breast thickness at the time of exposure. The compressed thickness is determined by the position of the compression paddle and is calibrated by engineers at service visits and tested by local physics services on routine QC visits. The radiographers write the data on a special form for the dose survey and this is supplied to their local medical physics services. For some digital systems, exposure and compressed breast thickness data were obtained from the images' digital imaging and communications in medicine (DICOM) headers. These data were passed to the local medical physics service where they were entered into a dose calculation database supplied by the NHSBSP.11 Once further data including tube output were added, the MGD per mammographic image was calculated by the software. All the data in these local copies of the database were combined to create a single central database. Each exposure was coded to identify the laterality and view, being either a mediolateral oblique projection (OB) or craniocaudal (CC) projection. Images were also identified as either “main” images or “extra” images. Extra images occur if a breast could not be completely imaged in one exposure. Unless otherwise indicated, the first image was assumed to be the main image. Screening generally involves OB and CC images of both breasts, but occasionally, dose data for only one view (1V) were supplied. Therefore, examinations were identified as either 1V or two view (2V).
The total dose for each screening procedure was determined by adding the doses for all images and averaging over both breasts. This includes the doses for the main films in a 2V examination, plus the doses for any additional images required to image large breasts.
Where mean values for MGD or breast thickness have been calculated, they are shown in the tables and figures with 95% confidence limits. As has been previously noted, breast thickness has a normal distribution while MGD is typically lognormal.9 This work also found that the confidence limits for means of MGD were effectively the same whether a normal or lognormal distribution was assumed.9 Therefore, here 95% confidence limits have been estimated using ±2 standard errors of the mean.
Diagnostic reference levels (DRLs) were introduced for radiodiagnostic examinations in the Ionising Radiation (Medical Exposure) Regulations 2000. DRLs are “dose levels for typical medical X-ray examinations for groups of standard-sized patients or standard phantoms and for broadly defined types of equipment”. The regulations require that employers establish DRLs and ensure that “procedures are in place for using them on the understanding that they are not expected to be exceeded for standard procedures when good and normal practice is being followed”. The current NDRL for mammography uses a dose audit measure which is the average MGD for OB mammograms for breasts with a compressed thickness of 55 ± 5 mm.12 A minimum of 10 women should be included in the dose sample. The NDRL for this dose audit measure is 3.5 mGy. In this study, the average MGD for all OB mammograms (main images only) with a compressed thickness of 55 ± 5 mm was calculated for each dose survey. For a few surveys, the number of OB mammograms in this thickness range was <20 (i.e. equivalent to <10 women), and these were excluded from this analysis.
RESULTS
Data included
29 medical physics departments contributed data from 449 dose surveys covering 419 X-ray sets used in 99 centres in England, Scotland, Wales and Northern Ireland. The data were collected over the period from January 2010 to September 2012 and included doses for 25,408 women. While 93% of surveys were for a sample of about 50–100 women per X-ray set, the overall range was from 20 to 574 women.
X-ray technique and systems used
All the X-ray sets were used in a mode that selected the beam quality automatically. The tube voltage selected ranged from 23 to 44 kV. The proportions of images taken with different target/filter combinations are shown for film-screen and digital mammography systems in Table 1 and compared with those in 1997–98 and 2001–02.7–9 All units [except Sectra (Stockholm, Sweden)/Philips MicroDose systems (Philips, Stockholm, Sweden)] operated with an antiscatter grid, which is standard practice within the NHSBSP. At the time of the dose survey, the Sectra systems were sold and maintained by Sectra, but these have since been taken over by Philips and are referred to here as Philips systems. The standard screening protocol is to obtain an OB and CC view of each breast. Thus, one would expect just two OB images and two CC images in a standard screening examination. However, some female breasts could not be fitted onto a single image and additional images were taken. Table 2 shows the number of images acquired for each view for the different types of system in a 2V examination.
Table 1.
Proportion of images taken with different target/filter combinations
| Target/filter combination used | Film 1997–98 | Film 2001–02 | Film 2010–12 | DR 2010–12 | CR 2010–12 |
|---|---|---|---|---|---|
| Mo/Mo | 96.0% | 58.5% | 55.4% | 1.5% | 33.6% |
| Mo/Rh | 3.0% | 40.0% | 44.1% | 3.9% | 66.4% |
| Rh/Rh | 0.4% | 1.2% | 0.5% | 25.5% | – |
| W/Rh | 0.0% | 0.2% | 0.0% | 52.1% | – |
| W/Ag | – | – | – | 11.1% | – |
| W/Al | – | – | – | 5.9% | – |
Ag, silver; Al, aluminium; CR, computed radiography; DR, digital radiography; Mo, molybdenum; Rh, rhodium, W, tungsten.
Table 2.
Number of images per view in two-view examinations
| Images per view | DR systems |
Film-screen systems |
CR systems |
|||
|---|---|---|---|---|---|---|
| OB | CC | OB | CC | OB | CC | |
| 1 | 369 (2.4%) | 360 (2.3%) | 173 (1.9%) | 155 (1.7%) | 41 (10.4%) | 39 (9.8%) |
| 2 | 14,728 (95.6%) | 14,915 (96.8%) | 8823 (94.7%) | 9088 (97.5%) | 355 (89.6%) | 357 (90.2%) |
| 3 | 243 (1.6%) | 94 (0.6%) | 148 (1.6%) | 49 (0.5%) | – | – |
| 4 | 58 (0.4%) | 31 (0.2%) | 156 (1.7%) | 25 (0.3%) | – | – |
| 5 | 2 (0.0%) | – | 8 (0.1%) | 1 (0.0%) | – | – |
| 6 | 3 (0.0%) | 3 (0.0%) | 11 (0.1%) | 2 (0.0%) | – | – |
| 7 | – | – | – | – | – | – |
| 8 | – | – | 1 (0.0%) | – | – | – |
CC, craniocaudal; CR, computed radiography; DR, digital radiography; OB, oblique projection.
