Abstract
Introduction
Currently, no systematic review/meta-analysis has examined studies that used online social networks (OSN) as a primary intervention platform. Therefore the purpose if this review was to evaluate the effectiveness of weight management interventions delivered through OSN.
Methods
PubMed, Embase, PsycINFO, Web of Science, and Scopus were searched (January 1990-November 2015) for studies with data on the effect OSNs on weight loss. Only primary source articles that utilized OSN as the main platform for delivery of weight management/healthy lifestyle interventions, were published in English language peer-reviewed journals, and reported outcome data on weight were eligible for inclusion in this systematic review. Five articles were included in this review.
Results
One-hundred percent of the studies (n=5) reported a reduction in baseline weight. Three of the five studies (60%) reported significant decreases in body weight when OSN was paired with health educator support. Only one study reported a clinical significant weight loss of ≥5%.
Conclusion
Using OSN for weight management is in its early stages of development and while these few studies show promise, more research is needed to acquire information about optimizing these interventions to increase their efficacy.
Keywords: Social Media, Obesity, Systematic Review, Weight loss
INTRODUCTION
Approximately 69% of U.S. adults are classified as overweight (BMI ≥ 25 kg/m2) while 35.1% are obese (BMI ≥ 30 kg/m2) (1). Being overweight/obese is associated with significant co-morbidity, and it is estimated that for every one-point increase in BMI, health care costs increase by 8% (2). The current recommended paradigm for weight management emphasizes a lifestyle modification program consisting of strategies to reduce energy intake, increase physical activity (PA), and provide cognitive behavior therapy to identify cues to unhealthy behaviors and restructure behavior to prompt healthy responses (3).
Changes in diet and PA facilitated by behavioral weight loss clinics are typically delivered face-to-face (FTF) by a health educator (HE) to a group of 12–15 individuals (4–6). However, this approach can require significant time commitments from both patients and educators as well as considerable economic costs (i.e. facility usage fees, travel costs, payroll, etc.). Healthcare systems need to find methods to address obesity that reach beyond the walls of clinics and hospitals using issues of lifestyle modification in a cost-conscious way. The need to develop alternative strategies to deliver weight management programs has resulted in investigations examining the efficacy of programs delivered through the mail or email (7–9), internet (10–12), a combination of phone, internet and email (13), individual phone counseling (7, 14–18), group phone counseling (19), and text messaging (20). While these alternate deliver programs have demonstrated successful weight loss; the dramatic increase in technology and online social networks (OSN) may present healthcare providers with innovative ways to deliver weight management programs that could have an impact on health care at the population level.
In 2013, Pew Internet survey reported that 70% of Americans over the age of 18 have high-speed internet in their homes (21). Furthermore, as of 2014, 74% of adults report using OSNs (22). An OSN as defined by Boyd and Ellison (23) is a web-based services that allow individuals to “(1) construct a public or semi-public profile within a bounded system, (2) articulate a list of other users with whom they share a connection, and (3) view and traverse their list of connections and those made by others within the system.” Due to this growth in technology and OSN, individuals have started to acquire information, share experiences, ask questions and provide support to peers about health online (24–26). Many individuals have reported feeling more comfortable and secure with expressing their problems and concerns remotely over the internet compared to talking FTF or over the phone (27, 28). Additionally, the more actively individuals participate within the OSN the more successful they are losing weight (29). For these reasons OSN have generated recent interest in OSN strategies as a delivery medium of health behavior change campaigns. Within the broad category of health issues, online support groups and communities have become an increasingly common way for individuals to share information and seek emotional support for issues surrounding weight loss (30).
Recent reviews of the efficacy of programs utilizing OSN components have found modest but significant evidence in improving health outcomes (31, 32). However, these reviews address studies that do not isolate the effect of OSNs; rather, they feature bulletin boards and chat rooms that were embedded within a larger intervention (33). Furthermore, data regarding the frequency of use of the social media components were rarely reported (33). To date, no systematic review/meta-analysis has examined studies that used OSNs as a primary intervention platform. Therefore, the objective of this systematic review is to identify and evaluate studies that have utilized OSNs to assess the impact on body weight, body composition and chronic disease risk factors.
METHODS
This systematic review was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines (34, 35).
