Abstract
The clinical application of sentinel node biopsies in early gastric cancer is still controversial even though it appears promising. This study was conducted as a prerequisite quality control for surgical standardization of laparoscopic sentinel basin dissection (SBD) prior to the initiation of a phase III trial.
Laparoscopic SBD was performed in patients with preoperative stage T1-2N0 and tumor size <4 cm in diameter. Intraoperative endoscopic submucosal injection of a standardized dual tracer was administered. All retrieved sentinel basin nodes (SBN) were investigated with intraoperative frozen hematoxylin and eosin (H&E) staining. A strict checklist consisting of 7 essential steps was followed during laparoscopic SBD as the quality control study for a phase III trial. Completion of all essential steps in the checklist for 10 cases was used to define a qualified institution.
Seven institutions participated and 112 patients were enrolled in this study. However, 4 patients were excluded owing to screening failure. The mean number of cases required for institutional qualification was 15 cases (range, 13–20 cases). Sentinel basins (SB) were detected and dissected in 100 of the 108 patients (92.6%); the median number of SB and SBN was 2 and 7, respectively. Lymph node metastases were detected in 10 patients by postoperative permanent H&E staining and they were detected by SBD in all 10 patients. Frozen results of SBN were compatible with permanent staining reports.
Laparoscopic SBD is feasible and demonstrated improved sensitivity in detecting metastatic lymph nodes compared to the previous study. A future phase III randomized trial comparing laparoscopic SBD with organ-preserving gastrectomy and laparoscopic standard gastrectomy seems promising for qualified institutions.
INTRODUCTION
Over the last decade, the proportion of early gastric cancer (EGC) among gastric cancer patients has markedly increased in Korea.1 The nationwide screening program, which has been implemented since 1999 due to the high prevalence of gastric cancer, seems to have largely influenced the trend toward early detection and improved overall survival in gastric cancer patients in Korea.2 As life expectancy became longer after curative surgery in EGC patients, the long-term quality of life of these patients became an important issue. There have been attempts to minimize surgical invasiveness, reduce the surgical extent of standard radical gastrectomy, and preserve remnant gastric function, unless these impair the survival of the patients.
One of these attempts is sentinel node (SN) navigation surgery. The SN concept was first introduced in penile cancer by Cabanas in 1977 and was then developed in melanoma by Morton et al in 1992.3,4 Since then, it has been well investigated and adopted in melanoma and breast cancer, allowing a reduction in the extent of surgical intervention with limited lymph node dissection.5,6 However, the clinical application of SN biopsy in EGC has long been debated due to the complicated lymphatic flow around the stomach and the inconsistent results with somewhat unsatisfactory sensitivity reported by previously published studies.7,8 However, a recent multicenter trial from Japan showed quite promising results with a low false-negative rate of SN biopsy in early-staged gastric cancer patients.9 Based on these results, the Korean Surgical Society planned a multicenter phase III trial comparing conventional laparoscopic gastrectomy to laparoscopic SN biopsy with organ-preserving surgery in patients with clinical stage IA gastric cancer: the trial is currently underway (NCT01804998).10
In multicenter trials associated with surgical procedures, quality control of the participating institution is essential to achieve optimal outcomes. The present quality control study was conducted as a prerequisite for the phase III trial by all participating institutions (NCT01544413).11 This study aimed to qualify the participating institutions for standardization of their surgical procedures before the phase III trial and also to evaluate the completion of the step-by-step procedure, learning curve, and feasibility of laparoscopic SN biopsy in gastric cancer patients.
PATIENTS AND METHODS
Patients
Patients with histologically confirmed adenocarcinoma in the stomach having clinical stage T1-2N0M0 according to the American Joint Committee on Cancer (AJCC) 7th edition were considered for inclusion in the present study.12 The clinical stage was determined by preoperative endoscopy and abdominal computed tomography and/or endoscopic ultrasound (EUS); EUS was not routinely performed in all patients enrolled in the present study. Additional preoperative eligibility criteria for the present study included the following: a tumor of <4 cm in the longest diameter under endoscopic measurement; a tumor at least 2 cm from the pylorus or cardia; and age of 20 to 80 years. Patients with tumors satisfying absolute indications for endoscopic resection were excluded from the study. Pregnant patients and patients with a history of drug-related anaphylactic reaction, prior upper abdominal surgery except for laparoscopic cholecystectomy, or radiation therapy were also excluded.
Seven institutions participated in this multicenter prospective quality control study. All patients enrolled in this study were preoperatively registered in a central data center (eVelos System; Velos, Inc., Fremont, CA). All patients provided written informed consent before the surgery. This study was approved by the local institutional review boards of all participating institutions.
