Introduction
The HIV epidemic in Peru disproportionally affects male sex workers (MSWs), with an estimated one in four MSWs being infected with HIV (1), compared with prevalences of 12.4% among men who have sex with men (MSM) in Lima (2) and 0.4% among the general population nationwide. (3,4) Existing yet limited HIV prevention efforts in Peru have focused on MSWs, who have specific social, cultural, and behavioral characteristics that place them at high risk for acquisition and transmission of HIV and sexually transmitted infections (STIs). (5)
Many of the behaviors that place sex workers at high risk for HIV acquisition, though not unique to the profession, have been well-documented.(6) Globally, MSWs have been shown to have numerous (7) and diverse sexual contacts, (8) high rates of sex without a condom, high prevalence of STIs, (5) and high rates of substance abuse. (9) In Peru, existing research shows additional factors that place MSM and MSWs at high risk of HIV acquisition, including work location, (10) sexual role, (11) and high risk sexual networks. (12)
Another significant risk factor shown to be associated with HIV infection is the experience of violence. (13–22) As defined by the World Health Organization (WHO), violence is “the intentional use of physical force or power, threatened or actual, against oneself, another person, or against a group or community, that either results in or has a high likelihood of resulting in injury, death, psychological harm, maldevelopment, or deprivation.” (23) For sex workers and other key groups, the existing literature focuses on intimate partner violence (IPV), which includes stable and casual non-paying partners, and client violence, which includes paying partners. IPV and client violence can be further separated into physical, emotional/psychological, and sexual violence. For the purposes of this paper, violence experience will refer to both IPV and client violence.
Violence has been well characterized in several key groups, including female sex workers (FSWs) and MSM, with results showing high rates of violence experienced. (24–30) In the context of male sex work, cross-sectional studies have consistently shown that being a victim of violence is a significant part of being a MSW, with reported rates of violence experienced by MSWs ranging from 24% per year in Spain (31) to 28% per year in Russia (9) to 57% in the past 5 years in Shanghai (32) to 44% lifetime in San Francisco. (33)
Across different general and key populations, studies have linked IPV and client violence with high risk sexual behavior and STI/HIV infection. (34–40) For example, two notable longitudinal studies of women in South Africa and women in Uganda both found a significant temporal relationship between IPV and HIV. (19,41) Studies of FSWs and MSM have also shown correlations between IPV and both sexual risk behaviors and STI/HIV prevalence. (13,15,17,24,28,29,42–48)
Despite the high rates of violence experienced by MSWs and its association with high risk sexual practices and STI/HIV in other populations, little research has addressed this link in MSWs. We were only able to find three published studies that examined the association of violence and high risk behaviors in MSWs; notably, none of these studies were from Latin America and none found significant associations of violence with a biologic outcome. (49–51)
Another overlooked aspect in violence literature is whether victims of IPV and client violence are also perpetrators of violence. Studies of perpetrators of violence in the general population have found that men who perpetrate violence against females are more likely to engage in sexual risk behaviors (52–54) and be diagnosed with HIV/STIs. (55) A study of heterosexual couples in Peru found that violence victims and perpetrators have strikingly similar personal characteristics, which has important implications for violence prevention strategies. (56) However, most studies among key populations, including FSWs, MSM and MSWs, focus only on whether these groups are victims of IPV and client violence. In fact, we were unable to find any studies that explored whether MSWs are perpetrators of violence.
IPV and client violence are important drivers of direct and indirect morbidity and mortality in different populations around the world and have justifiably received significant research attention. (36,57,35) However, MSWs remain under-represented in the violence literature. Street-based sex workers are specifically under-represented, an important oversight given their consistently high rates of reported HIV/STIs and violence experience. (32,50,51) The aims of this study, therefore, were to address this gap, by 1) characterizing the IPV and client violence experienced by a cohort of street-based MSWs in Lima, Peru, including being a victim and being a perpetrator of such violence and 2) examining whether an association exists between this violence experience and inconsistent condom use and HIV prevalence. The hypotheses were 1) MSWs experience a significant amount of IPV and client violence and 2) violence experience is associated with sexual risk behaviors and therefore potential HIV transmission.
Methods
Study Participants
The current study is part of a pilot randomized controlled trial to assess the initial efficacy of a skill building center intervention to prevent HIV and other STIs among MSWs in Lima. The current study is a cross-sectional analysis of the baseline characteristics of study participants. Data collection took place between January and August 2014.
