Abstract
Emergency and trauma care produces a “perfect storm” for radiological errors: uncooperative patients, inadequate histories, time-critical decisions, concurrent tasks and often junior personnel working after hours in busy emergency departments. The main cause of diagnostic errors in the emergency department is the failure to correctly interpret radiographs, and the majority of diagnoses missed on radiographs are fractures. Missed diagnoses potentially have important consequences for patients, clinicians and radiologists. Radiologists play a pivotal role in the diagnostic assessment of polytrauma patients and of patients with non-traumatic craniothoracoabdominal emergencies, and key elements to reduce errors in the emergency setting are knowledge, experience and the correct application of imaging protocols. This article aims to highlight the definition and classification of errors in radiology, the causes of errors in emergency radiology and the spectrum of diagnostic errors in radiography, ultrasonography and CT in the emergency setting.
INTRODUCTION
Errors in medicine have become eye-catching news in recent years, and legal acts against physicians for suspected malpractice is an increasing problem in all industrialized nations and in all fields of medicine. Radiology is not immune to this phenomenon and presents an amount of distinctive features linked to both the inherent characteristics of the discipline and its latest developments.1,2 In fact, diagnosis in radiology depends entirely on the visual perception and on the identification of specific characteristics on a radiograph. Radiologists play a pivotal role in the diagnostic assessment of patients in the emergency setting. The emergency room setting presents a scenario suitable for malpractice claims, such as rapid diagnosis and management of patients with whom we have had no prior interaction and who, quite often, may be uncooperative and/or under the influence of drugs or alcohol, and produces an environment with important risk.3
Fractures in some complicated anatomical locations are notoriously difficult to detect on plain radiographs that, overall, remain the primary imaging modality used in the emergency department (ED).4 Misinterpretation of fractures may determine a delayed treatment and poor outcome for patients treated in the ED.5 It is also one of the most frequent factors leading to medical legal claims.6
The present review aims to highlight: (1) definition and classification of errors in radiology, (2) causes of errors in emergency radiology, and (3) spectrum of diagnostic errors in radiography, ultrasonography and CT in the emergency setting.
DEFINITION AND CLASSIFICATION OF ERRORS IN RADIOLOGY
An error represents a deviation from the ordinary norm, regardless of whether it results in any damage. A diagnostic error has been defined as a diagnosis that is missed, wrong or delayed as discovered by later conclusive tests or findings.7 Errors may be categorized according to different approaches, and we have systems to facilitate their identification so that steps can be used to decrease their incidence. Usually, there are four leading causes why radiologists are litigated: (1) observer errors, (2) errors in interpretation, (3) failure to suggest the next appropriate procedure and (4) failure to communicate in a timely and clinically appropriate manner.8
Observer errors
Kundel et al9 reported the following three varieties of observer errors: scanning error, recognition error and decision-making error. Failure of the radiologist to fixate on the region of the lesion is a scanning error. Recognition error includes fixating on the area of the lesion yet failing to detect the lesion. Decision-making error is the inappropriate interpretation of a lesion as a normal finding.
Another type of observer error that may contribute to lesions being overlooked is the satisfaction of search (SOS) error.10 An SOS error is the consequence of the radiologist's attention being diverted from a tumour by an eye-catching but unrelated finding.
Failures of abnormality diagnosis during the evaluation of radiographs are subject to psychophysiological factors of visual perception.11,12 They are common to visual perceptual jobs and are significant to other professions (e.g. professional drivers, air traffic controllers) where observation is a crucial part of the professional activity.8
Errors in interpretation
An error of interpretation happens at the interpretation phase of film reading and typically consists of an incorrect diagnosis given to an abnormal finding (or, rarely, to a normal finding).
Interpretation errors in radiology can generally be classified into two categories: cognitive and perceptual. Cognitive errors are rare and might be owing to a lack of knowledge or mistaken judgment, for example, and are the minority. Perceptual errors, in which an abnormality is simply not seen, account for up to 80% of radiologic errors.
In a recent review of closed malpractice claims in the USA, radiology was the sixth most frequent specialty involved;13 approximately, three out of four claims against diagnostic radiologists mention errors in interpretation resulting in missed diagnoses.14
There are many explanations why radiologists make errors in interpreting abnormalities. Poor ergonomics and ambient light, recurrent telephone disturbances, working with an inexperienced resident, the absence of clinical history and other factors are important sources of error, especially in the emergency setting.
Failure to suggest the next appropriate procedure
Radiologists must warrant that their suggestions or recommendations for any additional radiological procedures are appropriate and will add significant information to explain, confirm or exclude the initial impression.15,16 Especially in the emergency setting, a radiologist may recommend supplementary imaging procedures (especially CT) that disclose injuries not evident on conventional radiographic examination (Figure 1). Radiologists more completely understand the limitations of radiography for certain diagnoses and can best indicate the need for more advanced imaging, such as CT, for a correct diagnosis in an appropriate time frame.17
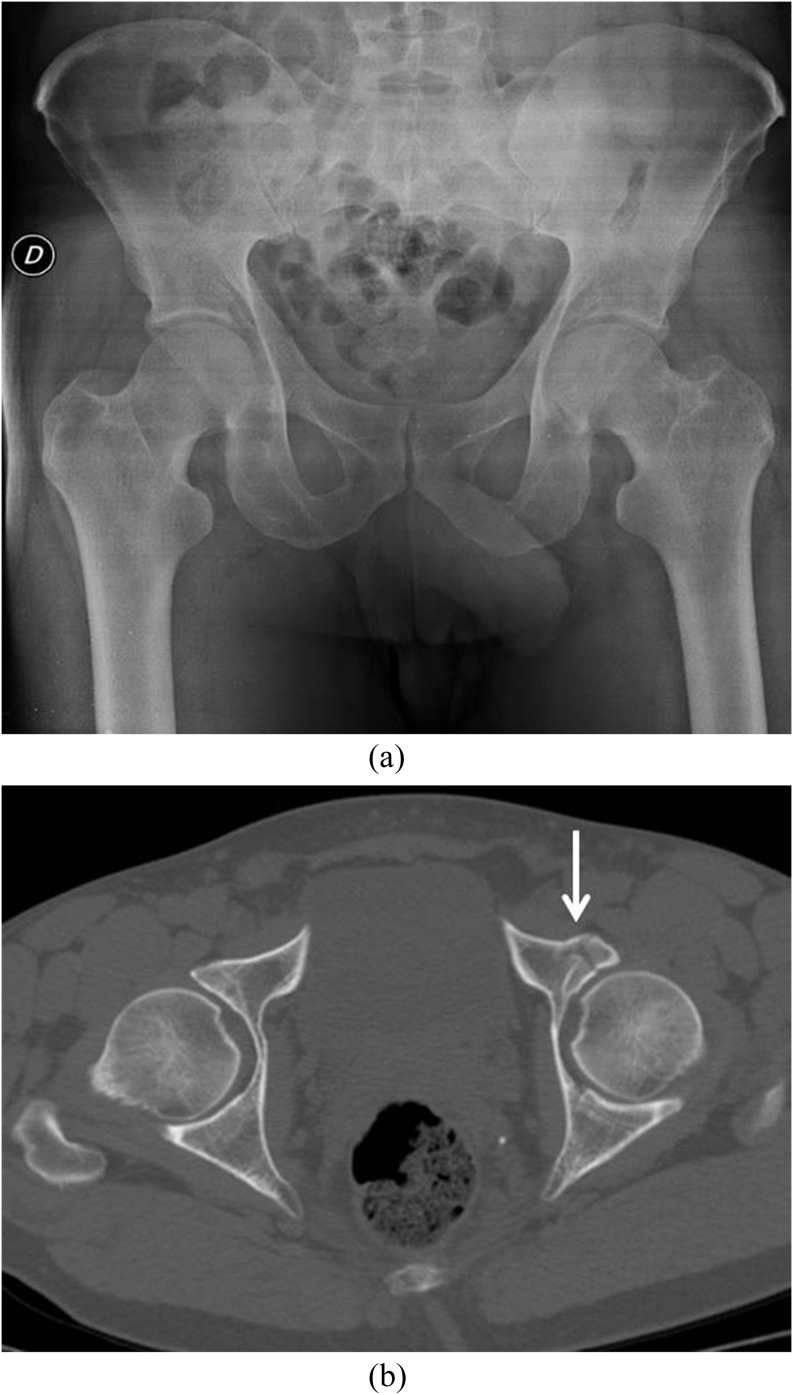
Figure 1.
