Abstract
Objective:
To study the precise location of fracture line in hangman's fracture to determine the fracture patterns, symmetry and involvement of different vertebral elements.
Methods:
32 cases of hangman's fractures were retrospectively evaluated. All patients presented with motor vehicle accidents. CT scans were studied to accurately localize the fracture lines. Symmetry of fracture lines on both sides was assessed, and involvement of the vertebral bodies, lamina, facet joints and foramen transversarium was also determined.
Results:
20 patients showed asymmetric fracture locations, 13 of them had a unilateral pedicle fracture and a contralateral pars fracture which comprised the most common injury pattern (40% of cases). Less frequent combinations for the two sides of asymmetric C2 ring disruption include pars–vertebral body (3 patients), pedicle–vertebral body (2 patients) and pedicle–lamina (2 patients). 12 patients showed symmetrical fractures (5 through the pars and 7 through the pedicles). Vertebral body and facet joint involvement were demonstrated in 15 (47%) and 16 (50%) cases, respectively. 18 cases had fractures extending into the foramen transversarium (56%). In total, 26 fracture lines primarily affected the pars (40%) and 31 affected the pedicles (49%).
Conclusion:
Asymmetric hangman's fracture is more common with the usual pattern being fracture pedicle on one side and pars on the other followed by the symmetric bilateral pedicle and bilateral pars fractures. Fracture lines running into the transverse foramen and facet joints are very frequent as well as those involving the vertebral bodies.
Advances in knowledge:
There is controversy in literature regarding the fracture locations in hangman's injury owing to lack of studies that address this subject. This article is the first to describe precisely the anatomical locations and patterns of this injury.
INTRODUCTION
Schneider was the first to describe hangman's fracture in individuals with injuries unrelated to judicial hanging.1 He described this injury as avulsion of the neural arch through the pedicle or lamina of C2 with spondylolisthesis of the C2 over C3: traumatic spondylolisthesis of the axis.
Since its first description, there was an ongoing controversy regarding the definition and exact location of this injury. Authors have reported variable sites, and in most of the cases, they used broad terms rather than accurately specified the anatomical locations.
Effendi et al2 in their treatise of 131 patients reported that the fractures of the ring (neural arch) of C2 may occur through the laminae, pedicles, pars interarticularis, facets and may extend to the body and foramen transversarium. They also suggested that this fracture tends to be asymmetrical. They reported four cases of vertebral artery injury that presented with hemiplegia/hemiparesis that were proven by angiography.
More recently, Duggal, Li, Muller, Tian and other authors have also used the general definition of traumatic spondylolisthesis of axis: a neural arch fracture.3–6 Duggal et al3 also suggested that this injury is almost always asymmetrical owing to the rotational element during the extension component of the injury vector.
However, other authors such as Francis et al,7 in their review of 123 cases, described the injury as a pedicle fracture of the C2 vertebra, and interestingly, they had only 6 cases with asymmetrical fractures.
Miligui, Ma, Xu and other authors have described traumatic spondylolisthesis of axis (hangman's fracture) as a fracture through the pars interarticularis of the axis.8–10
No studies so far (to the best of our knowledge) accurately describe the precise anatomical location and frequency of the fracture lines in this injury. Therefore, the objective of our study was to assess the anatomy of hangman's fracture with respect to location, pattern, extent and symmetry and to describe distinct fracture patterns that hopefully will replace the general [(neural arch fracture)] term. Consequently, proper understanding of fracture appearance and location may assist in planning the surgical treatment.
METHODS AND MATERIALS
The study project was approved by the institutional research and ethics committee.