Average doses
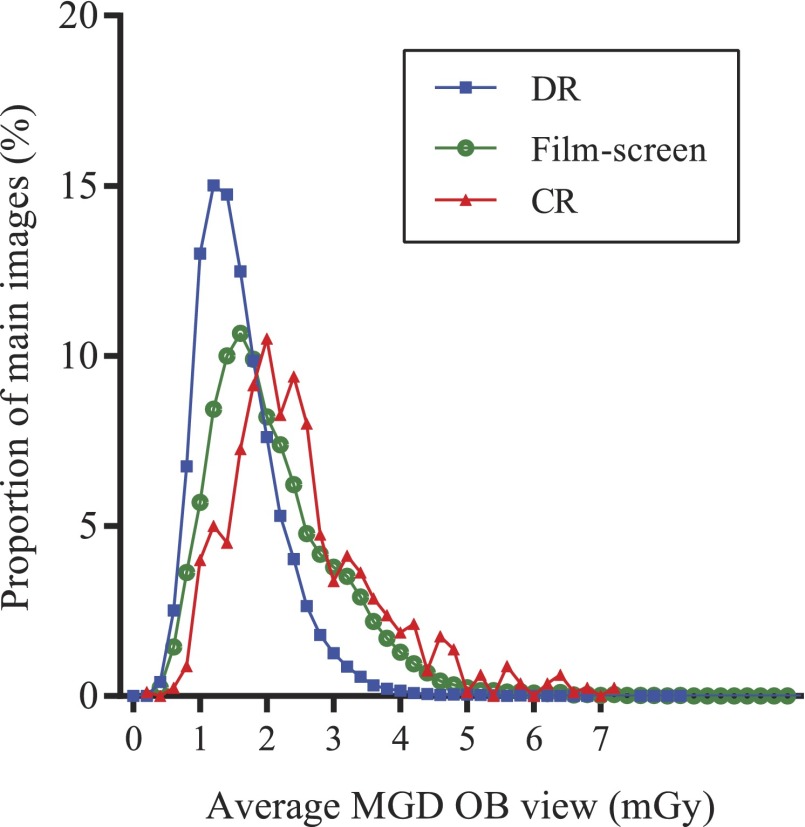
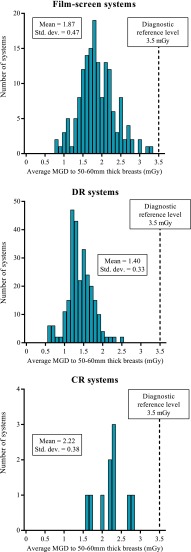
The average breast doses and compressed breast thicknesses recorded for main images are compared with those recorded in 1997–98 and 2001–02 in Tables 3 and 4.7–9 The average MGD for OB analogue films has decreased only slightly from 2.36 to 2.13 mGy from 1997–98 to 2010–12, and the MGD for analogue CC films is little changed. However, the dose for direct digital radiography (DR) systems was about 25% lower than for analogue films at 1.60 mGy for OB and 1.43 mGy for CC projections. The mean compressed breast thickness has increased slightly over time and was higher for DR and CR systems than for film-screen systems. The average compressed breast thickness for film-screen systems was similar to that found in the previous surveys. The histograms of doses for OB images for the three modalities are compared in Figure 1. The median and 5th and 95th percentile values are shown in Table 5. The average doses for 2V examinations are compared with the previous data in Table 6. The average MGDs for different types of system are shown for OB views in Table 7 and for CC views in Table 8.
Table 3.
Mean glandular dose (MGD) by projection compared with previous data
| Projection | Mean MGD per projection (mGy) (±2SEM) |
||||
|---|---|---|---|---|---|
| Film 1997–98 | Film 2001–02 | Film 2010–12 | DR 2010–12 | CR 2010–12 | |
| Oblique | 2.36 ± 0.03 | 2.23 ± 0.01 | 2.11 ± 0.01 | 1.58 ± 0.04 | 2.52 ± 0.08 |
| CC | 1.86 ± 0.02 | 1.96 ± 0.01 | 1.83 ± 0.01 | 1.42 ± 0.01 | 2.23 ± 0.07 |
CC, craniocaudal; CR, computed radiography; DR, digital radiography; SEM, standard error in the mean.
Table 4.
Average compressed breast thickness by projection compared with previous data
| Projection | Average compressed breast thickness (mm) (±SEM) |
||||
|---|---|---|---|---|---|
| Film 1997–98 | Film 2001–02 | Film 2010–12 | DR 2010–12 | CR 2010–12 | |
| Oblique | 54.3 ± 0.2 | 56.8 ± 0.2 | 56.2 ± 0.2 | 59.3 ± 0.2 | 58.2 ± 0.9 |
| CC | 51.5 ± 0.3 | 54.1 ± 0.2 | 53.5 ± 0.2 | 56.3 ± 0.2 | 56.1 ± 0.8 |
CC, craniocaudal; CR, computed radiography; DR, digital radiography; SEM, standard error in the mean.
Figure 1.
Distribution of mean glandular dose for oblique views. The axis represents the midpoint of 0.2 mGy bands.
Table 5.
Median mean glandular dose (MGD) by projection and system type
| Projection | Median MGD per projection (mGy) (5th–95th percentiles) |
||
|---|---|---|---|
| Film 2010–12 | DR 2010–12 | CR 2010–12 | |
| Oblique | 1.90 (0.88–3.91) | 1.46 (0.78–2.76) | 2.31 (1.08–4.69) |
| CC | 1.67 (0.84–3.33) | 1.32 (0.75–2.42) | 2.03 (1.12–3.95) |
CC, craniocaudal; CR, computed radiography; DR, digital radiography.
Table 6.
Breast dose for two-view examinations compared with previous data (errors represent 95% confidence limits)
| Mean MGD per two-view examination (mGy) |
|||||
|---|---|---|---|---|---|
| Film 1997–98 | Film 2001–02 | Film 2010–12 | DR 2010–12 | CR 2010–12 | |
| MGD | 4.19 ± 0.09 | 4.32 ± 0.05 | 4.01 ± 0.02 | 3.03 ± 0.01 | 4.69 ± 0.10 |
| Number of women | 3081 | 9562 | 9105 | 14,969 | 352 |
CR, computed radiography; DR, digital radiography; MGD, mean glandular dose.
Table 7.
Average mean glandular dose (MGD) and thickness for oblique projection views, for all breasts, for different types of digital radiography (DR), computed radiography (CR) and film-screen systems
| Manufacturer and model | Number of surveys | Number of main images | Mean MGD to breast (mGy) (±2SEM) | Mean thickness (mm) (±2SEM) |
|---|---|---|---|---|
| Fischer Senoscan® | 1 | 99 | 2.17 ± 0.16 | 56.9 ± 3.3 |
| Fujifilm Amulet | 10 | 1063 | 1.46 ± 0.04 | 57.3 ± 0.9 |
| GE 2000D | 2 | 199 | 1.70 ± 0.07 | 57.0 ± 0.8 |
| GE DS | 31 | 2891 | 1.55 ± 0.02 | 54.7 ± 0.6 |
| GE Essential | 61 | 5956 | 1.54 ± 0.02 | 62.4 ± 0.4 |
| Hologic Selenia® Mo | 16 | 1609 | 1.80 ± 0.03 | 55.6 ± 0.7 |
| Hologic Selenia® W | 45 | 4820 | 1.64 ± 0.01 | 56.7 ± 0.4 |
| Hologic Dimensions® | 31 | 4896 | 1.96 ± 0.02 | 63.3 ± 0.5 |
| IMS Giotto | 2 | 200 | 2.15 ± 0.12 | 57.6 ± 1.9 |
| Planmed Nuance | 1 | 1100 | 1.70 ± 0.03 | 60.8 ± 0.8 |
| Philips MicroDose | 22 | 1703 | 0.91 ± 0.02 | 63.2 ± 0.8 |
| Siemens Inspiration | 56 | 5430 | 1.37 ± 0.02 | 57.8 ± 0.4 |
| All DR systems | 278 | 29,966 | 1.58 ± 0.01 | 59.3 ± 0.2 |
| Fujifilm Profect CR | 9 | 799 | 2.52 ± 0.08 | 58.2 ± 0.9 |
| Film-screen systems | 160 | 18,408 | 2.11 ± 0.02 | 56.2 ± 0.2 |
| All systems | 447 | 49,702 | 1.79 ± 0.01 | 58.1 ± 0.1 |
SEM, standard error in the mean.
Fischer (Hologic, Inc., Marlborough, MA); Fujifilm (FUJIFILM UK Ltd, Bedford, UK); GE (GE Medical Systems, Buc, France); Hologic (Hologic, Inc.); IMS (Internazionale Medico Scientifica, Bologna Italy); Planmed (Planmed Oy, Helsinki, Finland); Philips (Philips Healthcare, Guildford, UK); Siemens (Siemens Healthcare GmbH, Erlangen, Germany).
Table 8.
