Supplemental Digital Content is available in the text
Abstract
The exact mechanisms of hypertension contributing to atherosclerosis have not been fully elucidated. Although multiple studies have clarified the association with low-density lipoprotein (LDL) subfractions, uncertainty remains about its relationship with high-density lipoprotein (HDL) subfractions. Therefore, we aimed to comprehensively determine the relationship between distribution of HDL subfractions and hypertensive status.
A total of 953 consecutive subjects without previous lipid-lowering drug treatment were enrolled and were categorized based on hypertension history (with hypertension [n = 550] or without hypertension [n = 403]). Baseline clinical and laboratory data were collected. HDL separation was performed using the Lipoprint System.
Plasma large HDL-cholesterol (HDL-C) and large HDL percentage were dramatically lower whereas the small HDL-C and small HDL percentage were higher in patients with hypertension (all P < 0.05). The antihypertensive drug therapy was not associated with large or small HDL subfractions (on treatment vs not on treatment, P > 0.05; combination vs single drug therapy, P > 0.05). However, the blood pressure well-controlled patients have significantly lower small HDL subfraction (P < 0.05). Moreover, large HDL-C and percentage were inversely whereas small HDL percentage was positively associated with incident hypertension after adjusting potential confounders (all P < 0.05). In the multivariate model conducted in patients with and without hypertension separately, the cardio-protective value of large HDL-C was disappeared in patients with hypertension (OR 95%CI: 1.011 [0.974–1.049]).
The distribution of HDL subfractions is closely associated with hypertensive status and hypertension may potentially impact the cardio-protective value of large HDL subfraction.
INTRODUCTION
Hypertension is a crucial independent risk factor for coronary artery disease (CAD) for all populations. According to the epidemiological reports, nearly one-fourth of the adult in the United States has hypertension based on the current definition.1 In the Chinese population, the prevalence of hypertension is also increased sharply in recent years, reaching a prevalence of 34% in 2010.2 Currently, hypertension has become a major public health issue in the world. However, the exact mechanisms contributing to atherosclerosis have not been fully elucidated.
Atherosclerosis, the precursor of CAD, is a very complex and multifactorial process. Besides the widely recognized inflammatory background, there is growing evidence suggesting an immunologic status,3 especially the links between allergy and vascular or thrombotic disorders 4 as well as the mammalian target of rapamycin (mTOR) pathway, 5 also play important roles in the progression of atherosclerosis. Although these new evidences have been proposed, current perspectives still regard dyslipidemia as the leading cause of atherosclerosis. Actually, hypertension often clusters with dyslipidemia, such as higher concentrations of low-density lipoprotein (LDL)-cholesterol (LDL-C) or lower high-density lipoprotein (HDL)-cholesterol (HDL-C),6–8 which have been supposed as major mediators of atherosclerosis. Recently, lipoprotein subfractions have been proposed to be more accurately capture the atherogenic properties than the concentrations of cholesterol contained in lipoproteins.9,10 During the past decades, the relationship between hypertension and LDL subfractions, especially with the small dense LDL or the particle size, has been reported by multiple clinical studies.11–13 It has, hence, suggested that hypertension may contribute to atherosclerosis with associated risk factors that influence LDL subfractions and particle size. In fact, HDL particle is more heterogeneous in its size and composition than LDL.14 However, few studies investigated the association of hypertension with HDL subfractions till now. Although it has been reported that small HDL particles had greater risk, whereas large HDL particles had lower risk of incident hypertension during 8 years follow-up,15 the study was conducted in initially healthy women and could not representative of the whole population. In addition, no data is currently available regarding the relationship between HDL subfractions and hypertensive status till now.
Thus, the present study was initiated to comprehensively test the association of HDL subfractions and hypertensive status including the presence of hypertension, antihypertensive therapy, and blood pressure control and further explored the interplay between hypertension and HDL subfractions in relation to CAD susceptibility.
METHODS
Study Design and Population
The study complied with the Declaration of Helsinki and was approved by the hospital's ethical review board (FuWai Hospital & National Center for Cardiovascular Diseases, Beijing, China). Each participant provided written, informed consent before enrollment.
A total of 4106 patients were hospitalized in our division from October 2012 to January 2015. Because the lipid-lowering medications have potential impact on HDL subfractions, confounding the association with hypertension or other clinical characteristics, we selected 982 consecutive patients who were not treated with lipid-lowering drugs. Additionally, patients with significant hematologic disorders, infectious or systemic inflammatory disease, thyroid dysfunction, severe liver and/or renal insufficiency, acute coronary syndrome (ACS), heart failure (HF) (left ventricular ejection fraction < 45%), arrhythmia, or with malignant tumors were excluded from the current analysis. Therefore, we enrolled 953 eligible patients for the present study. The flowchart of this analysis is presented in Figure 1.