Procedures for SBD
A mixture of indocyanine green (IGC; Diagnogreen®, Daiichi-Sankyo Co., Ltd., Tokyo, Japan; 2 mL, 5 mg) and radiolabeled human serum albumin (Tc99m-HSA; 2 mL, 0.1 mCi/mL) was used as a tracer to detect the SNs. HSA was uniformly prepared at the study center; the quality of HSA was checked with limulus amoebocyte lysate assay and bacterial test. The particle size and radiolabeling efficiency was also verified. The tracer separately prepared at the study center was delivered to the participating institutions. HSA was radiolabeled and then mixed with ICG solution at the department of nuclear medicine at each institution on the day of surgery before the endoscopic procedure. A 4 mL volume of the dual tracer was injected into the submucosal layer in 4 quadrants of the primary tumor (1 mL at each quadrant) via an intraoperative endoscopic approach. After 15 min of the endoscopic tracer injection, stained lymphatics, and lymph nodes were identified. At the same time, the hand held laparoscopic gamma probe was used to detect the radioactive SNs. The sentinel basins (SBs) containing sentinel nodes (green or hot) were carefully dissected and retrieved from the surgical field.13–15
The harvested SBs were dissected to isolate lymph nodes at a back-table located in the operating room. Lymph nodes stained in green were defined as green nodes (GNs) and those with radioactivity of 10 times or more than background were defined as hot nodes (HNs). Lymph nodes retrieved from the SBs but neither green nor hot were defined as basin nodes (BNs). All the isolated lymph nodes from the SBs, defined as sentinel basin nodes (SBNs), were classified into HN, GN, both hot and green nodes (HGN), and BN, labeled with the respective lymph node station numbers, and sent to the pathologist for intraoperative frozen section.
After sentinel basin dissection (SBD), standard gastrectomy with lymphadenectomy of D1+ or more was carried out in all patients according to the Japanese gastric cancer treatment guidelines.16
Intraoperative Histologic Examination for SBNs and Permanent Pathologic Examination
The harvested nodes from the SBs were histologically examined intraoperatively by hematoxylin and eosin (H&E) staining using 1 representative cut plane of a frozen section.
After the conventional surgery was completed, the remaining lymph nodes were classified into each lymph node station according to the anatomical definition of the Japanese guidelines and sent for permanent pathologic examination by H&E staining.17
Checklist and Definition of Qualified Institutions
The protocol was provided under the format of a checklist consisting of 7 critical steps to assess the adequacy of the procedure to be performed by endoscopists, surgeons, and pathologists (Table 1). Success was defined as the accurate execution of all 7 steps.
TABLE 1.
Checklist for the Quality Control of the Participating Institution
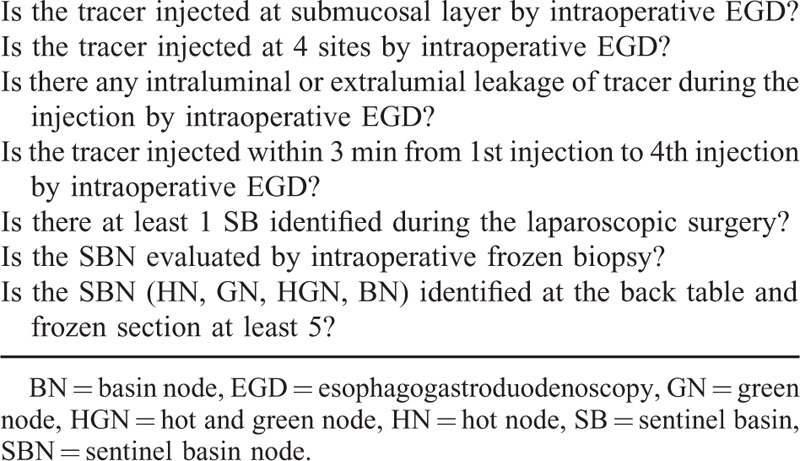
According to the previously published study from our institution, the learning period for SN mapping was estimated to be 26 cases to achieve a 95% success rate in cumulative sum analysis; the surgeons in the study succeeded in detecting sentinel lymph nodes in 84.6% of the cases during the learning period.18 Given that all participants, that is, the endoscopist, surgeon, and pathologist, are required to complete their own steps in the checklist to achieve “success” in the present study, the success rate of completing all 7 steps is estimated to be 31.0% applying a 84.6% success rate for each step. Therefore, success in a minimum of 10 cases at each institution was considered to be sufficient to surpass the initial learning curve and quality control of sentinel node navigation surgery for gastric cancer in the present study, qualifying the institution to participate in the upcoming phase III trial.10
Interim Analysis
The interim analysis was planned at the time point when 10 patients were enrolled at each institution to evaluate the safety of additional SBD in terms of postoperative complication occurrence compared to the standard surgery. The decision to continue the study was made at the investigators meeting based on the results of the interim safety analysis.
Study Assessment
The primary endpoint was to evaluate the performance of SBD, which was assessed by successful implementation of the checklist. The secondary endpoints were to calculate the detection rate of SBs and SBNs and the sensitivity and false-negative rate of the SBD in identifying metastatic lymph nodes.
