Abstract
Acute vascular injuries are the second most common cause of fatalities in patients with multiple traumatic injuries; thus, prompt identification and management is essential for patient survival. Over the past few years, multidetector CT (MDCT) using dual-phase scanning protocol has become the imaging modality of choice in high-energy deceleration traumas. The objective of this article was to review the role of dual-phase MDCT in the identification and management of acute vascular injuries, particularly in the chest and abdomen following multiple traumatic injuries. In addition, this article will provide examples of MDCT features of acute vascular injuries with correlative surgical and interventional findings.
INTRODUCTION
Trauma is one of most common causes of death or permanent disability in people younger than age 40 years and constitutes a serious medical dilemma.1–3 It is usually due to blunt force from deceleration, compression or impaction,4,5 particularly in motor vehicle collisions,6,7 which occur at a speed >65 km h−1 or in a motorcycle collision faster than 35 km h−1.8 With traumatic injuries, a timely approach is crucial; thus, the most appropriate imaging modality is necessary. Multidetector CT (MDCT) with intravenous contrast is excellent at detection and characterization of life-threatening injuries within seconds.8–10
Acute vascular injuries are the second most common cause of death in patients with high-energy polytrauma.11–13 Therefore, the identification and characterization of these injuries is important in order to direct management. An initial CT is important in the assessment of acute vascular injuries in order to determine whether a surgical, interventional or non-operative management is necessary.14–17
Vessel injuries may not be initially diagnosed if the patient is stable and the clinical suspicion is low and so, a high index of suspicion and detailed history such as the mechanism of the trauma is important. The diagnosis of acute vascular injuries usually depends on multiple factors such as radiologist experience, the presence of distraction injuries, lack of correlation with clinical presentation or inadequate CT scan protocol. Frequently, the detection and characterization of vessel injuries is limited because a single-phase CT was used instead of a dual-phase CT protocol.14,18,19
The purpose of this review article was to illustrate the value of dual-phase MDCT protocol in the identification and characterization of acute vascular injuries in the chest and abdomen in patients with high-energy trauma. The correlation between the CT features of vascular injuries and surgical/interventional findings will be discussed.
Multidetector CT PROTOCOL
MDCT is the primary imaging method for the evaluation of the entire chest and abdomen in patients with high-energy blunt trauma7,15 and is the primary tool to evaluate patients with suspected acute vascular injuries.10 CT has replaced catheter angiography as the primary screening study.15,20 However, CT examination protocols are still not standardized. In the emergency settings, all the examinations should be performed with the use of intravenous contrast and with a multiphasic, high-resolution protocol, with slice thickness and reconstruction interval values of about 1 mm, complete with multiplanar reconstructions and maximum intensity projection. At our institution, all examinations are performed by a 128-slice MDCT (Siemens SOMATOM® Definition Flash, Siemens Healthcare), with slice thickness of 1.2 mm, collimation of 2 × 128 × 0.6 mm and rotation time of 0.28 s. The patient should be positioned supine with the arms abducted, if possible.10,21
Basically, a dual-phase MDCT protocol includes a basal scan of the skull followed by an arterial phase from the circle of Willis to the symphysis pubis and venous phase from the diaphragm to the symphysis pubis. All the CT examinations are performed under the supervision of a consultant radiologist who provides full coverage 24 hours per day, 7 days per week. She or he will briefly review the CT scans when the patient is still in the CT scanner; thus, he or she will recommend additional phases (i.e. excretory phase) if required. An intravenous contrast material consists in 100–120 ml of iodinated contrast agent (Iomeron 400; Bracco Diagnostics, Milan, Italy) at 400 mg ml−1 concentration injected at 4–5 ml s−1, followed by 40 ml of saline chaser at the same flow rate to obtain optimal vessel depiction.
An automated bolus tracking, with region of interest placed in the aortic arch at an attenuation threshold of 100 HU, is used to time the beginning of the arterial phase. The venous phase is performed at 60–70-s delay from the end of the injection. Three-dimensional multiplanar reconstructions and maximum intensity projection are routinely performed to display the vessel anatomy and look for possible injuries. A delayed, excretory phase (180-s delay from the end of the venous phase or later) can be added in select cases, if there is suspected injury to the collecting system or bladder.
WHY IS A DUAL-PHASE MDCT PROTOCOL NECESSARY?
In patients with high-energy blunt trauma, significant vascular injuries may be unsuspected at the arrival at the emergency department, as their presence become clinically evident only when the shock status or haemodynamic instability occurs.1,22 To avoid underestimation, the choice of an appropriate dual-phase protocol, including the arterial and venous phases, is crucial.
When an acute vascular injury is detected, it is important to identify the vessel, type of vessel (arterial or venous) and type of injury, since this will affect management. Acute vascular injures encompass a wide spectrum of findings, ranging from spasm, intimal tears, intramural haematoma, pseudoaneurysms, arteriovenous fistula (AVF) and haemorrhage to vessel transection and avulsion.23 State-of-the-art MDCT provides optimal depiction and characterization of all these vascular injuries.1,5,14,23 Actually, the appropriate scan parameters and CT protocol of study are critical. The arterial phase of image acquisition improves the detection of arterial injures, pseudoaneurysms and AVF5,14 while the portal venous phase is essential to detect venous injuries, bleeding and to differentiate contained vascular injures from actively bleeding lesions.4,10,14,24,25 Therefore, both phases should be routinely included in the whole-body CT evaluation of patients with deceleration injury.1,5,14,18,19,26–28
VESSEL INJURIES
Contained vascular injuries
Intimal tears
An intimal or periadventitial defect can be frequently seen on the angiography CT scan of patients with blunt trauma. One of the vessels most frequently involved is the thoracic aorta. MDCT angiography has a reported sensitivity of 95–100% and a negative-predictive value approaching 100% for the detection of blunt traumatic injuries of the aorta.9
The most common imaging finding of an intimal tear is a rounded or triangular intraluminal filling defect <10 mm in length or width near to the vessel wall without external contour abnormality (Figure 1).9
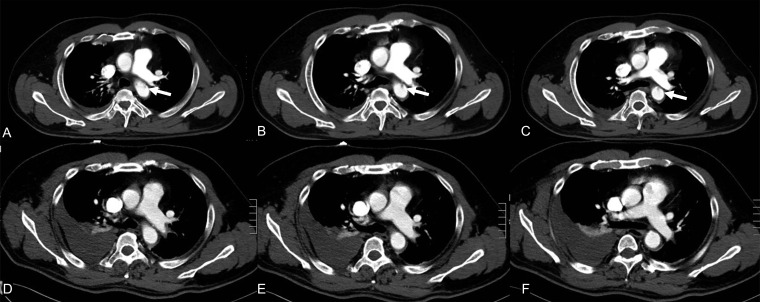
Figure 1.
Axial contrast-enhanced CT showing minimal traumatic intimal injury of the ascending thoracic aorta (arrows) (a–c). Typically, minimal aortic injuries heal spontaneously. Follow-up CT showing spontaneous resolution of the intimal defect (d–f).