Eligibility criteria
Only primary source articles that utilized OSN as the main platform for delivery of weight management/healthy lifestyle interventions and were published in English language peer-reviewed journals were eligible for inclusion in this systematic review. With the intention of isolating the effects of OSNs as a delivery system for weight management interventions at least one intervention group must have received all health education, materials, and recourses through an OSN. For example, if intervention groups were delivered by FTF, phone, email, etc with OSN supplemented as a tool then they were excluded from this review. Specific eligibility included: Participants: Adults (age 18 years and above). Studies of participants with elevated chronic disease risk factors and/or type 2 diabetes were included. Types of studies: Both non-randomized and randomized studies. Outcomes: Body weight was required for inclusion. Other outcomes included body composition (fat mass, fat-free mass, waist circumference) and chronic disease risk factors including total, HDL and LDL cholesterol, triglycerides, insulin, glucose, HbA1C, and blood pressure.
Information Sources
Studies were identified by searching electronic databases and related article reference lists. The search was applied to PubMed (1990-present) and adapted for EMBASE, PsycINFO, Web of Science, and Scopus (1990-present). The last search was conducted on November 11th, 2015. The search was developed with consultation with a Kansas University reference librarian and conducted by the first author (EW). No attempts were made to contact study investigators or sponsors to acquire any information missing from the published article.
Study Selection
Retrieved abstracts were independently assessed for inclusion in the review by 2 authors and coded as “yes”, “no” or “maybe.” All investigators who participated in eligibility assessments were trained regarding study inclusion/exclusion criteria. Disagreements regarding eligibility for inclusion were resolved via development of consensus among all co-authors. Eligibility assessments on the practice abstracts were reviewed by the author (EW). Full text articles for abstracts coded as “yes” or “maybe” were retrieved and reviewed and reviewed independently by 2 co-authors prior to inclusion in the review. An excel spread sheet was developed and used to track eligibility status.
Data collection
Extracted data was entered into the University of Kansas secure, REDCap (Research Electronic Data Capture, Version 4.14.5) database (36). A REDCap data extraction form was developed and has been used in previous reviews completed by our group (37–39). Relevant data were extracted from each manuscript by the author. Data extracted from each article included basic study information including sample size, groups compared, OSN platform, compliance with interventions, participant characteristics (age, sex, BMI, minority and health status), and results.
Risk of bias in individual studies
Risk of bias for studies was independently evaluated using the Cochrane risk of bias tool (40). Risk of bias was assessed in the following domains: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias. Studies were not excluded on the basis of risk of bias. Additionally, in present review we have attempted to summarize the strength of the available scientific evidence underlying the relationship of SM based interventions and health related outcomes using the following evidence scoring categories (41):
Evidence Level High: We are very confident that the estimate of effect lies close to the true effect for this outcome. The body of evidence has few or no deficiencies. We believe that the findings are stable, i.e., another study would not change the conclusions.
Evidence Level Moderate: We are moderately confident that the estimate of effect lies close to the true effect for this outcome. The body of evidence has some deficiencies. We believe that the findings are likely to be stable, but some doubt remains.
Evidence Level Low: We have limited confidence that the estimate of effect lies close to the true effect for this outcome. The body of evidence has major or numerous deficiencies (or both). We believe that additional evidence is needed before concluding either that the findings are stable or that the estimate of effect is close to the true effect.
Evidence Level Insufficient: We have no evidence, we are unable to estimate an effect, or we have no confidence in the estimate of effect for this outcome. No evidence is available or the body of evidence has unacceptable deficiencies, precluding reaching a conclusion.
