Abstract
Background:
Clinical evidence regarding the ability of braces to decrease the risk of curve progression to surgical threshold in patients with adolescent idiopathic scoliosis (AIS) continues to strengthen. Unfortunately, there is still a great deal of uncertainty regarding the impact of brace wear on psychosocial well-being or the impact of psychological well-being on brace wear adherence. The purpose of this study is to evaluate psychosocial well-being, in particular body image and quality of life (QOL), and brace wear adherence in female AIS patients undergoing brace treatment.
Methods:
The Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) was a multicenter, controlled trial using randomized and preference assignments into an observation or brace treatment group. BrAIST patients were skeletally immature adolescents diagnosed with AIS having moderate curve sizes (20 to 40 degrees). Patients in the bracing group were instructed to wear a thoracolumbosacral orthosis, at least 18 h/d. Scores on the Spinal Appearance Questionnaire and the PedsQL4.0 Generic Scales from 167 female BrAIST patients who were randomized to brace treatment (n=58) and patients who chose brace treatment (n=109) were analyzed.
Results:
At baseline and at 12 months, no differences were found between the least-adherent brace wear group (<6 h/d) and most-adherent brace wear group (≥12 h/d) patients in terms of major curve, body image, and QOL. In the most-adherent group, poorer body image scores were significantly correlated with poorer QOL scores at baseline, at 6 months, and at 12 months but not at 18 months. In general, body image scores and QOL scores were not significantly correlated in the least-adherent group. When comparing patients that had a ≥6 degree increase of their major curve between baseline and 12 months to patients that did not, there were no significant differences in body image or QOL scores.
Conclusions:
For females adolescents with AIS, body image and QOL do not have a significant impact on brace wear adherence and are subsequently not significantly impacted by brace wear.
Level of Evidence:
Level II—therapeutic (prospective comparative study).
Key Words: scoliosis, adolescent brace treatment, adherence, body image, quality of life, QOL, well-being, psychological, BrAIST
Adolescent idiopathic scoliosis (AIS) is an abnormal curvature of the spine, which develops during puberty, and is the most prevalent musculoskeletal deformity affecting children.1 Global rates of AIS range from 0.9% to 12% and within this population approximately 10% of adolescents will eventually need some form of treatment.2 For the past 45 years, the most common nonsurgical treatment of AIS has been brace treatment. The objective of bracing is to stop curve progression and restore normal alignment of the spine by using active pressure from the brace. Recommended brace wear is typically at least 18 h/d with treatment lasting from 2 to 4 years until the end of bone growth or until the curve progresses to 50 degrees, which is an indication for surgery.3 Recent evidence from the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) confirmed the effectiveness of brace treatment, including a strong dose-response relationship, in preventing spinal curve progression to the threshold for surgery.4,5
Although clinical evidence regarding bracing effectiveness continues to strengthen, there is still uncertainty regarding the impact of brace wear on psychosocial well-being, as well as the impact of psychological well-being on brace wear adherence. Some research has found that full-time brace wear can negatively impact a patient’s, emotional, and social well-being, including a significant worsening of body image.6 In addition, research has found that the adverse effects on a patients’ psychosocial well-being induced by brace treatment can then result in poor brace wear adherence.7–9 Furthermore, some research indicates that interventions aimed at improving poor psychological outcomes can improve brace adherence.9,10 However, other research has found no negative impact on psychological well-being induced by brace treatment.11–15
Some of the discrepancies in the brace wear adherence research could be due to the type of brace wear data used to assess adherence. The majority of research on brace wear adherence is based on subjective reports, such as self-reports through brace wear diaries and logs. In these studies adherence rates have ranged from 41% of wearing hours/prescribed to as high 100% of wearing hours prescribed.16,17 According to Hunter et al, using subjective reports of brace wear adherence has been a major barrier for research assessing relationships between brace wear adherence and clinical and/or psychosocial outcomes.17 This study addressed this limitation, by using monitor data from BrAIST rather than self-reports to assess relationships among body image, quality of life (QOL), and brace wear adherence.