This finding arises from an injury of the intima while the media and adventitia remain intact. It usually occurs within the proximity of the aortic isthmus, which is the site of attachment of the ligamentum arteriosum.29–31
Aortic injuries have been classified based upon their severity by Azizzadeh et al.24 An intimal tear is considered as Type I, intramural haematoma as Type II, pseudoaneurysm as Type III and ruptured vessel as Type IV.32
It is important to assess the grade of an aortic injury, since it affects patient management. Typically, Type I injuries heal spontaneously (Figure 1) while Types II–IV should be repaired surgically.32–34 When an intimal defect compromises the lumen for <10% or an intimal flap of <1 cm is present without or with minimal periaortic haematoma, the lesion can be considered “minimal” and follow-up is recommended (Figure 1). Intimal tears may also lead to intraluminal thrombosis owing to the endoluminal exposure of thrombotic subintimal factors or evolve in vessel dissection.35 Despite these possible complications, several studies recommend that in the acute phase, intimal tears can be managed conservatively and in the long term, imaging would be useful to evaluate the outcome.36
Intimal tear and dissection are less commonly observed in the ascending aorta, since these lesions cause early trauma mortality. In these cases, a good knowledge of the artefacts and pitfalls in the imaging of thoracic aortic dissections may help in avoiding misinterpretations.37 When an examination is conducted on new MDCT scans, fast image acquisition and post-processing improvements help eliminate or reduce breathing and/or cardiac artefacts, thus providing better quality images. However, in select cases, an electrocardiography-gated thoracic CT may be considered to avoid misinterpretations.37–39
Intramural haematoma
Intramural haematoma is a haematoma which develops in the media tunic of the vessel wall (Figure 2). Intramural haematoma is diagnosed by the presence of thickening of 0.5 mm of the vessel wall in the absence of evidence of blood flow.40,41
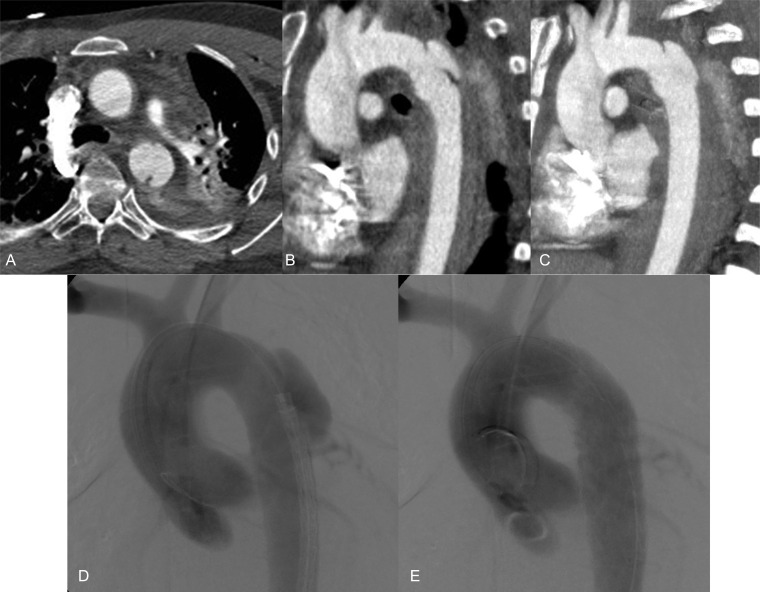
Figure 2.
Unenhanced CT showing hyperdensity of the aortic wall, periaortic haematoma and bilateral pleural effusion (a). Contrast-enhanced CT confirming the presence of active bleeding and intramural haematoma (b); after 2 h, owing to hypotension, tachycardia and fall of the haemoglobin level, the patient underwent angiography revealing an aortic pseudoaneurysm (PSA) of the descending thoracic aorta (c). Final angiogram showing the complete exclusion of PSA after positioning of endoprosthesis (d).
The sensitivity of MDCT, with unenhanced acquisition followed by contrast-enhanced acquisition, in the detection of this condition has been reported to be up to 96%.35 It is suggested that intramural haematomas should be treated (Figure 2), since they may progress to frank aortic dissection over time.41
Pseudoaneurysms