In 2013, ethnographic mapping identified commercial sex venues of MSWs in Lima. (58) Peer-based recruiters revisited street-based venues in 2014 and invited MSWs to participate in the skill building center. The use of the ethnographic map and recruiters familiar with the MSW community limited potential selection bias by recruiting broadly, rather than from a single venue or population. After confirmation of eligibility by the study team and provision of verbal consent by the participant, the MSW initiated his study participation. Eligibility criteria included: 1) born male and self-identified as male (non-transgender); 2) had traded sex for money, goods, or services at least once in the previous week; 3) resided in Lima; 4) age 15 or older; 5) able and willing to provide informed consent.
All appropriate institutional review boards, specifically the University of California, Los Angeles and Universidad Peruana Cayetano Heredia (Lima, Peru), reviewed and approved the study. All participants provided their verbal informed consent prior to enrolling and participating in any study activities.
Behavioral and Biologic Assessment
Participants completed behavioral surveys and testing for HIV. Behavioral surveys were completed using computer assisted personal interviewing (CAPI), through which the trained interviewers asked the participants the questions and completed the participant responses on the computer. The survey, which took approximately 90 minutes, assessed several topics, including: demographic characteristics, alcohol use (CAGE questionnaire), (59) any drug use in the past month, sexual role and orientation, sexual risk behaviors, and violence experience.
The main exposure variables in the current study are experience of non-paying IPV and/or client violence as a victim and/or perpetrator in the past six months. First, participants were asked about whether they had been victims of violence. Being a victim of violence was divided into three types: physical (“Has a sexual partner hit you or thrown an object at you?”), emotional (“Has a sexual partner harmed you emotionally?”), or sexual (“Has a sexual partner forced you to have a sexual encounter when you didn't want one?”). For each affirmative answer, the participant indicated whether the perpetrator was an 1) intimate partner or 2) client and a 1) man, 2) transwoman, or 3) woman. Next, participants were asked about whether they had perpetrated physical, emotional, or sexual violence against their intimate partners or clients. As with victimization, for each affirmative answer the participant indicated whether his victim was an intimate partner or client and a man, transwoman, or woman.
The men were dichotomized into 1) victims and 2) non-victims and 1) perpetrators and 2) non-perpetrators. Each man who experienced at least one of the three types of violence (physical, emotional, or sexual) as a victim was labeled a victim, independent of his perpetrator status. Similarly, each man who perpetrated at least one of the three types of violence was labeled a perpetrator, independent of his victim status. It is important to note that for multivariable modeling, violence experience is not exclusive (i.e. men can be both victims and perpetrators of violence and men can experience more than one type of violence).
The main outcome variables are experience of condomless anal intercourse (CLAI) and HIV status. Participants were asked about condom use during anal intercourse with male and/or transwomen sexual partners in the previous three months. Men were separated into two groups, those who reported one or more partners with whom they had CLAI (inconsistent condom users) versus those who reported no CLAI (consistent condom users). This dichotomization is appropriate because consistent condom users have been shown to be 10-20 times less likely to acquire HIV when exposed to the virus as compared with inconsistent or non-condom users. (60) Further, condom usage is the main risk reduction strategy to which this cohort of MSWs has access and knowledge. Given the different HIV/STI risk profiles with male and transwomen versus female sexual partners, we excluded female partners in our analysis.
To determine HIV status, we carried out rapid HIV testing using a finger-stick blood specimen (Bioline HIV 1/2 3.0, Standard Diagnostics, Korea), with confirmatory testing by HIV-1 antibody immunofluorescence assay (IFA) for reactive rapid tests. (61) All participants received pre- and post-test counseling. Men with positive HIV tests who were not yet linked to the Ministry of Health were referred to care and accompanied by a study staff member for one or more visits if they desired.
Data Analysis
Univariate analysis examined the prevalence and distributions of the MSWs' violence experience. Chi-squared testing was performed to analyze differences in demographics and violence experience by the two main outcomes, CLAI experience and HIV status. Generalized linear models (GLM), poisson distribution with robust variance, were used for bivariate and multivariable analyses. Bivariate analysis was performed with each exposure variable to estimate prevalence ratios (PR) of CLAI and HIV status. GLM multivariable modeling was used to analyze the association of violence experience with CLAI and HIV status through four separate models. GLM was chosen rather than logistic regression in order to calculate prevalence ratios, which have been demonstrated to be more conservative, consistent, and interpretable relative to odds ratios. (62) Dose responses were analyzed by using a Wilcoxon-type score test for trend (63) to measure whether experiencing an increased number of different types of violence (i.e., physical, emotional and/or sexual) was associated with CLAI and/or HIV status.