The secondary aims of BrAIST were to assess whether there are any substantial psychosocial effects induced by brace treatment. This study used data from BrAIST, including subject questionnaires, brace monitor data, and clinical data regarding physical deformity. The purpose of this study was to assess relationships, including changes over time, among body image, QOL, major curve, and brace wear adherence in female adolescents with AIS.
METHODS
BrAIST was a multicenter trial (22 sites in the United States and 3 sites in Canada) that either randomized (randomized arm) adolescents into 2 treatment groups (brace or observation) or allowed the adolescent to choose (preference arm) brace treatment or observation. Adolescents in BrAIST were considered to be at highest risk for major curve progression due to their age, skeletal immaturity, and degree of the major curve. Adolescents in the study had major curves between 20 and 40 degrees at baseline and had no previous orthopaedic treatment (brace or surgery) for treatment of AIS. Adolescents were instructed to wear a thoracolumbosacral orthosis, such as a Boston, Wilmington, or one of several other thoracolumbosacral orthosis brace designs, for at least 18 h/d and were asked to wear a monitor in their brace to track brace wear adherence. BrAIST found brace wear with a mean of <6 h/d was associated with a 41% success rate (skeletal maturity without curve progression <50 degrees or more), which was similar to the success rate of 48% in the observation group.4 Brace wear averaging at least 12.9 h/d was associated with success rates of 90% to 93%.4 On the basis of these findings, this study categorized patients as “least-adherent” (0 to 6 h/d) or “most-adherent” (>12 h/d). Baseline brace wear was determined from monitor data within the first 2 months of brace wear.
Owing to the small number of males in this population, only females were included in this study. Adolescents could switch treatment, to observation or to brace, at any point during the study. Female adolescents (n=37) that switched from observation to brace treatment were also included in the study. For female adolescents that switched to brace treatment, the visit that they started brace treatment became their baseline visit.
The Scoliosis Research Society defines brace treatment failure as an increase in curve magnitude of at least ≥6.18 Therefore, this study also assessed whether body image and QOL were impacted by changes in the major curve over time by grouping adolescents that had an increase that was ≥6 degrees in the major curve at the 12-month follow-up visit and those that did not.
The SAQ scores include the following 3 body image domains: appearance, expectations, and total score. The appearance domain (items 1 to 7, and 9) measures how the adolescent thinks she currently looks by using pictures of body areas oftentimes effected by AIS that include varying levels of deformity. Each picture is ranked on a 5-point scale with varying levels of deformity with 5 being the most deformed. The appearance domain scores range from 8 to 40. The SAQ expectation domain (items 10 to 17) is also ranked on a 5-point scale with 5 indicating a strong desire to look more “normal” regarding some aspect of their appearance such as wanting more even hips or shoulders. The expectation domain scores range from 8 to 40. The SAQ total score is the sum of the appearance domain and the expectation domain (range, 16 to 80). Higher SAQ total scores indicate a larger discrepancy between how individuals’ think they currently look (appearance domain) and how they want to look (expectation domain), which is an indication of overall poor body image. Previous research indicates that the SAQ is a valid measure of body image.19,20
Patients also completed the PedsQL 4.0 Generic Corse Scales at each visit. The PedsQL has been shown to distinguish health-related QOL between healthy children and children with chronic illnesses.21,22 Scores on the PedsQL range from 0 to 100 with higher scores indicating better QOL. The questionnaire consists of 23 items applicable to healthy populations, as well as populations with acute and chronic health conditions. The QOL measures include the following psychosocial domains: health and activities, feelings, how well one gets along with others, and school.
The SAQ and QOL scores were not normally distributed therefore the Wilcoxon rank-sum test was used for comparison between the 2 brace wear adherent groups. Spearman rank correlation was conducted to explore correlations within each adherent group. Finally, for comparison of variable change over time within groups, paired t tests were conducted. All significance tests were 2-tailed and conducted at the 5% significance level.