Pseudoaneurysm is an outpouching of the external vessel contour due to disruption of all three wall layers, which is contained only by the connective tissue around the vessel.40
On MDCT, a pseudoaneurysm is a round or oval irregularity of the outer contour of the vessel wall of equal density to the intra-arterial contrast material, with a collar of separation from the vessel lumen (Figure 3).
Figure 3.
Axial contrast-enhanced CT showing traumatic pseudoaneurysm of the descending thoracic aorta (a) with typical site and morphology; sagittal view (b) showing pseudoaneurysm and maximum intensity projection reconstruction (c). (d, e): initial angiogram confirming pseudoaneurysm in the descending thoracic aorta (a) and angiogram performed after placement of the endovascular stent (b).
On the venous phase, a pseudoaneurysm typically does not increase in size, and exhibits enhancement pattern synchronous with those of the other arterial vessels.3,41
When the intraluminal pressure increases, the pseudoaneurysm can easily rupture. Therefore, patients should be treated regardless of its diameter (Figure 3).32,34,40 A pseudoaneurysm can form suddenly after trauma or can be secondary to a less severely injured vessel; furthermore, if patients with high-energy blunt trauma are not evaluated with MDCT angiography, it can be undiagnosed and discovered later.
Chronic aortic pseudoaneurysms are detected in up to 5% of cases of undetected aortic injuries.7,32,42 They are usually asymptomatic and can be incidentally identified on chest radiograph or CT. They can be confused for a soft-tissue mass contiguous to the aortic wall or calcified lymph node, since a calcification rim may be present.31
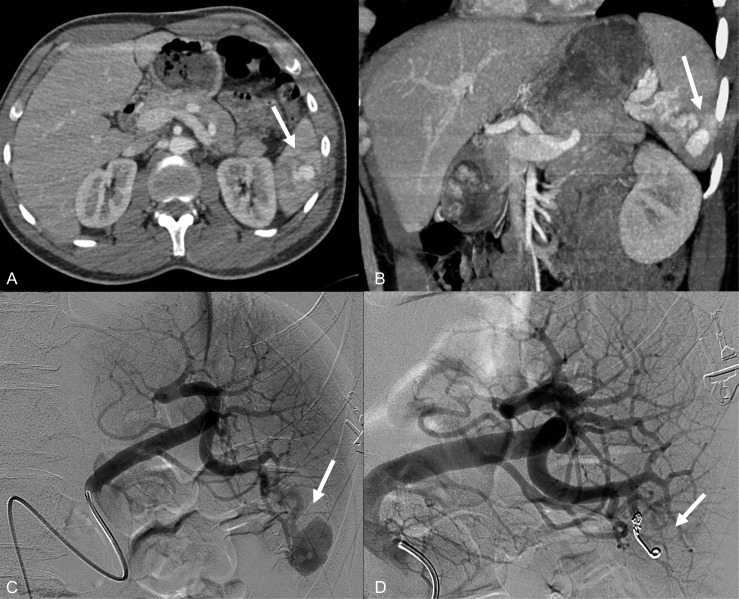
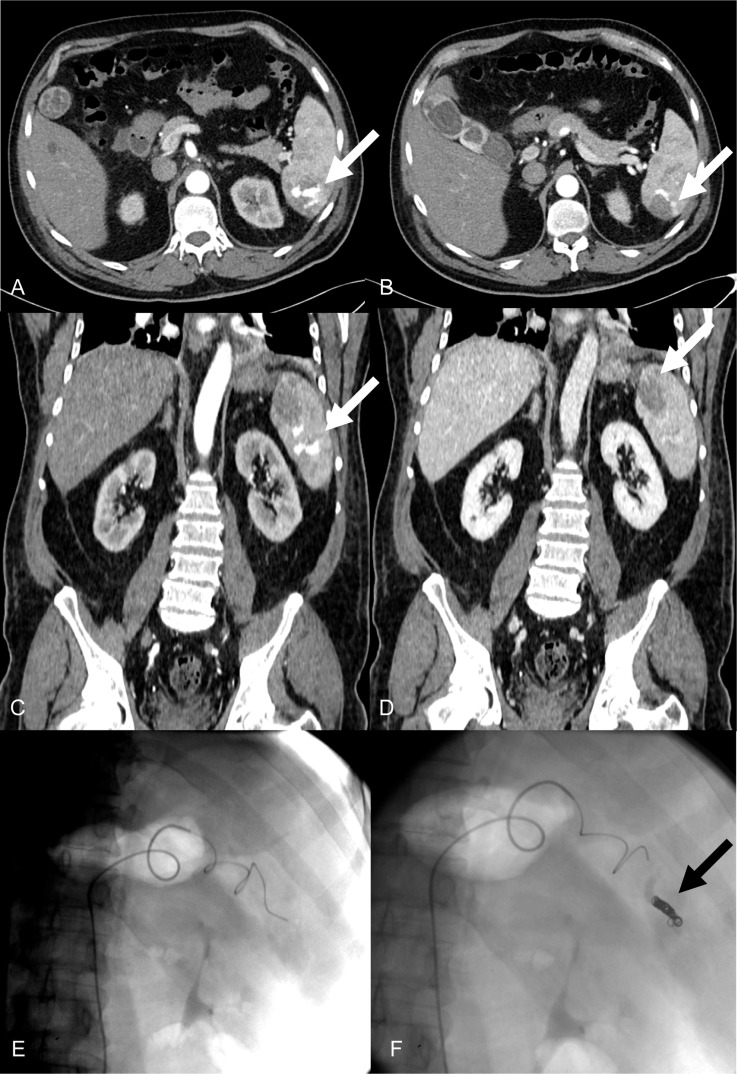
Within the abdomen, pseudoaneurysms are most frequently encountered in the spleen, since this is the most commonly injured abdominal organ in blunt trauma.5,43 An accurate identification is crucial, since angiographic embolization is the treatment of choice (Figures 4–6).5,25,43 MDCT protocol should include an arterial phase,1,14,25,43 since it allows the detection of AVF and improves the detection of pseudoaneurysm in the spleen (Figure 5).14,24 The arterial phase allows the identification of the circumscribed area of medium contrast attenuation with the wash in and washout similar to those of the contiguous artery; however, in the portal venous phase, the attenuation is similar to the parenchyma. Thus, the detection of a pseudoaneurysm on the portal venous phase is very difficult (Figure 5).10,25
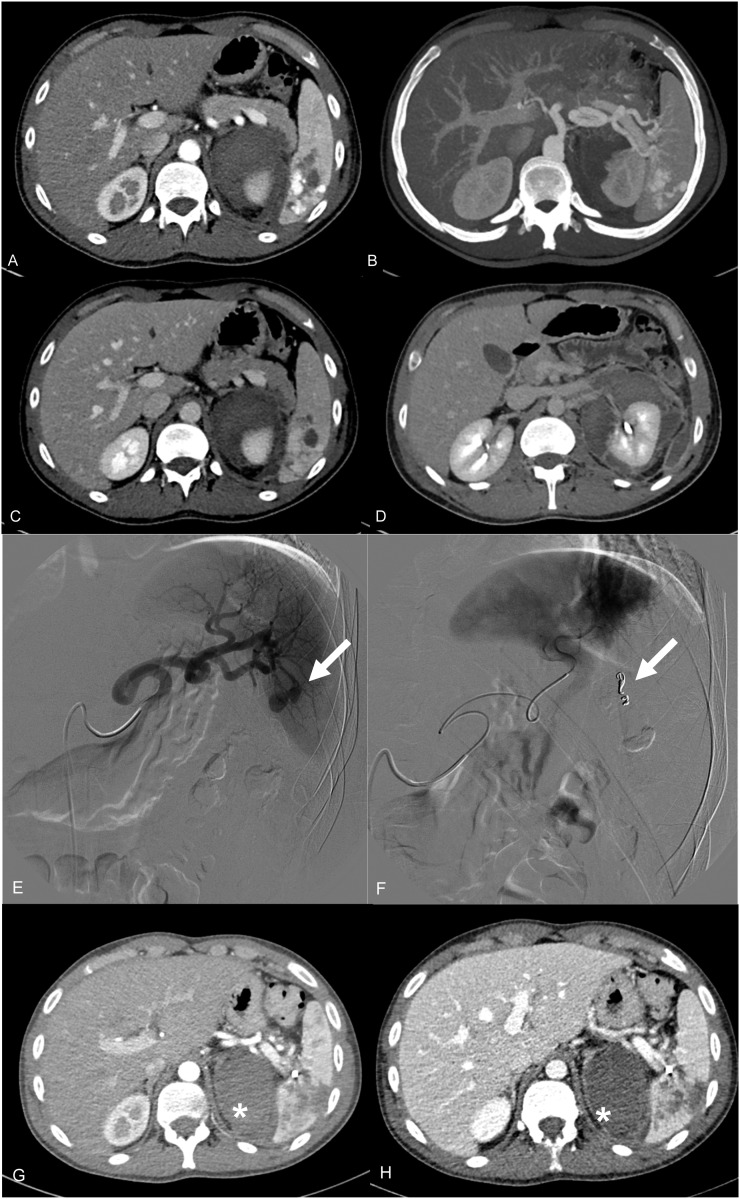
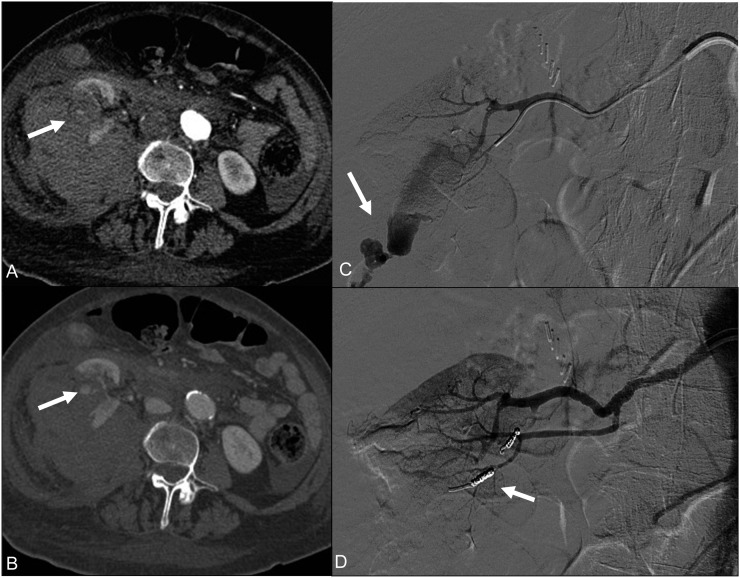
Figure 4.
Axial contrast-enhanced CT (a) and maximum intensity projection reconstruction in the coronal plane (b) revealing the presence of intraparenchymal pseudoaneurysm (PSA) of the splenic artery (arrows). (c, d): angiography confirming the presence of a large intraparenchymal pseudoaneurysm of the splenic artery (arrow). Angiogram was performed after selective embolization with coils (arrow) (b).
Figure 6.