The first two multivariable models had the experience of being a victim of violence as the main exposure variable, with CLAI and HIV status as the outcomes, respectively. The second two models had the experience of being a perpetrator of violence as the main exposure variable, again with CLAI and HIV status as the outcomes. The models were adjusted for: age (continuous), education (incomplete vs. complete high school), sexual role (activo/insertive vs. pasivo/receptive or moderno/versatile), CLAI (for the HIV model), and HIV status (for the CLAI model). (64) Confounding variables were chosen a priori based on prior research and then excluded from the final model if they were not statistically associated with the outcomes or the main exposures in bivariate analysis. Thus, substance abuse and number of sexual partners in the previous three months were excluded from the model (data not presented). Each variable analyzed included data from all study participants (no missing data). All analyses were performed using Stata 12.1. P values <0.05 were considered significant.
Results
Study Demographics and Overall Violence Experience
A total of 210 street-based MSWs participated in this study (Table 1). One third of the men had a stable partner at the time of the survey, many of whom were female (63%), followed by male (27%) and transwomen (10%). In contrast, the overwhelming majority of clients were male (91%), versus 7% transwomen and 2% female. The average number of clients per MSW in the previous three months was 31, with a median of 20 (interquartile range of 8 -37).
Table I. Characteristics of Male Sex Workers. Lima, Peru, 2014 (n=210).
| Characteristics of the study participants | Total | Condomless anal intercourse (CLAI) with male/transwomen partners (previous 3 months) | HIV Status | |||
|---|---|---|---|---|---|---|
| No (0 partners) | Yes (≥1 partners) | Positive | Negative | |||
| n=210 n (%) |
n=120 n (%) |
n=90 n (%) |
n=51 n (%) |
n=159 n (%) |
||
| Victim of Violencea (previous 6 months) | 89 (42.4%) | 40 (33.3%) | 49 (54.4%)** | 30 (58.8%)** | 59 (37.1%) | |
| Perpetrator of Violencea | 81 (38.6%) | 38 (31.7%) | 43 (47.8%)* | 25 (49.0%) | 56 (35.2%) | |
| Both Victim and Perpetratora | 57 (27.1%) | 23 (19.2%) | 34 (37.8%)** | 21 (41.2%)* | 36 (22.6%) | |
| No Violence Victimization or Perpetrationa | 97 (46.2%) | 65 (54.2%)** | 32 (35.6%) | 17 (33.3%) | 80 (50.3%)* | |
| Age, Mean (SD) | 25.4 (6.2) | 25.1 (6.3) | 25.8 (6.0) | 27 (5.9)* | 24.9 (6.2) | |
| Completed high school | 122 (58.1%) | 72 (60.0%) | 50 (55.6%) | 35 (68.6%) | 87 (54.7%) | |
| Alcohol abuse (CAGE ≥ 2) | 130 (61.9%) | 71 (59.2%) | 59 (65.6%) | 28 (54.9%) | 102 (64.2%) | |
| Any drug Use (previous month) | 79 (37.6%) | 54 (45.0%)* | 25 (27.8%) | 15 (29.4%) | 64 (40.3%) | |
| Self described sexual role | Activo (insertive) | 140 (66.7%) | 94 (67.1%) | 46 (32.9%) | 18 (12.9%) | 122 (87.1%) |
| Pasivo (receptive) | 9 (4.3%) | 3 (33.3%) | 6 (66.7%) | 3 (33.3%) | 6 (66.7%) | |
| Moderno (versatile) | 61 (29.0%) | 23 (37.7%) | 38 (62.3%)*** | 30 (49.2%)*** | 31 (50.8%) | |
| Self described sexual orientation | Heterosexual | 51 (24.4%) | 38 (74.5%) | 13 (25.5%) | 1 (2.0%) | 50(98.0%) |
| Homosexual | 38 (18.2%) | 16 (42.1%) | 22 (57.9%)** | 17 (44.7%)*** | 21 (55.3%) | |
| Bisexual | 120 (57.4%) | 66 (55.0%) | 54 (45.0%)** | 33 (27.5%)*** | 87 (72.5%) | |
Chi-squared testing was used to analyze associations between the exposures (left column) and the main outcomes (CLAI and HIV status).