Average mean glandular dose (MGD) and thickness for craniocaudal views, for all breasts, for different types of digital radiography (DR), computed radiography (CR) and film-screen systems
| Manufacturer and model | Number of surveys | Number of main images | Mean MGD to breast (mGy) (±2SEM) | Mean thickness (mm) (±2SEM) |
|---|---|---|---|---|
| Fischer Senoscan® | 1 | 100 | 1.87 ± 0.03 | 51.4 ± 2.4 |
| Fujifilm Amulet | 10 | 1064 | 1.30 ± 0.03 | 54.5 ± 0.8 |
| GE 2000D | 2 | 199 | 1.59 ± 0.06 | 55.3 ± 1.5 |
| GE DS | 31 | 2898 | 1.37 ± 0.02 | 51.7 ± 0.6 |
| GE Essential | 61 | 5946 | 1.32 ± 0.01 | 57.8 ± 0.4 |
| Hologic Selenia® Mo | 16 | 1306 | 1.68 ± 0.03 | 53.2 ± 0.7 |
| Hologic Selenia® W | 45 | 5537 | 1.48 ± 0.01 | 54.0 ± 0.3 |
| Hologic Dimensions® | 31 | 4719 | 1.78 ± 0.02 | 59.9 ± 0.4 |
| IMS Giotto | 2 | 199 | 1.85 ± 0.08 | 54.6 ± 1.6 |
| Planmed Nuance | 1 | 1116 | 1.57 ± 0.02 | 58.0 ± 0.7 |
| Philips MicroDose | 22 | 1706 | 0.87 ± 0.02 | 61.3 ± 0.7 |
| Siemens Inspiration | 56 | 5406 | 1.23 ± 0.01 | 55.6 ± 0.4 |
| All DR systems | 278 | 30,196 | 1.42 ± 0.01 | 56.3 ± 0.2 |
| Fujifilm Profect CR | 9 | 756 | 2.23 ± 0.07 | 56.1 ± 0.8 |
| Film-screen systems | 160 | 18,425 | 1.83 ± 0.01 | 53.5 ± 0.2 |
| All systems | 447 | 49,377 | 1.58 ± 0.01 | 55.2 ± 0.1 |
SEM, standard error in the mean.
Fischer (Hologic, Inc., Marlborough, MA); Fujifilm (FUJIFILM UK Ltd, Bedford, UK); GE (GE Medical Systems, Buc, France); Hologic (Hologic, Inc.); IMS (Internazionale Medico Scientifica, Bologna Italy); Planmed (Planmed Oy, Helsinki, Finland); Philips (Philips Healthcare, Guildford, UK); Siemens (Siemens Healthcare GmbH, Erlangen, Germany).
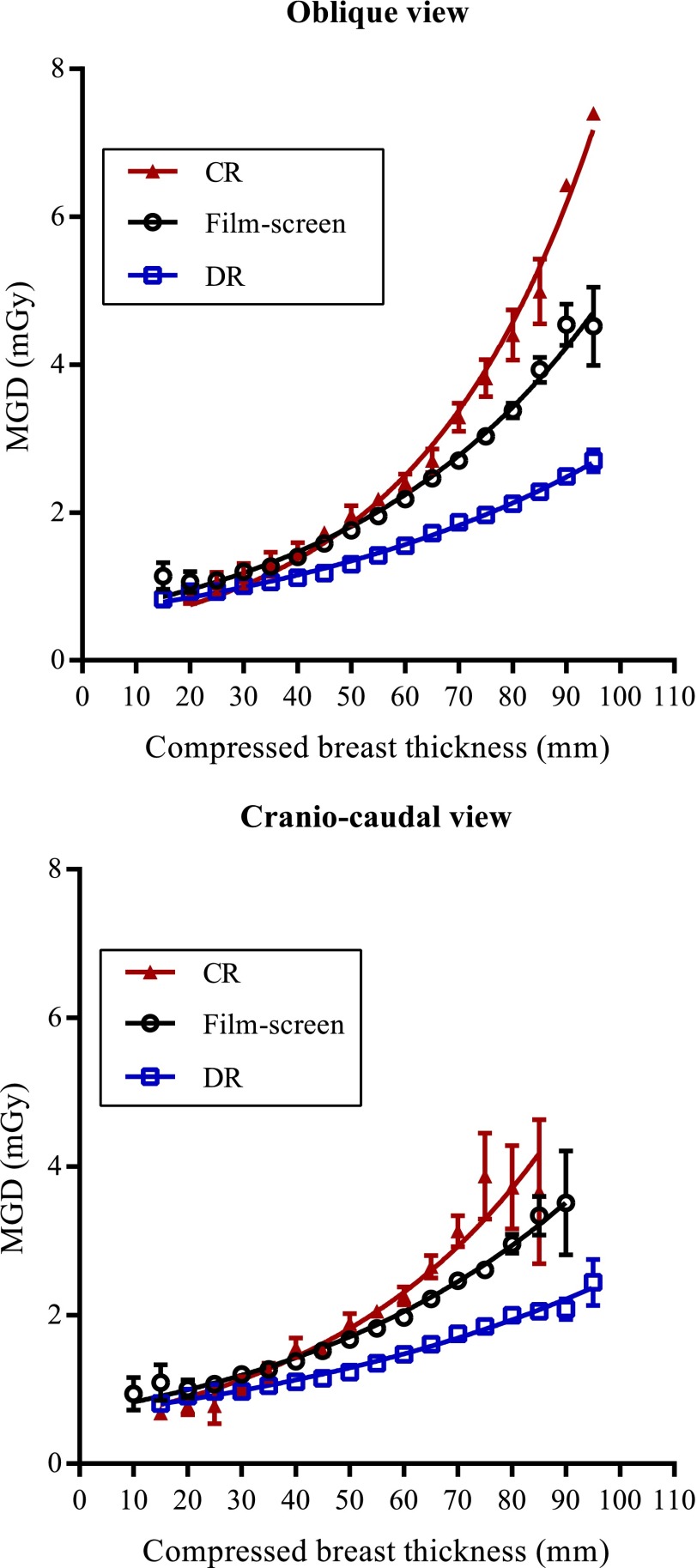
Variation in dose with compressed breast thickness
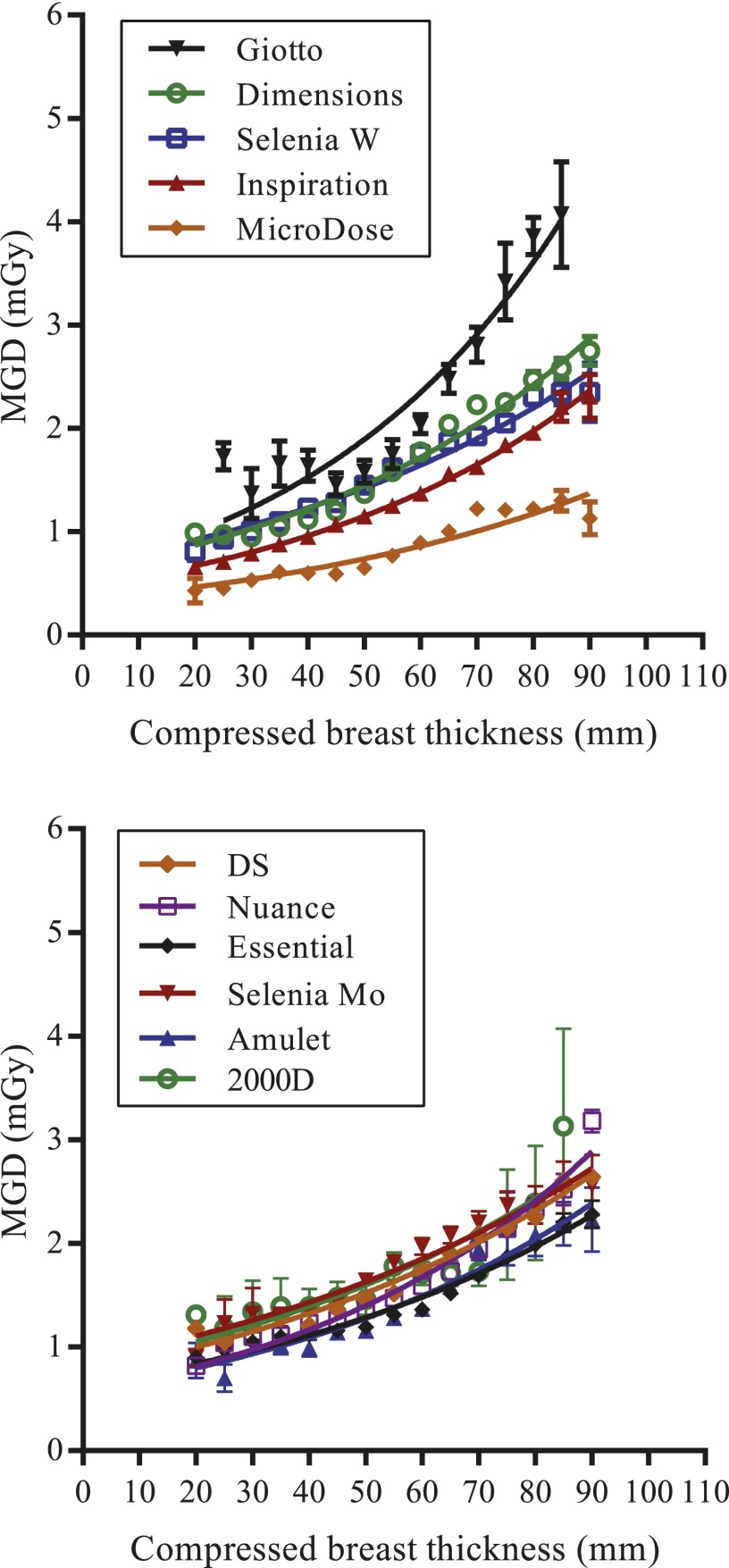
The average MGDs for OB and CC images are shown for film-screen, DR and CR systems as a function of compressed breast thickness in Figure 2. The variations in dose with breast thickness for some different models of DR system are shown in Figure 3.
Figure 2.
Average mean glandular dose per view as a function of compressed breast thickness. The error bars show 95% confidence limits; for some data points, the errors are too small to be seen.
Figure 3.