Contrast-enhanced CT in the arterial (a) and venous phases (b) in the axial and coronal planes (c, d) showing the presence of multiple splenic pseudoaneurysms (arrows). Endovascular embolization of the pseudoaneurysms (e) with coil placement (f, black arrow).
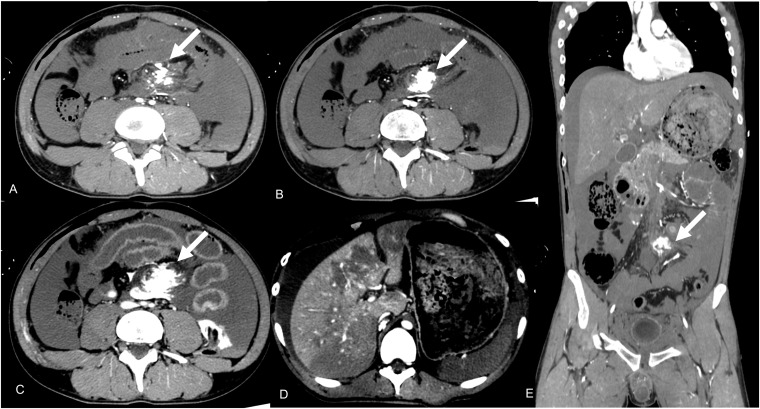
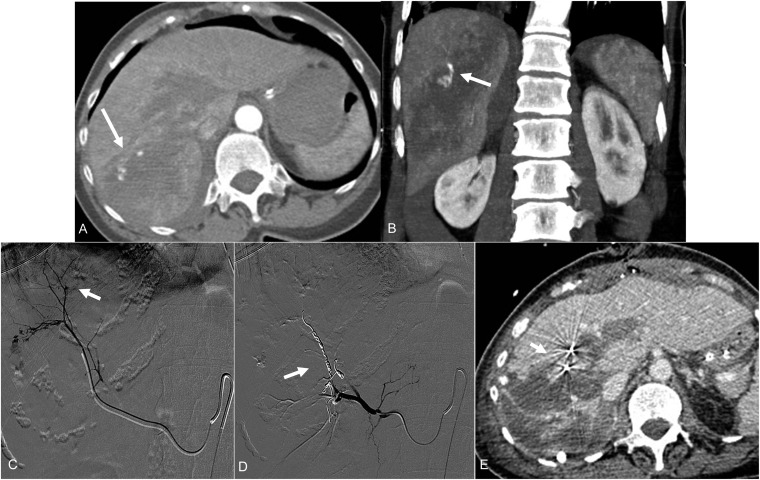
Figure 5.
Axial contrast-enhanced CT in the arterial phase (a) and maximum intensity projection reconstruction (b) demonstrating multiple splenic pseudoaneurysms. Axial contrast-enhanced CT in the portal phase (c): the attenuation of the pseudoaneurysm is similar to the attenuation of the parenchyma, thus making difficult to identify the presence of pseudoaneurysms. Axial contrast-enhanced CT in the arterial phase showing the presence of a large perirenal haematoma without evidence of active bleeding (d). Angiography confirming the presence of splenic pseudoaneurysms (arrow) (e), and catheter embolization was performed (arrow) (f). Enhanced CT in the arterial (g) and venous (h) phases after endovascular treatment showing the effectiveness of the procedure. The perirenal haematoma (asterisks) was managed conservatively.
Arteriovenous fistula
This is another contained vascular injury, which consists of a traumatic communication between the arterial and venous systems. An AVF may arise from a blunt or, more commonly, penetrating trauma.24,33
On MDCT, AVF is an asymmetrical, early contrast opacification of a vein, during the arterial phase (Figure 7); thus, an arterial phase is necessary to make the diagnosis.
Figure 7.
Contrast-enhanced CT in the axial (a) and coronal (b) planes: arterial phase revealing the presence of multiple pseudoaneurysms as well as opacification of the splenic vein consistent with the presence of the arteriovenous fistula (AVF). Angiogram confirming the presence of the AVF (arrow) and pseudoaneurysms (curved arrow) (c), which were successfully treated with onyx embolization coils (d).
It is important to detect a traumatic AVF, since it usually enlarges with time and may lead to haemodynamic alterations because of the abnormal shunt of blood from the artery into the vein; thus, the distal circulation and capillaries are bypassed.44
An undiagnosed AVF can become more difficult to repair and can cause congestive heart failure and irreversible venous stasis changes.33 AVF can occur in the spleen, frequently with pseudoaneurysm. Therefore, the arterial phase plays a key role in AVF detection, since the early enhancement of the splenic vein is diagnostic.5,14,24,45 AVF can be asymptomatic or may lead to abdominal pain, congestion of the mesenteric vessels and portal hypertension.46,47
Actively bleeding injuries
Haemorrhage
MDCT angiography plays an important role in the detection of bleeding and assists in directing patient management.48 Acute haemorrhage is treated with emergency surgery when associated with parenchymal disruption, and with transarterial embolization1,49 or conservative management, depending on its origin (arterial or venous), shape (spot, jet and pooling) and flow rate when the parenchymal injury is limited. Therefore, a single phase is not sufficient. Dual phase is recommended in most cases to provide a complete assessment in patients with polytrauma.
On MDCT, active bleeding is recognized as a region of extraluminal contrast agent extravasation, which increases and changes its morphology during multiphasic acquisitions (Figure 8).5,24 Its shape depends on the blood flow rate and appears as jet-like, linear or spot-like or pooling of bleeding (Figure 8).5,25,45,50 A spot or small jet of bleeding is frequently seen within the abdominal solid organs, mesentery or muscles (Figures 9–11). In most cases, non-operative management or transcatheter embolization can be effective depending on the patient age and initial haemodynamic status (Figures 12 and 13).
Figure 8.
Axial contrast-enhanced CT in the arterial (a, b) and venous phases (c) showing pooling of active bleeding in the mesentery root (arrows). Signs of parenchymal ischaemia in the liver due to systemic hypoperfusion are evident (d). (e) Coronal multiplanar reconstruction view demonstrating the source of active extravasation in the mesentery (arrow).
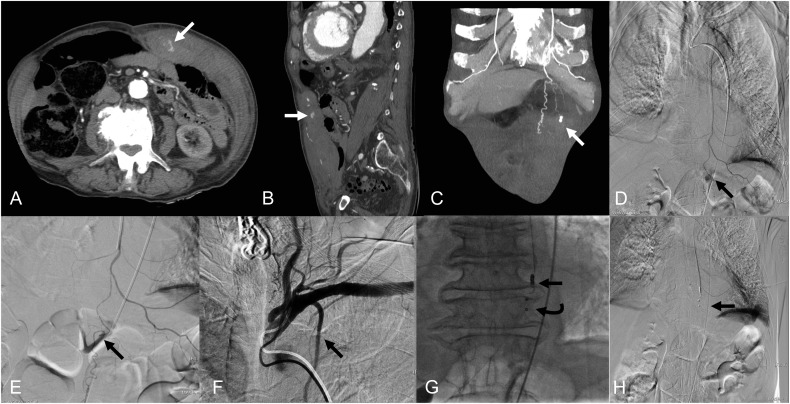
Figure 9.
Multidetector CT in the arterial phase in axial (a), sagittal (b) and maximum intensity projection coronal (c) planes showing active arterial bleeding from the left internal mammary artery (white arrows). Opacification of the left mammary artery with microcatheter showing active bleeding (black arrow) (d). Super-selective angiography of the left mammary artery with microcatheter (black arrow) (e). Angiography of the subclavian artery with opacification of the left mammary artery (black arrow) (f). Controlled coils release, 2 × 20 mm Hilar Cook (curved white arrow) and 1 × 140 mm Nester Cook (straight black arrow) (g). Final angiogram check after coil release demonstrates no active bleeding (black arrow) (h).