p<0.05,
p<0.01,
p<0.001
Experience of physical, emotional or sexual intimate partner or client violence (previous 6 months)
Over half the men (n=113, 54%) reported experiencing at least one type of violence, either as a victim or a perpetrator, in the previous six months. Men reported similar rates of being a victim (n=89, 42%) and a perpetrator (n=81, 39%), though for sexual violence men were more likely to report being victims (n=34, 16%) than perpetrators (n=14, 7%). Of the 89 men reporting being a victim of violence, 64% (57/89) were also perpetrators, and of the 81 men reporting being a perpetrator of violence, 70% (57/81) were also victims. This association between being a victim and a perpetrator was statistically significant (p<0.001).
MSWs as Victims of Violence
As mentioned, 42% or 89 of the men reported being a victim of at least one type of violence, with 53 men (25%) reporting physical, 56 (27%) emotional, and 34 (16%) sexual violence. Forty-six men (22%) were the victims of one type of violence, 32 (15%) of two types, and 11 (5%) of all three types of violence. Having been the victim of one type of violence was significantly associated with having been the victim of the other types of violence (p<0.01).
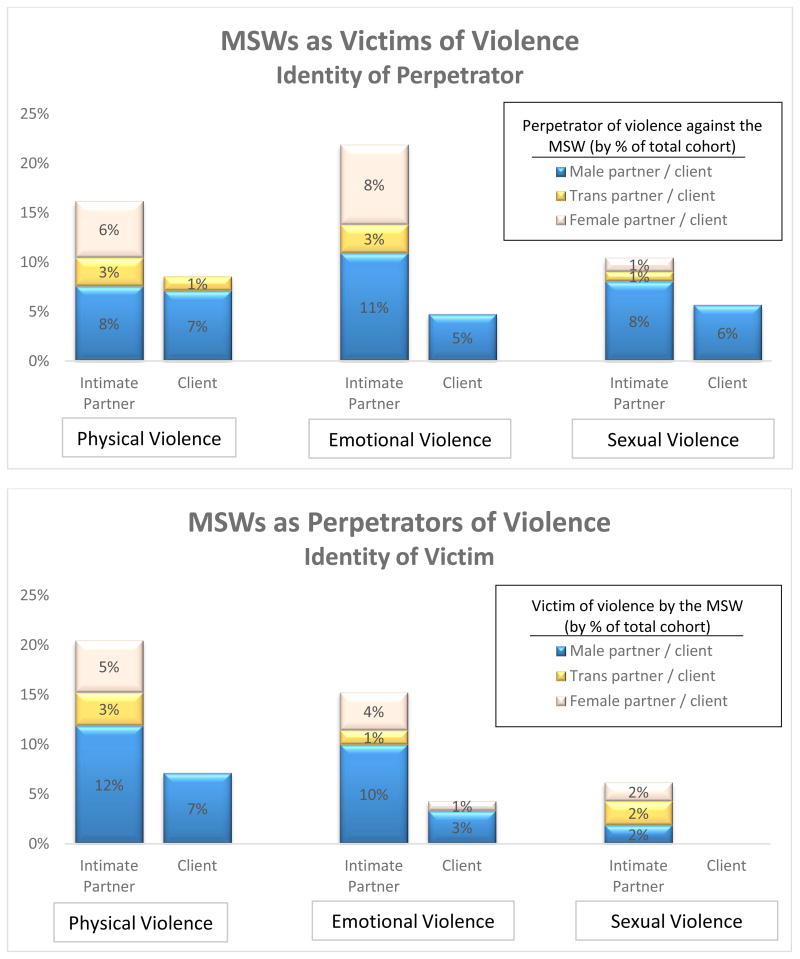
The majority of violence against MSWs was committed by intimate partners, with 75% (67/89) of MSWs who were violence victims reporting aggression by an intimate partner and 38% (34/89) reporting aggression by a client. Further, 27% of the MSWs reported being victims at the hands of men, 11% reported being victims of violence by women, and 6% by transwomen. The top panel of Figure 1 presents a more detailed breakdown of violence against MSWs by type of violence and the identity of the violence aggressor.
Figure 1.