Anteroposterior radiograph of the pelvis (a): the absence of fracture. The radiologist recommends the need of a CT examination. Subsequent CT (axial section, b) reveals an anterior left-column acetabular fracture (arrow).
Failure to communicate in a timely and clinically appropriate manner
In addition to the final written report, the radiologist is responsible for communicating these findings directly to the referring physician.18 Documentation should include the date, time, name of the person spoken to and what was discussed.8 A radiologist who interprets an imaging examination and writes a report of the results controls what happens to them next.
CAUSES OF ERROR IN EMERGENCY RADIOLOGY
The causes of errors in emergency radiology are multifactorial and frequently joined.11,19 Technical factors such as the quality of images and the views obtained, quantity of clinical information (Figure 2), the absence of previous imaging studies, the reading room atmosphere, the level of alertness of the interpreter, errors of speed, failure of perception, the lack of knowledge, errors in interpretation (Figure 3), SOS, errors due to multitasking, increased workload, rising quality expectations, misjudgement and poorly understood factors seemingly inherent to “human nature” may all play an important role.20–23 Diagnosis of fracture in some anatomical sites is particularly challenging on plain radiographs that remain the primary imaging modality used in the ED. Leading factors contributing to fractures missed on radiographs are the lack of relevant clinical information, inappropriate or insufficient radiographs performed, multiple fractures and severe osteoporosis.
Figure 2.
Plain abdominal radiograph: missed diagnosis of ingested foreign body (arrow). The clinician did not report an adequate history.
Figure 3.
Cross-table lateral radiograph of the abdomen (a). Evidence of a translucent image (arrow) not correctly interpreted as pneumoperitoneum. Subsequent multidetector CT examination (sagittal reconstruction, b) shows the presence of a faecal impaction and the absence of free intraperitoneal air. Fracture of T12 body.
In the ED, a patient with polytrauma is a catalyst for multiple errors as well as serious complications for various reasons: inadequate history, quick life-saving decisions, severity and complexity of the injuries or owing to the patient's pre-existing medical conditions, multiple concurrent tasks and multidisciplinary approach. Moreover, the majority of physicians working at a Level 1 trauma centre include junior medical staff, often still poorly experienced in the management of polytrauma patients.3,24–26
ERRORS IN RADIOGRAPHY IN THE EMERGENCY SETTING
Traditional radiography as the first and widespread procedure for evaluating the appendicular skeleton and skeletal parts of the torso and the chest is limited by its low intrinsic resolution. Plain radiographs are still the main imaging tool in the ED for detecting bony fractures in patients sustaining trauma; two perpendicular imaging views are the lowest requirements to visualize the injured site, even if imaging in two planes may not show non-displaced fractures.27 Failure to identify fractures (Figure 4) is the most common diagnostic error, which may account for 41–80% of diagnostic errors in the ED.4–6,28 Missed or late diagnosis of skeletal injuries, especially those of the appendicular skeleton statistically account for the mainstream of claims in radiography malpractice suits.29
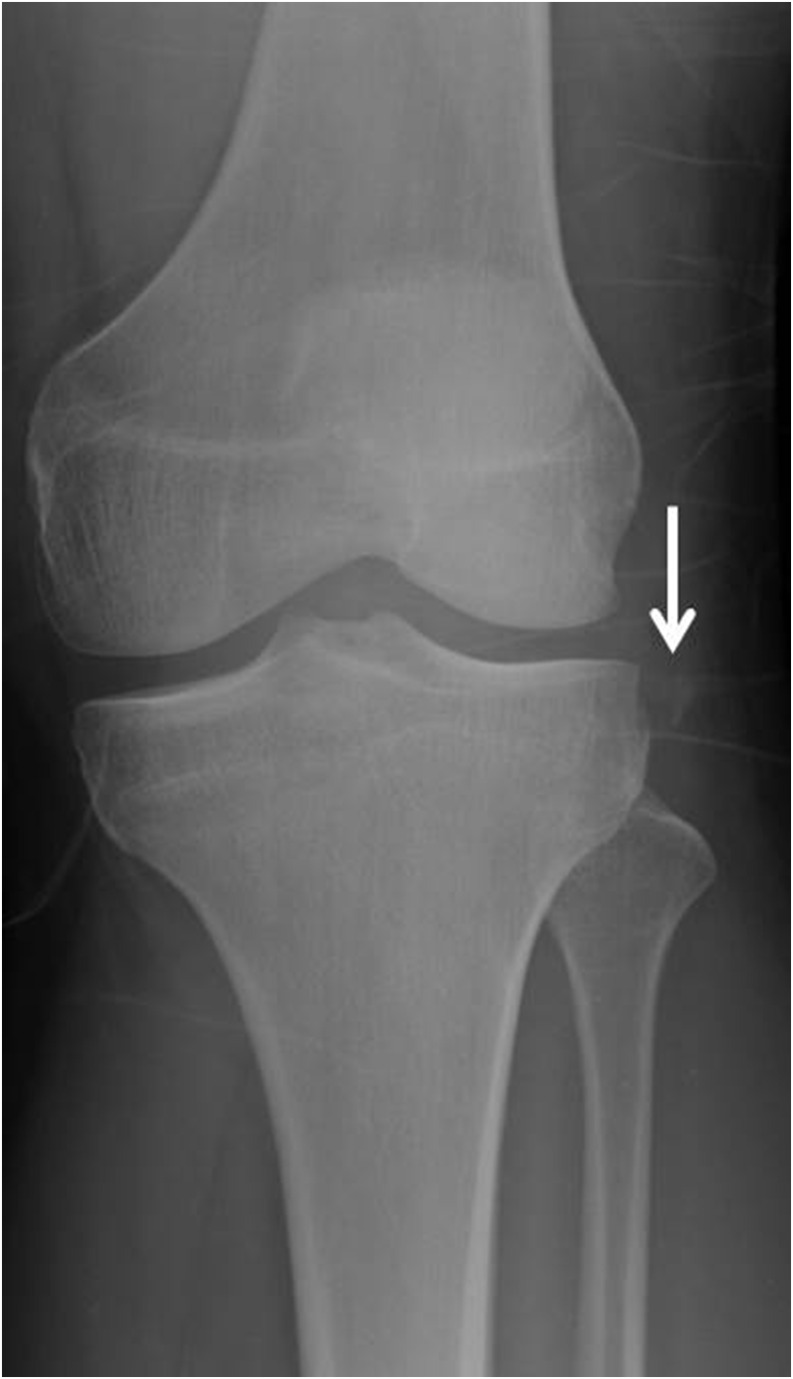
Figure 4.