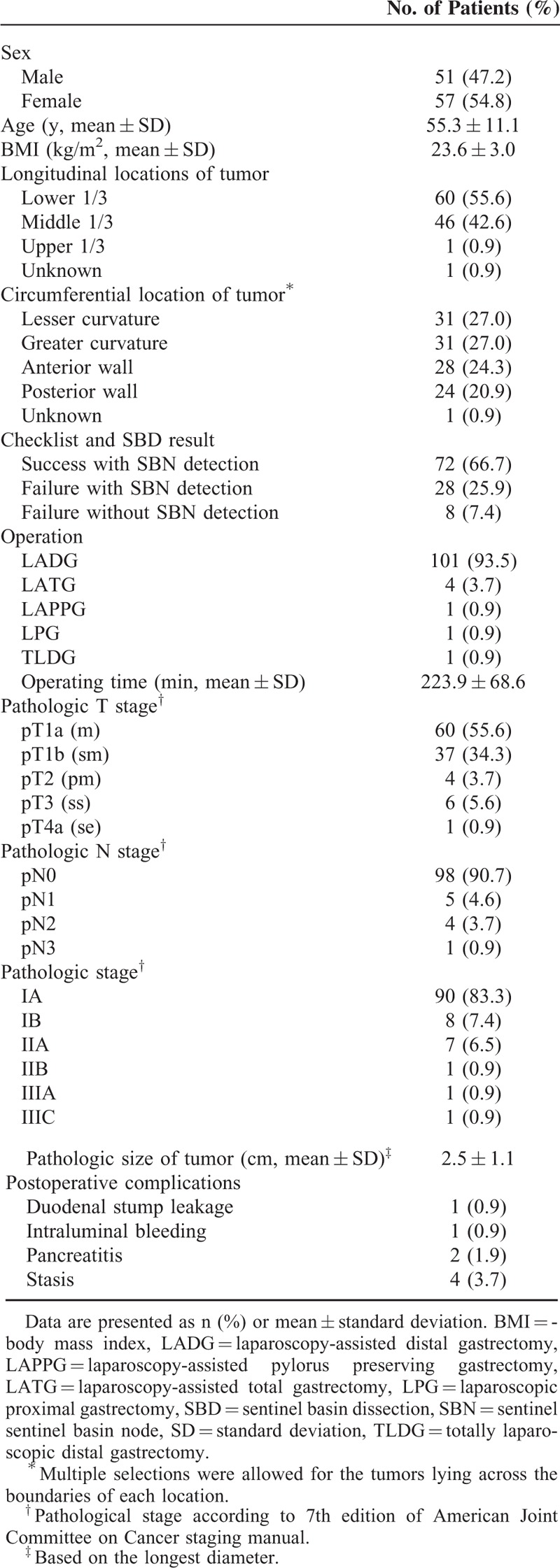
Sensitivity and false-negative rate were defined as follows:
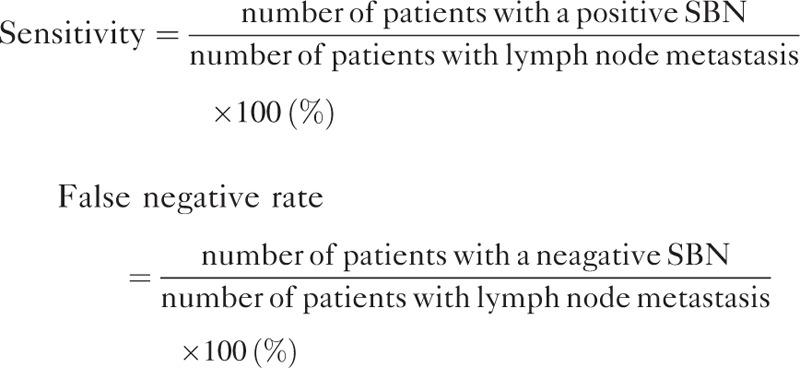 |
In addition, positive- and negative-predictive values were calculated to evaluate the predictability of non-SBN metastasis in SBN-positive patients.
 |
RESULTS
The present quality control study was conducted in 7 participating institutions from April 2012 to September 2014; 112 patients were preoperatively enrolled. Interim analyses midway through the study revealed that the study protocol did not jeopardize the safety of the enrolled patients and the study was continued thereafter. Four patients were excluded from the study because of screening failure (2 patients withdrew after enrolment, 1 double primary cancer, 1 poor bowel preparation for intraoperative endoscopic procedure), which left 108 patients eligible for the final analyses.
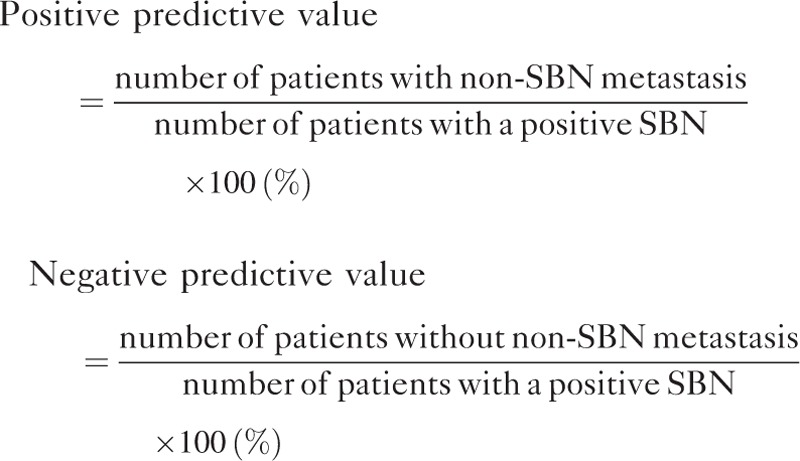
Laparoscopy-assisted distal gastrectomy was the most commonly performed surgical procedure after SBD (101/108, 93.5%) (Table 2). Eight patients (7.4%) experienced postoperative complications in the early postoperative period (<30 days), but none were directly related to the additional procedure of SBD.