FIGURE 1.
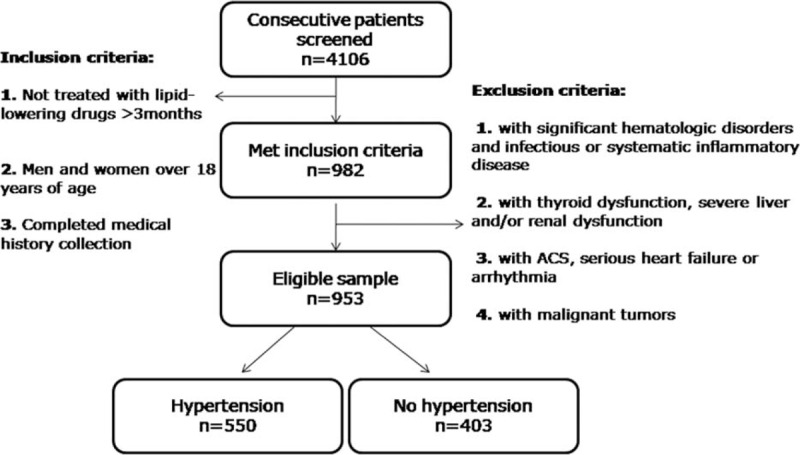
The flowchart of this study. The inclusion and exclusion criteria of population enrollment are shown.
The definition of traditional risk factors has been described in our previous studies.16 Hypertension was defined as repeated blood pressure measurements ≥ 140/90 mm Hg (at least 2 times in different environments) or currently taking antihypertensive drugs. Blood pressure was measured through a mercury sphygmomanometer after checking for the device accuracy. Diabetes mellitus (DM) was defined as a fasting serum glucose level ≥ 126 mg/dL in multiple determinations, and/or the current use of medication for diabetes. Dyslipidemia was defined by medical history or fasting total cholesterol (TC) ≥200 mg/dL or triglyceride (TG) ≥150 mg/dL and/or HDL-C < 40 mg/dL (for male) or < 50 mg/dL (for female). The body mass index (BMI) was calculated as weight (kg) divided by height (m) squared. Obesity was defined as patients with BMI ≥ 30 kg/m2. Patients with a reported smoking habit of at least 1 cigarette per day on admission were classified as current smokers.
Biochemical Examinations
After hospitalized, fasting blood samples were collected for all enrolled subjects. The automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan) was used to test the levels of lipid profiles. The levels of TC, TG, apolipoprotein AI (apo AI), and apo B levels were measured using commercially available kits. The HDL-C and LDL-C levels were analyzed by the selective solubilization method (Determiner L HDL, LDL test kit Kyowa Medex, Tokyo).
HDL Subfraction Analysis
The HDL subfractions were determined electrophoretically by the use of high-resolution 3% polyacrylamide gel tubes and the Lipoprint System (Lipoprint HDL System Quantimetrix Corporation, Redondo Beach, CA) as our previously described.17,18 By this method, the HDL was divided into 10 subfractions. The large HDL particles included subfraction 1 to 3, the medium HDL particles comprised of subfraction 4 to 7, and the small HDL particles covered subfraction 8 to 10.
Statistical Analysis
The data were expressed as the mean ± SD for the continuous normally distributed variables and the number (percentage) for the categorical variables. The Student t tests were used for the comparisons between 2 groups of continuous parameters and the chi-square tests were performed for the categorical variables. Univariate and multivariate logistic regression analyses were used for determining the association of HDL subfractions with incident hypertension as well as with CAD susceptibility in patients with or without hypertension separately. A P value of <0.05 was considered statistically significant. Statistical studies were carried out with the SPSS program (version 19.0, SPSS, Chicago, IL).
RESULTS
Summary of Study Subjects
Selected characteristics of the study population at baseline are shown in Table 1, both overall and according to the incident hypertension. Overall, 953 patients with 606 (63.6%) men and at the mean age of 56.2 years were studied. The cholesterol levels of large, medium, and small HDL were 13.18 ± 6.80 mg/dL, 20.43 ± 5.75 mg/dL, and 8.44 ± 3.02 mg/dL, respectively.
TABLE 1.