An average mean glandular dose per view (main oblique projection only) as a function of compressed breast thickness for different models of the digital radiography system. The error bars show 95% confidence limits; for some data points, the errors are too small to be seen.
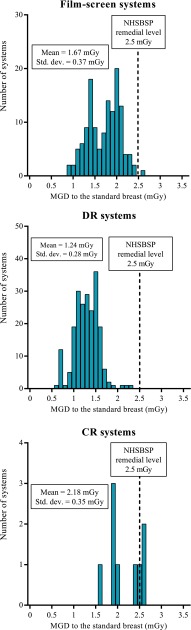
Standard breast dose
The MGD to the 53 mm-thick standard breast simulated with 45 mm of PMMA was reported for 359 systems and averaged 1.43 ± 0.04 mGy and was similar to the average of 1.42 ± 0.04 for screening in 2001–02. The minimum was 0.60 and the maximum 2.64 mGy. For three systems, the MGD to the standard breast was above the 2.5 mGy remedial level set by the NHSBSP. Two of these were CR systems and the other a film-screen system. The distributions of the MGD to the standard breast for DR, CR and film-screen systems are shown in Figure 4. The average MGD to the standard breast for the different imaging systems are shown in Table 9.
Figure 4.
Histograms of the average mean glandular dose to the 53 mm-thick standard breast for different types of imaging system.
Table 9.
Average mean glandular dose (MGD) to the 53 mm-thick standard breast model for different types of digital radiography (DR), computed radiography (CR) and film-screen systems
| Manufacturer and model | Number of systems | Mean MGD to standard breast (mGy) (±2SEM) |
|---|---|---|
| Fujifilm Amulet | 7 | 1.06 ± 0.08 |
| GE DS | 26 | 1.19 ± 0.03 |
| GE Essential | 40 | 1.24 ± 0.04 |
| Hologic Selenia® Mo | 3 | 2.06 ± 0.25 |
| Hologic Selenia® W | 45 | 1.43 ± 0.04 |
| Hologic Dimensions® | 27 | 1.46 ± 0.02 |
| IMS Giotto | 2 | 1.56 ± 0.24 |
| Philips MicroDose | 16 | 0.68 ± 0.03 |
| Siemens Inspiration | 47 | 1.10 ± 0.06 |
| All DR systems | 214 | 1.24 ± 0.04 |
| Fujifilm Profect CR | 9 | 2.15 ± 0.26 |
| Film-screen systems | 160 | 1.67 ± 0.06 |
| All systems | 359 | 1.43 ± 0.04 |
SEM, standard error in the mean.
Fischer (Hologic, Inc., Marlborough, MA); Fujifilm (FUJIFILM UK Ltd, Bedford, UK); GE (GE Medical Systems, Buc, France); Hologic (Hologic, Inc.); IMS (Internazionale Medico Scientifica, Bologna Italy); Planmed (Planmed Oy, Helsinki, Finland); Philips (Philips Healthcare, Guildford, UK); Siemens (Siemens Healthcare GmbH, Erlangen, Germany).