TABLE 2.
Clinicopathologic Characteristics of the Patients (n = 108)
The mean number of cases required for institutional qualification was 15 cases (range, 13–20) and success was achieved in 72 out of 108 patients (66.7%) (Fig. 1). The process of patient enrolment and the time frame to complete the quality control study at each institution are schematized in Figure 1.
FIGURE 1.
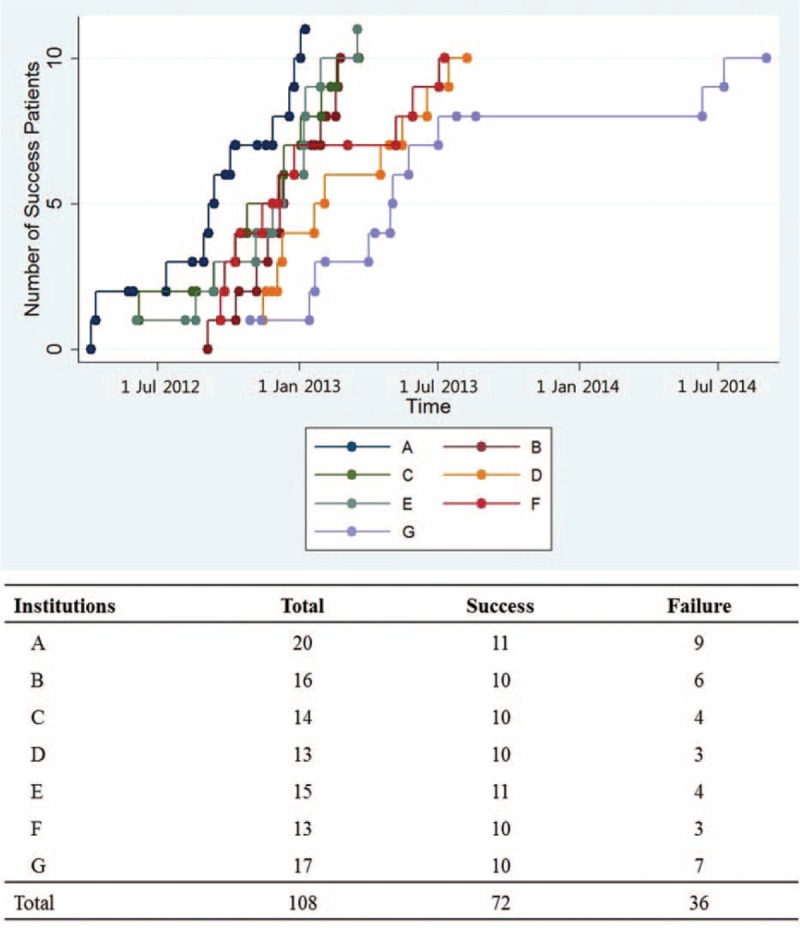
The time frame and the number of cases required to complete the quality control study at each institution.
SBs were detected and dissected in 100 of 108 patients (detection rate, 92.6%) whether they were designated as a success or not. These included 72 cases of success and additional 28 cases of failure with respect to the checklist completion. All the harvested SBs from these patients were subjected to further analyses to evaluate the characteristics of the SNs. The most frequently detected SB was station no. 3 (n = 64), followed by no. 4d (n = 43) (Table 3). Forty-one patients (41.0%) had 1 SB, 50 (50.0%) had 2, and 9 (9.0%) had 3 SBs. The median number of retrieved SBs was 2 (interquartile range [IQR], 1–2) overall.
TABLE 3.