Baseline Characteristics
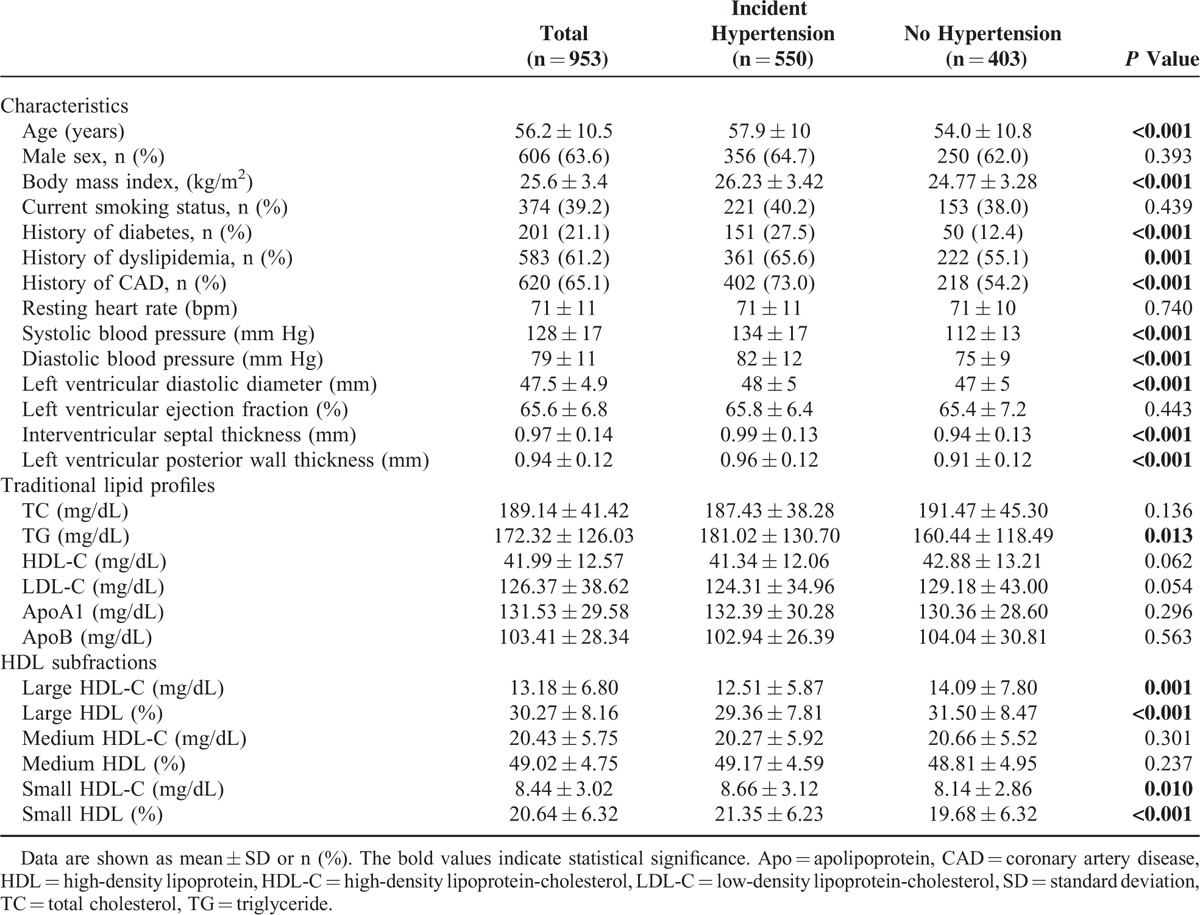
The incident hypertension predominated among the enrolled subjects (n = 550). Patients with hypertension were more likely to be old, to have higher BMI, and to have a higher prevalence of DM, dyslipidemia, and eventually CAD, and to have higher left ventricular diastolic diameter, interventricular septal thickness, and left ventricular posterior wall thickness compared with those without hypertension. Although the mean baseline HDL-C levels were similar, the HDL subfraction measures were significantly differed. In particular, the hypertensive populations have lower large HDL (large HDL-C: 12.51 ± 5.87 vs 14.09 ± 7.80, P = 0.001; large HDL percentage: 29.36 ± 7.81 vs 31.50 ± 8.47, P < 0.001) but higher small HDL subfractions (small HDL-C: 8.66 ± 3.12 vs 8.14 ± 2.86, P = 0.01; small HDL percentage: 21.35 ± 6.23 vs 19.68 ± 6.32, P < 0.001).
HDL Subfractions According to AntiHypertensive Drug Therapy
As indicated in Table 2, among the hypertensive patients, 319 (58.0%) applied antihypertensive treatment at least 3 months before entering the study, among which 193 (60.5%) used single drug therapy, and 126 (39.5%) patients were on drug combination therapy. In addition, 231 (42.0%) patients had life style intervention and were not on drug therapy. Obviously, the plasma HDL-C levels were markedly decreased in patients who were on drug combination therapy. Interestingly, among HDL subfractions, both the large and small HDL subfractions remained the similar level (both P > 0.05) except the decreased medium HDL percentage compared with the single drug therapy (P < 0.05). In addition, no significant difference was found in patients with or without antihypertensive drug therapy with regard to the HDL subfractions (all P > 0.05).
TABLE 2.