Figure 11.
Contrast-enhanced CT revealing a retroperitoneal haematoma with active extravasation (arrow) (a). Angiography confirming the presence of active haemorrhage (arrow) (b). (c, d) Angiogram performed after embolization with AVP IV (straight arrows), and coils (curved arrows).
Figure 12.
Contrast-enhanced axial CT scans demonstrating multiple lacerations of the right kidney (arrows) with a large right perirenal haematoma (a, b). Angiography confirming the presence of important arterial bleeding (arrow) (c). Successful angiogram after embolization with coils (arrow) (d).
Figure 13.
Contrast-enhanced CT revealing intraparenchymal bleeding within the right lobe of the liver (arrow) (a) and its coronal view (arrow) (b). Initial selective angiogram revealing multiple intraparenchymal bleedings (arrow) (c). Final angiogram performed after embolization with spongel and coils (arrow) (d) demonstrating successful embolization. Contrast-enhanced CT performed after embolization showing the coils of previous embolization (arrow) (e) and lack of bleeding.
Figure 10.
Contrast-enhanced CT showing an arterial bleeding from the right intercostal artery (arrows) (a, b). Selective angiography was performed (c) confirming the bleeding (arrow). Angiogram performed after endovascular treatment demonstrating embolization of the bleeding vessel (arrow) (d).
On the contrary, with a large region of active haemorrhage especially within the mesentery or adjacent to bowel loops (Figure 8) or if associated with parenchymal disruption, emergency surgery is necessary (Figure 14). Therefore, dual-phase MDCT is critical for identification and characterization of bleeding and to differentiate contained vascular injuries from actively bleeding.
Figure 14.
Contrast-enhanced CT in the arterial phase in the coronal (a) and axial (b) planes and in the venous phase (c) showing a spleen fracture with active bleeding (a, b; arrows), large perisplenic haematoma and free haemoperitoneum. Due to the haemodynamic instability, splenectomy was performed.
Another important issue is to identify the origin of the bleeding, if it is arterial or venous in origin, since it affects management. This is crucial especially in the setting of pelvic blunt trauma. Actually, when the CT is limited to the portal phase, it is not possible to obtain an adequate differentiation between the two haemorrhage types or to correctly identify the vessel of origin.51 When an arterial bleeding occurs in the pelvis, it is mostly treated with emergent intervention or angiographic embolization, while venous bleeding can be initially treated non-operatively (Figures 15–17).4,5,49
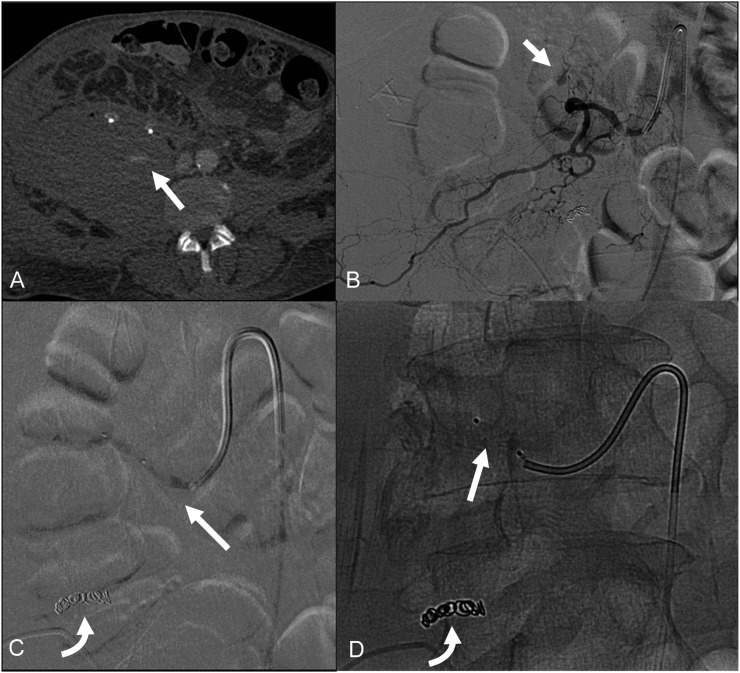
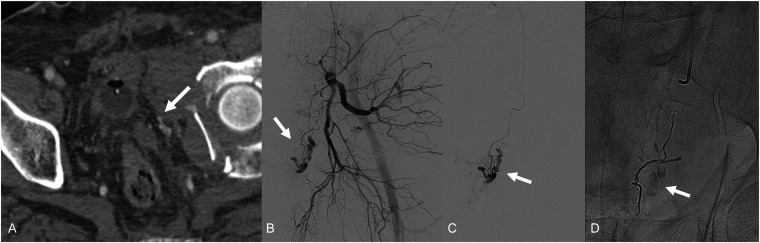
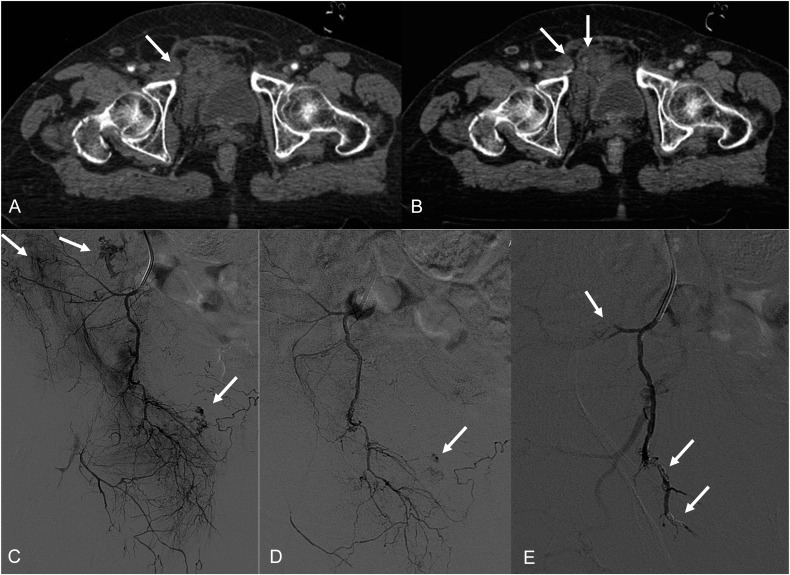
Figure 15.
Contrast-enhanced CT scan (a) demonstrating pelvic haematoma with arterial bleeding (arrows) secondary to a comminuted fracture of the right acetabulum. There is a haematoma with mass effect upon the bladder (a). Angiography confirming arterial bleeding (arrow) (b); selective angiography of a branch of the pudendal artery showing the arterial bleeding (arrow) (c). Final angiogram performed after embolization with Onyx (arrow) (d).