Missed fracture of the lateral plateau on the anteroposterior view of the knee radiograph (arrow).
Isolated fractures of the scapula are commonly overlooked in interpretation of both chest radiographs and thoracic CT.30 These injuries are important because they indicate the likelihood of significant chest wall impact and may be a cause of pain and limitation of shoulder girdle motion.
Another frequent cause of errors in traditional radiology comprises the evaluation of costal fracture, which can usually be recognized only several days after the traumatic event; injuries to the sternum are also frequently underestimated.31
The anatomical complexity of the wrist commonly results in a misdiagnosis, especially in patients with semilunar dislocations of the carpal and scaphoid bones, both of which can determine disability as well as neurological complications. On the other hand, fracture of the scaphoid bone is associated with 60–70% of all carpal injuries and is the most common form of wrist fracture.32–37 Not surprisingly, it is estimated that up to 40% of scaphoid fractures are missed at first presentation;38 failure to diagnose and immobilize scaphoid injuries can lead to osteoarthritis, malunion, non-union and avascular necrosis, and indeed, non-union occurs in 5–12% of the cases.39,40
A recurring scenario in the ED is hip pain after falling or motor vehicle collision. Evaluation of the hip joint starts with adequate radiographs that include an anteroposterior (AP) pelvic radiograph with accompanying AP and frog leg views of the hip. Even with careful inspection, the incidence of radiographically occult hip fractures ranges from 4% to 9% in patients presenting with pain after trauma;41–43 in fact, visualizing the fracture may be quite subtle owing to overlapping osseous structures.
Fractures in infants and children are different in comparison with fractures involving adults. Some fractures are very subtle and difficult to detect on radiographs. Specific attention should be given to “incomplete fractures”, i.e. hairline fractures (toddler's fracture) and subtle avulsion fractures. In the ED, injuries more often undetected in paediatric patients include fractures of the following segments: hand phalanges, metatarsal bones, distal radius, tibia and phalanges of the foot.44 Moreover, non-displaced greenstick fractures of the wrist, fractures of the scaphoid, skull, zygoma and radial head can be missed on plain radiographs.45 Traumatic vertebral lesions represent about 10% of all misdiagnoses; in particular, at the craniocervical junction (40–50%) and at the cervical–dorsal transition are more commonly involved.46
Standard radiographic assessment of the cervical spine includes at least the following three projections: anteroposterior, cross-table lateral and open mouth odontoid views.47 However, standard radiographs are insufficient for identification of 50% of the fractures detected.48 The American College of Radiologists recommended multidetector CT (MDCT) with multiplanar reconstruction as the procedure of choice in patients with suspected spinal trauma, replacing standard radiographs for patients with a suspicious clinical framework according to the criteria of the National Emergency X-Radiography Utilization Study or the Canadian C-Spine Rule.49
Fractures of the thoracic spine may be easily overlooked when interpreting the frontal chest radiograph in acute blunt trauma patients. The admission chest radiograph in the acute trauma setting is frequently compromised by patient motion, overlying support lines and tubes, and scatter radiation.30
Underdetection of a lumbar spine fracture (Figure 5) is more likely in overweight patients. The frequency of unrecognized spinal injuries seems to be higher when injuries of the hollow viscera are also present, followed by those of the mesentery, solid organs and large vessels;50 moreover, transverse process fractures are identifiable with traditional radiology only in 60% of cases.51
Figure 5.
Lateral radiograph: missed diagnosis of subtle depression of the superior endplate of L1 (arrow).