RESULTS
In the study population (n=167), the mode of the appearance score was 2, which was the second least distorted picture of the 5 images of physical distortion and the mode for the expectation score was 2, which was a “somewhat true” response to wanting to look more normal regarding certain aspects of the body. The following were the median scores of each SAQ body image domain: appearance was 17, expectation was 16, and total score was 34. The mean QOL score at baseline was 84.6 (±13.7), which is similar to the healthy adolescent population.22
At baseline, 126 (75%) of female patients were in the least-adherent group (n=39) or the most-adherent (n=92) brace wear groups. In general, the curve patterns or location of the curvature did not have an effect on brace adherence. There were no significant differences between the least-adherent and the most-adherent groups with regard to age, body mass index, QOL scores, and SAQ’s appearance, expectation, and total scores. Table 1 describes the baseline demographic, clinical, SAQ body image domains, and QOL by least-adherent and most-adherent brace wear groups.
TABLE 1.
Brace Baseline Characteristics for Least-adherent and Most-adherent Brace Wear
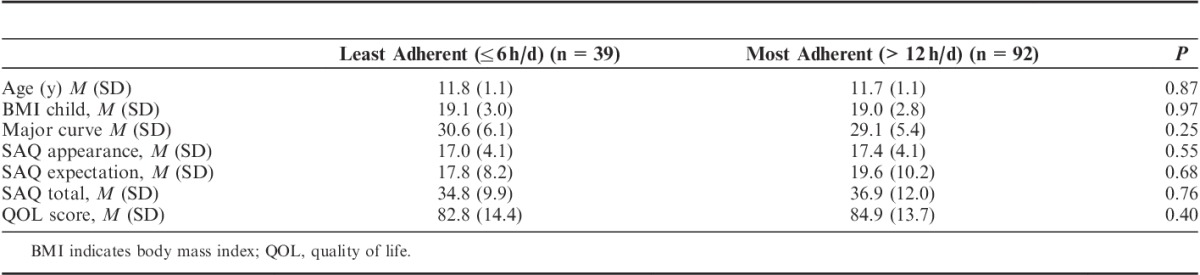
Table 2 summarizes the relationships between body image scores and QOL in the least-adherent and most-adherent groups at baseline, 6, 12, and 18 months.
TABLE 2.
Spearman Rank Correlations in SAQ Scores With Adherence and QOL Over Time
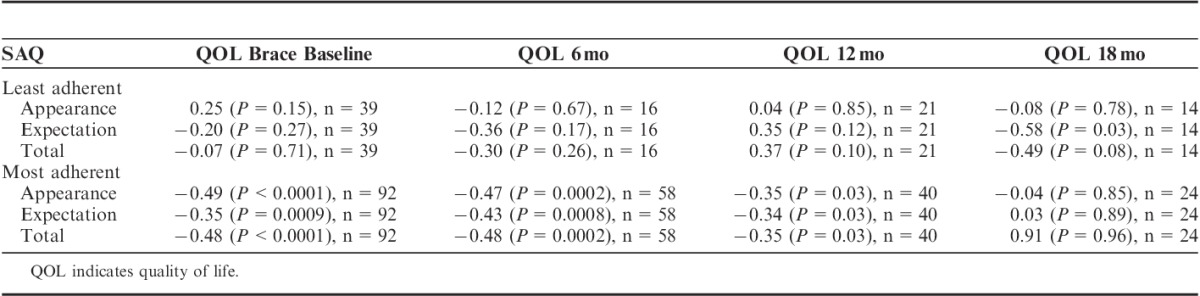
In general, there were no significant correlations between SAQ body image domains and QOL in the least-adherent group. In the most-adherent group, all 3 body image domains had significant negative correlations with QOL at baseline, 6 months, and 12 months, which indicates poorer body image is significantly correlated with poorer QOL. However, there were no longer significant correlations between body image domains and QOL at the 18-month visit.
Table 3 summarizes the SAQ body image domains, QOL, and brace wear adherence between groups and within groups for patients who did or did not have a ≥6 degree increase in major curve during the first 12 months of brace treatment.
TABLE 3.
Comparisons Between and Within Female Adolescents Having (Progression) and Not Having a ≥6 Degree Increase (No Progression) in Major Curve at the Brace Baseline and 12-month Visits

There were no significant differences at baseline or at the 12-month visit in SAQ body image scores and QOL scores between adolescents that had a ≥6 degree increase in major curve compared with those that did not. In addition, there were no changes within each progression change group in body image scores or in QOL scores between the brace baseline and 12-month visit.