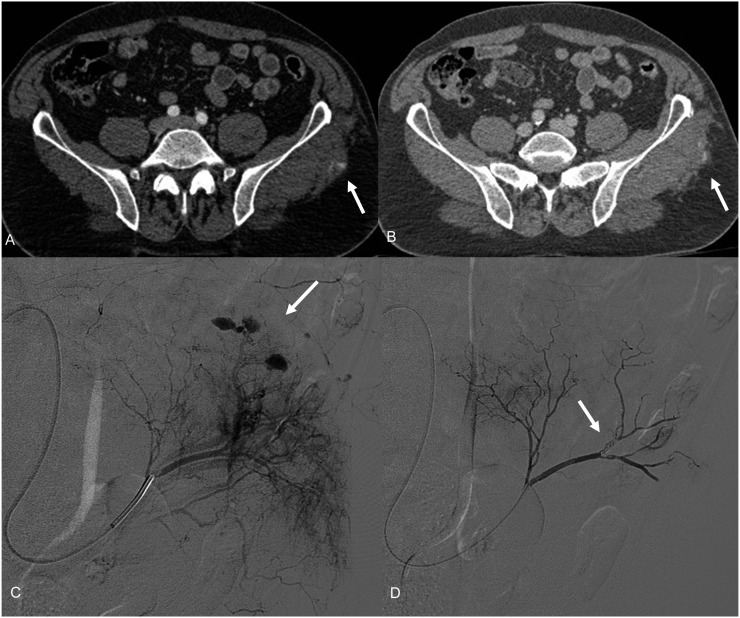
Figure 17.
Contrast-enhanced CT scan showing gluteal active bleeding (arrows) in the arterial (a) and venous phases (b). Selective angiogram of the left gluteal artery confirming multiple spots of active bleeding (arrow) (c), and final angiogram showing the success of the procedure (arrow) (d).
Figure 16.
Contrast-enhanced CT scan demonstrating pelvic haematoma with evidence of multiple spots of active bleeding (arrows), in the arterial (a) and venous (b) phases. Selective (c) and super-selective (d) angiograms of the hypogastric artery (descending artery) confirming multiple sources of active bleeding (arrows); final angiogram showing successful embolization (arrows) (e).
Transection and avulsion
Vessel transection may be complete or incomplete,33 but it represents a life-threatening condition leading in almost all cases to patient death.52 Transection or vessel avulsion is either an indication for immediate surgery (Figure 18) or embolization. Rupture is seen as an abnormality in the vessel contour due to full thickness laceration with free contrast extravasation detectable in the arterial phase (Figure 19) and becomes a hyperdense blood collection. It can occur in the ascending or descending thoracic aorta, causing haemopericardium or haemomediastinum. It can also occur in the abdominal aorta causing haemoperitoneum or in a branch vessel causing active bleeding and devascularization of the supplied organs.31 When a vessel is transected, immediate endovascular (in incomplete transection) or surgical treatment (in avulsion) should be attempted, even if the prognosis is usually poor.40
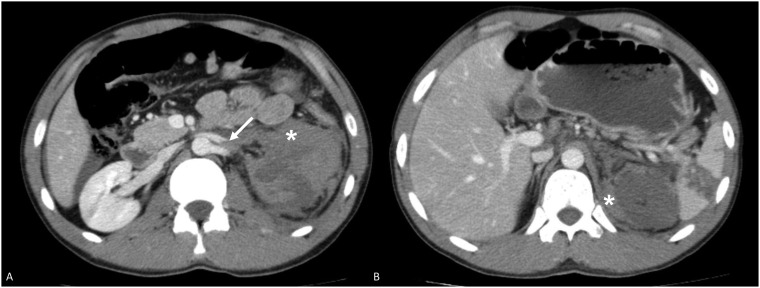
Figure 18.
Axial contrast-enhanced CT showing traumatic transection of both the renal artery and vein (arrow) (a) with no enhancement of the left kidney (a, b) and fresh perirenal haematoma (asterisks) (a, b).
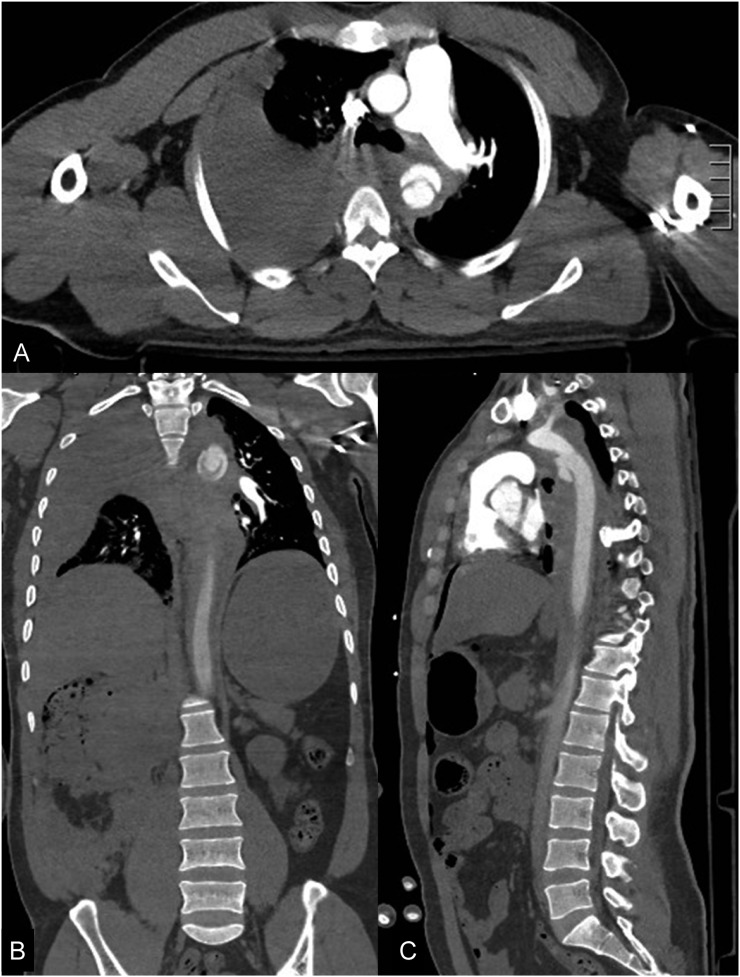
Figure 19.
Axial (a), coronal (b) and sagittal (c) contrast-enhanced CT showing post-traumatic rupture of the descending thoracic aorta with large haemomediastinum and haemothorax (a, b, c).
CONCLUSION
MDCT angiography represents the gold standard for polytraumatized patients with vascular injury from high-energy blunt trauma and is also effective in the follow-up of patients undergoing vascular surgery. In the diagnostic MDCT approach of patients with blunt trauma and suspected vascular injury, a dual-phase CT protocol is strongly recommended because it identifies all types of arterial injuries, from intimal tears which are treated conservatively to vascular injuries which require prompt surgical intervention or frequent surveillance.
Contributor Information
Francesca Iacobellis, Email: iacobellisf@gmail.com.
Anna M Ierardi, Email: amierardi@yahoo.it.
Maria A Mazzei, Email: mamazzei@gmail.com.
Alberto Magenta Biasina, Email: magentabiasina@libero.it.
Gianpaolo Carrafiello, Email: gcarraf@gmail.com.
Refky Nicola, Email: rnicola04@gmail.com.
Mariano Scaglione, Email: mscaglione@tiscali.it.