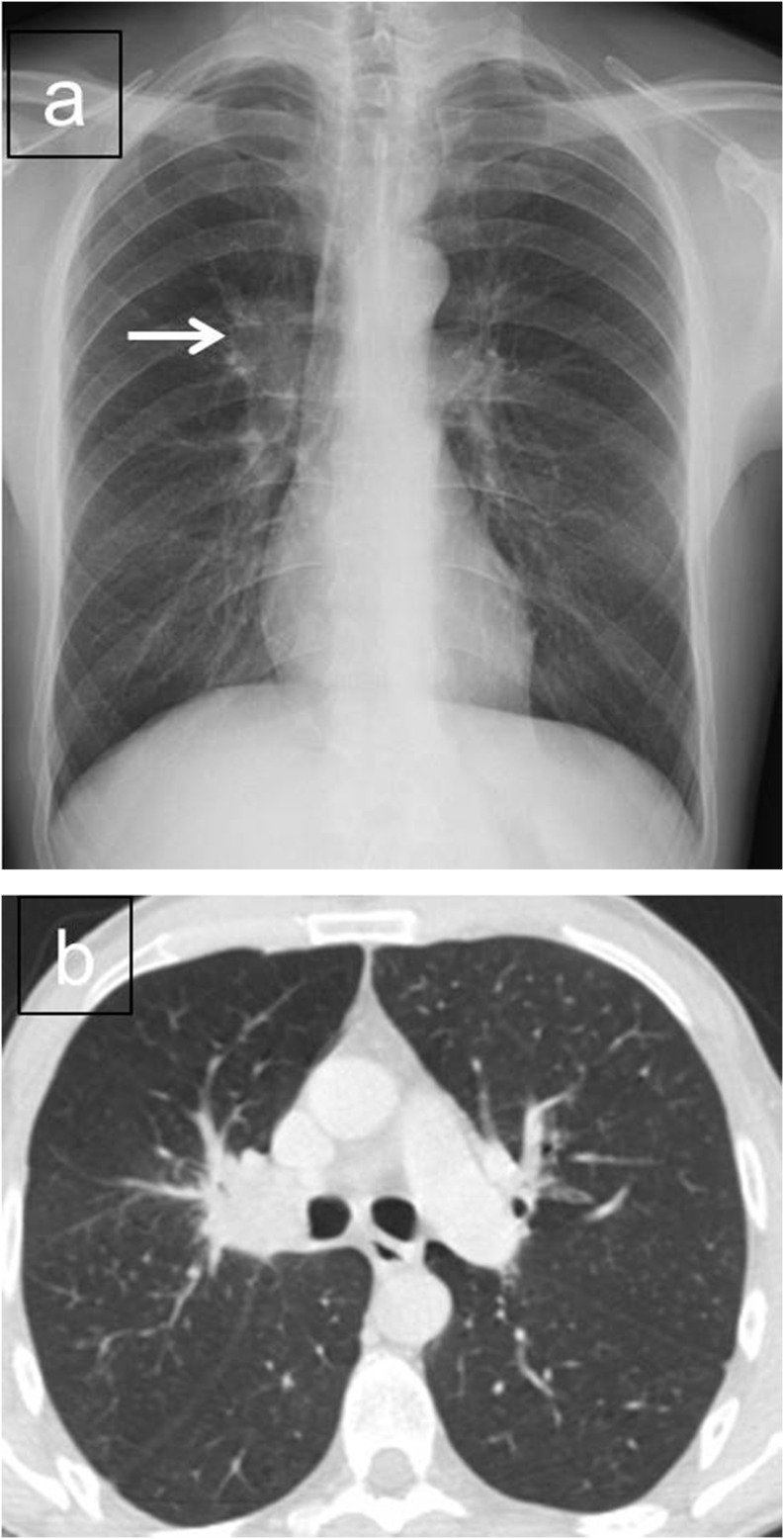
In the emergency setting, the diagnosis of a subtle lung tumour at plain chest film (Figure 6) remains a terrible challenge. Pitfalls of interpretation related to overlapping structures and to the tiny size and low conspicuity typical of several lesions have been reported.52–55 Despite the difficulty to provide the correct diagnosis, missed lung cancer represents the second frequent cause of malpractice claims against radiologists.56 Undetected lung cancers on chest plain films have the following characteristics: (a) most missed neoplastic nodules are subtle, but they are not usually very small (median diameter, 16–20 mm); (b) missed cancers are mainly placed in the upper pulmonary lobes; (c) distracting lesions as well as superposing structures are frequently present; and (d) image quality is commonly low.52,56,57
Figure 6.
Missed lung cancer (arrow) on chest radiograph (a). Corresponding axial CT examination of the same patient outlining the missed lesion (b).
Moreover, lung cancer nodules are frequently missed on chest radiographs by radiologists in clinical practice, especially in the emergency setting, where the single plain chest film is often performed in supine decubitus.
ERRORS IN ULTRASONOGRAPHY IN THE EMERGENCY SETTING
Ultrasonography is an important diagnostic tool for the evaluation of an increasing number of acute non-traumatic abdominal conditions or as the first evaluation of the trauma patient. Ultrasonography imaging can be executed at bedside. Further features of this technique are non-invasive nature, safety and reduced cost, which justify its utilization as a first-line diagnostic procedure in several clinical scenarios.
The causes of errors in emergency ultrasonography are multifactorial and, as in other diagnostic imaging techniques,58–61 are frequently seen at the same time and include the lack of attention to the clinical history and examination, low knowledge of the technical equipment, employment of inappropriate probes, incorrect optimization of the images, poor communication with the patient, lack of perception, reduced knowledge of the differential diagnoses, overestimation of one's own skill and failure to indicate other ultrasonography examinations or further imaging techniques, such as CT or MRI.62–65
In the management of polytrauma patients, an error can raise the mortality and morbidity rate, and more frequently, errors in radiology occur during traditional imaging studies, i.e. plain radiographs and ultrasonography examinations, owing to their inherent low resolution and/or restricted field of view. Ultrasonography represents an operator-dependent examination, therefore it is crucial that the operator is well trained in emergency radiology in order to be able to implement the diagnostic capabilities of this technique.62 As a first step in correct ultrasonography scanning, the sonographer must be aware of the mechanism of the injury, patient's symptoms and clinical findings.66,67 Furthermore, the operator should consider the patient in terms of the physical constitution (in obese patients, the thickness of the subcutaneous fat can reduce the ultrasonography diagnostic capabilities because of wide sound attenuation) and the presence of conditions possibly limiting the examination, such as obliged decubitus, scars, asking for more comprehensive diagnostic imaging procedures (multidetector row CT).63
ERRORS IN CT IN THE EMERGENCY SETTING
The correct use of advanced diagnostic procedure, which in many thoracoabdominal non-traumatic emergencies and in polytrauma patients almost exclusively involves the use of contrast-enhanced MDCT, may tangibly reduce the amount of diagnostic errors associated with the use of traditional procedures. This is due to the high sensitivity and accuracy intrinsic to MDCT in the assessment of patients in the emergency setting.68 The important information obtained from correctly performed contrast-enhanced MDCT studies accounts for the “gold standard” rating of this technique in the assessment of major trauma. However, the use of contrast-enhanced MDCT is not immune to the possibility of errors.69,70
Since one of the leading causes of death in polytrauma patients is massive monolateral or bilateral pneumothorax, it is crucial for the radiologist to carefully evaluate the CT scout view of the contrast-enhanced MDCT study. Another common situation that may produce errors is the inadequate flow of intravenously injected contrast material. Consequently, adequate catheter access and a flow rate of intravenous contrast of 3.5 ml s−1 or higher should be established, as such conditions will help for the correct identification of vascular injuries. In fact, in polytrauma patients, the correct characterization of such injuries is crucial; the site of vascular contrast extravasation (blush) must be identified and the nature of the extravasation must be characterized, which is possible using the recent MDCT equipments.71 A correct multiphase CT study will discriminate all sites of active arterial bleeding in the early contrast-enhanced phase from the slower venous bleeding characteristic of the portal and late phases, allowing the identification and characterization of pseudoaneurysms and arterovenous fistulas, which would otherwise remain underestimated.46,72–75
Injuries of the diaphragm are not common and represent 5% of missed injuries, half of which are not recognised in the first 24 h after the traumatic event.76 Diagnosis of the injured diaphragm is particularly difficult,77 resulting in a late diagnosis, and some studies77,78 have reported that the sensitivity CT examination for the diagnosis of fractures of the diaphragm is relatively low (50–73%).
