Abstract
Patent foramen ovale (PFO) is a remnant of the fetal circulation exist in 20% of the general population. The purpose of our study was to compare of transthoracic echocardiography (TTE) and contrast-transcranial Doppler sonography (c-TCD) in the diagnosis and quantification of PFO with or without the Valsalva maneuver (VM).
We studied 106 patients with a high clinical suspicion for PFO prospectively. Simultaneous c-TCD and TTE were conducted using agitated saline solution to detect right to left shunt (RLS). To classify RLS, mainly PFO, we applied a 4-level visual classification for c-TCD test: no occurrence of micro-embolic signals; grade I, 1 to 10 signals; grade II, 10 to 30 signals but not curtain; and grade III, curtain pattern. We used the number of micro-bubbles appeared in left atrium per frame image to define classification for TTE test: no occurrence of micro-bubbles; grade I, 1 to 10 micro-bubbles; grade II, 10 to 30 micro-bubbles; and grade III, more than 30 micro-bubbles or left atrium nearly filled with micro-bubbles or left atrial opacity. Statistical analyses were performed using SPSS Version 18.0.
RLS was detected in 36.0% in c-TCD test and in 46% in TTE test at rest (P = 0.158). And during the VM, RLS was detected in 99.0% in c-TCD test and in 83.0% in TTE test (P < 0.001). Compared with the positive results of c-TCD and TTE at rest, the positive results of them with VM is more higher, respectively (all P < 0.001). The VM obviously increased the number of micro-bubbles shunting.
Both c-TCD and TTE should used as initial screening tool for PFO. VM increases the size of shunt. VM resulted in detection of more RLS both in c-TCD and TTE tests.
INTRODUCTION
Patent foramen ovale (PFO) is a common finding in the healthy population, with a prevalence of 27.3% for all age in 1 autopsy study of 965 normal hearts.1 A population-based study reported that PFO has a highly prevalent of 24.3%.2 And a recently study reported that about 25% population of potential possibility for right-to-left shunting during adult life.3 Therefore, PFO should be regarded as a normal structural variant even without paradoxical embolism or other discomfortable clinical conditions existed. A atrial right-to-left shunt (RLS) through PFO is the most frequent finding in young patients (<55 years of age) who suffered from an unexplained cerebrovascular event, probably owing to paradoxical emboli.4 It is well known that paradoxical thrombotic embolism through a cardiac RLS is an important cause of stroke, especially in younger patients.5 It is reported that PFO has also been associated with several disease processes such as paradoxical embolism in cryptogenic stroke,6,7 arterial gas embolism due to decompression,8 transient ischemic attack (TIA),5,9 or platypnea-orthodeoxia syndrome.10,11 Echo-contrast transesophageal echocardiography (c-TEE) is regarded as the “gold standard” for the diagnosis of cardiac RLS.12 However, TEE test is supposed to time-consuming and semi-invasive by the patients, besides, other less invasive techniques detection for PFO, such as TTE and TCD, have been improved.13 Performaning Valsalva maneuver (VM) during TEE test requires the patient's good cooperation and previous training, which may does harm to some poststroke patients.14 Another limitation is that TEE requires an excellent echocardiographer, patients cannot tolerant the test, and patients often failed to perform VM properly owing to sedation and endoscope in the throat.15These disadvantages limit the routine application of TEE. RLS across PFO can be detected with contrast agent with other 2 different modalities: contrast-transthoracic echocardiography (TTE) and contrast-transcranial Doppler sonography (c-TCD). TTE and c-TCD have some advantages compared with TEE. They are less invasive, and the results are more quantifiable. Both during TTE and c-TCD tests, some authors suggested to perform VM. Because the functional grading of the cardiac shunt might influenced by VM.15 A previous standardized c-TCD study reported that the VM increases the positive results 45% by increasing the right atrial pressure (RAP) to cause or reveal flow inversion through PFO.16 We investigated the ability of TTE with or without VM to detect RLSs compared with TCD in patients suspected of PFO. We also assessed the effect of the VM on shunt size as estimated by the number of agitated saline micro-bubbles crossing the left atrium.