Synthesis of results
There was considerable heterogeneity across studies for several important parameters including: 1) participant characteristics (age, sex, BMI, health status), 2) version of social network platform, and 3) duration of the weight loss period. Given this heterogeneity, a meta-analysis was considered inappropriate. Results based on the extracted data were instead synthesized and presented grouped by interventions (e.g. PA, diet, diet+PA)
SEARCH RESULTS
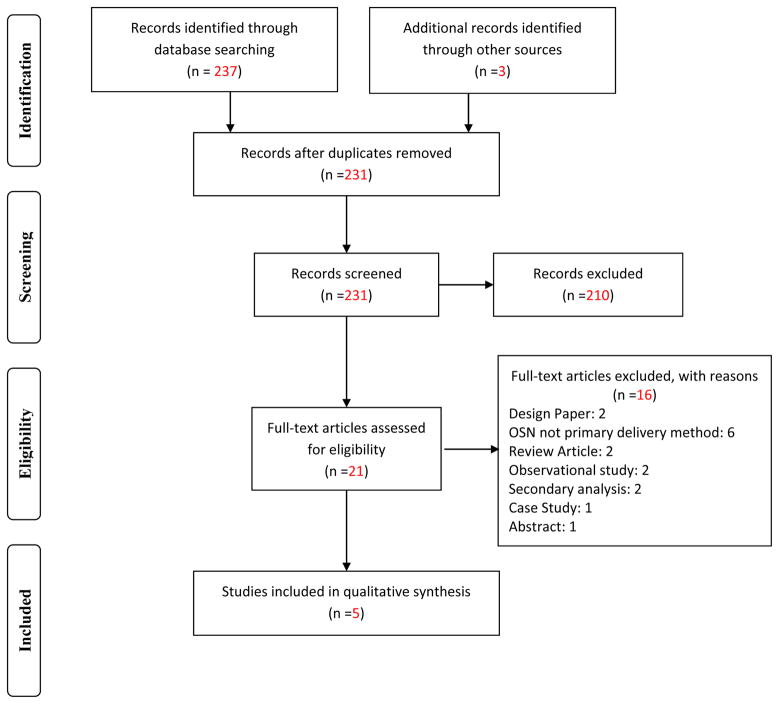
The initial database search identified 231 unique records, 210 of which were excluded based on review of title and abstract. Full-text articles for the remaining 21 citations were reviewed. Sixteen articles did not satisfy the inclusion criteria and were excluded, thus 5 articles were included in the review (Figure 1). Of the included studies, one study focused only on PA (42), four studies on both diet and PA (43–46) and only one of the 5 studies in this review reported on weight maintenance after weight loss (45). None of the studies focused on only diet. Collectively they involved 707 participants, 521 of whom received an intervention utilizing OSNs. Study and baseline participant characteristics are presented in Table 1.
Figure 1.
Online Social Network Search Flow Diagram
Table 1.
Participant Baseline Characteristics
| Reference | Intervention Groups |
n | % Completion Rate |
% Female |
% Minority |
Age (yrs.) | BMI (kg/m2) |
PA (min/wk.) |
Health Status | Length weight loss |
Length follow- up |
Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PA Intervention | ||||||||||||
| Valle et al. | OSN: Self-help group | 41 | 82.9 | 90.2 | 12.2 | 32.7 ± 4.2 | 29.1 ± 8.9 | MVPA < 150 | Previously diagnosed with cancer and had been in remission and completed treatment over 1 year ago. Participants could have no other medical conditions(s) or contraindications. | 12 wks. | NA | Weight, BMI, PA |
| OSN+Support | 45 | 71.1 | 91.1 | 6.7 | 30.8 ± 5.7 | 28.4 ± 8.2 | ||||||
| PA+Diet | ||||||||||||
| Greene et al. | OSN Intervention | 180 | 68.0 | NR by group | NR by group. | NR by group. | NR | All PA = 2056 | Healthy individuals | 6 mos. | NA | Weight, triglycerides, LDL, HDL, PA |
| Control | 169 | 68.0 | 78.9 | 7.3 | Range: 18–79 | All PA = 1951 | ||||||
| Napolitano et al. | OSN | 17 | 100 | NR by group | NR by group | NR by group | NR by group | NR | Healthy individuals | 8 wks. | NA | Weight, PA |
| OSN+Support | 18 | 88.9 | 86.5 | 42.3 | 20.5 ± 2.2 | 31.36+−5.3 | ||||||
| Control | 17 | 100 | ||||||||||
| Sepah et al. | Single group design: OSN Intervention | 220 | 85 | 62.0 | 49.8 | 45.8 ± 9. 7 | 36.6 ± 7.5 | NR | Self-reported diagnosis of prediabetes | 16 wks | 12 mos. | Weight, HbA1C |
| Pagoto et al. | Single group design: OSN Intervention | 12 | 100 | 92.0 | 25.0 | 43.6±12.4 | 34.1 ± 3.6 | NR | Healthy individuals | 12 wks | NA | Weight |
PA Interventions
PA Study Characteristics
Sample size/completion rate
The sample size for the study using a PA intervention delivered using an OSN was 86. The proportion of randomized participants who completed the intervention and provided data for comparison was 77%.
Study length
The length of the study was 12 weeks.
Intervention components
Valle et al. (42) randomized participants into an OSN: Self-help group or an OSN group facilitated by a HE (OSN+Support) with the primary aim to increase PA. An established publically available OSN platform (Facebook) was used. Both groups received weekly messages through the OSN that featured resources on PA, overcoming exercise barriers, goal setting, and social support. All participants also received a pedometer to self-monitor steps. The OSN+Support group received additional behavioral therapy materials as well as access to a separate online PA tracking site. HEs facilitated interaction with the OSN+Support group by posting discussion questions, links to videos, and weekly reminders.