In abdominal traumas, a significant cause of errors is the presence of respiration artefacts on the images. These are characteristically identified, presenting as an indistinct margin of the scanned vascular structures associated with hyperechoic bands near the adjacent parenchymatous organs and hollow viscera.
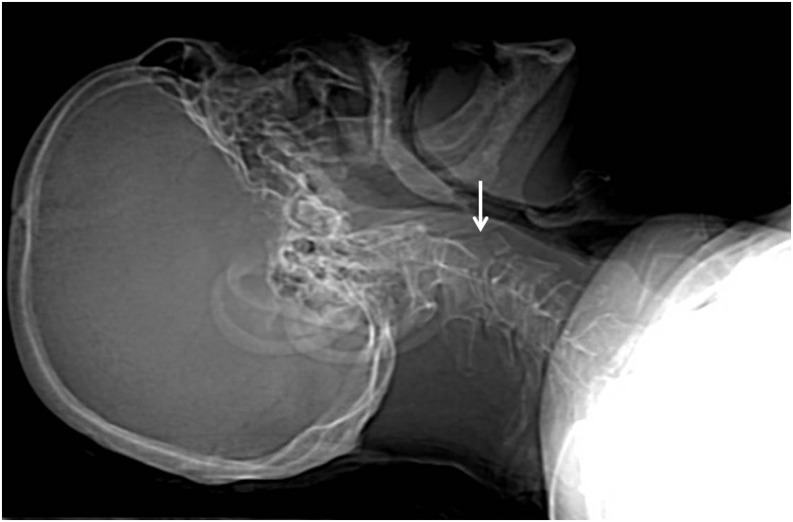
Moreover, the CT scout view need to be routinely reviewed as part of the CT interpretation, in order to avoid misdiagnosis of significant pathological findings (Figure 7).79
Figure 7.
CT examination of the brain. Missed diagnosis of fracture of C2 body on CT scout view (arrow).
In the evaluation of patients with acute non-traumatic thoracic or abdominal pain, diagnostic errors in CT examinations can arise from the use of an inadequate CT protocol; moreover, normal anatomical structures or anatomic variants may represent potential pitfalls in that they can mimic pathological entities.
Technical parameters of CT scans (region of interest, use of a contrast agent and scanning timing) differ according to the clinical suspected diseases, and if performed under inappropriate conditions, CT images will not provide appropriate information for diagnosis. Thus, to avoid missing positive CT findings, in addition to careful readings, radiologists need to obtain such patient information from clinicians.80–82
HOW TO REDUCE ERRORS IN EMERGENCY RADIOLOGY
The problem of misdiagnosis cannot be solved without education, but it cannot also be solved with education alone.83
In the emergency setting, diagnostic errors can be reduced by increases in both knowledge and systems. Key elements are communication of the patient's clinical history, comparison of the current imaging procedure with the previous radiological investigation and the correct selection of the initial and subsequent radiological procedure.22 Better system organization arises from improvements in working conditions and the time available for reporting, equipment changes to prevent accidental error, double reporting and in good communication between clinicians and radiologists.22
Learning from errors needs a serious review of our own practice and the employment of change to increase performance levels. Peer review is essential in order to evaluate radiologists' performance and to increase diagnostic accuracy.
In order to decrease the likelihood of diagnostic errors, we recommend to be part of educational programs and morbidity meetings, as well as to perform a comprehensive and respected root cause analysis process.
SUMMARY
EDs face an increasing number of diagnostic problems, with several medicolegal consequences. Radiographs remain the mainstay for fracture assessment, and their assessment remains challenging. On plain radiographs, an error in diagnosing a bone fracture can occur because it is radiologically imperceptible or equivocal; indeed, some subtle and non-displaced fractures may be radiographically occult. Accordingly, in patients with negative plain radiographs and high clinical suspicion of occult fracture, a diagnostic error may arise if the radiologist does not highlight in the report the need of other more appropriate examinations.
Radiologists play a pivotal role in the diagnostic assessment of polytrauma patients, and key elements to reduce errors in the emergency setting are knowledge, experience and correct application of imaging protocols.
It is crucial to encourage a safety culture within radiology departments, where in presence of a diagnostic error made by a colleague, we discuss it together with the department's medical staff in a constructive fashion.
Contributor Information
Antonio Pinto, Email: antoniopinto_pa@libero.it.
Fabio Pinto, Email: fpinto1966@libero.it.