METHODS
We enrolled 106 consecutive patients with a high clinical suspicion for PFO referred to our neurology department or cardiology department of our hospital for the evaluation of cardiac sources of embolism. All the patients were recruited from February 2014 to June 2015 in Shaanxi Province, China. Before our test, all the patients were given training to perform standard VM. All the patients had previously given signed informed consent. The study protocol was approved by the ethics committee of the Second Affiliated Hospital of Xi’an Jiaotong University. All the patients were subjected to 2 diagnostic examinations: The c-TCD was performed as first check by a neurologist; subsequently, the patients were sent to our echocardiography laboratory and were subjected to the TTE examination. After both examinations, patients were followed up at least 12 hours. No patient had an adverse event during or after the examination either at rest or during VM. All patients performed TCD and TTE examinations successively, and both methods were used for RLS diagnosis, which suggested a good comparability of our study. Previous intracranial or extracranial arterial disease and pulmonary arteriovenous malformation were ruled out using computed tomography or magnetic resonance imaging. Patients willing to participate in both TTE and TCD tests were included in our study. Patients absence of temporal window and could not cooperate by undergoing VM during the c-TCD tests and TTE test were excluded.
Transcranial Sonography
A Vivid 7 system fitted with 2.9 to 8.0 MHz multi-frequency probe was used in the c-TCD examination. The patients should be in the supine position and an 18-gauge needle was inserted into the cubital vein before the test. For c-TCD embolus detection, the middle cerebral artery (MCA) should be insonated bilaterally with the satisfactory temporal bone windows. The contrast agent consisted of 9 mL saline solution and 1 mL air should be mixed between the two 10-mL syringes connected by a 3-way stopcock at least 10 times and then vertical injected into the cubital vein as a bolus both at rest and during VM. We trained patients in performance of the VM before the tests. We assessed the effective VM by monitoring the peak flow velocity of the MCA Doppler spectrum decreased at least 25%.17 First, 10 mL of mixed contrast agent consisting of 9 mL of saline and 1 mL of air was injected into cubital vein in basal conditions and the test was repeated during VM, and the MCA Doppler spectrum was recorded for 25 seconds. Then the VM was started immediately after the contrast injection, and during a period of 25 seconds, the Doppler spectrum was also recorded. To avoid potential bias in c-TCD study, VM was performed 3 times and the 1 that mostest micro-embolic signals (MES) were detected was treated as the final results. Besides, each interval was at least 5 min. When more than 1 micro-embolic appeared within 25 seconds after contrast agent injection, we regarded the c-TCD result as positive and assumed cardiac RLS passage through the PFO. When the micro-embolic appeared in the Doppler spectrum later than 25 seconds, pulmonary passage shunt was assumed. If no high-intensity transient signals (HITS) were detected at c-TCD test, we classified the patients as having no RLS (negative); if 1 to 10 HITS were detected, a classification of “grade I” shunt was diagnosed; if 10 to 30 HITS were detected, a classification of “grade II” shunt was diagnosed; if more than 30 HITS or curtain were detected, a classification of “grade III” shunt was diagnosed13 (Fig. 1).
FIGURE 1.