Outcomes assessed
In addition to weight, the study assessed changes in BMI, light PA, and moderate to vigorous PA
PA Intervention Results
PA
Valle et al. (42) reported a significant increase in moderate to vigorous PA (OSN: Self-help=46.3 min/wk; OSN+Support=67.0 min/wk), however, the between group difference was not statistically significant. Valle et al. (42) reported a significant increase in light intensity PA in the OSN+Support group only. Total PA significantly increased in both OSN groups, however there were significant between group differences. The difference for change between groups was not significant.
Body weight
The mean weight loss was 0.1% for the OSN: Self-help group and 2.6% in the OSN+Support group. The weight change in the OSN+Support group was statistically significant from baseline to 12 weeks compared to no significant change over time in the OSN: self-help group. Weight change between groups were not significant.
BMI
The mean BMI modestly yet significantly decreased for the OSN+Support group (−0.6kg/m2) while the OSN: Self-help group remained relativity unchanged (+0.01kg/m2).
Chronic disease risk factors
Valle et al. (42) did not present data on any chronic disease risk factors
Diet and PA Interventions
Eighty percent of the studies selected for this review (N=4), included both diet and PA components (43–46). Two studies compared weight loss between participants randomly assigned to an OSN intervention group/groups vs. a control group (43, 44) One study was not randomized but provided data for both a weight loss and a self-guided weight maintenance intervention (45). With the exception of the trial by Sepah et al (45), who reported both efficacy and intent-to-treat results, all other randomized trials employed an efficacy approach.
Diet and PA Study Characteristics
Sample size/completion rate
The range for sample size across the studies was 12–349. The range of participants who completed the intervention and provided data for weight loss was 68–100%.
Study length
The range in intervention length of the studies was 8–24 weeks with one study conducting a follow-up after an eight-month maintenance intervention.
Intervention components
Platforms
Two of the four studies used an established publically available OSN platform (Facebook/Twitter) (44). Two other studies created a study-specific OSN accessible only by study participants (43, 45). These OSN allowed participants to connect (‘friend”) others in the network, send individual messages, make public group postings, view other group member’s postings, and “like” comments of their peers to express social support and empathy.
Diet
All studies employed an energy restricted meal plan diet during the active intervention (43–46). Only one study reported specific calorie goals given to participants (44).
PA
All studies provided exercise recommendations and encouraged participants to increase PA (43–45). Two studies reported a specific exercise goal of gradually increasing moderate-vigorous PA to 150 minutes per week (46) and 250 minutes per week (44).
Self-monitoring
One study provided both accelerometers and a wireless scale that had the capability to upload directly to the OSN for feedback (43). Sepah et. al. (45) supplied wireless scales that had capabilities to upload directly to the OSN and reported self-monitoring of PA and diet but did not specify the methods used to monitor these components (45). Napolitano et. al. (44) randomized participants into two OSN groups. The first group had minimal contact with HE but received weekly podcasts, handouts, access to polls, and healthy activity events through the OSN. The second group received the same OSN content however they were given additional intervention targets (e.g. goal setting, self-monitoring, etc.), digital scale, and a pedometer to track steps as well as receiving personalized feedback from HEs through text messaging. Pagoto et. al. (46) required participants to have personal scales to qualify for the study. Self-reported weights were emailed to HEs and energy intake was report through a mobile app (MyFitnessPal).
Comparison Groups
Two of the three studies had randomized control groups (43, 44). One study provided print materials to the control participants regarding sample meal plans, recommendations on serving sizes and PA, and information regarding the benefits of PA and healthy eating (43) while the other study had a no contact waitlist control (44). All other studies implemented a single group design (45, 46).
Outcomes assessed
In addition to body weight, two of the four trials assessed PA levels via questionnaire (43, 44), one study assessed HBA1C (45), and one study assessed triglycerides, low density lipoproteins (LDL), high-density lipoprotein (HDL) (43). One study with assessments after a long term maintenance period assessed HbA1C (45).
Diet and PA Intervention Results
Results for all studies both diet and PA components are presented in Table 2.
Table 2.