Frequency of the Harvested Sentinel Basins at Each Nodal Station and the Mean Number of Identified Sentinel Basin Nodes Among the Patients Whose Sentinel Basins Were Detected (n = 100)
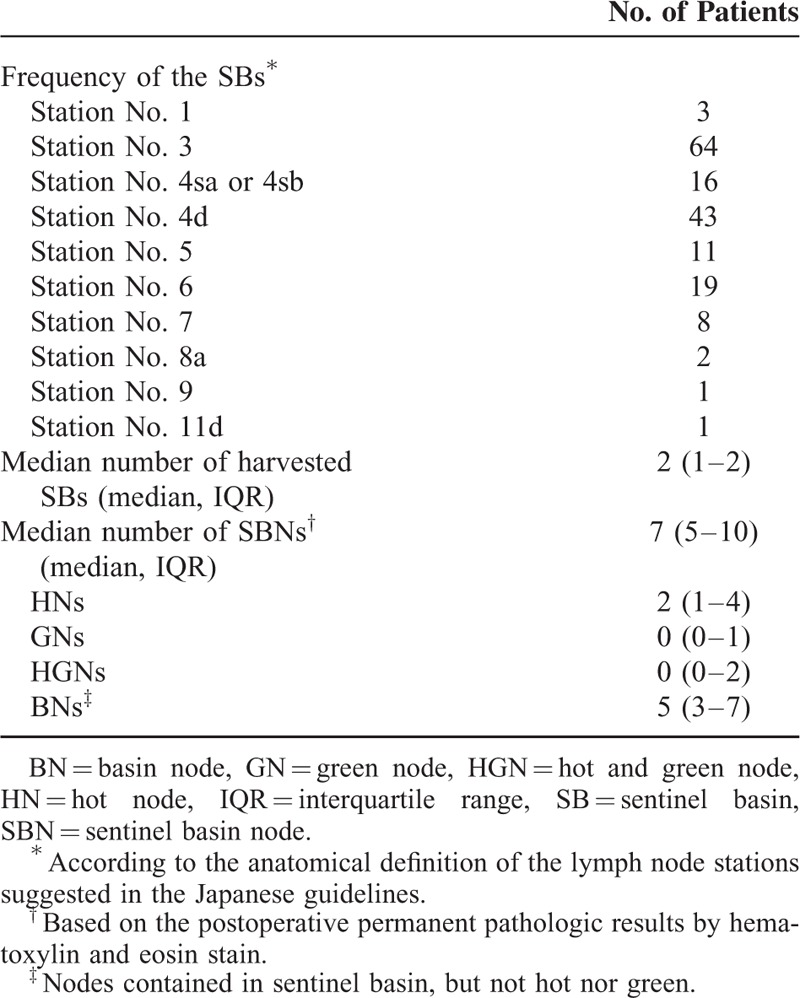
The median number of SBNs examined at the back-table was 9 (IQR, 6–12). However, there was some difference in the actual number of identified SBNs by the permanent pathologic examination and the number tended to be smaller (median, IQR; 7, 5–7) (Table 3). More than half were BNs (54.1%), while HNs (28.7%) were the most prevalent among the true SNs based on the permanent pathology test.
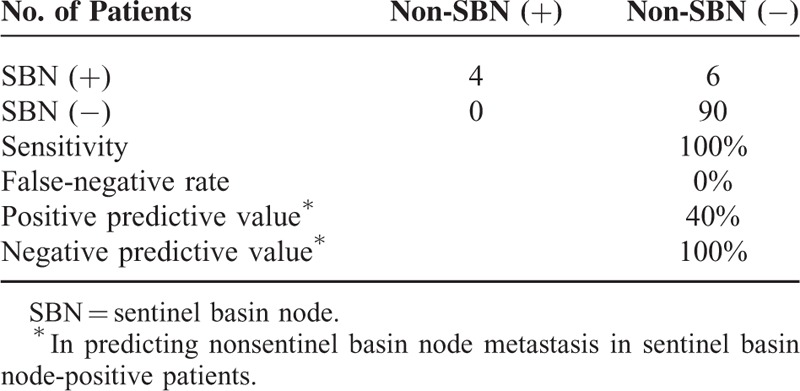
Ten patients (9.3%) had lymph node metastasis at permanent pathologic examination by H&E staining. There were no patients with metastasis in non-SBNs alone without metastatic SBs nodes according to the final pathologic results, which indicated 100% and 0% sensitivity and false-negative rate of SBD, respectively (Table 4). In 3 patients, the metastatic lymph nodes were neither hot nor green but confined to the SBs. The positive predictive value of SBD was 40.0% for the metastasis in non-SBs in patients with positive SBNs.
TABLE 4.
Evaluation of the Sentinel Basins and Nonsentinel Basins by Postoperative Pathologic Examination With Hematoxylin and Eosin Stain (n = 100)
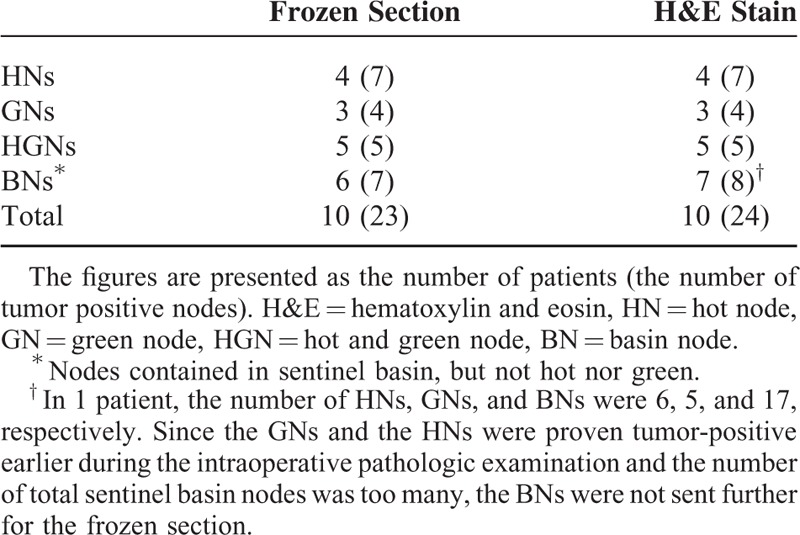
Lymph node metastasis was detected by intraoperative frozen section in 10 patients (Table 5). No patients were proven to have metastatic node on permanent H&E examination after negative findings on frozen sections and vice versa. Based on these results, the method of intraoperative pathologic examination used in the present study had an accuracy rate of 100.0% in terms of detecting metastatic lymph node when compared to the permanent pathologic results by H&E staining.