DISCUSSION
Previous research regarding the impact of brace wear adherence on psychosocial well-being and the impact of psychosocial well-being on brace wear adherence was conflicting. This study addressed several weakness of previous AIS research by using data from BrAIST. BrAIST was an innovative study because it combined components never included in previous AIS research including: being a multicenter trial, having a randomized control group, an a priori determination of effect size, use of blinded clinical outcome measurements, and use of objective brace wear monitor data to measure brace wear adherence.5
The purpose of this study was to assess whether there were any substantial negative psychosocial effects induced by brace treatment or whether poor psychosocial well-being negatively impacted brace wear adherence. This study analyzed relationships among brace wear adherence, body image, and QOL. When looking at differences between the least-adherent and the most-adherent brace wear groups, findings from this study supply no evidence that the amount of brace wear negatively impacts body image or QOL, or that poor body image and poor QOL negatively impacts brace wear adherence.
Results from this study do not support research suggesting that brace wear has a negative impact on body image and QOL, but corroborates previous studies which found brace treatment did not negatively impact psychosocial well-being.11–14 Results from this study are similar to previous BrAIST findings comparing females with AIS that were untreated (observation) to brace-treated females, which found that brace-treated females did not have significantly poorer body image or QOL compared with females undergoing observation.11
Although there were no differences in body image and QOL between least-adherent and most-adherent groups, findings from this study suggest that for female adolescents that already have poor body image and poor QOL, wearing a brace for >12 hours may add another layer of distress to psychological well-being. However, the lack of significant correlations between body image and QOL at 18 months in the most-adherent treatment group suggests that adolescents may develop coping skills and adjust to the brace over time. These findings support several research studies indicating that, over time, adolescents undergoing brace treatment may develop self-protective, coping strategies that enables them to adapt to their new body image, and reestablish their social lives.9,11,13 Finally, results from this study indicate that, regardless of the amount of brace wear and whether adolescents had a significant worsening (≥6 degrees) of their major curve over time, body image and QOL were not significantly impacted in the first 12 months of brace treatment.
A limitation of this study might be the relatively small number of females in some of the adherence and degree of major curve progression groups over time and therefore the comparisons and correlations lack statistical power. Furthermore, although several studies have found the SAQ to be a valid and reliable measure for measuring body image19,20 other studies have found that adolescents had difficulty reading and comprehending the SAQ.23
Results from this study, in particular that the amount of time the brace was worn did not adversely impact body image and QOL, should be relayed to clinicians, adolescents, and parents so they can weigh the psychosocial risks and the lack of psychosocial risks with the clinical benefits of brace treatment. In addition, findings from this study indicate that adolescent’s body image and QOL should be assessed throughout brace treatment. When body image distress and/or poor QOL are detected, efforts should be made to improve both. If efforts to improve body image and QOL are not successful, the physician, adolescent, and parents should weigh the psychosocial risks with the clinical benefits of brace treatment and determine whether brace treatment and the amount of current prescribed brace wear is appropriate. For example, the benefit of reducing brace wear to <13 h/d might be more beneficial psychologically and socially than the clinical benefits of wearing the brace for >13 h/d.
Footnotes
The devices(s)/drugs(s) that is/are the subject of this manuscript is/are exempt from FDA or corresponding national regulations. The project described was supported by Award Numbers R21AR049587 and R01AR052113 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (S.L.W., PI); the Shriners Hospitals for Children (#79125, M.B. Dobbs, PI); the Canadian Institutes of Health Research (FRN-81050, J.G. Wright, PI); the University of Rochester (J.O. Sanders, PI); the Children’s Mercy Hospital and Clinics (N.J. Price, PI); and the Children’s Miracle Network (S.L.W., PI). For the remaining authors none were declared.
The authors declare no conflicts of interest.