Comparison of change in weight, body composition, and chronic disease risk factors
| Reference | Intervention Groups | Weight kg/% | BMI | Total PA (min/wk.) | Triglycerides | LDL | HDL | HbA1C |
|---|---|---|---|---|---|---|---|---|
| PA Intervention | ||||||||
| Valle et al. | OSN: Self-help group | −0.1/−0.1NS | +0.01NS | 76* | NA | NA | NA | NA |
| OSN+Support | −2.1/−2.6* | −0.6* | 237* | NA | NA | NA | NA | |
| PA+Diet | ||||||||
| Greene et al. | OSN Intervention | −2.4/−2.8* | NA | +631NS | +2.6NS | +0.1NS | −3.4NS | NA |
| Control | −0.7/−0.8NS | NA | +298NS | +6.1NS | +4.2NS | −3.0NS | NA | |
| Napolitano et al. | OSN | −0.63/NANR | NA | NS | NA | NA | NA | NA |
| OSN+Support | −2.4kg/NANR | NA | NS | NA | NA | NA | NA | |
| Control | −0.24kg/NANR | NA | NS | NA | NA | NA | NA | |
| Sepah et al. | Single group design: OSN Intervention | WL: −5.0/−5.0* | NA | NA | NA | NA | NA | +0.03 |
| WM: −4.9/4.8* | NA | NA | NA | NA | NA | −0.37* | ||
| Pagoto et al. | Single group design: OSN Intervention | −2.5/−3.0NR | NA | NA | NA | NA | NA | NA |
Body weight
The range of weight loss for the four studies that provided both diet and PA components was −0.63 kg to −5.0 kg for the OSN intervention groups. Napolitano et. al. (44) reported significantly greater weight loss when OSN was supplemented with additional HE feedback (−2.4±2.5 kg) compared to a self-guided OSN group (−0.63±2.4kg) or a no treatment control (−0.24±2.6kg). Percent weight change was not reported and could not be calculated since baseline weight was not available. Greene et. al. (43) observed greater weight loss in the OSN intervention group (−2.4kg; 2.8%) compared to a no contact control group (0.73kg; 1.0%) however these differences were not significant. Sepah et al. (45) evaluated weight change following 16 weeks of active weight loss and a 12 month self-guided weight maintenance period. An intent to treat analysis indicated mean weight loss of 4.1% and 4.0% at 16 weeks and 12 months, respectively. Program engagement was strongly associated with weight loss. Weight loss among participants who completed all lessons (5.6%) was significantly greater than among participants who did not complete one or more lessons??? (3.2%). Pagoto et. al. reported a mean weight loss of 2.5 kg (3.0%). Clinically significant weight loss (i.e., ≥5% of baseline weight) was observed in 42% of the sample (5/12) e,), 33% (4/12) lost < 5%, and 25% (3/12) gained weight (46).
BMI
No trial reported end study data for BMI.
Chronic disease risk factors
Two of the four studies reported changes in chronic disease risk factors (43, 45). Greene et al. (43) reported no significant between or within group differences for change in triglycerides, or for LDL, or HDL values. Sepah et al. (45) reported no significant change in HbA1C levels following completion of the weight loss intervention (16 weeks). At end of the maintenance intervention (12 months) the within group change from baseline in HbA1C were statistically significant. Napolitano et. al. (44), and Pagoto et. al. (46) did not report disease risk factors.
PA
Two of the four studies reported changes in PA levels (43, 44). Napolitano et al. (44) reported no significant between or within group differences among groups PA level. Greene et al. (43) reported the OSN intervention group significantly increased their leisure time walking (+164%) compared to the control group (+47%) however there was no significant between or within group differences for time spent in all PA.
Risk of bias
The risk of bias is presented in Table 3. Of the three studies that used randomized design (42–44) the description of the procedures for random sequence generation were unclear in 2 of the studies (67%) (43, 44). One study adequately described randomization procedures and was considered low risk of bias (42). No trials described procedures for allocation concealment. The blinding of participants and personnel is not feasible in a study comparting delivery methods. While blinding of personnel performing outcome assessments is feasible, these procedures were not employed in any of the randomized studies (42–44) and is not feasible in studies using a single group design (45, 46). The risk of attrition bias was high in one trial where the study sample represented approximately 68% of those randomized at baseline (43). The most important other source of potential bias was inadequate statistical power. None of the studies included in this review (42–46) reported adequate statistical power to detect between group differences for change in body weight.
Table 3.