Diagnostic reference level
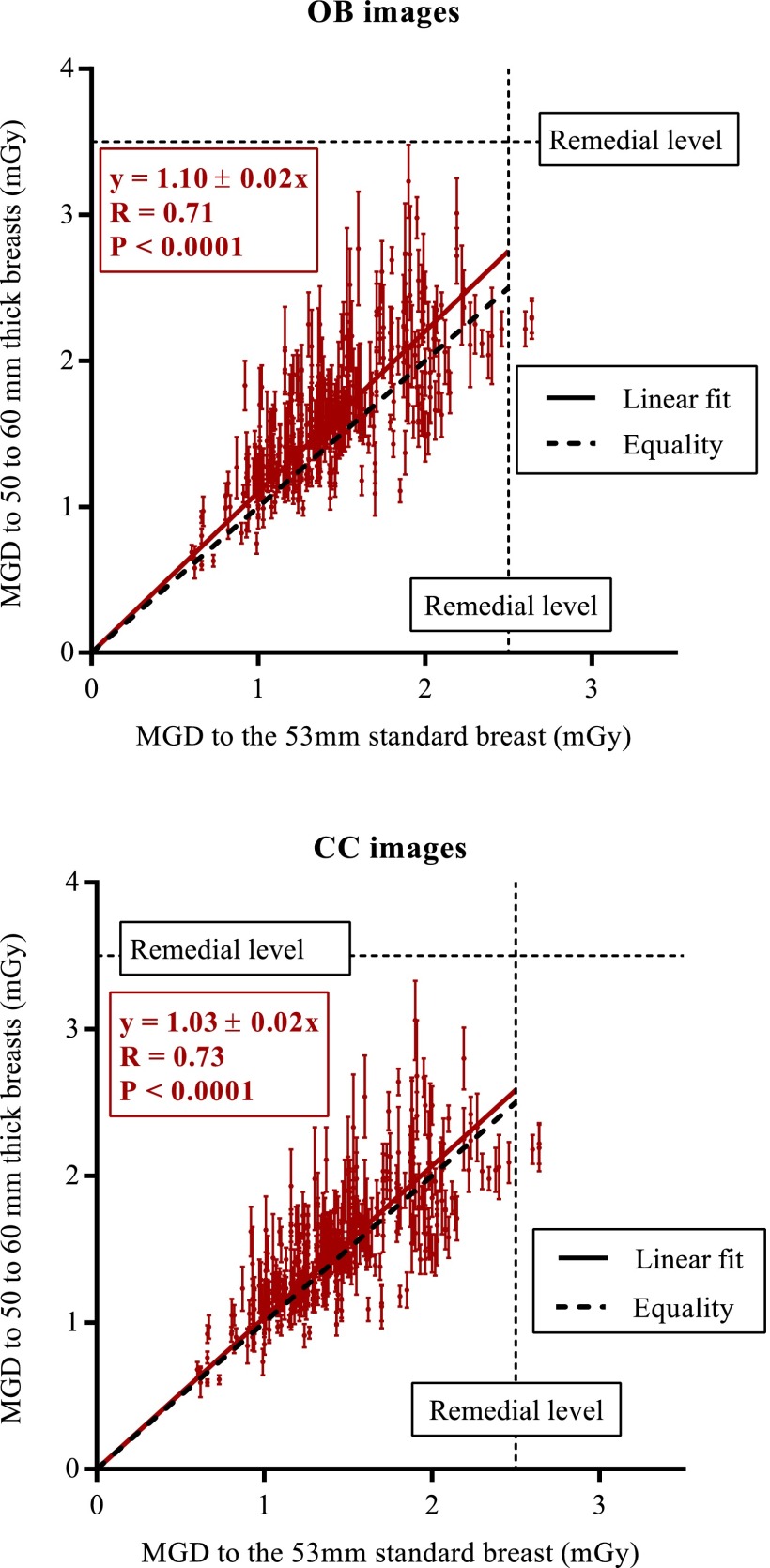
The average MGD for main OB films for 50–60 mm-thick breasts was 1.70 ± 0.01 mGy, with a minimum of 0.58 mGy and maximum of 3.26 mGy, with distributions by system type shown in Figure 5. No systems exceeded the NDRL of 3.5 mGy. Figure 6 shows the MGD for 50–60 mm-thick breasts plotted against the MGD for the 53 mm-thick standard breast for OB and CC views. The regression lines were set to intercept the origin and had a significance of p < 0.0001. For the OB images, the correlation coefficient was 0.71 with a gradient of 1.10 (95% confidence limits: 1.08–1.12). For the CC images, the correlation coefficient was 0.74 with a gradient of 1.04 (95% confidence limits: 1.01–1.05). The average doses for 50–60 mm-thick compressed breasts for OB and CC views for the different imaging systems are shown in Tables 10 and 11.
Figure 5.
Histograms of the average mean glandular dose to 50–60 mm-thick breasts for different types of imaging system.
Figure 6.
The average mean glandular dose (MGD) for main oblique projection and craniocaudal images of 50–60 mm-thick breasts plotted against the MGD to the 53 mm-thick standard breast for each unit. A linear correlation fitted to pass through the origin is shown. The error bars show 95% confidence limits.
Table 10.
Mean glandular dose (MGD) and thickness for oblique projection views, for 50–60 mm breasts, for different types of digital radiography (DR), computed radiography (CR) and film-screen systems
| Manufacturer and model | Number of main images | Mean MGD to breast (mGy) (±2SEM) | Mean thickness (mm) (±2SEM) |
|---|---|---|---|
| Fischer Senoscan® | 19 | 1.92 ± 0.10 | 55.1 ± 1.5 |
| Fujifilm Amulet | 284 | 1.28 ± 0.04 | 55.1 ± 0.4 |
| GE 2000D | 70 | 1.67 ± 0.08 | 56.0 ± 0.8 |
| GE DS | 662 | 1.57 ± 0.04 | 55.2 ± 0.2 |
| GE Essential | 1261 | 1.30 ± 0.02 | 55.4 ± 0.2 |
| Hologic Selenia® Mo | 396 | 1.83 ± 0.03 | 55.2 ± 0.3 |
| Hologic Selenia® W | 1559 | 1.82 ± 0.05 | 55.3 ± 0.2 |
| Hologic Dimensions® | 843 | 1.60 ± 0.03 | 55.4 ± 0.2 |
| IMS Giotto | 50 | 1.79 ± 0.08 | 55.8 ± 0.9 |
| Planmed Nuance | 299 | 1.47 ± 0.03 | 55.3 ± 0.4 |
| Philips MicroDose | 233 | 0.79 ± 0.03 | 55.7 ± 0.4 |
| Siemens Inspiration | 1370 | 1.25 ± 0.02 | 55.1 ± 0.2 |
| All DR systems | 7046 | 1.45 ± 0.01 | 55.3 ± 0.1 |
| Fujifilm Profect CR | 243 | 2.20 ± 0.07 | 55.5 ± 0.4 |
| Film-screen systems | 5494 | 1.99 ± 0.02 | 55.2 ± 0.1 |
| All systems | 12,848 | 1.70 ± 0.01 | 55.3 ± 0.6 |
SEM, standard error in the mean.
Fischer (Hologic, Inc., Marlborough, MA); Fujifilm (FUJIFILM UK Ltd, Bedford, UK); GE (GE Medical Systems, Buc, France); Hologic (Hologic, Inc.); IMS (Internazionale Medico Scientifica, Bologna Italy); Planmed (Planmed Oy, Helsinki, Finland); Philips (Philips Healthcare, Guildford, UK); Siemens (Siemens Healthcare GmbH, Erlangen, Germany).
Table 11.
Mean glandular dose (MGD) and thickness for craniocaudal views, for 50–60 mm breasts, for different types of digital radiography (DR) system and film-screen for comparison
| Manufacturer and model | Number of main images | Mean MGD to breast (mGy) (±2SEM) | Mean thickness (mm) (±2SEM) |
|---|---|---|---|
| Fischer Senoscan® | 35 | 2.01 ± 0.16 | 54.1 ± 0.9 |
| Fujifilm Amulet | 425 | 1.20 ± 0.03 | 54.8 ± 0.3 |
| GE 2000D | 77 | 1.60 ± 0.07 | 55.3 ± 0.8 |
| GE DS | 744 | 1.45 ± 0.03 | 55.0 ± 0.2 |
| GE Essential | 1627 | 1.23 ± 0.02 | 55.2 ± 0.2 |
| Hologic Selenia® Mo | 449 | 1.76 ± 0.04 | 55.1 ± 0.3 |
| Hologic Selenia® W | 1816 | 1.52 ± 0.02 | 55.0 ± 0.1 |
| Hologic Dimensions® | 1159 | 1.55 ± 0.03 | 55.4 ± 0.2 |
| IMS Giotto | 77 | 1.72 ± 0.08 | 55.6 ± 0.6 |
| Planmed Nuance | 379 | 1.48 ± 0.02 | 55.4 ± 0.3 |
| Philips MicroDose | 319 | 0.74 ± 0.02 | 55.6 ± 0.3 |
| Siemens Inspiration | 1571 | 1.18 ± 0.02 | 55.0 ± 0.2 |
| All DR systems | 8678 | 1.37 ± 0.01 | 55.2 ± 0.1 |
| Fujifilm Profect CR | 353 | 2.18 ± 0.06 | 55.5 ± 0.3 |
| Average film-screen | 6418 | 1.83 ± 0.02 | 55.1 ± 0.1 |
| All systems | 15,449 | 1.58 ± 0.01 | 55.1 ± 0.1 |
CR, computed radiography; SEM, standard error in the mean.