Between June 2009 and January 2015, 41 cases of hangman's injuries were admitted to Khoula Hospital, a tertiary care trauma facility in Oman, Middle East. Complete imaging studies, including X-rays, CT scans and three-dimensional reconstructions, were available for 32 of these patients and these formed the cohort studied. There were 27 males and 5 females in this series and their age ranged from 28 to 54 years. All cases were omitted owing to road traffic accidents. For the purpose of this review, only pre-treatment lateral view X-rays, axial plane CT scans, sagittal and coronal plane reconstructions and three-dimensional reconstructed images were utilized. All CT images were acquired using a 64-slice multidetector CT scanner; the protocol used was 0.65 mm acquisition, axial sections with multiplanar reformatting into sagittal and coronal 2.5-mm images. All the images were studied by a Consultant Orthopaedic Surgeon and a Consultant Radiologist and consensus was obtained. The pars interarticularis and the pedicle of the axis vertebra as defined by Naderi et al11 were used for this study (Figures 1 and 2). Fractures extending into the laminae and the facet joint were documented. Fracture lines extending into the vertebral body was also documented.
Figure 1.
Serial CT slices of a normal C2 vertebra demonstrating the location of the pedicle (blue arrow) and pars interarticularis (red arrow). Sections are from cephalad to caudad end. (a) is at the level of the superior facet of the axis, (b) at the level of the body and (c) at the base of the inferior facet.
Figure 2.
Three-dimensional model of the axis vertebra depicting the exact location of the pedicle (marked by the green cross hatched area) and the pars interarticularis (marked by the red cross hatched area).
RESULTS
32 patients were enrolled in this study. 20 patients were found to have asymmetrical fracture lines while 12 patients showed symmetrical fracture lines.
The most common pattern noted was asymmetric injury with fracture pedicle on one side and pars on the other side (13 patients; 40%) (Figure 3).
Figure 3.
Two young males with hangman's fracture: (a) axial and (b) sagittal images for one patient and (c) axial image for another. Both cases show the most common injury pattern; asymmetric fracture line running through the pars on one side (red arrows) and the pedicle on the other (blue arrows).
For the symmetrical fractures, two patterns were identified:
–bilateral symmetric pedicle fracture (seven patients; 22%) which constituted the second most common pattern noted (Figure 4)
–bilateral symmetric pars fracture (five patients; 16%) (Figure 5).
Figure 4.
A 49-year-old male with hangman's fracture showing symmetric bilateral pedicle fractures (blue arrows) clearly seen on the axial image.
Figure 5.
A 23-year-old male with hangman's fracture. Sagittal and axial CT slices of a typical bilateral symmetric pars fracture (red arrows). Note that in the subaxial spine, the pedicle (white arrow) and pars (green arrow) are well delineated.
Other less frequent fracture patterns were asymmetrical in nature:
–asymmetric fracture involving pedicle on one side and vertebral body on the other side (two patients; 6%)
–asymmetric fracture involving pars on one side and vertebral body on the other side (three patients; 9%)
–asymmetric fracture involving the pedicle on one side and lamina on the other side (two patients; 6%).
Taking into consideration the two sides of C2 ring injury, we have got a total of 26 fracture lines that are primarily involving the pars (40%) and 31 fracture lines primarily involving the pedicles (49%).