TABLE 5.
Number of Patients With Metastatic Sentinel Basin Nodes
DISCUSSION
The present study demonstrated that the quality control for surgical standardization of laparoscopic SBD could be achieved after experience with an average of 15 cases. Based on the detection rate and the sensitivity of this quality control study, laparoscopic SN navigation surgery using SBD is technically feasible and can be safely applied in the upcoming phase III clinical trial.10
The checklist used in the present study consisted of 7 items describing mandatory requirements for performing the SBD. The details of the checklist were established via comprehensive discussion among participating investigators. The checklist not only involves surgeons but also demands that endoscopists and pathologists follow specific steps during the procedure; 4 items are directly related to the endoscopic procedures; 2, to surgeons; and 2, to pathologists. This indicates that close cooperation among these participants is essential to complete the checklist, which will be required in the subsequent phase III clinical trial to achieve optimal outcomes from SBD in gastric cancer.
The number of cases required for quality control in the present study was on average 15 due to the reduced failure rate, which was below the estimated number based on the 26 cases of the learning curve in the previous report.18 Plausible reasons could include: prior experience with SN biopsy in gastric cancer at most of the participating institutions,13,19–21 repeated review of the instructional video, in-depth discussion of the lessons learned through trial and error in prior experience, and expertise in laparoscopic surgery of all the participating surgeons. Nonetheless, the accuracy and the sensitivity of SBD appeared to be acceptable in the present study indicating that the SBD is feasible as long as the participants adequately comply with the details of each step in the checklist.
Several factors appeared to influence the surgical performance of SBD in the present study. The primary tumors located at the lesser curvature were usually more difficult to deal with than those at the greater curvature. It might be attributable to more complicated lymphatic drainage and vascular structures; the tracers sometimes spread diffusely and quickly to the second tier nodal stations causing difficulties in determining the exact range of SBs. SBs in lesser curvature were also subjected to frequent bleeding during surgery due to abundant blood supply. Tumors near the pyloric ring or esophagogastric junction were tricky to handle because it is easy to damage major nerve branches during SBD.
The dual tracer of dye and radioisotope is known to provide high detection rate of SNs and better sensitivity than the dye-guided method.22,23 The dye washes out and flows into the second tier nodes quickly because it is small in size and water soluble; this, however, makes it difficult to identify GNs at the back-table. The present study also showed that a very small number of true GNs remained after back-table dissection. It is particularly difficult to directly visualize stained nodes in a deep-seated area, particularly in patients with visceral obesity. The radioisotope serves as a supplementary measure to compensate for the low retention rate and poor visibility of the dye method. Although radiolabeled tin colloid has been used in most studies regarding SN biopsy in gastric cancer, the relatively large particle size resulted in slow migration and a redundant endoscopic procedure was required before surgery.9 The small particle-sized HSA (2–3 nm) used in the present study served as an ideal tracer to be applied during the surgery simultaneously with ICG. HSA is very stable, readily available, and biodegradable and with reduced potential for allergic reactions.14,24,25 The use of the dual tracer resulted in a 92.6% detection rate of SBs in the present study, which is within the range of reported rates of 91.2% to 97.5% in previous studies using dual tracer methods.9,13,22 Since the present study included cases during the learning period, the SB detection is expected to further improve in future studies.
Miyashiro et al reported a high false-negative rate in the Japanese multicenter trial (JCOG0302 trial) that was a result of the unreliability of the frozen section examinations using only a single plane.26 Nonetheless, the present study demonstrated a 100% accuracy rate of intraoperative H&E staining using bivalve frozen sections. All patients with lymph node metastasis by permanent H&E stain were identified by intraoperative pathologic diagnosis using H&E stain on bivalve frozen sections. However, 1 participating institution routinely performed immunohistochemistry (IHC) with cytokeratin for gastric cancer patients in parallel with the appointed protocol in the present study. The additional IHC revealed that 1 patient with submucosal cancer had micrometastasis in 1 of the HNs that was not detected by H&E staining (Fig. 2) and there were no additional lymph nodes with evidence of metastasis. Thus, is it truly necessary to adopt more precise intraoperative diagnostic methods, such as step section analysis, rapid IHC, or real-time reverse transcriptase polymerase chain reaction, for SN navigation surgery for gastric cancer? In the ordinary clinical setting, these appear to be neither clinically practical nor universally feasible, and furthermore, costly and time consuming. Some investigators suggested the application of SBD instead of pick-up biopsy of individual SNs.13,15 Kitagawa et al revealed that all patients with a false-negative intraoperative pathologic diagnosis proved to have metastatic spread confined to the SNs per se or within the SBs.9 The present study also showed consistent results demonstrating that all patients with node metastasis were successfully identified by adopting the SBD method because positive nodes were present within the SBs even in those without HN or GN involvement. Although the number of relevant cases in the present study was very small due to the low incidence of lymph node metastasis in EGC, this indicates that SBD instead of pick-up biopsy can compensate for an incomplete intraoperative pathologic examination. Even if a true metastatic node were falsely diagnosed as negative intraoperatively, the node would have been already cleared during SBD and, consequently, would not have any critical influence on the disease-free survival of the patient. However, long-term results with disease-free survival need to be investigated in well-designed studies in the future.