Fischer (Hologic, Inc., Marlborough, MA); Fujifilm (FUJIFILM UK Ltd, Bedford, UK); GE (GE Medical Systems, Buc, France); Hologic (Hologic, Inc.); IMS (Internazionale Medico Scientifica, Bologna Italy); Planmed (Planmed Oy, Helsinki, Finland); Philips (Philips Healthcare, Guildford, UK); Siemens (Siemens Healthcare GmbH, Erlangen, Germany).
High-dose subgroup
Some women with relatively large compressed breast thicknesses received the highest doses. This was quantified by determining the doses per view for women with a compressed breast thickness in excess of 90 mm (Table 12). A subgroup comprising 0.6% and 1.8% of women screened using the film-screen and DR systems, respectively, had a compressed breast thickness ≥90 mm for the OB view. Smaller proportions (0.1% and 0.5%) had breasts with a compressed breast thickness ≥90 mm in the CC view. The women with thicker breasts (i.e.>90 mm) who were screened using film-screen systems had average doses of 4.61 mGy per OB view, which is about 2.2 times the average dose of 2.13 mGy for all women screened with these systems. Those women screened using DR systems with thicker breasts had an average OB dose of 2.65 mGy, which is about 1.7 times the average dose of 1.60 mGy for all women screened with DR systems and 43% less than if they had been screened with an average film-screen system.
Table 12.
Average doses for breasts with compressed thickness ≥90 mm
| View | 2001–02 All | 2010–12 film-screen | 2010–12 DR | 2010–12 CR | |
|---|---|---|---|---|---|
| MGD per film (mGy) (±2 standard error in mean) | OB | 5.07 ± 0.27 | 4.61 ± 0.38 | 2.65 ± 0.09 | 6.92 ± 0.98 |
| CC | 3.55 ± 0.72 | 3.64 ± 0.76 | 2.30 ± 0.18 | – | |
| Number of films (proportion of women) | OB | 261 (0.81%) | 109 (0.64%) | 446 (1.75%) | 2 |
| CC | 28 (0.15%) | 23 (0.13%) | 116 (0.46%) | 0 | |
| Average compressed breast thickness (mm) (±2 standard error in mean) | OB | 95.0 ± 0.5 | 95.9 ± 1.0 | 94.7 ± 0.4 | 92.0 ± 2.0 |
| CC | 95.8 ± 1.8 | 93.3 ± 1.2 | 93.9 ± 0.8 | – |
CC, craniocaudal; CR, computed radiography; DR, digital radiography; MGD, mean glandular dose; OB, oblique projection.
DISCUSSION
Data included
The data analysed here are broadly representative of the NHSBSP. In general, the data collected represent one data set per X-ray system, but, in a few cases, the dose survey was repeated at another date on the same system. The women were almost all in the normal screening age range of 50–70 years with an average age of 57 years. In a previous work, it has been shown that age between 40 and 64 years is not a major factor affecting patient dose.9 The equipment included a wide range of digital X-ray systems and film-screen systems.
X-ray technique
The introduction of digital mammography systems into the NHSBSP has caused some dramatic changes since the publication on radiation doses in the NHSBSP covering the period 2001–02. Where film-screen systems were still used in 2010–12, the target/filter combination selected remained dominated by molybdenum (Mo)/Mo and Mo/rhodium (Rh) for 99% of exposures. DR systems use a limited selection of target and filter materials which vary from one model to another. The change in the combinations used in the NHSBSP has therefore been driven by the changes in the installed equipment base and decisions made by manufacturers at the design stage. Thus, for DR systems, Mo/Mo and Mo/Rh target/filter combinations were used for only about 5% of exposures. Most exposures with DR systems used other target/filter combinations such as Rh/Rh (26%), tungsten (W)/Rh (52%), W/silver (Ag) (11%) and W/aluminium (Al) (6%). These latter target/filter combinations produce higher energy spectra that can be expected to lower patient dose. As the NHSBSP moves towards being fully digital, this increased use of higher energy spectra will continue.
Average doses
The average MGD per OB image using film-screen systems has fallen by about 5% since 2001–02. The average MGD for CC films has reduced by about 6%. The average MGD per OB image using DR systems was about 25% lower than for film-screen systems. The average MGD per CC image using DR systems was about 22% lower than for film-screen systems. The average thickness for both OB and CC views using film-screen systems was about the same as for film-screen systems in 2001–02. The average thickness for both OB and CC films was greater with DR systems than with film-screen systems in 2010–12 by about 3 mm. This difference may be due to the way in which the systems have their thickness scales calibrated. It may also be related to the use of tilting paddles with some models. Table 4 also shows that compressed breast thickness has increased by about 2 mm from 1997–98 to 2010–12. Doses for CC images were about 11–14% lower than for OB images. In previous dose surveys, CC images had doses that were about 19% lower than for OB images. The small difference of about 3 mm found in the compressed breast thickness may explain some of this dose difference.
The MGD for a full 2V examination is slightly higher than the sum of the doses for the OB and CC projections in Table 5 because of the inclusion of extra dose from additional images shown in Table 2. This is shown in Table 6, where the dose using film-screen systems has reduced slightly to 4.06 mGy as compared with 4.32 mGy in 2001–02. The average dose for a 2V examination using a DR system is about 25% lower than for film-screen systems at 3.06 mGy.
The range of doses for different types of DR system was quite marked, with the Philips MicroDose giving the lowest average doses per main image of 0.99 mGy and 0.93 mGy for OB and CC views, respectively. The Internazionale Medico Scientifica (IMS) Giotto system had the highest average doses of 2.23 mGy and 1.85 mGy for OB and CC views, respectively. Thus, the amount of dose reduction on switching from film-screen to DR systems is very dependent on which DR system is used. Centres using the Philips systems are using radiation doses that are about half of the average for film-screen systems.
Compressed breast thickness and beam quality selection
Compressed breast thickness is a major factor affecting the radiation dose received by a female for a particular mammography system. Compressed thicknesses ranged from 10 to 100 mm with averages of about 58 mm for OB images and 55 mm for CC images. The thicknesses reported in 1997–98 were about 4 mm less than these (Table 4). Explanations for this apparent change are a real increase in breast size due to a rise in obesity levels, application of less compression force or changes in thickness calibration, e.g. due to new tilting paddles. Table 7 shows that the average compressed breast thickness depends on the imaging system used. Thus, the older Hologic Selenia systems had average compressed breast thicknesses of 56 mm (Mo target) or 57 mm (W target), while breasts imaged with the newer Hologic Dimensions systems had an average thickness of 63 mm. Such a difference may be due to either the calibration method or paddle design. Thus, it is likely that the increase in average breast thickness seen in Table 4 is due to changes in equipment rather than women.
The difference in thickness partly explains why doses are higher for OB than for CC images. However, Figure 6 shows that there appears to be an additional factor. For breasts with thickness in the range 50–60 mm, average doses were 1.70 and 1.58 mGy for OB and CC views; a difference of 7.6%. It is possible that it is the presence of the pectoral muscle affecting the automatic exposure control (AEC) selection that is the cause of greater doses for OB images of the same compressed breast thickness as for CC images. In general, there was a curvilinear relationship between the compressed breast thickness and the dose per image. For the film-screen and CR systems, the dose rises increasingly steeply with increasing breast thickness (Figure 2). For film-screen systems, the average dose per image rose from 1.09 mGy for a 20 mm-thick compressed breast to 4.59 mGy for a 90-mm-thick compressed breast (Figure 2). For DR systems, the average dose per image rose from 0.92 mGy for a 20 mm-thick compressed breast to 2.46 mGy for a 90 mm-thick compressed breast. Thus, DR systems gave doses to 90-mm-thick breasts which were about 46% less than that for film-screen systems. For CR systems, the average dose per image rose from 0.81 mGy for a 20 mm-thick compressed breast to 6.34 mGy for a 90-mm-thick compressed breast.