Regarding the involvement of different parts of the vertebra, we have noticed the following:
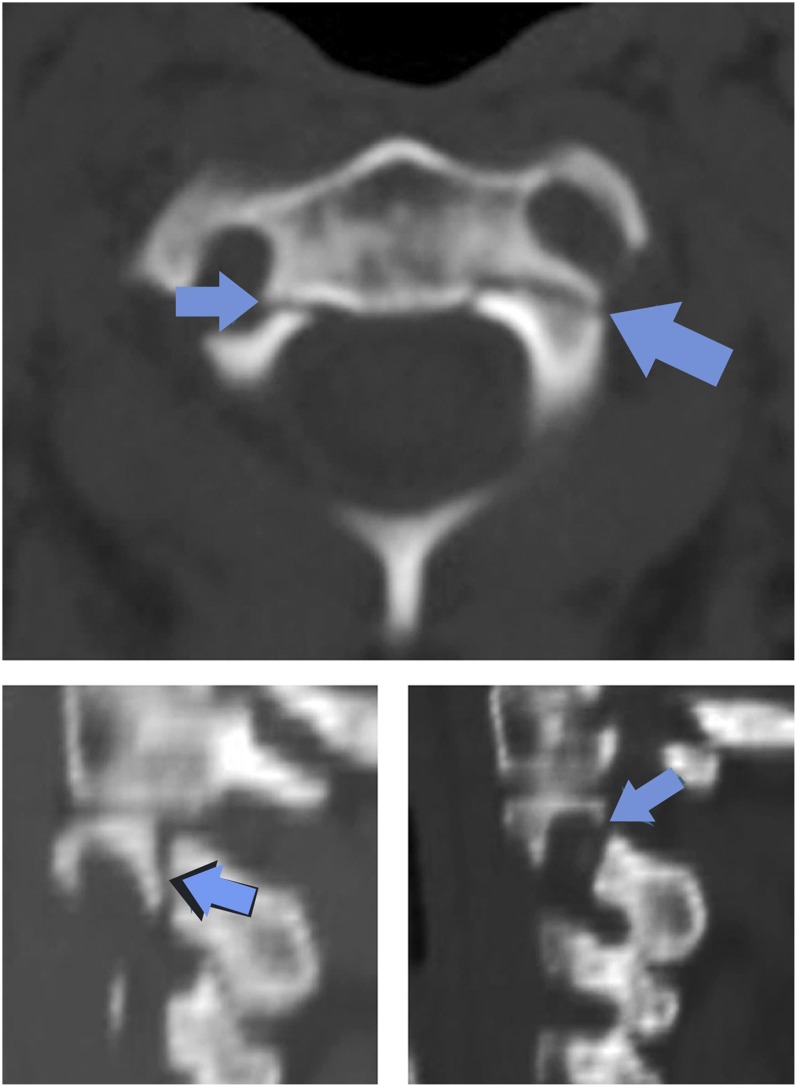
C2 facet joints were involved in 16 patients (50%), either superior (10 patients) or inferior (6 patients) (Figure 6).
The lamina was involved in only three patients (9%) with hangman's injury; one of them had ipsilateral pars fracture, and two had no fracture in the ipsilateral pedicle or pars therefore by itself constituted one side of the ring disruption.
Involvement of the posterior aspect of vertebral body (Figure 7) was noted in 15 patients (47%), 11 of them were in association with ipsilateral pedicle fracture, whereas in 4 patients, an isolated posterior vertebral body fractures comprised one side of the ring disruption with a fractured neural arch on the other side.
The foramen transversarium was involved in 18 patients (56%): 13 out of 20 asymmetric fractures and 5 out of 12 symmetrical fractures (Figure 8). 14 of them were associated with a pedicle fracture on the same side.
Figure 6.
A 41-year-old male with hangman's fracture showing a fracture line (blue arrows) passing through the superior facet.
Figure 7.
A 46-year-old male with hangman's fracture showing asymmetric fracture line involving the posterior third of the body of the vertebra (blue arrows).
Figure 8.
Two representative cases with hangman's fracture involving the foramen transversarium. (a) A 33-year-old female showing bilateral involvement by pedicle fractures (blue arrows). (b) A 28-year-old male showing unilateral foramen involvement by left pedicle fracture (blue arrow). Red arrow points to a contralateral pars fracture.
In our series, only two patients had neurological evidence of spinal cord injury for whom MRI was performed and confirmed the diagnosis. CT scan revealed bilateral symmetrical pars fractures involving foramen transversarium in one patient and asymmetrical pars and vertebral body fracture involving the facet joint and foramen transversarium in the other patient.
DISCUSSION
Since its first description, several authors tried to classify hangman's injury and correlate the different patterns with treatment options and clinical outcomes. Previous classification systems, however, were dependent primarily on the degree of instability, radiological displacement and mechanism of injury as in Effendi classification which was later modified by Levine and Edwards.2,5,7,12 There is a paucity of literature with respect to the anatomical features and involvement of variable vertebral elements in this type of injury.