The Impact of Antihypertensive Drug Numbers on HDL Subfractions
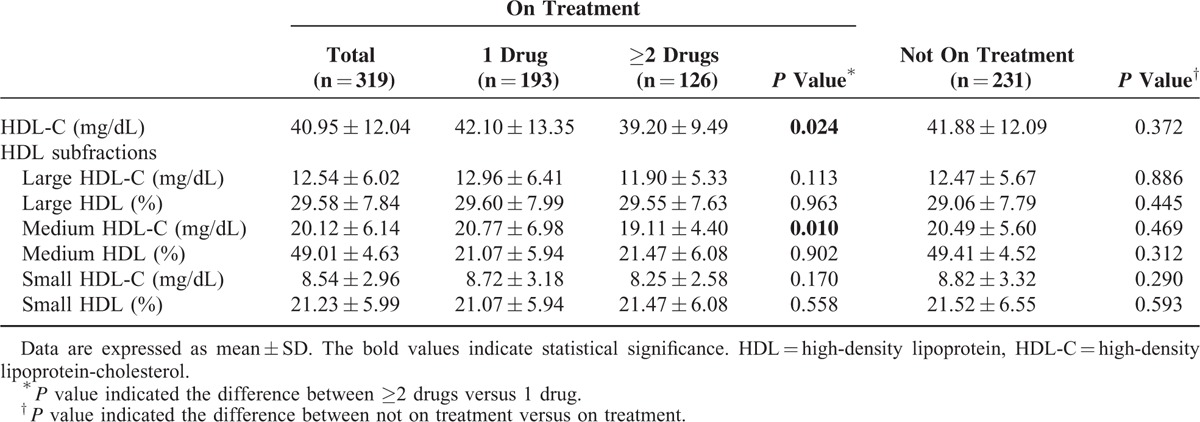
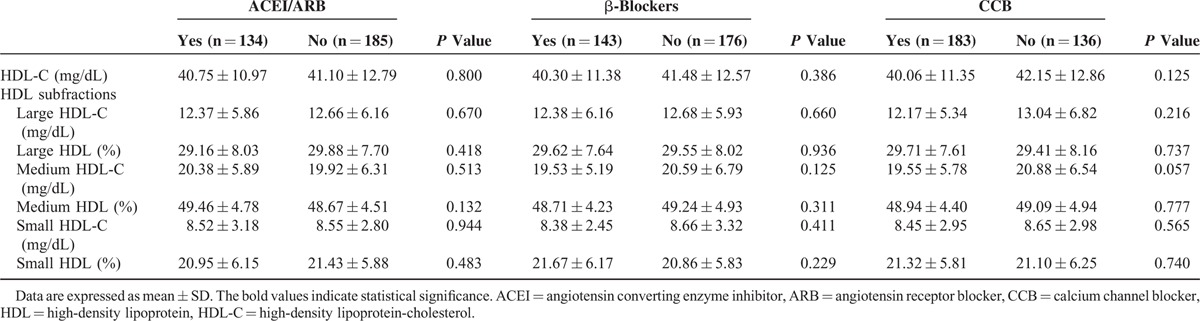
Besides that, among 319 patients on hypertensive drug therapy, 134 (42.0%) used angiotensin receptor blockers or angiotensin-converting enzyme inhibitors, 143 (44.8%) used β-blockers, and 183 (57.4%) used calcium channel blockers. However, we did not observe statistical significance in patients who took either drug regarding plasma levels of all the HDL subfractions (all P > 0.05, Table 3).
TABLE 3.
Association Between Antihypertensive Drug Type and HDL Subfractions
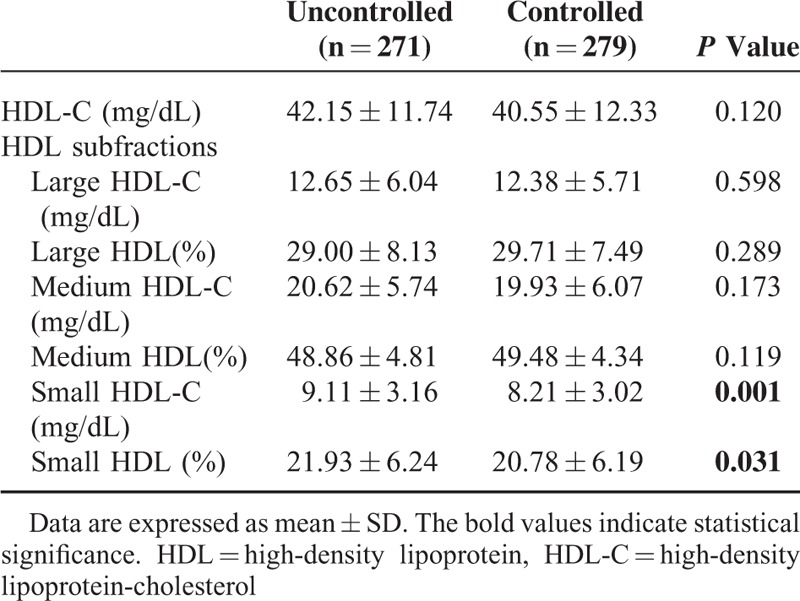
Finally, a total of 271 (49.3%) patients have their blood pressure successfully controlled (systolic blood pressure < 140 mm Hg and diastolic blood pressure < 90 mm Hg). Although the plasma HDL-C levels were not significantly changed compared with the uncontrolled patients, the small HDL subfractions including small HDL-C and small HDL percentage were significantly decreased in patients with well-controlled blood pressure (8.21 ± 3.02 vs 9.11 ± 3.16, P = 0.001; 20.78 ± 6.19 vs 21.93 ± 6.24, P = 0.031, respectively, Table 4).