REFERENCES
- 1.Schueller G, Scaglione M, Linsenmaier U, Schueller-Weidekamm C, Andreoli C, De Vargas Macciucca M, et al. The key role of the radiologist in the management of polytrauma patients: indications for MDCT imaging in emergency radiology. Radiol Med 2015; 120: 641–54. doi: 10.1007/s11547-015-0500-x [DOI] [PubMed] [Google Scholar]
- 2.Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, et al. Epidemiology of trauma deaths: a reassessment. J Trauma 1995; 38: 185–93. doi: 10.1097/00005373-199502000-00006 [DOI] [PubMed] [Google Scholar]
- 3.Stone TJ, Norbet C, Rhoades P, Bhalla S, Menias CO. Computed tomography of adult blunt abdominal and pelvic trauma: implications for treatment and interventions. Semin Roentgenol 2014; 49: 186–201. doi: 10.1053/j.ro.2014.01.004 [DOI] [PubMed] [Google Scholar]
- 4.Vu M, Anderson SW, Shah N, Soto JA, Rhea JT. CT of blunt abdominal and pelvic vascular injury. Emerg Radiol 2010; 17: 21–9. doi: 10.1007/s10140-009-0813-y [DOI] [PubMed] [Google Scholar]
- 5.Soto JA, Anderson SW. Multidetector CT of blunt abdominal trauma. Radiology 2012; 265: 678–93. doi: 10.1148/radiol.12120354 [DOI] [PubMed] [Google Scholar]
- 6.Palas J, Matos AP, Mascarenhas V, Herédia V, Ramalho M. Multidetector computer tomography: evaluation of blunt chest trauma in adults. Radiol Res Pract 2014; 2014: 864369. doi: 10.1155/2014/864369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scaglione M, Pinto A, Pedrosa I, Sparano A, Romano L. Multi-detector row computed tomography and blunt chest trauma. Eur J Radiol 2008; 65: 377–88. doi: 10.1016/j.ejrad.2007.09.023 [DOI] [PubMed] [Google Scholar]
- 8.Commitee on Trauma of the American College of Surgeons. Resources for optimal care of the injured patient. Chicago, IL; ACS; 2014. [Google Scholar]
- 9.Gunn ML, Lehnert BE, Lungren RS, Narparla CB, Mitsumori L, Gross JA, et al. Minimal aortic injury of the thoracic aorta: imaging appearances and outcome. Emerg Radiol 2014; 21: 227–33. doi: 10.1007/s10140-013-1187-8 [DOI] [PubMed] [Google Scholar]
- 10.Uyeda JW, Anderson SW, Sakai O, Soto JA. CT angiography in trauma. Radiol Clin North Am 2010; 48: 423–38. doi: 10.1016/j.rcl.2010.02.003 [DOI] [PubMed] [Google Scholar]
- 11.Pfeifer R, Tarkin IS, Rocos B, Pape HC. Patterns of mortality and causes of death in polytrauma patients–has anything changed? Injury 2009; 40: 907–11. doi: 10.1016/j.injury.2009.05.006 [DOI] [PubMed] [Google Scholar]
- 12.Muckart DJ, Pillay B, Hardcastle TC, Skinner DL. Vasc injuries following blunt polytrauma. Eur J Trauma Emerg Surg 2014; 40: 315–22. doi: 10.1007/s00068-014-0382-y [DOI] [PubMed] [Google Scholar]
- 13.Sobrino J, Shafi S. Timing and causes of death after injuries. Proc (Bayl Univ Med Cent) 2013; 26: 120–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uyeda JW, LeBedis CA, Penn DR, Soto JA, Anderson SW. Active hemorrhage and vascular injuries in splenic trauma: utility of the arterial phase in multidetector CT. Radiology 2014; 270: 99–106. doi: 10.1148/radiol.13121242 [DOI] [PubMed] [Google Scholar]
- 15.Patterson BO, Holt PJ, Cleanthis M, Tai N, Carrell T, Loosemore TM; London Vascular Injuries Working Group. Imaging vascular trauma. Br J Surg 2012; 99: 494–505. doi: 10.1002/bjs.7763 [DOI] [PubMed] [Google Scholar]
- 16.Fishman JE. Imaging of blunt aortic and great vessel trauma. J Thorac Imaging 2000; 15: 97–103. doi: 10.1097/00005382-200004000-00004 [DOI] [PubMed] [Google Scholar]
- 17.Scaglione M, Pinto A, Pinto F, Romano L, Ragozzino A, Grassi R. Role of contrast-enhanced helical CT in the evaluation of acute thoracic aortic injuries after blunt chest trauma. Eur Radiol 2001; 11: 2444–8. doi: 10.1007/s003300100836 [DOI] [PubMed] [Google Scholar]
- 18.Hamilton JD, Kumaravel M, Censullo ML, Cohen AM, Kievlan DS, West OC. Multidetector CT evaluation of active extravasation in blunt abdominal and pelvic trauma patients. Radiographics 2008; 28: 1603–16. doi: 10.1148/rg.286085522 [DOI] [PubMed] [Google Scholar]
- 19.Crönlein M, Sandmann GH, Beirer M, Wunderlich S, Biberthaler P, Huber-Wagner S. Traumatic bilateral carotid artery dissection following severe blunt trauma: a case report on the difficulties in diagnosis and therapy of an often overlooked life-threatening injury. Eur J Med Res 2015; 20: 62. doi: 10.1186/s40001-015-0153-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fox N, Schwartz D, Salazar JH, Haut ER, Dahm P, Black JH, et al. Evaluation and management of blunt traumatic aortic injury:a practice management guideline from the Eastern Association for the Surgery of Trauma. J Trauma Acute Care Surg 2015; 78: 136–46. doi: 10.1097/TA.0000000000000470 [DOI] [PubMed] [Google Scholar]
- 21.Sica G, Guida F, Bocchini G, Codella U, Mainenti PP, Tanga M, et al. Errors in imaging assessment of polytrauma patients. Semin Ultrasound CT MR 2012; 33: 337–46. doi: 10.1053/j.sult.2012.01.012 [DOI] [PubMed] [Google Scholar]
- 22.Scaglione M, Salvolini L, Casciani E, Giovagnoni A, Mazzei MA, Volterrani L. The many faces of aortic dissections: beware of unusual presentations. Eur J Radiol 2008; 65: 359–64. doi: 10.1016/j.ejrad.2007.09.021 [DOI] [PubMed] [Google Scholar]
- 23.Osgood MJ, Heck JM, Rellinger EJ, Doran SL, Garrard CL, 3rd, Guzman RJ, et al. Natural history of grade I-II blunt traumatic aortic injury. J Vasc Surg 2014; 59: 334–41. doi: 10.1016/j.jvs.2013.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boscak AR, Shanmuganathan K, Mirvis SE, Fleiter TR, Miller LA, Sliker CW. et al. Optimizing trauma multidetector CT protocol for blunt splenic injury: need for arterial and portal venous phase scans. Radiology 2013; 268: 79–88. doi: 10.1148/radiol.13121370 [DOI] [PubMed] [Google Scholar]
- 25.Anderson SW, Varghese JC, Lucey BC, Burke PA, Hirsch EF, Soto JA. Blunt splenic trauma: delayed-phase CT for differentiation of active hemorrhage from contained vascular injury in patients. Radiology 2007; 243: 88–95. doi: 10.1148/radiol.2431060376 [DOI] [PubMed] [Google Scholar]
- 26.Scaglione M, Iaselli F, Sica G, Feragalli B, Nicola R. Errors in imaging of traumatic injuries. Abdom Imaging 2015; 40: 2091–8. doi: 10.1007/s00261-015-0494-9 [DOI] [PubMed] [Google Scholar]