Figure 3 showed that the change in dose with thickness varied from one model of DR system to another. For Philips systems, the average dose per image rose from 0.43 mGy for a 20 mm-thick compressed breast to 1.13 mGy for a 90 mm-thick compressed breast. By comparison, the Hologic Dimensions gave doses that rose from 0.99 mGy to 2.75 mGy from 20- to 90 mm breast thickness. Thus, for the largest breasts, the differences in doses between digital systems was quite marked.
Standard breast dose
The MGD to the standard breast model is calculated relatively easily by combining the mAs for correct exposure of different thicknesses of blocks of PMMA with values of tube output and beam quality.2 Here, data have been analysed for the 53 mm-thick standard breast simulated using a 45 mm-thick block of PMMA. The advantage of this approach is that the effect of equipment factors can be assessed, while eliminating patient variables. The exposure factors are those selected automatically by the X-ray set. The limitation of the standard breast method is that it does not indicate the actual doses to individual women. The doses calculated for real breasts depend on how the AEC systems respond to the heterogeneous nature of the breast tissue so that doses may be different from those for the standard breast model. Nonetheless, one would expect mammography systems to have a correlation between standard breast doses and average breast doses. Figure 6 shows that the average MGD for 50–60 mm-thick breasts and the MGD to the 53 mm-thick standard breast were linearly correlated for OB and CC views. The gradients of the correlations showed that the dose for an OB image on an average-sized breast (i.e. 55 mm thick) was about 11% higher than the dose to the standard breast on the same system. Part of this difference is owing to the fact that the standard breast is only 53 mm thick. In addition, breast tissue is inhomogeneous unlike PMMA, and this affects the operation of AEC systems. Figure 6 also shows that the dose for CC images on average-sized breasts (i.e. 55-mm thick) was about 4% higher than the dose to the standard breast on the same system.
The average MGD to the 53 mm-thick standard breast was 1.43 mGy for all systems. Again, doses for different types of system were quite different, with the Philips systems giving the lowest average doses of 0.68 mGy and the CR systems giving the highest average doses of 2.15 mGy (Table 9).
Diagnostic reference level
No systems exceeded the NDRL of 3.5 mGy for OB images of 50–60 mm-thick breasts (Figure 5). The NDRL should be kept under review but should only be reduced if this is possible without significantly impacting image quality. It would be undesirable to set a lower DRL whereby many systems failed as this could lead to dose reductions which might compromise image quality. Average doses for OB and CC views of average sized breasts (50–60 mm thick) were fairly well correlated with the dose to the 53 mm-thick standard breast, and were on average 10% and 3% higher, respectively.
High-dose subgroup
While the average dose per OB image was about 1.8 mGy, there are subgroups of women for whom the doses are higher. One identifiable subgroup of women who receive larger doses than the average comprises those women with relatively thick breasts on compression. It is shown in Table 12 that the small subgroup of women with compressed breasts of thickness ≥90 mm had doses for OB films of about 2.2 times the average for film-screen systems and 1.66 times the average for DR systems. Another factor that affects the doses to women is the equipment used. This can be appreciated by examining the doses to the standard breast, which ranged from 0.60 to 2.64 mGy. 3 out of 441 systems exceeded the remedial level for the MGD to the standard breast of 2.5 mGy.
For a mammography system with the highest acceptable standard breast dose of 2.5 mGy, breast doses of about 1.50 times the average can be expected for film systems and 2.02 times the average for DR systems. It is assumed here that doses to breasts of all sizes will be greater by approximately these factors. Thus, using this assumption, one can expect that a few women with large breasts (>90 mm thick) would receive doses of about 7.0 mGy per OB view (i.e. 2.2 × 1.50 × 2.11 mGy) if imaged with a film-screen system at the maximum permitted standard breast dose. If a DR system was used at the maximum permitted dose, a few women would receive doses of about 5.3 mGy per OB view (i.e. 1.66 × 2.02 × 1.58 mGy). In fact, only 36 out of 18,491 film-screen OB images (i.e. 0.07%) had doses in excess of 7.0 mGy. Only 22 out of 30,525 DR OB images (i.e. 0.19%) had doses in excess of 5.3 mGy. Therefore, these doses per image can be regarded as upper limits to what can normally be expected for film-screen and DR screening mammograms in the NHSBSP. Using the same arguments as above and the data from Table 12, one can estimate the maximum normally expected dose for a CC view. The highest expected dose for a CC view is 5.4 mGy (i.e. 1.99 × 1.50 × 1.83 mGy) using a film-screen system and 4.5 mGy (i.e. 1.62 × 2.02 × 1.42 mGy) using a DR system. Thus, the maximum dose that may be normally expected for a 2V examination is 12.4 mGy for a film-screen system and 9.8 mGy for a DR system, if there is one image per view. In practice, only 6 women (0.09%) out of 8775 women received >12.4 mGy for a 4-image 2V examination using a film-screen system. Only 8 women (0.05%) out of 14,569 women received >9.8 mGy for a 4-image 2V examination using a DR system. Thus, one may conclude that a very small proportion of women will receive about 3.1 times (i.e. 12.4 ÷ 4.01) the average dose for the screening programme using film-screen systems. Where DR systems are used, a very small proportion of women will receive about 3.2 times (i.e. 9.8 ÷ 3.03) the average dose. These identifiable subgroups should be considered in any risk–benefit analysis. The trend towards using DR imaging systems will lower doses for women with breasts with a large compressed breast thickness.
Optimization
The Ionising Radiation (Medical Exposure) Regulations 2000 require that X-ray systems be optimized. This means that radiation doses should be “as low as reasonably practicable consistent with the intended purpose”. The intended purpose here is the detection of breast cancers by screening. The data provided here give some information to help decide whether specific designs of digital mammography system are operating at an appropriate dose level, i.e. neither too high nor too low. Recent research has shown that the detection of cancers (and specifically microcalcifications) using digital mammography systems is very sensitive to the radiation dose used.13 Given the wide variation in doses being used with digital mammography, further research to fully optimize the dose setting of these systems seems merited and in particular to evaluate the risks and benefits of using higher or lower doses with specific designs of system.