FIGURE 2.
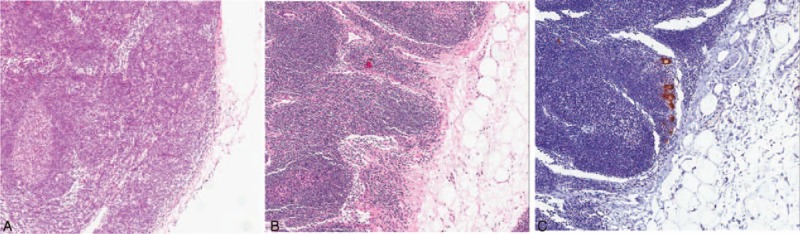
Microscopic view of the micrometastatic lymph node detected by additional immunohistochemistry (IHC) with cytokeratin. (A) Frozen section with hematoxylin and eosin (H&E) staining, (B) permanent pathology by H&E stain, and (C) IHC with cytokeratin.
The risk of skip metastasis seems to be very low in EGC given the results of the present study demonstrating 0% detection of metastasis in non-SBs node alone with no metastatic SBs nodes. In previously published literature, tumor size was reported to be closely related to the presence of skip metastasis in EGC patients.27,28 Tumor size is also important in the control of primary tumor during SN navigation surgery to secure safe margins, as the accuracy in measurement of tumor size generally decreases in larger tumors.29 Therefore, the indications for SN navigation surgery should be limited to small-sized tumors and it should be strictly respected in the upcoming phase III clinical trial to minimize the false-negative rate and insufficient treatment. Nonetheless, the relatively high positive predictive value in the present study suggests that cancer-positive SBNs are strongly suggestive of the probability of non-SB involvement even in EGC patients. When the intraoperative pathologic examination reveals the presence of metastasis in SBNs, standard radical lymph node dissection is imperative in order to prevent the risk of not eliminating metastatic lymph nodes.
The present quality control study has shown that laparoscopic SBD is feasible and applicable in EGC patients with improved sensitivity compared with previous studies. This study has provided a basis for the planned phase III randomized trial comparing laparoscopic SBD with organ-preserving gastrectomy to conventional laparoscopic distal or total gastrectomy for qualified institutions. The future phase III trial is expected to corroborate the oncologic safety as well as the clinical benefit of organ-preserving gastrectomy with SBD in terms of quality of life in EGC patients.
Footnotes
Abbreviations: AJCC = American Joint Committee on Cancer, BN = basin node, CT = computed tomography, EGC = early gastric cancer, EUS = endoscopic ultrasound, GN = green node, H & E = hematoxylin and eosin, HGN = hot and green node, HN = hot node, HSA = human serum albumin, ICG = indocyanine green, IHC = immunohistochemistry, IQR = interquartile range, SB = sentinel basin, SBD = sentinel basin dissection, SBN = sentinel basin node, SN = sentinel node.
Drs YJL, SHJ, S-UH, JSM, JYA, GSC, GAJ, OJ, YKP, MRJ, Y-WK, HMY, BWE, JYP, and KWR have no financial interests to disclose. Dr HH is receiving research funds from Dong-A SCIO Holding, Hanmi Pharma. Co., and Daewoong Pharm. Co., and Dr. Hyung WJ reported to have a paid advisory role for Ethicon.
This research was supported by the National Cancer Center, Republic of Korea (Grant 1410140-1).
The authors report no conflicts of interest.