At present, Effendi–Levine Edwards classification system is still the most widely used. This classification divides hangman's injury into four types:
Type I: <3-mm anterior displacement of C2, no angulation.
Type II: >3-mm anterior displacement and significant angulation.
Type IIa: significant angulation without anterior translation
Type III: bilateral facet joint dislocation.
It is also evident from literature that hangman's fractures have been differently described as pedicle, pars or neural arch fractures and that there is no agreement on whether they are most often symmetrical or not. The reason for this discrepancy is perhaps the non-standard nomenclature of the anatomical structures particularly with respect to the axis vertebra which is considered as atypical cervical vertebra.
In the typical subaxial cervical vertebra, it is easy to identify the pedicle which represents the junction of the neural arch and the body; and the pars which is the area between the superior and inferior facets (Figure 5). In contrast, the C2 has anatomical peculiarities that render accurate description of the fracture lines extremely challenging.
Several authors have described these anatomical peculiarities and tried to determine the precise location of the pedicle and pars of the C2 vertebra.11,13–17 In this study, we used Naderi criteria for identifying the pedicle and pars. Naderi et al believed that C2 isthmus (pars interarticularis) and the C2 pedicle are distinct structures. The pars is present between the superior and inferior articular processes covering the pedicle which is located beneath and is draped by C2 pars. Therefore, C2 pedicle can be seen on the inferior aspect of the vertebra. The pedicle connects posterior vertebral elements (lateral mass and inferior articular process) to the axial body.11
The authors of the current study have used the above anatomical features for defining the location of the fracture lines in hangman's injury (traumatic spondylolisthesis of axis). It must be noted that fractures often run from one region to the adjacent anatomical areas; yet for the sake of convenience, the region bearing the larger part of the fracture line is considered the primary site. For the purpose of this study, fracture lines that run from the pedicle or pars into the posterior third of the body are still considered as pedicular or pars fractures in contrast to pure body fractures in those without ipsilateral pedicle or pars injury (Figure 7).
In this study, different fracture patterns have been identified; the most common was found to be the asymmetric fracture involving pedicle on one side and the pars on the other (Figure 3). Asymmetry has been found to be the usual appearance in this study.
Several other fracture combinations were observed, the second common being bilateral symmetric pedicle fracture followed by bilateral symmetric pars fractures (Figures 4 and 5). Other patterns like those involving pedicle or pars on one side and vertebral body or lamina on the other were observed less frequently.
Furthermore, fracture extensions and involvement of variable vertebral elements were described and frequency of occurrence was determined. Extension of pedicle or pars fracture into the posterior vertebral body and a nearby facet (Figure 6) was a frequent observation in our series occurring in about half of cases.
The authors believe that this anatomical information can potentially aid surgical decision making in the management of hangman's cases. Most hangman's fractures are stable injuries and can be managed non-operatively though several authors have reported poor results with conservative care ranging from 9 to 32%.2,18 Li et al4 have suggested that Type IIa, and III lesions (those associated with significant angulation or facet disruption) are best treated by surgery. However, when surgery is indicated, the usual practice is to undertake C2-3 fixation and fusion through the anterior approach or trans-pedicular fixation of the C2 fracture. The question before us is whether pedicle fractures, pars fractures, body fractures, lamina fractures and facet fractures can all be treated by the same technique, as is currently advocated, or whether they need to be tailored according to the fracture pattern and location. We hope the information obtained in this study will help in deciding between different approaches and choices of surgery as well as instrumentation used.
Another interesting observation is the frequency of foramen transversarium involvement that was noted in more than half of our patients (Figure 8). However, none of those patients showed clinical or radiological evidence of vascular injury. Payabvash et al19 have demonstrated that blunt vertebral artery injury seen in this category of fractures in the upper cervical spine were associated with only 10% incidence of posterior circulation stroke. They also suggested that the presence of associated displaced fractures in the subaxial cervical spine was accompanied with more frequent circulatory symptoms. McKinney et al have reported approximately 15.5% vertebral artery injuries in fractures running through the foramen transversarium in the 71 cases they studied.20 Although no CT angiogram or MR angiograms were performed in our cases, CT revealed no haematoma or fat stranding in the region of vertebral artery to suggest its injury. Moreover, all the conscious and alert patients showed no clinical evidence of stroke nor did they demonstrate neurological deficits that could be explained by vascular injury.