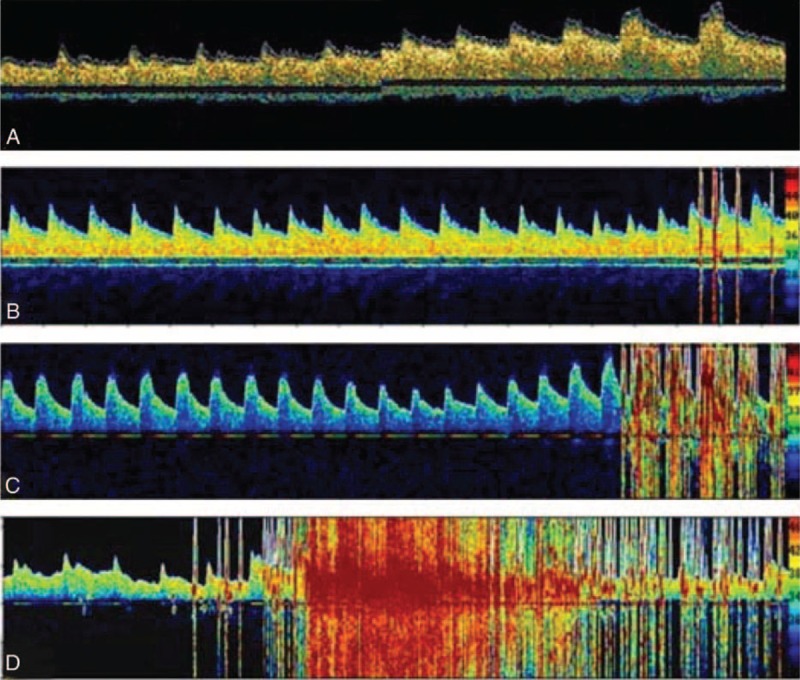
Quantification of the shunt by transcranial Doppler ultrasound. (A) No occurrence of micro-embolic signals (negative). (B) Grade I, 1 to 10 micro-embolic signals. (C) Grade II, 10 to 30 micro-embolic signals but no curtain. (D) Grade III, curtain pattern.
Transthroracic Echocardiograpy
The TTE test was performed with Philips iE33 platform, with S5–1 transducer (5–1 MHz). We used the apical 4-chamber view to optimize visualization of the interatrial septum, atria and ventricles. Gain settings were adjusted to make the interatrial septum, myocardium and valvular structures optimize visualized. Before contrast medium injection, TTE test was routinely conducted to exclude other reasons for cardiac embolism and cardiac abnormalities. We kept continuous recording during contrast injections under the condition of an apical 4-chamber view. Following continuous recordings during normal respiration was repeated with a VM. This was produced by the patients blowing into a small soft plastic tube connected to the manometer device. Patients were also trained in performance of the VM before the tests to achieve and to maintain a pressure of 40 mm Hg lasting 5 seconds. The standard VM was assessed by observing a minimum reaching 40mm Hg of manometer.18 The same contrast agent consisted of 9 mL saline solution and 1 mL air should also be mixed between the two 10-mL syringes connected by a 3-way stopcock at least 10 times and then vertical injected into the cubital vein as a bolus both at rest and during VM. When micro-bubbles appeared in the right atrium, the standard VM was conducted and was lasting for 5 seconds.19 If the testing results with or without VM was positive, a further 2 times operation was needed to assess its reproducibility. And each interval was at least 5 min. The 1 operation that mostest micro-bubbles appeared in the left atrium was regarded as the final results. Then all TTE recordings were reported retrospectively by 2 experienced sonographer blinded to the result of the c-TCD. All the patients had previously given signed informed consent. RLS was diagnosed when TTE detected micro-bubbles in the left atrium, and the degree of shunt severity was quantified according to following criteria: no occurrence of micro-bubbles (negative); grade I, 1 to 10 micro-bubbles; grade II, 10 to 30 micro-bubbles; and grade III, more than 30 micro-bubbles or left atrium nearly filled with micro-bubbles or left atrial opacity (Fig. 2).
FIGURE 2.