Figure 1 shows the identity of the other person involved in the physical, emotional, or sexual violence, as a percent of the total cohort. The top panel shows how frequently MSWs were victims of violence and who committed the violence against MSWs. For example, 11% of MSWs were victims of emotional violence by male intimate partners. The bottom panel shows how frequently MSWs were perpetrators of violence and against whom the MSWs committed violence. For example, 10% of MSWs were perpetrators of emotional violence against male intimate partners.
*please include Figure 1 in color if possible.
MSWs as Perpetrators of Violence
As with violence victimization, about 4 in 10 (39%, 81/210) of the MSWs reported being perpetrators of recent violence, with 58 men (28%) reporting physical, 41 (20%) emotional, and 14 (7%) sexual violence perpetration. Fifty-four men (26%) perpetrated one type of violence, 22 (10%) two types, and 5 (2%) all three types of violence. As with violence victimization, having been the perpetrator of one type of violence was significantly associated with having been the perpetrator of the other types of violence (p<0.01).
The majority of violence perpetration by MSWs was committed against their intimate partners. Of the 81 men who reported being violence perpetrators, 79% (64/81) reported perpetrating violence against intimate partners and 28% (23/81) reported perpetrating violence against clients. Further, 26% of the MSWs reported having perpetrated violence against men, 10% against women, and 5% against transwomen. The bottom panel of Figure 1 presents a more detailed breakdown of violence perpetrated by MSWs by type of violence and the identity of their victim.
Violence and its Association with CLAI and HIV Status
Of the 210 MSWs in the study, 90 (43%) reported inconsistent condom use during anal intercourse with male and/or transwomen sexual partners in the previous three months. Fifty-one men (24%) tested positive for HIV.
In descriptive (Table I) and bivariate (Table II) analyses, CLAI was significantly associated both with being a victim and being a perpetrator of violence. In the multivariable model (Table II), CLAI remained significantly associated with being a victim of violence (adjusted Prevalence Ratio (aPR)=1.49 (95% Confidence Interval (CI) 1.09 – 2.03)) and with being a perpetrator of violence (aPR=1.39 (95%CI 1.03 – 1.87)) (Table II).
Table II. Adjusted and Unadjusted Prevalence of Recent Condomless Anal Intercourse (CLAI) with Male and Transwomen Partners and HIV among Male Sex Workers. Lima, Peru, 2014 (n=210).
| Victimization of Intimate Partner or Client Violence as the Main Exposure | ||||
|---|---|---|---|---|
|
| ||||
| Any Recent CLAI (unadjusted) | Any Recent CLAI (adjusted) | HIV Status (unadjusted) | HIV Status (adjusted) | |
| Prevalence Ratio (CI) | Prevalence Ratio (CI) | Prevalence Ratio (CI) | Prevalence Ratio (CI) | |
| Victim of recent violence | 1.62 (1.19-2.22)* | 1.49 (1.09-2.03)* | 1.62 (1.19-2.22)* | 1.65 (1.04-2.62)* |
| Age (Continuous) | 1.01 (0.99-1.03) | 1.01 (0.99-1.04) | 1.04 (1.01-1.07)* | 1.04 (0.99-1.07) |
| Education (Ref: Incomplete high school) | 0.90 (0.66-1.23) | 0.72 (0.53-0.99)* | 1.58 (0.93-2.67) | 1.07 (0.65-1.77) |
| Sexual Role (Ref: Activo) | 1.91 (1.42-2.58)* | 1.84 (1.32-2.54)* | 3.67 (2.23-6.04)* | 3.08 (1.85-5.14)* |
| Any Recent CLAI | - | - | 2.25 (1.36-3.70)* | 1.47 (0.90-2.40) |
| HIV Status | 1.72 (1.28-2.31)* | 1.26 (0.91-1.74) | - | - |
|
| ||||
| Perpetration of Intimate Partner or Client Violence as the Main Exposure | ||||
|
| ||||
| Any Recent CLAI (unadjusted) | Any Recent CLAI (adjusted) | HIV Status (unadjusted) | HIV Status (adjusted) | |
| Perpetrator of recent violence | 1.46 (1.07-1.98)* | 1.39 (1.03-1.87)* | 1.53 (0.95-2.46) | 1.45 (0.92-2.29) |
| Age (Continuous) | 1.01 (0.99-1.03) | 1.02 (0.99-1.04) | 1.04 (1.01-1.07)* | 1.04 (1.00-1.08)* |
| Education (Ref: Incomplete high school) | 0.90 (0.66-1.23) | 0.72 (0.53-0.99)* | 1.58 (0.93-2.67) | 1.07 (0.65-1.76) |
| Sexual Role (Ref: Activo) | 1.91 (1.42-2.58)* | 1.85 (1.34-2.54)* | 3.67 (2.23-6.04)* | 3.12 (1.87-5.20)* |
| Any Recent CLAI | - | - | 2.25 (1.36-3.70)* | 1.53 (0.93-2.49) |
| HIV Status | 1.72 (1.28-2.31)* | 1.31 (0.96-1.78) | - | - |
Table II shows the unadjusted and adjusted results of bivariate and multivariable modeling, using generalized linear models, poisson distribution with robust variance. The outcome (dependent) variables are at the top of each column and the exposure (independent) variables are to the left of each row. The top section of the table shows the models with being a victim of violence as the main exposure and the bottom section shows the models with being a perpetrator of violence as the main exposure. Violence includes physical, emotional or sexual violence by intimate partners or clients in the last 6 months.