There were only two patients in our series who had hangman's fracture extending to foramen transversarium and a concomitant head injury (both with diffuse axonal injury). They were evaluated and managed by the neurosurgical team and when last reviewed they showed no symptoms or signs of a cerebrovascular episode.
Theoretically, however, there is still a small possibility that one of those patients with foramen transversarium fracture having a subtle vascular injury which could be proven only by angiography. This aspect therefore needs further evaluation in future studies.
Review of the contemporary literature shows that most of hangman's injury cases were caused by road traffic accidents. Other causes include fall from a height and rarely diving accidents.2,4,21 Motor vehicle accidents were the sole cause of injury in our series of 32 patients. Whether a different mechanism of injury, with presence of rotational force, plays a role in our findings of high percentage of asymmetrical fractures, vertebral bodies and posterior elements involvement need to be confirmed by further studies.
Our series like the rest of previous literature shows relatively low incidence of neurological damage in hangman's injury.2,5,12,21 This observation can be well explained by the fact that the central canal diameter at upper cervical region is wide and typically tends to expand following neural arch fracture. Neurological deficit due to cord injury was seen in only two patients in our series that was proven by MRI. Whether there is any relation of the previously mentioned fracture patterns to presence of spinal cord injury cannot be inferred in the current study due to the small percentage of patients with neurological deficit and cord changes.
Correlation of fractures types to various MRI findings and the abnormalities noted in the soft tissues will be thoroughly explained in a separate study.
CONCLUSION
In our series of 32 patients presented with road traffic accidents, hangman's fracture is more commonly asymmetric with the most frequent pattern being pedicle fracture on one side and pars fracture on the other followed by symmetric pedicle and symmetric pars fractures. However, variable less frequent patterns were also observed, which involve the vertebral body and lamina in addition to pedicle and pars.
This study shows high incidence of facet joints and foramen transversarium involvement (>50%); however, none of the patients show definite evidence of vertebral artery injury neither clinically nor on imaging.
Fractures involving the posterior aspect of the vertebral body are very common, and as such, can constitute one side of the hangman's injury. However, it occurs in association with pedicle fracture in most of the cases.
The anatomical information presented in this study has the potential to modify the surgical treatment in hangman's injury.
Contributor Information
K Venugopal Menon, Email: kvm422@hotmail.com.
Sawsan Taif, Email: sawsantaif@gmail.com.
REFERENCES
- 1.Schneider RC, Livingston KE, Cave AJ, Hamilton G. “Hangman's fracture” of the cervical spine. J Neurosurg 1965; 22: 141–54. doi: 10.3171/jns.1965.22.2.0141 [DOI] [PubMed] [Google Scholar]
- 2.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg Br 1981; 63-B: 319–27. [DOI] [PubMed] [Google Scholar]
- 3.Duggal N, Chamberlain RH, Perez-Garza LE, Espinoza-Larios A, Sonntag VK, Crawford NR. Hangman's fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976). 2007; 32: 182–7. doi: 10.1097/01.brs.0000251917.83529.0b [DOI] [PubMed] [Google Scholar]