REFERENCES
- 1.Busardò FP, Frati P, Santurro A, Zaami S, Fineschi V. Errors and malpractice lawsuits in radiology: what the radiologist needs to know. Radiol Med 2015; 120: 779–84. doi: 10.1007/s11547-015-0561-x [DOI] [PubMed] [Google Scholar]
- 2.Caranci F, Tedeschi E, Leone G, Reginelli A, Gatta G, Pinto A, et al. Errors in neuroradiology. Radiol Med 2015; 120: 795–801. doi: 10.1007/s11547-015-0564-7 [DOI] [PubMed] [Google Scholar]
- 3.West RW. Radiology malpractice in the emergency room setting. Emerg Radiol 2000; 7: 14–18. doi: 10.1007/s101400050004 [DOI] [Google Scholar]
- 4.Wei CJ, Tsai WC, Tiu CM, Wu HT, Chiou HJ, Chang CY. Systematic analysis of missed extremity fractures in emergency radiology. Acta Radiol 2006; 47: 710–17. doi: 10.1080/02841850600806340 [DOI] [PubMed] [Google Scholar]
- 5.Guly HR. Diagnostic errors in an accident and emergency department. Emerg Med J 2001; 18: 263–9. doi: 10.1136/emj.18.4.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berlin L. Defending the “missed” radiographic diagnosis. AJR Am J Roentgenol 2001; 176: 317–22. doi: 10.2214/ajr.176.2.1760317 [DOI] [PubMed] [Google Scholar]
- 7.Graber M. Diagnostic errors in medicine: a case of neglect. Jt Comm J Qual Patient Saf 2005; 31: 106–13. [DOI] [PubMed] [Google Scholar]
- 8.Pinto A, Brunese L. Spectrum of diagnostic errors in radiology. World J Radiol 2010; 2: 377–83. doi: 10.4329/wjr.v2.i10.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kundel HL, Nodine CF, Carmody D. Visual scanning, pattern recognition and decision-making in pulmonary nodule detection. Invest Radiol 1978; 13: 175–81. doi: 10.1097/00004424-197805000-00001 [DOI] [PubMed] [Google Scholar]
- 10.Samuel S, Kundel HL, Nodine CF, Toto LC. Mechanism of satisfaction of search: eye position recordings in the reading of chest radiographs. Radiology 1995; 194: 895–902. doi: 10.1148/radiology.194.3.7862998 [DOI] [PubMed] [Google Scholar]
- 11.Tuddenham WJ. Visual search, image organization, and reader error in roentgen diagnosis: studies of the psychophysiology of roentgen image perception. Radiology 1962; 78: 694–704. doi: 10.1148/78.5.694 [DOI] [PubMed] [Google Scholar]
- 12.Yerushalmy J. The statistical assessment of the variability in observer perception and description of roentgenographic pulmonary shadows. Radiol Clin North Am 1969; 7: 381–92. [PubMed] [Google Scholar]
- 13.Whang JS, Baker SR, Patel R, Luk L, Castro A, 3rd. The causes of medical malpractice suits against radiologists in the United States. Radiology 2013; 266: 548–54. doi: 10.1148/radiol.12111119 [DOI] [PubMed] [Google Scholar]
- 14.Berlin L, Berlin JW. Malpractice and radiologists in Cook County, IL: trends in 20 years of litigation. AJR Am J Roentgenol 1995; 165: 781–8. doi: 10.2214/ajr.165.4.7676967 [DOI] [PubMed] [Google Scholar]
- 15.American College of Radiology. ACR practice guideline for communication of diagnostic imaging findings. In: 2005 practice guideline & technical standards. Reston, VA: American College of Radiology; 2005. pp. 5–9. [Google Scholar]
- 16.Berlin L. Errors of omission. AJR Am J Roentgenol 2005; 185: 1416–21. doi: 10.2214/AJR.05.0838 [DOI] [PubMed] [Google Scholar]
- 17.Gyftopoulos S, Chitkara M, Bencardino JT. Misses and errors in upper extremity trauma radiographs. AJR Am J Roentgenol 2014; 203: 477–91. doi: 10.2214/AJR.14.12589 [DOI] [PubMed] [Google Scholar]
- 18.Harrigal CL, Erly WK. On-call radiology: community standards and current trends. Semin Ultrasound CT MR 2007; 28: 85–93. doi: 10.1053/j.sult.2007.01.007 [DOI] [PubMed] [Google Scholar]
- 19.FitzGerald R. Error in radiology. Clin Radiol 2001; 56: 938–46. doi: 10.1053/crad.2001.0858 [DOI] [PubMed] [Google Scholar]
- 20.Robinson PJA. Radiology's Achilles' heel: error and variation in the interpretation of the Roentgen image. Br J Radiol 1997; 70: 1085–98. doi: 10.1259/bjr.70.839.9536897 [DOI] [PubMed] [Google Scholar]
- 21.Pinto A, Acampora C, Pinto F, Kourdioukova E, Romano L, Verstraete K. Learning from diagnostic errors: a good way to improve education in radiology. Eur J Radiol 2011; 78: 372–6. doi: 10.1016/j.ejrad.2010.12.028 [DOI] [PubMed] [Google Scholar]
- 22.Goddard P, Leslie A, Jones A, Wakeley C, Kabala J. Error in radiology. Br J Radiol 2001; 74: 949–51. doi: 10.1259/bjr.74.886.740949 [DOI] [PubMed] [Google Scholar]
- 23.Leslie A, Jones AJ, Goddard PR. The influence of clinical information on the reporting of CT by radiologists. Br J Radiol 2000; 73: 1052–5. doi: 10.1259/bjr.73.874.11271897 [DOI] [PubMed] [Google Scholar]
- 24.Scaglione M, Iaselli F, Sica G, Feragalli B, Refky N. Errors in imaging of traumatic injuries. Abdom Imaging 2015; 40: 2091–8. doi: 10.1007/s00261-015-0494-9 [DOI] [PubMed] [Google Scholar]
- 25.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2,594 deaths. Ann Surg 2006; 244: 371–80. doi: 10.1097/01.sla.0000234655.83517.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buduhan G, McRitchie DI. Missed injuries in patients with multiple trauma. J Trauma 2000; 49: 600–5. doi: 10.1097/00005373-200010000-00005 [DOI] [PubMed] [Google Scholar]
- 27.Greenspan A, Norman A, Rosen H. Radial head-capitellum view in elbow trauma: clinical application and radiographic-anatomic correlation. AJR Am J Roentgenol 1984; 143: 355–9. doi: 10.2214/ajr.143.2.355 [DOI] [PubMed] [Google Scholar]
- 28.Williams SM, Connelly DJ, Wadsworth S, Wilson DJ. Radiological review of accident and emergency radiographs: a 1-year audit. Clin Radiol 2000; 55: 861–5. doi: 10.1053/crad.2000.0548 [DOI] [PubMed] [Google Scholar]
- 29.Brooks A, Holroyd B, Riley B. Missed injury in major trauma patients. Injury 2004; 35: 407–10. doi: 10.1016/S0020-1383(03)00219-5 [DOI] [PubMed] [Google Scholar]
- 30.Mirvis SE. Diagnostic imaging of thoracic trauma. In: Mirvis SE, Shanmuganathan K, eds. Imaging in trauma and critical care. 2nd edn. Philadelphia, PA: Saunders; 2003. pp. 297–367. [Google Scholar]