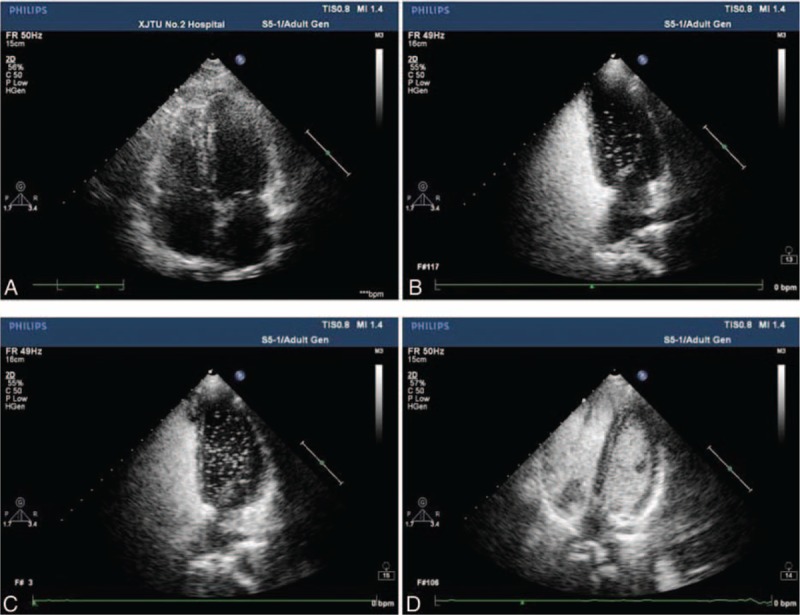
Quantification of the shunt by transthoracic echocardiography. (A) No occurrence of micro-bubbles (negative). (B) Grade I, 1 to 10 micro-bubbles. (C) Grade II, 10 to 30 micro-bubbles. (D) Grade III, more than 30 micro-bubbles or left atrium nearly filled with micro-bubbles or left atrial opacification.
Statistical Analysis
Categorical variables and continuous are expressed as percentages and mean ± standard deviation, respectively. Positive results percentage of c-TCD at rest, c-TCD under VM, and TTE at rest, TTE under VM was calculated. Comparison of the findings between c-TCD and TTE was performed using a chi-squared test. A 2-tailed P value of <0.05 was used as a cutoff for statistical significance. Statistical analyses were performed using SPSS Version 18.0 (SPSS, Chicago, IL).
RESULTS
The study population consisted of 106 consecutive patients (mean age 39.16 ± 1.41 years, 87 were <55 years old; men 67 and women 39) who were admitted to our neurology department or cardiology department. None of the patients withdrew from the study at each stage of examinations. All the patients suffered cerebrovascular event. The final examination results are summarized in Table 1.
TABLE 1.
Results of c-TCD and TTE at Rest and During the Valsalva Maneuver

Owing to the cooperation of patients and the skill level of operator, not every VM will lead to satisfactory results. So after a further 2 times operation both in c-TCD test and in TTE test, we detected at least 1 MES in 70 patients (66.0%) at rest in c-TCD test, whereas the percentage of positive tests was 56.6% (60 patients) in TTE test (no statistically significant difference; χ2 = 1.989, P = 0.158). When the VM was performed, the test result was positive in 105 patients (99.0%) in c-TCD examination and in 88 patients (83.0%) in TTE examination, and the difference was statistically significant (χ2 = 16.708, P < 0.001). For c-TCD test, the test result was positive in 70 patients (66.0%) at rest and 105 patients (99.0%) during VM (statistically significant difference; χ2 = 40.108, P < 0.001). And for TTE test, the test result was positive in 60 patients (56.6%) at rest and 88 patients (83.0%) during VM (statistically significant difference; χ2 = 17.547, P < 0.001).
When it comes to grade classification in c-TCD examination, 70 (66.0%) tests were negative, 25 (23.5%) were grade I, 5 (4.70%) were grade II, and 6 (5.80%) were grade III at rest, whereas when TTE were used; there were 60 (56.6%) negative, 34 (32.0%) grade I, 7 (6.6%) grade II, and 5 (4.8%) grade III tests at rest.
The VM yielded 1 (1.0%) negative test, 30 (28.3%) were grade I, 32 (30.2%) were grade II, and 43 (40.5%) was grade III when c-TCD were used. When TTE were used, 18 (17.0%) tests were negative, 15 (14.1%) were grade I, 24 (22.6%) were grade II, and 49 (46.3%) were grade III. The differences between the results using c-TCD and TTE were statistically significant both at rest and during the VM (χ2 = 40.108, P < 0.001 and χ2 = 17.547, P < 0.001, respectively). VM increases the size of shunt. In all c-TCD positive tests, we observed the MES in the first 25 seconds after contrast injection. The VM was performed in TTE test when bubbles appeared in the right atrium and was continued for 5 seconds.