Study Risk of Bias
| Reference | Random Sequence Generation (selection bias) | Allocation concealment (selection bias) | Blinding participants and personnel (performance bias) | Blinding of outcome assessment (detection bias) | Incomplete outcome data (attrition bias) | Selective reporting (reporting bias) | Other bias |
|---|---|---|---|---|---|---|---|
| PA Intervention | |||||||
| Valle et al. | Low Risk | NR | NA | NR | High Risk | Low Risk | Unclear |
| PA+Diet | |||||||
| Greene et al. | Unclear | NR | NA | NR | High Risk | High Risk | Unclear |
| Napolitano et al. | Unclear | NR | NA | NR | High Risk | NA | Unclear |
| Sepah et al. | NA | NA | NA | NA | High Risk | Low Risk | Unclear |
| Pagoto et al. | NA | NA | NA | NA | Low Risk | Low Risk | Unclear |
DISCUSSION
Summary of evidence
This paper provides a systematic review of five studies, which employed non-randomized and randomized study designs to address the question: Do weight management interventions delivered by OSNs effectively improve body weight, body composition, and chronic disease risk factors? As in previous reviews (31–33), our literature search identified multiple internet-based behavioral studies that have utilized components of OSNs such as bulletin boards, chat rooms, etc. however, the OSN was not the primary delivery method. Instead these components were used as add-ins or optional tools in the intervention so these studies were excluded. Based on our review, the literature on the effectiveness of weight management interventions delivered through OSNs is extremely limited. Thus, conclusions regarding the effectiveness of this weight management approach are currently not possible, and will require additional trials.
Although limited, available results suggest the potential for weight management delivered using OSNs. For example, weight loss, although modest, was statistically significant in the OSN groups independent of intervention length in all 5 studies included in this review. Both participant compliance in completing study modules, and interaction with the HE, appear to be associated with improved weight loss with an OSN intervention. For instance, both Napolitano et al. (44) and Valle et al. (42) reported participation of trained HEs, who provided professional advice and feedback, resulted in superior intervention effects compared to those who received a self-guided OSN intervention. Thus, OSN interventions may decrease the burden on healthcare staff conducting weight loss interventions; however, staff involvement appears to be an important component for success. In addition to weight loss, significant changes in PA were reported in the OSN arms in two of the three studies providing data on this outcome. However, PA in these studies was measured by self-report questionnaire, not objectively. Thus, the PA results should be interpreted cautiously. Our review identified two studies that compared changes in chronic disease risk factors (43, 45). Greene et al. showed no beneficial changes in triglyceride, HDL, and LDL levels between individuals in the OSN group compared to controls (43). These results are most likely attributed to the minimal weight loss (2.8%) in the OSN group. Sepah et al. observed no significant decrease in HbA1C, levels following active weight loss (16 weeks); however, levels significantly decrease at end of weight maintenance intervention (12 months) (45). This review did not identify any studies that measured body composition or other chronic disease risk factors (e.g. blood pressure, waist circumference, insulin, glucose).
It has been hypothesized that OSNs, with their ability to reach large numbers of individuals, would provide a potentially cost-effective strategy for weight management. However, to date, the cost-effectiveness and feasibility of using OSN interventions in clinical weight management has not been evaluated.
Limitations in the available literature
Several important limitations in the literature were identified resulting in an Evidence Level of Low relative to addressing the primary question regarding OSNs interventions impact on body weight, body composition and chronic disease risk factors. First, the literature is limited by a lack of studies that have addressed this question. This review identified only five studies that satisfied inclusion criteria (42–46). Second, the studies included in this review were of short duration (< 6 months) and were not statically powered to address this question of interest. Only one study had an active weight loss period of at least 6 months (43). Additionally, only Sepah et al. (45) reported any type of weight maintenance/follow-up results. Third, adherence to diet and PA recommendations, changes in caloric intake, or objectively measured changes in PA were not reported in any study. Fourth, there was a variety of OSN utilized by each study so no conclusions on effectiveness of individual OSN platform type can be concluded from this review. Examination of these factors would provide needed insight into whether or not OSN interventions produce measurable behavioral changes. Finally, no study has assessed the cost effectiveness of OSN interventions. As cost saving is the main appeal to using OSNs, a formal cost-analysis is important.
Limitations of this review
These conclusions should be cautiously interpreted as they are based on data from a limited number of studies. In addition, we did not contact authors to obtain missing data or for clarification of any information presented in the published reports; therefore missing information may reflect reporting bias as opposed to any limitations in the conduct of the study.
Conclusions
The use of OSNs for weight management is in the early stages of development and evaluation. Although the results from the studies reviewed show promise for the OSN approach, more research is needed to acquire additional information regarding methods for optimizing and increasing the effectiveness of weight management delivered using OSNs. As previously discussed, the available literature on this topic is extremely limited and suffers numerous methodological shortcomings. Therefore, we recommend randomized trials to specifically evaluate the efficacy of OSN interventions on weight loss and chronic disease risk factors that include the following: 1) adequate statistical power to detect clinically significant differences, 2) assessment of measures such as caloric intake and PA using objective methods, 3) evaluation if the cost-effectiveness, and 4) evaluation of the impact of participant characteristics (age, gender, BMI, race/ethnicity).