- 31.Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994; 37: 975–9. doi: 10.1097/00005373-199412000-00018 [DOI] [PubMed] [Google Scholar]
- 32.Ring D, Jupiter JB, Herndon JH. Acute fractures of the scaphoid. J Am Acad Orthop Surg 2000; 8: 225–31. [DOI] [PubMed] [Google Scholar]
- 33.Ritchie JV, Munter DW. Emergency department evaluation and treatment of wrist injuries. Emerg Med Clin North Am 1999; 17: 823–42. doi: 10.1016/S0733-8627(05)70099-7 [DOI] [PubMed] [Google Scholar]
- 34.Berger RA. The ligaments of the wrist: a current overview of anatomy with consideration of their potential functions. Hand Clin 1997; 13: 63–82. [PubMed] [Google Scholar]
- 35.Nguyen DT, McCue FC, Urch SE. Evaluation of the injured wrist on the field and in the office. Clin Sports Med 1998; 17: 421–32. doi: 10.1016/S0278-5919(05)70094-6 [DOI] [PubMed] [Google Scholar]
- 36.Zemel MP, Stark HH. Fractures and dislocations of the carpal bones. Clin Sports Med 1986; 5: 709–23. [PubMed] [Google Scholar]
- 37.Wackerle JF. A prospective study identifying the sensitivity of radiographic findings and the efficacy of clinical findings in carpal navicular fractures. Ann Emerg Med 1987; 16: 733–7. [DOI] [PubMed] [Google Scholar]
- 38.Waizengger M, Barton NJ, David TR, Wastie ML. Clinical signs in scaphoid fractures. J Hand Surg Br 1994; 19: 743–6. [DOI] [PubMed] [Google Scholar]
- 39.Leslie IJ, Dickson RA. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg Br 1981; 63: 225–30. [DOI] [PubMed] [Google Scholar]
- 40.Dias JJ, Brenkel IJ, Finlay DB. Patterns of non union in fractures in the waist of scaphoid. J Bone Joint Surg Br 1989; 71: 307–10. [DOI] [PubMed] [Google Scholar]
- 41.Yu JS. Easily missed fractures in the lower extremity. Radiol Clin N Am 2015; 53: 737–55. doi: 10.1016/j.rcl.2015.02.003 [DOI] [PubMed] [Google Scholar]
- 42.Dominguez S, Liu P, Roberts C, Mandell M, Richman PB. Prevalence of traumatic hip and pelvic fractures in patients with suspected hip fracture and negative initial standard radiographs—a study of emergency department patients. Acad Emerg Med 2005; 12: 366–70. [DOI] [PubMed] [Google Scholar]
- 43.Parker MJ. Missed hip fractures. Arch Emerg Med 1992; 9: 23–7. doi: 10.1136/emj.9.1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hernandez JA, Swischuk LE, Yngve DA, Carmichael KD. The angled buckle fracture in pediatrics: a frequently missed fracture. Emerg Radiol 2003; 10: 71–5. doi: 10.1007/s10140-003-0288-1 [DOI] [PubMed] [Google Scholar]
- 45.Wardrope J, Chennells PM. Should all casualty radiographs be reviewed? Br Med J (Clin Res Ed) 1985; 290: 1638–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Guida F, Bocchini G, Sica G, Frezza A, Scaglione M. Errors in polytrauma. In: Romano L, Pinto A, eds. Errors in radiology. Springer-Verlag, Italia; 2012. pp. 27–37. [Google Scholar]
- 47.Woodring JH, Lee C. The role and limitations of computed tomographic scanning in the evaluation of cervical trauma. J Trauma 1993; 34: 32–9. doi: 10.1097/00005373-199301000-00006 [DOI] [PubMed] [Google Scholar]
- 48.Davis JW, Phreaner DL, Hoyt DB, Mackersie RC. The etiology of missed cervical spine injuries. J Trauma 1993; 34: 342–6. doi: 10.1097/00005373-199303000-00006 [DOI] [PubMed] [Google Scholar]
- 49.Daffner RH, Weissman BN, Wippold FJ, II, Angtuaco EJ, Appel M, Berger KL, et al. ACR appropriateness criteria® suspected spine trauma. [online publication]. Reston, VA: American College of Radiology (ACR); 2012. [Google Scholar]
- 50.Beaunoyer M, St-Vil D, Lallier M, Blanchard H, et al. Abdominal injuries associated with thoracolumbar fractures after motor vehicle collision. J Pediatr Surg 2001; 36: 760–2. doi: 10.1053/jpsu.2001.22954 [DOI] [PubMed] [Google Scholar]
- 51.Krueger MA, Green DA, Hoyt D, Garfin SR. Overlooked spine injuries associated with lumbar transverse process fractures. Clin Orthop 1996; 327: 191–5. doi: 10.1097/00003086-199606000-00024 [DOI] [PubMed] [Google Scholar]
- 52.Quekel LG, Kessels AG, Goei R, van Engelshoven JM. Miss rate of lung cancer on the chest radiograph in clinical practice. Chest 1999; 115: 720–4. doi: 10.1378/chest.115.3.720 [DOI] [PubMed] [Google Scholar]
- 53.Monnier-Cholley L, Arrive L, Porcel A, Shehata K, Dahan H, Urban T, et al. Characteristics of missed lung cancer on chest radiographs: a French experience. Eur Radiol 2001; 11: 597–605. doi: 10.1007/s003300000595 [DOI] [PubMed] [Google Scholar]
- 54.Shah PK, Austin JH, White CS, Patel P, Haramati LB, Pearson GD, et al. Missed non-small cell lung cancer: radiographic findings of potentially resectable lesions evident only in retrospect. Radiology 2003; 226: 235–41. doi: 10.1148/radiol.2261011924 [DOI] [PubMed] [Google Scholar]
- 55.Turkington PM, Kennan N, Greenstone MA. Misinterpretation of the chest x ray as a factor in the delayed diagnosis of lung cancer. Postgrad Med J 2002; 78: 158–60. doi: 10.1136/pmj.78.917.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.White CS, Salis AI, Meyer CA. Missed lung cancer on chest radiography and computed tomography: imaging and medicolegal issues. J Thorac Imaging 1999; 14: 63–8. doi: 10.1097/00005382-199901000-00006 [DOI] [PubMed] [Google Scholar]
- 57.Fardanesh M, White C. Missed lung cancer on chest radiography and computed tomography. Semin Ultrasound CT MRI 2012; 33: 280–7. doi: 10.1053/j.sult.2012.01.006 [DOI] [PubMed] [Google Scholar]
- 58.Caranci F, Cicala D, Cappabianca S, Briganti F, Brunese L, Fonio P. Orbital fractures: role of imaging. Semin Ultrasound CT MR 2012; 33: 385–91. doi: 10.1053/j.sult.2012.06.007 [DOI] [PubMed] [Google Scholar]
- 59.Reginelli A, Mandato Y, Solazzo A, Berritto D, Iacobellis F, Grassi R. Errors in the radiological evaluation of the alimentary tract: part II. Semin Ultrasound CT MR 2012; 33: 308–17. doi: 10.1053/j.sult.2012.01.016 [DOI] [PubMed] [Google Scholar]