TABLE 4.
Relation of HDL Subfractions to Status of Blood Pressure Control
Association of HDL Subfractions With Incident Hypertension
After observed the interesting association of HDL subfractions with hypertension and antihypertensive therapy, logistic regression analysis was performed in the present study. In unadjusted analysis (Figure 2A), no significant relationship was found with regard to traditional lipid profiles including HDL-C, TC, LDL-C, apoA1, and apoB except the positive association between TG and hypertension susceptibility (OR 95%CI: 1.002 [1.000–1.003]). Specifically, among different HDL subfractions, large HDL measures were inversely (large HDL-C: OR 95%CI 0.966 [0.947–0.985]; large HDL percentage: OR 95%CI 0.968 [0.953–0.984]) whereas small HDL measures were positively (small HDL-C: OR 95%CI 1.060 [1.014–1.108]; small HDL percentage: OR 95%CI 1.044 [1.022–1.066]) associated with prevalent hypertension.
FIGURE 2.
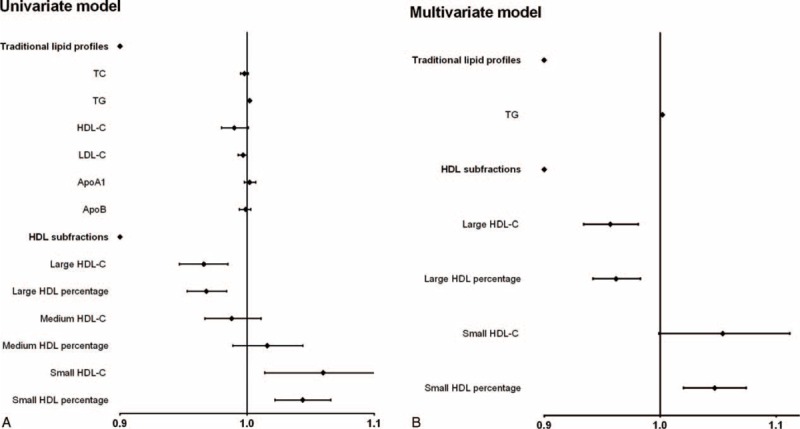
Traditional lipid profiles and HDL subfractions in relation to the incidence of hypertension. The multivariate model was adjusted for age, gender, obesity, smoking, alcohol, diabetes, dyslipidemia, and antihypertensive drugs. Apo = apolipoprotein, HDL = high-density lipoprotein, HDL-C = high-density lipoprotein-cholesterol, LDL-C = low-density lipoprotein-cholesterol, TC = total cholesterol, TG = triglyceride.
Additionally, we next investigated the gender difference with regard to the presence of hypertension and the distribution of HDL subfractions. As a result, we observed that the hypertension susceptibility was similar between men and women (P = 0.414, supplemental Figure 1, http://links.lww.com/MD/A484). Meanwhile, the women had relatively higher HDL subfractions especially large and medium HDL-C (P < 0.001, both in the whole population and hypertensive patients, supplemental Figure 2, http://links.lww.com/MD/A484). Therefore, in the following multivariate logistic regression analysis, we further adjusted for gender as well as other potential risk factors covering age, obesity, smoking, alcohol, DM, dyslipidemia, and antihypertensive drugs. Finally, we found that large HDL-C (OR 95%CI 0.957 [0.934–0.981]) and large HDL percentage (OR 95%CI 0.962 [0.942–0.983]) remained negatively whereas small HDL percentage (OR 95%CI 1.047 [1.020–1.074]) was positively related to hypertension susceptibility (Figure 2B).