Acknowledgments
None
Footnotes
Declaration of conflicting interests
The Authors declare that there is no conflict of interest
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Algazy J, Gipstein S, Riahi F, Tryon K. Why governments must lead the fight against obesity. Medicine. 2009;361(23):2252–60. [Google Scholar]
- 3.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology. 2014;63(25_PA):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 4.Wing R. In: Behavioral approaches to the treatment of obesity. 2. Bray GABC, editor. New York: Marcel Dekker, Inc; 2004. pp. 147–67. [Google Scholar]
- 5.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12(Suppl):151S–62S. doi: 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- 6.Wadden TA, Berkowitz RI, Womble LG, et al. Effects of sibutramine plus orlistat in obese women following 1 year of treatment by sibutramine alone: a placebo-controlled trial. Obesity Research. 2000;8(6):431–7. doi: 10.1038/oby.2000.53. [DOI] [PubMed] [Google Scholar]
- 7.Jeffery RW, Sherwood NE, Brelje K, et al. Mail and phone interventions for weight loss in a managed-care setting: Weigh-To-Be one-year outcomes. Int J Obes Relat Metab Disord. 2003;27(12):1584–92. doi: 10.1038/sj.ijo.0802473. [DOI] [PubMed] [Google Scholar]
- 8.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166(15):1620–5. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 9.Van Wier MF, Ariens GA, Dekkers JC, et al. Phone and e-mail counselling are effective for weight management in an overweight working population: a randomized controlled trial. BMC Public Health. 2009;9:6. doi: 10.1186/1471-2458-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harvey-Berino J, West D, Krukowski R, Prewitt E, et al. Internet delivered behavioral obesity treatment. Prev Med. 2010;51(2):123–8. doi: 10.1016/j.ypmed.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manzoni GM, Pagnini F, Corti S, et al. Internet-based behavioral interventions for obesity: an updated systematic review. Clin Pract Epidemiol Ment Health. 2011;7:19–28. doi: 10.2174/1745017901107010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krukowski RA, Tilford JM, Harvey-Berino J, et al. Comparing behavioral weight loss modalities: incremental cost-effectiveness of an internet-based versus an in-person condition. Obesity (Silver Spring) 2011;19(8):1629–35. doi: 10.1038/oby.2010.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Appel LJ, Clark JM, Yeh HC, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365(21):1959–68. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hellerstedt WL, Jeffery RW. The effects of a telephone-based intervention on weight loss. Am J Health Promot. 1997;11(3):177–82. doi: 10.4278/0890-1171-11.3.177. [DOI] [PubMed] [Google Scholar]
- 15.Digenio AG, Mancuso JP, Gerber RA, et al. Comparison of methods for delivering a lifestyle modification program for obese patients: a randomized trial. Ann Intern Med. 2009;150(4):255–62. doi: 10.7326/0003-4819-150-4-200902170-00006. [DOI] [PubMed] [Google Scholar]
- 16.Neve M, Morgan PJ, Collins CE. Weight change in a commercial web-based weight loss program and its association with website use: cohort study. J Med Internet Res. 2011;13(4):e83. doi: 10.2196/jmir.1756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rock CL, Flatt SW, Sherwood NE, et al. Effect of a free prepared meal and incentivized weight loss program on weight loss and weight loss maintenance in obese and overweight women. JAMA. 2010;304(16):1803–10. doi: 10.1001/jama.2010.1503. [DOI] [PubMed] [Google Scholar]
- 18.Sherwood NE, Crain AL, Martinson BC, et al. Keep it off: a phone-based intervention for long-term weight-loss maintenance. Contemp Clin Trials. 2011;32(4):551–60. doi: 10.1016/j.cct.2011.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donnelly JE, Goetz J, Gibson C, et al. Equivalent weight loss for weight management programs delivered by phone and clinic. Obes. 2013;21(10):1951–9. doi: 10.1002/oby.20334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: randomized controlled trial. J Med Internet Res. 2009;11(1):e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zickuhr K, Smith A. Home broadband 2013. 2013. [Google Scholar]
- 22.Sheet SNF. Pew Research Internet Project. 2014. [Google Scholar]
- 23.Ellison NB. Social network sites: Definition, history, and scholarship. Journal of Computer-Mediated Communication. 2007;13(1):210–30. [Google Scholar]