DISCUSSION
Our results indicate that c-TCD yielded a no statistically difference positive tests compared with the TTE test at rest (P = 0.158). However, c-TCD yielded a larger number of positive tests compared with TTE test with VM (P < 0.001). Our study also found that compared with the positive tests with c-TCD and TTE at rest, c-TCD and TTE test with VM yielded a larger number of positive tests, respectively (P < 0.001).
The above results suggested that TTE test yielded a lower positive test compared with c-TCD. Several previous studies demonstrate the low sensitivity of TTE compared with TEE.20,21 A meta-analysis also suggested that when contrast TEE is used as the gold standard, routine c-TTE diagnoses intracardiac RLS with a sensitivity of 46% and specificity of 99%,22 which was similar to that reported in our study. Another meta-analysis revealed that TCD yielded a weighted mean sensitivity and specificity for were 97% and 93%, respectively.23 We think there may be several reasons resulting in the lower sensitivity of TTE than c-TCD. Firstly, owing to the longer time window of TCD, positive results may include intracranial or extracranial arterial disease and pulmonary arteriovenous malformation. Secondly, the differentiation between cardiac and pulmonary shunts by c-TCD is hardly possible, because a very small intra-cardiac shunt cannot be excluded,24 which may detect more positive results. Besides, when performed the VM during TTE test, the patients cannot keep absolutely still, especially in the release phase of VM. The poor images quality of TTE is regarded as another factor.
Now, TTE with contrast agent is still the most widespread initial screening tool for PFO because of its low cost, easy availability, and noninvasiveness. However, its low sensitivity makes it a poor rule out tool for PFO. Even TTE was regarded as an initial screening tool, previous study13,25 has reported that TTE with second harmonic imaging and c-TCD had a comparable sensitivity compared with TEE, which suggested that TTE may need to be replaced by them. A recently study hold that TCD has a favorable sensitivity and specificity when TEE was used as reference for PFO diagnosis, and they recommended TCD as the first choice for screening PFO.24 However, they also found that a very small intra-cardiac shunt cannot be excluded by c-TCD. Besides, TCD falls to provide the anatomical information and therefore cannot be used in isolation. So we believed that both c-TCD and TTE should be used as initial screening test for PFO.
The original maneuver was described by Valsalva in 1704. Then it was first used to expel pus from the middle ear by forced expiration against a closed mouth and nose. Since then, the VM has been widely used by physicians during physical examinations.26 It is reported that VM may increase the sensitivity of TTE examination.27 Under normal circumstances, the left atrial pressure (LAP) is higher when compared with the RAP; therefore, no obvious RLS appears only when the RAP exceeds the LAP. As the heart is confined to the thoracic cavity and connected to the outside of chest cavity through a vein and artery system,28 so it is always exposed to the changes effects of intrathoracic pressure, such as coughing, straining to defecate, during a VM, or lifting heavy objects,29 which can causes RAP increased, thus, RLS through a PFO is more easier. Study reported that RAP exceeding the LAP can promote the contrast agent in right atrium get through a PFO to the left atrium.30 The sensitivity of such technique is improved when VMs were used, which cause transient increased in the pressure gradient between the right atria (RA) and left atria (LA), which was also demonstrated by our study. Under the condition of VM, the increased intrathoracic pressure results in a series of rapid changes, including preload decreased, venous return decreased, and peripheral venous pressure increased, which subsequently results in LAP decreased and atrial septal swing. And therefore the VM can increase the amount of right atrium to left atrium contrast shunting across a PFO.27 The VM is therefore vital both during the TTE examination and c-TCD examination when assessing for a cardiac shunt.
Our work has important clinical implications. We found that patients who are unable to tolerant to semi-invasive examination, such as TEE, benefited from standard performance of the VM, which was regarded as an essential element of the examination. Both TCD and TTE with VM are necessary and complementary to detect a significant foramen ovale. The age of our patients ranged from 14 to 69 years and men accounted for 63.2%, which suggested that our study had a good generalizability. However, our study has some limitations. Six patients were excluded from the study, primarily due to not cooperate by undergoing VM during the c-TCD or TTE tests, which might influence the results. Besides, our patients were not conducted transesophageal echocardiography (TEE) to confirm whether the presence of PFO existed and evaluated its size. However, the aim of our study was to compare c-TCD and TTE in PFO diagnosis with or without VM rather than to confirm the association between the detection of RLS and the presence of PFO. Another limitation is the small number of patients in our population; and further prospective studies with larger populations are warranted to confirm the results of our study.