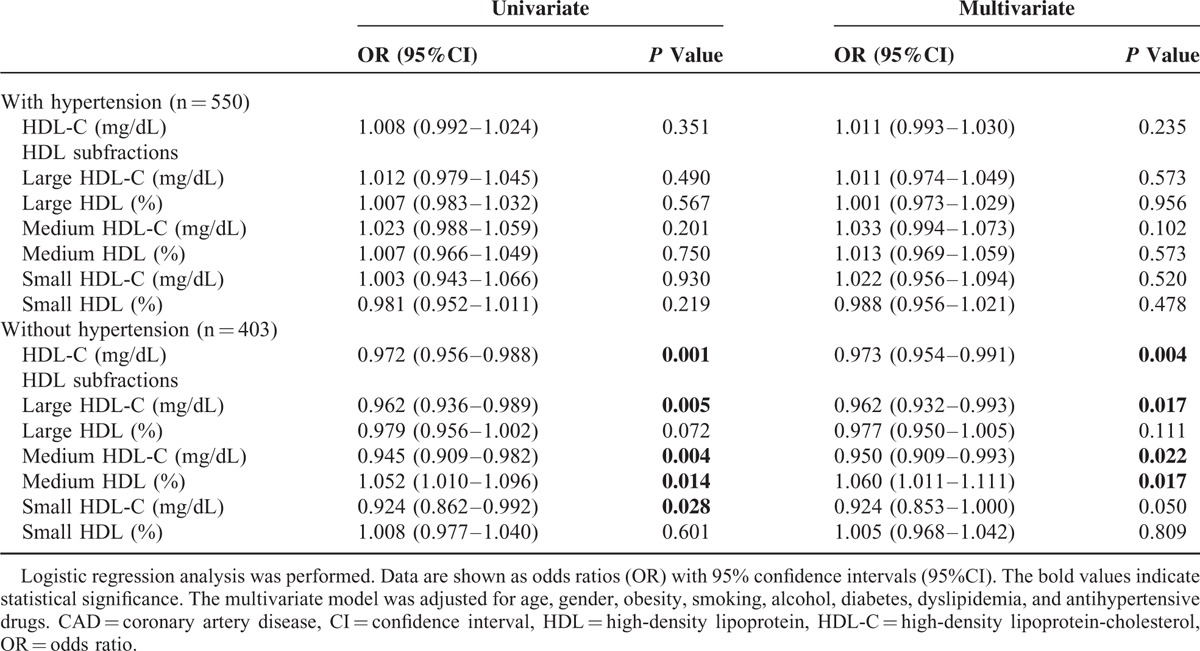
Relationship of HDL Subfractions With CAD Susceptibility According to Hypertension
To reveal whether the presence of hypertension influenced the association between HDL subfractions and the occurrence of CAD, patients were classified into 2 groups due to the incident hypertension. As presented in Table 5, for those without hypertension, large HDL-C levels were negatively associated with CAD susceptibility in univariate logistic regression analysis (OR 95%CI 0.962 [0.936–0.989]), and this association remained significant even after fully adjusting for potential risk factors, including age, gender, obesity, smoking, alcohol, DM, dyslipidemia, and antihypertensive drugs (OR 95%CI 0.962 [0.932–0.993]). In addition, the relationship between medium HDL subfraction and CAD susceptibility was unstable (medium HDL-C: OR 95%CI 0.945 [0.909–0.982]; medium HDL percentage: OR 95%CI 1.060 [1.011–1.111]) in the fully adjusted analysis. Additionally, small HDL-C was not related to CAD susceptibility after adjusting for potential confounders (OR 95%CI 0.924 [0.853–1.000]). However, for those with hypertension, all of the HDL subfractions were not associated with CAD incidence in univariate and multivariate logistic regression analysis (all P > 0.05).
TABLE 5.
The Predictive Value of Lipoprotein Subfractions to Incident CAD by Hypertension
DISCUSSION
To date, there is a paucity of studies, which are primarily aimed to determine the association of dyslipidemia including low HDL-C, hypertriglyceridemia, and even small dense LDL subfractions with hypertension.8,18 Our study involving 953 patients who were not treated with lipid-lowering drugs is the first to document the complex relationship between distribution of HDL subfractions and hypertensive status. Specifically, we found that hypertensive patients have significantly lower large HDL subfractions and higher small HDL subfractions, which were not affected by antihypertensive drugs. Patients with successfully controlled blood pressure have markedly lower small HDL subfractions. Large HDL subfractions were associated with lower risk whereas small HDL subfractions were related to higher risk of hypertension, and this relationship remained significant after adjusting for age, gender, and other potential confounders. The presence of hypertension may have potential impact on the cardio-protective value of large HDL subfractions. Our data may provide additive information to hypertension and atherosclerosis.