- 24.Turner JW, Grube JA, Meyers J. Developing an optimal match within online communities: An exploration of CMC support communities and traditional support. Journal of Communication. 2001;51(2):231–51. [Google Scholar]
- 25.Eysenbach G, Powell J, Englesakis M, Rizo C, et al. Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions. Bmj. 2004;328(7449):1166. doi: 10.1136/bmj.328.7449.1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jayanti RK, Singh J. Pragmatic learning theory: an inquiry-action framework for distributed consumer learning in online communities. Journal of Consumer Research. 2010;36(6):1058–81. [Google Scholar]
- 27.Hwang KO, Ottenbacher AJ, Green AP, et al. Social support in an Internet weight loss community. International journal of medical informatics. 2010;79(1):5–13. doi: 10.1016/j.ijmedinf.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wu J-J, Chen Y-H, Chung Y-S. Trust factors influencing virtual community members: A study of transaction communities. Journal of Business Research. 2010;63(9):1025–32. [Google Scholar]
- 29.Poncela-Casasnovas J, Spring B, McClary D, et al. Social embeddedness in an online weight management programme is linked to greater weight loss. Journal of The Royal Society Interface. 2015;12(104):20140686. doi: 10.1098/rsif.2014.0686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright KB, Rains S, Banas J. Weak-Tie Support Network Preference and Perceived Life Stress Among Participants in Health-Related, Computer-Mediated Support Groups. Journal of Computer-Mediated Communication. 2010;15(4):606–24. [Google Scholar]
- 31.Ashrafian H, Toma T, Harling L, et al. Social Networking Strategies That Aim To Reduce Obesity Have Achieved Significant Although Modest Results. Health Affairs. 2014;33(9):1641–7. doi: 10.1377/hlthaff.2014.0370. [DOI] [PubMed] [Google Scholar]
- 32.Maher CA, Lewis LK, Ferrar K, et al. Are health behavior change interventions that use online social networks effective? a systematic review. Journal of medical Internet research. 2014;16(2) doi: 10.2196/jmir.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chang T, Chopra V, Zhang C, et al. The role of social media in online weight management: systematic review. Journal of medical Internet research. 2013;15(11) doi: 10.2196/jmir.2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Donnelly JE, Herrmann SD, Lambourne K, et al. Does increased exercise or physical activity alter ad-libitum daily energy intake or macronutrient composition in healthy adults? A systematic review. PLoS One. 2014;9(1):e83498. doi: 10.1371/journal.pone.0083498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Washburn R, Lambourne K, Szabo A, et al. Does increased prescribed exercise alter non-exercise physical activity/energy expenditure in healthy adults? A systematic review. Clin obes. 2014;4(1):1–20. doi: 10.1111/cob.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Washburn RA, Szabo AN, Lambourne K, et al. Does the method of weight loss effect long-term changes in weight, body composition or chronic disease risk factors in overweight or obese adults? A systematic review. PLoS One. 2014;9(10):e109849. doi: 10.1371/journal.pone.0109849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; updated March 2011. [Google Scholar]
- 41.Berkman ND, Lohr KN, Ansari M, McDonagh M, Balk E, Whitlock E, et al. Grading the strength of a body of evidence when assessing health care interventions for the effective health care program of the Agency for Healthcare Research and Quality: an update. 2013 [PubMed] [Google Scholar]
- 42.Valle CG, Tate DF, Mayer DK, et al. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. Journal of Cancer Survivorship. 2013;7(3):355–68. doi: 10.1007/s11764-013-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greene J, Sacks R, Piniewski B, et al. The impact of an online social network with wireless monitoring devices on physical activity and weight loss. Journal of primary care & community health. 2012 doi: 10.1177/2150131912469546. 2150131912469546. [DOI] [PubMed] [Google Scholar]
- 44.Napolitano MA, Hayes S, Bennett GG, et al. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 45.Sepah SC, Jiang L, Peters AL. Translating the Diabetes Prevention Program into an Online Social Network Validation against CDC Standards. The Diabetes Educator. 2014 doi: 10.1177/0145721714531339. 0145721714531339. [DOI] [PubMed] [Google Scholar]
- 46.Pagoto SL, Waring ME, Schneider KL, et al. Twitter-Delivered Behavioral Weight-Loss Interventions: A Pilot Series. JMIR research protocols. 2015;4(4):e123. doi: 10.2196/resprot.4864. [DOI] [PMC free article] [PubMed] [Google Scholar]