CONCLUSIONS
We found that under the condition of VM, c-TCD test had a higher positive results compared with TTE. The VM can enhanced the possibility of diagnosis an RLS both during the TTE examination and c-TCD examination. We hold that both c-TCD and TTE should used as initial screening test for PFO.
Footnotes
Abbreviations: c-TCD = contrast-transcranial Doppler sonography, MES = micro-embolic signals, PFO = patent foramen ovale, RLS = right-to-left shunt, TTE = transthoracic echocardiography, VM = Valsalva maneuver.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clinic Proc 1984; 59:17–20. [DOI] [PubMed] [Google Scholar]
- 2.Meissner I, Khandheria BK, Heit JA, et al. Patent foramen ovale: innocent or guilty? Evidence from a prospective population-based study. J Am Coll Cardiol 2006; 47:440–445. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh AK, Jain A. Diagnosis and management of patent foramen ovale. Br J Hosp Med (Lond) 2015; 76:C98–C102. [DOI] [PubMed] [Google Scholar]
- 4.Piechowski-Jozwiak B, Bogousslavsky J. Stroke and patent foramen ovale in young individuals. Eur Neurol 2013; 69:108–117. [DOI] [PubMed] [Google Scholar]
- 5.Wozniak L, Mielczarek M, Sabiniewicz R. Paradoxical brain embolism in a young man: is it only a patent foramen ovale? Neurol Neurochir Pol 2015; 49:61–64. [DOI] [PubMed] [Google Scholar]
- 6.Schuchlenz HW, Weihs W, Horner S, et al. The association between the diameter of a patent foramen ovale and the risk of embolic cerebrovascular events. Am J Med 2000; 109:456–462. [DOI] [PubMed] [Google Scholar]
- 7.Rigatelli G, Rigatelli A. Closing patent foramen ovale in cryptogenic stroke: the underscored importance of other interatrial shunt variants. World J Cardiol 2015; 7:326–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knauth M, Ries S, Pohimann S, et al. Cohort study of multiple brain lesions in sport divers: role of a patent foramen ovale. BMJ (Clin Res ed) 1997; 314:701–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calvert PA, Rana BS, Kydd AC, et al. Patent foramen ovale: anatomy, outcomes, and closure. Nat Rev Cardiol 2011; 8:148–160. [DOI] [PubMed] [Google Scholar]
- 10.Godart F, Rey C, Prat A, et al. Atrial right-to-left shunting causing severe hypoxaemia despite normal right-sided pressures. Report of 11 consecutive cases corrected by percutaneous closure. Eur Heart J 2000; 21:483–489. [DOI] [PubMed] [Google Scholar]
- 11.Mojadidi MK, Gevorgyan R, Noureddin N, et al. The effect of patent foramen ovale closure in patients with platypnea-orthodeoxia syndrome. Catheter Cardiovasc Interv 2015; 86:701–707. [DOI] [PubMed] [Google Scholar]
- 12.Caputi L, Carriero MR, Falcone C, et al. Transcranial Doppler and transesophageal echocardiography: comparison of both techniques and prospective clinical relevance of transcranial Doppler in patent foramen ovale detection. J Stroke Cerebrovasc Dis 2009; 18:343–348. [DOI] [PubMed] [Google Scholar]
- 13.Maffe S, Dellavesa P, Zenone F, et al. Transthoracic second harmonic two- and three-dimensional echocardiography for detection of patent foramen ovale. Eur J Echocardiogr 2010; 11:57–63. [DOI] [PubMed] [Google Scholar]
- 14.Shariat A, Yaghoubi E, Nemati R, et al. Comparison of agitated saline mixed with blood to agitated saline alone in detecting right-to-left shunt during contrast-transcranial Doppler sonography examination. Acta Neurol Taiwan 2011; 20:182–187. [PubMed] [Google Scholar]