Other studies
Other breast-screening programmes have also reported on the impact of adopting digital imaging on radiation doses. The Flemish screening programme reported that the replacement of film-screen systems with DR systems lead to a 26% reduction in MGD for breasts simulated with 45-mm PMMA and a similar 26% reduction for the median MGD for patients.14 Where film-screen systems were replaced with CR systems, there was a 35% increase in the MGD estimated using a 45 mm thickness of PMMA and a 29% increase for the median patient doses. In a smaller study, Gennaro and di Maggio15 reported a 27% lower dose when using the GE 2000D DR system compared with a film-screen system using a GE DMR X-ray set. The Ontario breast-screening programme reported for 2009 average MGD for DR systems that were 1.16 mGy per view which was 27.5% lower than the MGD for screen film systems which was 1.60 mGy.16 Unusually, the MGD for CR systems was also lower by 15% at an MGD of 1.36 mGy. Thus, it seems that there has been a reduction in dose of about 25% where programmes have switched to using DR systems instead of film-screen systems. As in our study, the Flemish programme reported larger dose reductions for larger breasts of about 36%. Tables 7–9 show how the choice of make and model of DR system has a great effect on the MGD. This has also been reported by the Irish screening programme, where the average total examination dose was 1.86 mGy where the Sectra MDM L30 (same design as the Philips MicroDose) was used and 3.03 mGy where the GE Essential was used.17
Limitations
The main limitation of this study is owing to the limitations of the dose estimation methodology in UK and European Guidelines.2–4 In this procedure, the actual composition of the breasts for which doses are estimated is usually unknown, and a simple relationship between breast thickness and composition is assumed.5 It is further assumed that the glandular tissue is uniformly distributed with a 5 mm adipose layer at the top and bottom of the compressed breast. In practice, glandular tissue is non-uniformly distributed, and doses estimated for any particular breast could be in error by as much as 43%.18 The expectation is that these errors will be averaged out for the population as a whole. However, there may be some systematic overestimation or underestimation of doses. A recent article using breast CT data has suggested that the use of realistic heterogeneous glandular distributions reduces dose estimates by 30%.19 Nonetheless, the major findings here, for example, concerning differences between different manufacturer systems and the reduction in dose following the introduction of DR systems should be valid.
CONCLUSION
We have reported the results of a very large sample of doses, which give a good representation of the performance of breast-screening units in the UK. All the units complied with the NDRL standard for MGD to the standard size breast. Increasing use of DR systems has reduced the radiation dose for all types of breast but especially large breasts. The introduction of DR systems reduces average dose by approximately 25% as compared with film-screen systems. While a modest dose reduction may be justified by the increasing efficiency of modern systems, going beyond this is not desirable as it will reduce image quality and hence cancer detection.
Acknowledgments
ACKNOWLEDGMENTS
The authors would like to acknowledge the work of the many radiographers and physicists throughout the UK who collected the raw data analysed in this article. We would also like to acknowledge the support of the National Health Service Breast Screening Quality Assurance Coordinating Group for Physics.
Contributor Information
Kenneth C Young, Email: ken.young@nhs.net.
Jennifer M Oduko, Email: jenny.oduko@nhs.net.
FUNDING
The National Office of the NHS Cancer Screening Programmes (now within the Health and Wellbeing Directorate of Public Health England) funded the authors.
REFERENCES
- 1.Breast screening programme, England—2011–12. London, UK: Health & Social Care Information Centre. Published 27 February, 2013. Available from: http://www.hscic.gov.uk/catalogue/PUB10339 [Google Scholar]
- 2.Moore AC, Dance DR, Evans DS, Lawinski CP, Pitcher EM, Rust A, et al. The commissioning and routine testing of mammographic X-ray systems. (IPEM Report 89). York, UK: Institute of Physics and Engineering in Medicine; 2005. [Google Scholar]
- 3.Dance DR. Monte Carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol 1990; 35: 1211–19. doi: 10.1088/0031-9155/35/9/002 [DOI] [PubMed] [Google Scholar]
- 4.van Engen RE, Bosmans H, Dance DR, Heid P, Lazzari B, Marshall N, et al. Digital mammography update. European protocol for the quality control of the physical and technical aspects of mammography screening. S1, Part 1: Acceptance and constancy testing. In: European guidelines for quality assurance in breast cancer screening and diagnosis. Perry N, Broeders M, de Wolf C, Törnberg S, Holland R, von Karsa L. (eds.). Luxembourg, Europe. European Commission, Office for Official Publications of the European Union; 2013. pp. 1–54. [Google Scholar]
- 5.Dance DR, Skinner CL, Young KC, Beckett JR, Kotre CJ. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol 2000; 45: 3225–40. doi: 10.1088/0031-9155/45/11/308 [DOI] [PubMed] [Google Scholar]
- 6.Dance DR, Young KC, van Engen RE. Further factors for the estimation of mean glandular dose using the United Kingdom, European and IAEA dosimetry protocols. Phys Med Biol 2009; 54: 4361–72. doi: 10.1088/0031-9155/54/14/002 [DOI] [PubMed] [Google Scholar]
- 7.Young KC, Burch A. Radiation doses received in the UK Breast Screening Programme in 1997 and 1998. Br J Radiol 2000; 73: 278–87. doi: 10.1259/bjr.73.867.10817044 [DOI] [PubMed] [Google Scholar]
- 8.Young KC. Radiation doses in the UK trial of breast screening in women aged 40 –48. Br J Radiol 2002; 75: 362–70. doi: 10.1259/bjr.75.892.750362 [DOI] [PubMed] [Google Scholar]
- 9.Young KC, Burch A, Oduko JM. Radiation doses received in the UK breast screening programme in 2001 and 2002. Br J Radiol 2005; 78: 207–18. doi: 10.1259/bjr/41095952 [DOI] [PubMed] [Google Scholar]
- 10.Oduko JM, Young KC, Burch A. A survey of patient doses from digital mammography systems in the UK in 2007 to 2009. In: Martí EA, ed. Proceedings of the 10th International Workshop on digital mammography; 2010 June 16-18; Girona, Spain. Berlin, Germany: Springer-Verlag, Lecture Notes in Computer Science 6136: 365–70, 2010.
- 11.Young KC. Breast dose surveys in the NHSBSP: software and instruction manual. [Published July 2004]. Available from: http://www.nccpm.org/.
- 12.Guidance on the establishment and use of diagnostic reference levels for medical X-ray examinations. (IPEM Report 88). York, UK: Institute of Physics and Engineering in Medicine; 2004. [Google Scholar]
- 13.Warren LM, Mackenzie A, Cooke J, Given-Wilson RM, Wallis MG, Chakraborty DP, et al. Effect of image quality on calcification detection in digital mammography. Med Phys 2012; 39: 3202–13. doi: 10.1118/1.4718571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Timmermans L, De Hauwere A, Bacher K, Bosmans H, Lemmens K, Bleyen L. et al. Impact of the digitalisation of mammography on performance parameters and breast dose in the Flemish Breast Cancer Screening Programme. Eur Radiol 2014; 24: 1808–19. doi: 10.1007/s00330-014-3169-y [DOI] [PubMed] [Google Scholar]
- 15.Gennaro G, di Maggio C. Dose comparison between screen/film and full-field digital mammography. Eur Radiol 2006; 16: 2559–66. doi: 10.1007/s00330-006-0314-2 [DOI] [PubMed] [Google Scholar]
- 16.Yaffe MJ, Bloomquist AK, Hunter DM, Mawdsley GE, Chiarelli AM, Muradali D, et al. Comparative performance of modern digital mammography systems in a large breast screening program. Med Phys 2013; 40: 121915. doi: 10.1118/1.4829516 [DOI] [PubMed] [Google Scholar]
- 17.McCullagh JB, Baldelli P, Phelan N. Clinical dose performance of full field digital mammography in a breast screening programme. Br J Radiol 2011; 84: 1027–33. doi: 10.1259/bjr/83821596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dance DR, Hunt RA, Bakic PR, Maidment AD, Sandborg M, Ullman G, et al. Breast dosimetry using high-resolution voxel phantoms. Radiat Prot Dosimetry 2005; 114: 359–63. doi: 10.1093/rpd/nch510 [DOI] [PubMed] [Google Scholar]
- 19.Hernandez AM, Seibert JA, Boone JM. Breast dose in mammography is about 30% lower when realistic heterogeneous glandular distributions are considered. Med Phys 2015; 42: 6337. doi: 10.1118/1.4931966 [DOI] [PMC free article] [PubMed] [Google Scholar]