REFERENCES
- 1.Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer 2011; 11:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung K-W, Won Y-J, Kong H-J, et al. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat 2013; 45:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992; 127:392–399. [DOI] [PubMed] [Google Scholar]
- 4.Cabanas RM. An approach for the treatment of penile carcinoma. Cancer 1977; 39:456–466. [DOI] [PubMed] [Google Scholar]
- 5.Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med 2003; 349:546–553. [DOI] [PubMed] [Google Scholar]
- 6.Morton DL, Thompson JF, Essner R, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: a multicenter trial. Ann Surg 1999; 230:453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryu KW, Eom BW, Nam BH, et al. Is the sentinel node biopsy clinically applicable for limited lymphadenectomy and modified gastric resection in gastric cancer? A meta-analysis of feasibility studies. J Surg Oncol 2011; 104:578–584. [DOI] [PubMed] [Google Scholar]
- 8.Kitagawa Y, Fujii H, Kumai K, et al. Recent advances in sentinel node navigation for gastric cancer: a paradigm shift of surgical management. J Surg Oncol 2005; 90:147–151. [DOI] [PubMed] [Google Scholar]
- 9.Kitagawa Y, Takeuchi H, Takagi Y, et al. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol 2013; 31:3704–3710. [DOI] [PubMed] [Google Scholar]
- 10.Ryu KW. Multicenter phase III trial of laparoscopic sentinel node biopsy and stomach preserving surgery in early gastric cancer. March 2013; https://www.clinicaltrials.gov/ct2/show/NCT01804998 Accessed March 19, 2015. [Google Scholar]
- 11.Ryu KW. Quality control study for multicenter phase III trial of laparoscopic sentinel node biopsy and stomach preserving surgery in early gastric cancer. https://www.clinicaltrials.gov/ct2/show/NCT01544413 Accessed March 19, 2015. [Google Scholar]
- 12.Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol 2010; 17:3077–3079. [DOI] [PubMed] [Google Scholar]
- 13.Lee YJ, Ha WS, Park ST, et al. Which biopsy method is more suitable between a basin dissection and pick-up biopsy for sentinel nodes in laparoscopic sentinel-node navigation surgery (LSNNS) for gastric cancer? J Laparoendosc Adv Surg Tech A 2008; 18:357–363. [DOI] [PubMed] [Google Scholar]
- 14.Lee JH, Ryu KW, Kook MC, et al. Feasibility of laparoscopic sentinel basin dissection for limited resection in early gastric cancer. J Surg Oncol 2008; 98:331–335. [DOI] [PubMed] [Google Scholar]
- 15.Miwa K, Kinami S, Taniguchi K, et al. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br J Surg 2003; 90:178–182. [DOI] [PubMed] [Google Scholar]
- 16.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011; 14:113–123. [DOI] [PubMed] [Google Scholar]
- 17.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–112. [DOI] [PubMed] [Google Scholar]
- 18.Lee JH, Ryu KW, Lee SE, et al. Learning curve for identification of sentinel lymph node based on a cumulative sum analysis in gastric cancer. Dig Surg 2009; 26:465–470. [DOI] [PubMed] [Google Scholar]
- 19.Lee JH, Ryu KW, Nam BH, et al. Factors associated with detection failure and false-negative sentinel node biopsy findings in gastric cancer: results of prospective single center trials. J Surg Oncol 2009; 99:137–142. [DOI] [PubMed] [Google Scholar]
- 20.Hur H, Lim SG, Byun C, et al. Laparoscopy-assisted endoscopic full-thickness resection with basin lymphadenectomy based on sentinel lymph nodes for early gastric cancer. J Am Coll Surg 2014; 219:e29–e37. [DOI] [PubMed] [Google Scholar]
- 21.Hyung WJ, Kim YS, Lim JS, et al. Preoperative imaging of sentinel lymph nodes in gastric cancer using CT lymphography. Yonsei Med J 2010; 51:407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Park do J, Kim HH, Park YS, et al. Simultaneous indocyanine green and (99m)Tc-antimony sulfur colloid-guided laparoscopic sentinel basin dissection for gastric cancer. Ann Surg Oncol 2011; 18:160–165. [DOI] [PubMed] [Google Scholar]
- 23.Hayashi H, Ochiai T, Mori M, et al. Sentinel lymph node mapping for gastric cancer using a dual procedure with dye- and gamma probe-guided techniques. J Am Coll Surg 2003; 196:68–74. [DOI] [PubMed] [Google Scholar]
- 24.Wilhelm AJ, Mijnhout GS, Franssen EJ. Radiopharmaceuticals in sentinel lymph-node detection—an overview. Eur J Nucl Med 1999; 26:S36–S42. [DOI] [PubMed] [Google Scholar]
- 25.Bedrosian I, Scheff AM, Mick R, et al. 99mTc-human serum albumin: an effective radiotracer for identifying sentinel lymph nodes in melanoma. J Nucl Med 1999; 40:1143–1148. [PubMed] [Google Scholar]
- 26.Miyashiro I, Hiratsuka M, Sasako M, et al. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer 2014; 17:316–323. [DOI] [PubMed] [Google Scholar]
- 27.Lee SE, Lee JH, Ryu KW, et al. Sentinel node mapping and skip metastases in patients with early gastric cancer. Ann Surg Oncol 2009; 16:603–608. [DOI] [PubMed] [Google Scholar]
- 28.Son SY, Park JY, Ryu KW, et al. The risk factors for lymph node metastasis in early gastric cancer patients who underwent endoscopic resection: is the minimal lymph node dissection applicable? A retrospective study. Surg Endosc 2013; 27:3247–3253. [DOI] [PubMed] [Google Scholar]
- 29.Park JY, Ryu KW, Eom BW, et al. Proposal of the surgical options for primary tumor control during sentinel node navigation surgery based on the discrepancy between preoperative and postoperative early gastric cancer diagnoses. Ann Surg Oncol 2014; 21:1123–1129. [DOI] [PubMed] [Google Scholar]