REFERENCES
- 1.Nachemson AL, Lonstein JE, Weinstein SL. Report of the prevalence and natural history committee of the Scoliosis Research Society. Denver: Scoliosis Research Society; 1982. [Google Scholar]
- 2.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Spine (Phila Pa 1976). 2010;35:1285–1293. [DOI] [PubMed] [Google Scholar]
- 3.Schiller JR, Thakur NA, Eberson CP. Brace management in adolescent idiopathic scoliosis. Clinical Orthopaedics and Related Research. 2010;468:670–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369:1512–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein SL, Dolan LA, Wright JG, et al. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST). Spine (Phila Pa 1976). 2013;21:1832–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pham VM, Houlliez A, Caprentier A, et al. Determination of the influence of the Cheneau brace on quality-of-life for adolescent with idiopathic scoliosis. Ann Readapt Med Phys. 2007;51:3–8. [DOI] [PubMed] [Google Scholar]
- 7.Rivett L, Rothberg A, Stewart A, et al. The relationship between quality of life and compliance to a brace protocol in adolescents with idiopathic scoliosis: a comparative study. BMC Musculoskeletal Disorders. 2009;10:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan SL, Cheung KM, Luk KD, et al. A correlation study between in-brace correction, compliance to spinal orthosis and health-related quality of life of patients with adolescent idiopathic scoliosis. Scoliosis. 2014;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Donnelly MJ, Dolan LA, Grande L, et al. Patient and parent perspectives on treatment for adolescent idiopathic scoliosis. The Iowa Orthopaedic Journal. 2004;24:76–83. [PMC free article] [PubMed] [Google Scholar]
- 10.Matsunaga S, Hayashi K, Naruo T, et al. Psychologic management of brace therapy for patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2005;30:547–550. [DOI] [PubMed] [Google Scholar]
- 11.Hasler CC, Wietlisbach S, Buchler P. Objective compliance of adolescent girls with idiopathic scoliosis in a dynamic SpineCor brace. J of Children's Orthop. 2010;4:211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwieger T, Campo S, Weinstein SL, et al. Body Image and Quality-of-Life in Untreated Versus Brace-Treated Females with Adolscent Idiopathic Scoliosis. Spine (Phila Pa 1976). 2016;41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Danielsson AJ, Wiklund I, Pehrsson K, et al. Health-related quality of life in patients with adolescent idiopathic scoliosis: A matched follow-up at least 20 years after treatment with brace or surgery. Eur Spine J. 2001;10:278–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merenda L, Costello K, Santangelo AM, et al. Perceptions of self-image and physical appearance: Conversations with typically developing youth and youth with idiopathic scoliosis. Orthop Nurs. 2011;30:383–390. [DOI] [PubMed] [Google Scholar]
- 15.Olafsson Y, Saraste H, Ahlgren R. Does bracing affect self-image? A prospective study on 54 patients with adolescent idiopathic scoliosis. Eur Spine J. 1999;8:401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miller DJ, Franzone JM, Matsumoto H, et al. Electronic monitoring improves brace-wearing compliance in patients with adolescent idiopathic scoliosis: A randomized clinical trial. Spine (Phila Pa 1976). 2012;37:717–721. [DOI] [PubMed] [Google Scholar]
- 17.Hunter LN, Sison-Williamson M, Mendoza MM, et al. The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine (Phila Pa 1976). 2008;33:1554–1561. [DOI] [PubMed] [Google Scholar]
- 18.Richards SB, Bernstein RM, D’Amato CD, et al. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS committee on bracing and nonoperative management. Spine (Phila Pa 1976). 2005;30:2068–2075. [DOI] [PubMed] [Google Scholar]
- 19.Sanders JO, Harrast JJ, Kuklo TR, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2719–2722. [DOI] [PubMed] [Google Scholar]
- 20.Carreon LY, Sanders JO, Polly DW, et al. Spinal appearance questionnaire: factor analysis, scoring, reliability, and validity testing. Spine (Phila Pa 1976). 2011;36:1240–1244. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Limbers CA, Burwinkle TM. The PedsQL in type 1 and type 2 diabetes feasibility, reliability, and validity of the pediatric quality of life inventory. Diabetes Care. 2008;31:672–677. [DOI] [PubMed] [Google Scholar]
- 22.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales in healthy and patient populations. Med Care. 2001;39:800–812. [DOI] [PubMed] [Google Scholar]
- 23.Mulcahey MJ, Chafetz RS, Santangelo AM, et al. Cognitive testing of the spinal appearance with typically developing youth and youth with idiopathic scoliosis. J Pediatr Orthop. 2011;31:661–667. [DOI] [PubMed] [Google Scholar]