- 4.Li XF, Dai LY, Lu H, Chen XD. A systematic review of the management of hangman's fractures. Eur Spine J 2006; 15: 257–69. doi: 10.1007/s00586-005-0918-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Müller EJ, Wick M, Muhr G. Traumatic spondylolisthesis of the axis: treatment rationale based on the stability of the different fracture types. Eur Spine J 2000; 9: 123–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian W, Weng C, Liu B, Li Q, Hu L, Li ZY, et al. Posterior fixation and fusion of unstable hangman’s fractures by using intraoperative three dimensional fluoroscopy based navigation. Eur Spine J 2012; 21: 863–71. doi: 10.1007/s00586-011-2085-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Francis WR, Fielding JW, Hawkins RJ, Pepin J, Hensinger R. Traumatic spondylolisthesis of the axis. J Bone Joint Surg Br 1981; 63-B:313–18. [DOI] [PubMed] [Google Scholar]
- 8.ElMiligui Y, Koptan W, Emran I. Transpedicular screw fixation for type II hangman's fracture: a motion preserving procedure. Eur Spine J 2010; 19: 1299–305. doi: 10.1007/s00586-010-1401-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma W, Xu R, Liu J, Sun S, Zhao L, Hu Y. Posterior short-segment fixation and fusion in unstable hangman’s fracture. Spine 2011; 36: 529–33.doi: 10.1097/BRS.0b013e3181d60067 [DOI] [PubMed] [Google Scholar]
- 10.Xu H, Zhao J, Yuan J, Wang C. Anterior discectomy and fusion with internal fixation for unstable hangman's fracture. Int Orthop 2010; 34: 85–8. doi: 10.1007/s00264-008-0658-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naderi S, Arman C, Güvençer M, Korman E, Senoğlu M, Tetik S, et al. An anatomical study of the C2 pedicle. J Neurosurg Spine 2004; 1: 306–10. doi: 10.3171/spi.2004.1.3.0306 [DOI] [PubMed] [Google Scholar]
- 12.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985; 67: 217–26. [PubMed] [Google Scholar]
- 13.Ebraheim NA, Fow J, Xu R, Yeasting RA. The location of the pedicle and pars interarticularis in the axis. Spine (Phila Pa 1976) 2001; 26: E34–7. doi: 10.1097/00007632-200102150-00002 [DOI] [PubMed] [Google Scholar]
- 14.Howington JU, Kruse JJ, Awasthi D. Surgical anatomy of the C-2 pedicle. J Neurosurg 2001; 95(Suppl. 1): 88–92. [DOI] [PubMed] [Google Scholar]
- 15.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ. Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine (Phila Pa 1976) 2005; 30: 1519–23. doi: 10.1097/01.brs.0000168546.17788.49 [DOI] [PubMed] [Google Scholar]
- 16.Yuan F, Yang HL, Guo KJ, Li JS, Xu K, Zhang ZM, et al. A clinical morphologic study of the C2 pedicle and isthmus. Eur Spine J 2013; 22: 39–45. doi: 10.1007/s00586-012-2417-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bogduk N, Mercer S. Biomechanics of the cervical spine.1: normal kinematics. Clin Biomech (bristol, Avon) 2000; 15: 633–48. doi: 10.1016/S0268-0033(00)00034-6 [DOI] [PubMed] [Google Scholar]
- 18.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997; 22: 1843–52. [DOI] [PubMed] [Google Scholar]
- 19.Payabvash S, McKinney AM, McKinney ZJ, Palmer CS, Truwit CL. Screening and detection of blunt vertebral artery injury in patients with upper cervical fractures: the role of cervical CT and CT angiography. Eur J Radiol 2014; 83: 571–7. doi: 10.1016/j.ejrad.2013.11.020 [DOI] [PubMed] [Google Scholar]
- 20.McKinney A, Ott F, Short J, McKinney Z, Truwit C. Angiographic frequency of blunt cerebrovascular injury in patients with carotid canal or vertebral foramen fractures on multidetector CT. Eur J Radiol 2007; 62: 385–93. doi: 10.1016/j.ejrad.2007.01.008 [DOI] [PubMed] [Google Scholar]
- 21.Ferro FP, Borgo GD, Letaif OB, Cristante AF, Marcon RM, Lutaka AS. Traumatic spondylolisthesis of the axis: epidemiology, management and outcome. Acta Ortop Bras 2012; 20: 84–7. doi: 10.1590/S1413-78522012000200005 [DOI] [PMC free article] [PubMed] [Google Scholar]