To date, postulated mechanisms for the relationship between hypertension and atherosclerosis have not been fully clarified. As indicated previously, although hypertension represents an independent risk factor for CAD, and evidence indicated that there were interactions with other recognized cardiovascular risk factors and could result in a multiplicative increase in risk for cardiovascular events.19 Therefore, multiple studies investigated the relationship between hypertension and lipid profiles and found that traditional lipid measures such as lower HDL-C and higher TG were associated with increased risk.8,20 Our study confirms these findings for TG in this group of patients who were not received lipid-lowering drug therapy, although we did not find the association between HDL-C and the prevalence of hypertension. However, the HDL particles are highly heterogeneous and the subfractions of HDL particles may be more valuable in predicting atherosclerosis. In spite of the exact role of different HDL subfractions in the pathogenesis of atherosclerosis remained in debate,21,22 multiple studies reported that highly lipidated large HDL subfraction was inversely associated with CAD risk.9,23,24 Hence, we thoroughly investigated HDL subfractions and hypertensive status in the present analysis.
In consistent with previous reports, we observed that large HDL subfractions were associated with lower risk of hypertension whereas small HDL subfractions were related to higher hypertensive risk.15 The risk of CAD in the patient with hypertension was greatly reduced with effective antihypertensive therapy. Besides the blood pressure lowering effect, whether there are any effects on HDL subfractions have not been reported yet. In the current analysis, we found that although the HDL-C levels were significantly reduced, the large and small HDL subfractions were not changed in patients with combination therapy than single therapy. However, patients with successfully controlled blood pressure have significantly lower small HDL subfractions. From this perspective, our study may provide more evidence for the benefit of blood control in hypertension management.
Based on the current guidelines, lower systolic blood pressure values may be associated with better stroke outcomes, but the evidence for CAD outcomes is equivocal.25 Numerous data from clinical trials showed a J-shaped relationship between blood pressure and the primary cardiovascular outcomes.26 One theoretically possible explanation was that further reduction of diastolic blood pressure could reduce coronary blood flow and translate to an upturn in the incidence of coronary events. However, this issue remains unresolved. In light of the interesting relationship of HDL subfractions with hypertensive status, we compared the protective value of large HDL subfractions on CAD susceptibility in patients with or without hypertension separately in the current analysis. As a result, we found that the large HDL-C was not related to CAD susceptibility in patients with hypertension while inversely associated with CAD in patients without hypertension. Although the small HDL subfractions were lower in patients with successfully controlled blood pressure, the cardio-protective value of large HDL subfractions were disappeared in hypertensive status in the current analysis. Therefore, our data may partly explain the undeclined CAD outcomes by intensive blood control.
There were several limitations of the present study. First, this was a single center study. The conclusions need to be testified by large-scale studies in the future. Second, the HDL subclassification was performed by the Lipoprint system, and the results should be testified by other methodologies. Finally, the cross-sectional design was another limitation. Therefore, the results should be evaluated with some degree of caution. Longitudinal follow-up and interventional studies were necessary in the following investigations.
In summary, the hypertensive patients had relatively lower large HDL subfractions whereas higher small HDL subfractions. For subjects with hypertension, successful blood pressure control is more relevant to lower small HDL subfractions irrespective what methods (lifestyle intervention, single or combination drug therapy) were applied in clinical practice; large and small HDL subfractions were independently associated with incident hypertension in a negative or positive manner respectively; hypertension may have potential impact on the cardio-protective effect of large HDL subfractions.
Acknowledgments
The authors are grateful to the field staff and the participants of our study.
Footnotes
Abbreviations: CAD = coronary artery disease, CI = confidence interval, DM = diabetes mellitus, HDL = high-density lipoprotein, HDL-C = high-density lipoprotein-cholesterol, LDL = low-density lipoprotein, LDL-C = low-density lipoprotein-cholesterol, TC = total cholesterol, TG = triglyceride.