- 27.Desouza RM, Crocker MJ, Haliasos N, Rennie A, Saxena A. Blunt traumatic vertebral artery injury: a clinical review. Eur Spine J 2011; 20: 1405–16. doi: 10.1007/s00586-011-1862-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liang T, Tso DK, Chiu RY, Nicolaou S. Imaging of blunt vascular neck injuries: a clinical perspective. AJR Am J Roentgenol 2013; 201: 893–901. doi: 10.2214/AJR.12.9663 [DOI] [PubMed] [Google Scholar]
- 29.Kerut EK, Kelley G, Falco VC, Ovella T, Diethelm L, Helmcke F. Traumatic deceleration injury of the thoracic aorta. Echocardiography 2005; 22: 697–704. doi: 10.1111/j.1540-8175.2005.40150.x [DOI] [PubMed] [Google Scholar]
- 30.Creasy JD, Chiles C, Routh WD, Dyer RB. Overview of traumatic injury of the thoracic aorta. Radiographics 1997; 17: 27–45. doi: 10.1148/radiographics.17.1.9017797 [DOI] [PubMed] [Google Scholar]
- 31.Steenburg SD, Ravenel JG. Multi-detector computed tomography findings of atypical blunt traumatic aortic injuries: a pictorial review. Emerg Radiol 2007; 14: 143–50. doi: 10.1007/s10140-007-0620-2 [DOI] [PubMed] [Google Scholar]
- 32.Azizzadeh A, Keyhani K, Miller CC, 3rd, Coogan SM, Safi HJ, Estrera AL. Blunt traumatic aortic injury: initial experience with endovascular repair. J Vasc Surg 2009; 49: 1403–8. doi: 10.1016/j.jvs.2009.02.234 [DOI] [PubMed] [Google Scholar]
- 33.McPherson SJ. Thoracic aortic and great vessel trauma and its management. Semin Intervent Radiol 2007; 24: 180–96. doi: 10.1055/s-2007-980042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shalhub S, Starnes BW, Tran NT, Hatsukami TS, Lundgren RS, Davis CW, et al. Blunt abdominal aortic injury. J Vasc Surg 2012; 55: 1277–85. doi: 10.1016/j.jvs.2011.10.132 [DOI] [PubMed] [Google Scholar]
- 35.Shea K, Stahmer S. Carotid and vertebral arterial dissections in the emergency department. Emerg Med Pract 2012; 14: 1–23. [PubMed] [Google Scholar]
- 36.Aladham F, Sundaram B, Williams DM, Quint LE. Traumatic aortic injury: computerized tomographic findings at presentation and after conservative therapy. J Comput Assist Tomogr 2010; 34: 388–94. doi: 10.1097/RCT.0b013e3181d0728f [DOI] [PubMed] [Google Scholar]
- 37.Batra P, Bigoni B, Manning J, Aberle DR, Brown K, Hart E, et al. Pitfalls in the diagnosis of thoracic aortic dissection at CT angiography. Radiographics 2000; 20: 309–20. doi: 10.1148/radiographics.20.2.g00mc04309 [DOI] [PubMed] [Google Scholar]
- 38.Ko SF, Hsieh MJ, Chen MC, Ng SH, Fang FM, Huang CC, et al. Effects of heart rate on motion artifacts of the aorta on non-ECG-assisted 0.5-sec thoracic MDCT. AJR Am J Roentgenol 2005; 184: 1225–30. doi: 10.2214/ajr.184.4.01841225 [DOI] [PubMed] [Google Scholar]
- 39.McMahon MA, Squirrell CA. Multidetector CT of aortic dissection: a pictorial review. Radiographics 2010; 30: 445–60. doi: 10.1148/rg.302095104 [DOI] [PubMed] [Google Scholar]
- 40.Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H, et al. ; ESC Committee for Practice Guidelines. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014; 35: 2873–926. doi: 10.1093/eurheartj/ehu281 [DOI] [PubMed] [Google Scholar]
- 41.Voitle E, Hofmann W, Cejna M. Aortic emergencies-diagnosis and treatment: a pictorial review. Insights Imaging 2015; 6: 17–32. doi: 10.1007/s13244-014-0380-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marcu CB, Nijveldt R, Van Rossum AC. Unsuspected chronic traumatic aortic pseudoaneurysm–what to do about it. Late post-traumatic aortic pseudoaneurysm. Can J Cardiol 2008; 24: 143–4. doi: 10.1016/S0828-282X(08)70571-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brillantino A, Iacobellis F, Robustelli U, Villamaina E, Maglione F, Colletti O, et al. Non operative management of blunt splenic trauma: a prospective evaluation of a standardized treatment protocol. Eur J Trauma Emerg Surg 2015 [Epub ahead of print]. doi: 10.1007/s00068-015-0575-z [DOI] [PubMed] [Google Scholar]
- 44.Fritz J, Efron DT, Fishman EK. Multidetector CT and three-dimensional CT angiography of upper extremity arterial injury. Emerg Radiol 2015; 22: 269–82. doi: 10.1007/s10140-014-1288-z [DOI] [PubMed] [Google Scholar]
- 45.Atluri S, Richard HM, 3rd, Shanmuganathan K. Optimizing multidetector CT for visualization of splenic vascular injury. Validation by splenic arteriography in blunt abdominal trauma patients. Emerg Radiol 2011; 18: 307–12. doi: 10.1007/s10140-011-0961-8 [DOI] [PubMed] [Google Scholar]
- 46.Goffette PP, Latterre PF. Imaging and intervention of posttraumatic abdominal complications. In: Dondelinger RF, ed. Imaging and intervention in abdominal trauma. Berlin Heidelberg: Springer Verlag; 2004. pp. 577–87. [Google Scholar]
- 47.Goffette PP. Imaging and intervention in post-traumatic complications. In: Emergency radiology. Imaging and intervention. Marincek B, Dondelinger F, eds. Berlin Heidelberg: Springer Verlag; 2007. pp. 62. [Google Scholar]
- 48.Wada D, Nakamori Y, Yamakawa K, Yoshikawa Y, Kiguchi T, Tasaki O, et al. Impact on survival of whole-body computed tomography before emergency bleeding control in patients with severe blunt trauma. Crit Care 2013; 17: R178. doi: 10.1186/cc12861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pinto A, Niola R, Tortora G, Ponticiello G, Russo G, Di Nuzzo L, et al. Role of multidetector-row CT in assessing the source of arterial haemorrhage in patients with pelvic vascular trauma. Comparison with angiography [. In Italian.] Radiol Med 2010; 115: 648–67. doi: 10.1007/s11547-010-0494-0 [DOI] [PubMed] [Google Scholar]
- 50.Scaglione M, Di Mizio V, Pinto A, Mazzei MA, Romano L, Grassi R. Gastrointestinal tract. In: Scaglione M, Linsenmaier U, Schueller G, eds. Emergency radiology of the abdomen. Springer-Verlag Mailand; 2012. pp. 133–54. [Google Scholar]
- 51.Anderson SW, Soto JA, Lucey BC, Burke PA, Hirsch EF, Rhea JT. Blunt trauma: feasibility and clinical utility of pelvic CT angiography performed with 64-detector row CT. Radiology 2008; 246: 410–9. doi: 10.1148/radiol.2462070082 [DOI] [PubMed] [Google Scholar]
- 52.Kidane B, Abramowitz D, Harris JR, DeRose G, Forbes TL. Natural history of minimal aortic injury following blunt thoracic aortic trauma. Can J Surg 2012; 55: 377–81. doi: 10.1503/cjs.007311 [DOI] [PMC free article] [PubMed] [Google Scholar]