- 60.Mandato Y, Reginelli A, Galasso R, Iacobellis F, Berritto D, Cappabianca S. Errors in the radiological evaluation of the alimentary tract: part I. Semin Ultrasound CT MR 2012; 33: 300–7. doi: 10.1053/j.sult.2012.01.011 [DOI] [PubMed] [Google Scholar]
- 61.Caranci F, Brunese L, Reginelli A, Napoli M, Fonio P, Briganti F. Neck neoplastic conditions in the emergency setting: role of multidetector computed tomography. Semin Ultrasound CT MR 2012; 33: 443–8. doi: 10.1053/j.sult.2012.06.011 [DOI] [PubMed] [Google Scholar]
- 62.Farina R, Sparano A. Errors in sonography. In: Romano L, Pinto A, eds. Errors in radiology. Springer-Verlag Italy; 2012: 79–85. [Google Scholar]
- 63.Pinto A, Pinto F, Faggian A, Rubini G, Caranci F, Macarini L, et al. Sources of error in emergency ultrasonography. Crit Ultrasound J 2013; 5(Suppl. 1): S1. doi: 10.1186/2036-7902-5-S1-S1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Casciani E, De Vincentiis C, Mazzei MA, Masselli G, Guerrini S, Polettini E, et al. Errors in imaging the pregnant patient with acute abdomen. Abdom Imaging 2015; 40: 2112–26. doi: 10.1007/s00261-015-0508-7 [DOI] [PubMed] [Google Scholar]
- 65.Chang PT, Schooler GR, Lee EY. Diagnostic errors of right lower quadrant pain in children: beyond appendicitis. Abdom Imaging 2015; 40: 2071–90. doi: 10.1007/s00261-015-0482-0 [DOI] [PubMed] [Google Scholar]
- 66.Stone PC, Hilton CF. Medicolegal aspects of emergency department radiology. Radiol Clin North Am 1992; 30: 495–501. [PubMed] [Google Scholar]
- 67.Berbaum KS, Franken EA, Dorfman DD, Barloon TJ. Influence of clinical history upon detection of nodules and other lesions. Invest Radiol 1988; 23: 48–55. doi: 10.1097/00004424-198801000-00011 [DOI] [PubMed] [Google Scholar]
- 68.Reginelli A, Pinto A, Russo A, Fontanella G, Rossi C, Del Prete A, et al. Sharp penetrating wounds: spectrum of imaging findings and legal aspects in the emergency setting. Radiol Med 2015; 120: 856–65. doi: 10.1007/s11547-015-0553-x [DOI] [PubMed] [Google Scholar]
- 69.West OC, Anderson J, Lee SJ, Finnell CW, Ravak BK. Patterns of diagnostic error in trauma abdominal CT. Emerg Radiol 2002; 9: 195–200. doi: 10.1007/s10140-002-0225-8 [DOI] [PubMed] [Google Scholar]
- 70.Mazzei MA, Volterrani L. Errors in multidetector row computed tomography. Radiol Med 2015; 120: 785–94. doi: 10.1007/s11547-015-0558-5 [DOI] [PubMed] [Google Scholar]
- 71.Schueller G, Scaglione M, Linsenmaier U, SchuellerWeidekamm C, Andreoli C, De Vargas Macciucca M, et al. The key role of the radiologist in the management of polytrauma patients: indications for MDCT imaging in emergency radiology. Radiol Med 2015; 120: 641–54. doi: 10.1007/s11547-015-0500-x [DOI] [PubMed] [Google Scholar]
- 72.Sica G, Bocchini G, Guida F, Tanga M, Guaglione M, Scaglione M. Multidetector computed tomography in the diagnosis and management of renal trauma. Radiol Med 2010; 115: 936–49. doi: 10.1007/s11547-010-0565-5 [DOI] [PubMed] [Google Scholar]
- 73.Sica G, Guida F, Bocchini G, Codella U, Mainenti PP, Tanga M, et al. Errors in imaging assessment of polytrauma patients. Semin Ultrasound CT MR 2012; 33: 337–46. doi: 10.1053/j.sult.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 74.Scaglione M, Romano L, Bocchini G, Sica G, Guida F, Pinto A, et al. Multidetector computed tomography of pancreatic, small bowel, and mesenteric traumas. Semin Roentgenol 2012; 47: 362–70. doi: 10.1053/j.ro.2012.05.005 [DOI] [PubMed] [Google Scholar]
- 75.Caleo O, Bocchini G, Paoletta S, Ierardi AM, Scionti A, Tonerini M, et al. Spontaneous non-aortic retroperitoneal hemorrhage: etiology, imaging characterization and impact of MDCT on management. A multicentric study. Radiol Med 2015; 120: 133–48. doi: 10.1007/s11547-014-0482-0 [DOI] [PubMed] [Google Scholar]
- 76.Voeller GR, Reisser JR, Fabian TC, Kudsk K, Mangiante EC. Blunt diaphragm injuries. A five-year experience. Am Surg 1990; 56: 28–31. [PubMed] [Google Scholar]
- 77.Reber PU, Schmied B, Seiler CA, Baer HU, Patel AG, Büchler MW. Missed diaphragmatic injuries and their long-term sequelae. J Trauma 1998; 44: 183–8. doi: 10.1097/00005373-199801000-00026 [DOI] [PubMed] [Google Scholar]
- 78.Demos TC, Solomon C, Posniak HV, Flisak MJ. Computed tomography in traumatic defects of the diaphragm. Clin Imaging 1989; 13: 62–7. doi: 10.1016/0899-7071(89)90128-9 [DOI] [PubMed] [Google Scholar]
- 79.Johnson PT, Scott WW, Gayler BW, Lewin JS, Fishman EK The CT scout view: does it need to be routinely reviewed as part of the CT interpretation? AJR Am J Roentgenol 2014; 202: 1256–63. doi: 10.2214/AJR.13.10545 [DOI] [PubMed] [Google Scholar]
- 80.Suzuki S, Ikusaka M, Ohira Y, Miyahara M, Noda K, Kajiwara H, et al. Effect of diagnostic predictions combined with clinical information on avoiding perceptual errors of computed tomography. Jpn J Radiol 2013; 31: 731–6. doi: 10.1007/s11604-013-0244-2 [DOI] [PubMed] [Google Scholar]
- 81.Lo Re G, Cappello M, Tudisca C, Galia M, Randazzo C, Craxì A, et al. CT enterography as a powerful tool for the evaluation of inflammatory activity in Crohn's disease: relationship of CT findings with CDAI and acute-phase reactants. Radiol Med 2014; 119: 658–66. doi: 10.1007/s11547-013-0377-5 [DOI] [PubMed] [Google Scholar]
- 82.Lo Re G, Galia M, Bartolotta TV, Runza G, Taibbi A, Lagalla R, et al. Forty-slice MDCT enteroclysis: evaluation after oral administration of isotonic solution in Crohn's disease. Radiol Med 2007; 112: 787–97. doi: 10.1007/s11547-007-0187-8 [DOI] [PubMed] [Google Scholar]
- 83.Lee CS, Nagy PG, Weaver SJ, Newman-Toker DE. Cognitive and system factors contributing to diagnostic errors in radiology. AJR Am J Roentgenol 2013; 201: 611–17. doi: 10.2214/AJR.12.10375 [DOI] [PubMed] [Google Scholar]