this work was partly supported by National Natural Science Foundation (81070171, 81241121); Specialized Research Fund for the Doctoral Program of Higher Education of China (20111106110013); Capital Special Foundation of Clinical Application Research (Z121107001012015); Capital Health Development Fund (2011400302); and Beijing Natural Science Foundation (7131014) awarded to Dr. Jian-Jun Li, MD, PhD.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Verdecchia P, Angeli F. The Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation and Treatment of High Blood Pressure: the weapons are ready. Rev Esp Cardiol 2003; 56:843–847. [DOI] [PubMed] [Google Scholar]
- 2.Li H, Wei X, Wong MC, et al. A comparison of the quality of hypertension management in primary care between Shanghai and Shenzhen: a cohort study of 3196 patients. Medicine (Baltimore) 2015; 94:e455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolf D, Zirlik A, Ley K. Beyond vascular inflammation—recent advances in understanding atherosclerosis. Cell Mol Life Sci 2015; 72:3853–3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Potaczek DP. Links between allergy and cardiovascular or hemostatic system. Int J Cardiol 2014; 170:278–285. [DOI] [PubMed] [Google Scholar]
- 5.Tarantino G, Capone D. Inhibition of the mTOR pathway: a possible protective role in coronary artery disease. Ann Med 2013; 45:348–356. [DOI] [PubMed] [Google Scholar]
- 6.Halperin RO, Sesso HD, Ma J, et al. Dyslipidemia and the risk of incident hypertension in men. Hypertension 2006; 47:45–50. [DOI] [PubMed] [Google Scholar]
- 7.de Simone G, Devereux RB, Chinali M, et al. Risk factors for arterial hypertension in adults with initial optimal blood pressure: the Strong Heart Study. Hypertension 2006; 47:162–167. [DOI] [PubMed] [Google Scholar]
- 8.Laaksonen DE, Niskanen L, Nyyssonen K, et al. Dyslipidaemia as a predictor of hypertension in middle-aged men. Eur Heart J 2008; 29:2561–2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu RX, Li S, Li XL, et al. High-density lipoprotein subfractions in relation with the severity of coronary artery disease: a Gensini score assessment. J Clin Lipidol 2015; 9:26–34. [DOI] [PubMed] [Google Scholar]
- 10.Martin SS, Khokhar AA, May HT, et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: the Lipoprotein Investigators Collaborative. Eur Heart J 2015; 36:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Landray MJ, Edmunds E, Li-Saw-Hee FL, et al. Abnormal low-density lipoprotein subfraction profile in patients with untreated hypertension. Qjm 2002; 95:165–171. [DOI] [PubMed] [Google Scholar]
- 12.Kim YK, Seo HS, Lee EM, et al. Association of hypertension with small, dense low-density lipoprotein in patients without metabolic syndrome. J Hum Hypertens 2012; 26:670–676. [DOI] [PubMed] [Google Scholar]
- 13.Takiwaki M, Tomoda F, Koike T, et al. Increased levels of small dense low-density lipoprotein cholesterol associated with hemorheological abnormalities in untreated, early-stage essential hypertensives. Hypertens Res 2014; 37:1008–1013. [DOI] [PubMed] [Google Scholar]
- 14.Rosenson RS, Brewer HB, Jr, Chapman MJ, et al. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin Chem 2011; 57:392–410. [DOI] [PubMed] [Google Scholar]
- 15.Paynter NP, Sesso HD, Conen D, et al. Lipoprotein subclass abnormalities and incident hypertension in initially healthy women. Clin Chem 2011; 57:1178–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Y, Xu RX, Li S, et al. Association of plasma small dense LDL cholesterol with PCSK9 levels in patients with angiographically proven coronary artery disease. Nutr Metab Cardiovasc Dis 2015; 25:426–433. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Xu RX, Li S, et al. Lipoprotein subfractions partly mediate the association between serum uric acid and coronary artery disease. Clin Chim Acta 2015; 441:109–114. [DOI] [PubMed] [Google Scholar]
- 18.Xu RX, Li S, Zhang Y, et al. Relation of plasma PCSK9 levels to lipoprotein subfractions in patients with stable coronary artery disease. Lipids Health Dis 2014; 13:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kannel WB. Some lessons in cardiovascular epidemiology from Framingham. Am J Cardiol 1976; 37:269–282. [DOI] [PubMed] [Google Scholar]
- 20.Sesso HD, Buring JE, Chown MJ, et al. A prospective study of plasma lipid levels and hypertension in women. Arch Intern Med 2005; 165:2420–2427. [DOI] [PubMed] [Google Scholar]
- 21.Mack WJ, Krauss RM, Hodis HN. Lipoprotein subclasses in the Monitored Atherosclerosis Regression Study (MARS): treatment effects and relation to coronary angiographic progression. Arterioscler Thromb Vasc Biol 1996; 16:697–704. [DOI] [PubMed] [Google Scholar]
- 22.Sharrett AR, Ballantyne CM, Coady SA, et al. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: the Atherosclerosis Risk in Communities (ARIC) Study. Circulation 2001; 104:1108–1113. [DOI] [PubMed] [Google Scholar]
- 23.Salonen JT, Salonen R, Seppanen K, et al. HDL, HDL2, and HDL3 subfractions, and the risk of acute myocardial infarction: a prospective population study in eastern Finnish men. Circulation 1991; 84:129–139. [DOI] [PubMed] [Google Scholar]
- 24.Lamarche B, Moorjani S, Cantin B, et al. Associations of HDL2 and HDL3 subfractions with ischemic heart disease in men: prospective results from the Quebec Cardiovascular Study. Arterioscler Thromb Vasc Biol 1997; 17:1098–1105. [DOI] [PubMed] [Google Scholar]
- 25.Messerli FH, Bangalore S, Ram VS. Telmisartan, ramipril, or both in patients at high risk of vascular events. N Engl J Med 2008; 359:426–427.author reply 427. [PubMed] [Google Scholar]
- 26.Denardo SJ, Gong Y, Nichols WW, et al. Blood pressure and outcomes in very old hypertensive coronary artery disease patients: an INVEST substudy. Am J Med 2010; 123:719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]