- 15.Paliwal PR, Sharma VK. Valsalva maneuver in detection of right-to-left shunt by transcranial Doppler. Arq Neuropsiquiatr 2010; 68:979. [DOI] [PubMed] [Google Scholar]
- 16.Lange MC, Zetola VF, de Souza AM, et al. Transcranial Doppler for patent foramen ovale screening: is there a good correlation with transesophageal echocardiography? Arq Neuropsiquiatr 2008; 66:785–789. [DOI] [PubMed] [Google Scholar]
- 17.Zanette EM, Mancini G, De Castro S, et al. Patent foramen ovale and transcranial Doppler. Comparison of different procedures. Stroke 1996; 27:2251–2255. [DOI] [PubMed] [Google Scholar]
- 18.Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 2009; 10:165–193. [DOI] [PubMed] [Google Scholar]
- 19.Wei D, Ju Y. Importance of an adequately performed Valsalva maneuver for detecting a right-to-left shunt indicating foramen ovale reopening. J Ultrasound Med 2015; 34:879–883. [DOI] [PubMed] [Google Scholar]
- 20.Zito C, Dattilo G, Oreto G, et al. Patent foramen ovale: comparison among diagnostic strategies in cryptogenic stroke and migraine. Echocardiography (Mount Kisco, NY) 2009; 26:495–503. [DOI] [PubMed] [Google Scholar]
- 21.Martinez-Sanchez P, Medina-Baez J, Lara-Lara M, et al. [Low sensitivity of the echocardiograph compared with contrast transcranial Doppler in right-to-left shunt. Neurologia (Barcelona, Spain) 2012; 27:61–67. [DOI] [PubMed] [Google Scholar]
- 22.Mojadidi MK, Winoker JS, Roberts SC, et al. Accuracy of conventional transthoracic echocardiography for the diagnosis of intracardiac right-to-left shunt: a meta-analysis of prospective studies. Echocardiography (Mount Kisco, NY) 2014; 31:1036–1048. [DOI] [PubMed] [Google Scholar]
- 23.Mojadidi MK, Roberts SC, Winoker JS, et al. Accuracy of transcranial Doppler for the diagnosis of intracardiac right-to-left shunt: a bivariate meta-analysis of prospective studies. JACC Cardiovasc Imag 2014; 7:236–250. [DOI] [PubMed] [Google Scholar]
- 24.Komar M, Olszowska M, Przewlocki T, et al. Transcranial Doppler ultrasonography should it be the first choice for persistent foramen ovale screening? Cardiovas Ultrasound 2014; 12:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Madala D, Zaroff JG, Hourigan L, et al. Harmonic imaging improves sensitivity at the expense of specificity in the detection of patent foramen ovale. Echocardiography (Mount Kisco, NY) 2004; 21:33–36. [DOI] [PubMed] [Google Scholar]
- 26.Nishimura RA, Tajik AJ. The Valsalva maneuver-3 centuries later. Mayo Clinic Proc 2004; 79:577–578. [DOI] [PubMed] [Google Scholar]
- 27.Clarke NR, Timperley J, Kelion AD, et al. Transthoracic echocardiography using second harmonic imaging with Valsalva manoeuvre for the detection of right to left shunts. Eur J Echocardiogr 2004; 5:176–181. [DOI] [PubMed] [Google Scholar]
- 28.Wang Z, Yuan LJ, Cao TS, et al. Simultaneous beat-by-beat investigation of the effects of the Valsalva maneuver on left and right ventricular filling and the possible mechanism. PLoS ONE 2013; 8:e53917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kerut EK, Norfleet WT, Plotnick GD, et al. Patent foramen ovale: a review of associated conditions and the impact of physiological size. J Am Coll Cardiol 2001; 38:613–623. [DOI] [PubMed] [Google Scholar]
- 30.Beigel R, Goland S, Siegel RJ. Comparison of the effect on right atrial pressure of abdominal compression versus the Valsalva maneuver. Am J Cardiol 2014; 113:183–186. [DOI] [PubMed] [Google Scholar]