In descriptive and bivariate analyses, HIV infection was significantly associated with being a victim of violence and was borderline significantly associated with being a perpetrator of violence. In multivariable modeling, HIV status was again significantly associated with being a victim of violence (aPR=1.65 (95% CI 1.04 – 2.62). However, having HIV was not significantly associated with having perpetrated violence (aPR=1.45 (95% CI 0.92 – 2.29)); a larger sample size might reveal a significant association.
A dose-response was observed for both outcomes (Table III). Experience of increasing numbers of violence types (physical, emotional, sexual) was associated with a higher likelihood of CLAI, a significant trend seen in both victims and perpetrators (p<0.001 and p=0.005, respectively). As with CLAI, there was a dose response in that an increasing number of violence types experienced was significantly associated with an increasing likelihood of HIV infection among violence victims (p=0.004). This significant association was not observed for perpetrators (p=0.118).
Table III. Dose Response of MSW Victimization and Perpetration of Intimate Partner or Client Violence to Recent Condomless Anal Intercourse (CLAI) with Male and Transwomen Partners and HIV among Male Sex Workers. Lima, Peru, 2014 (n=210).
| MSWs as Victims of Intimate Partner or Client Violence | ||
|---|---|---|
|
| ||
| Number of types of violence experienced as victim | Any Recent CLAI (p<0.001) | HIV Positive (p=0.004) |
| 0 (n=121) | 41 (34%) | 21 (17%) |
| 1 (n=46) | 22 (48%) | 14 (30%) |
| 2 (n=32) | 18 (56%) | 11 (34%) |
| 3 (n=11) | 9 (82%) | 5 (45%) |
|
| ||
| MSWs as Perpetrators of Intimate Partner or Client Violence | ||
|
| ||
| Number of types of violence experienced as perpetrator | Any Recent CLAI (p=0.005) | HIV Positive (p=0.118) |
| 0 (n=129) | 47 (36%) | 26 (20%) |
| 1 (n=54) | 25 (46%) | 16 (30%) |
| 2 (n=22) | 15 (68%) | 8 (36%) |
| 3 (n=5) | 3 (60%) | 1 (20%) |
Table III examines the dose response of recent condomless anal intercourse (CLAI) and HIV status to the number of types of violence experienced in the last 6 months. The top section of the table examines the associations of CLAI and HIV status with the number of types of violence (physical, emotional, sexual) experienced as a victim; the bottom section examines these associations with the number of types of violence experienced as a perpetrator. P values were calculated using a Wilcoxon-type score test for trend (reference 62).
Discussion
These results show that Peruvian MSWs face alarmingly high rates of IPV and client violence victimization. In addition, they reported a high rate of violence perpetration against their intimate, non-client partners. Over half of the cohort had experienced some form of IPV or client violence in the previous six months, either as a victim or perpetrator. The results regarding who is committing the violence against MSWs and who are the victims of violence by MSWs, especially the role of intimate partners and in particular female intimate partners, represent important additions to the literature. Finally, the associations between IPV and client violence and inconsistent condom use during anal sex and HIV status warrant attention.
Forty-two percent of MSW participants reported having been victims of IPV and/or client violence in the previous six months, consistent with prior studies that report high rates of violence against MSWs in other settings. (9,31,32,49,50) MSWs face many barriers to preventing and addressing violence, making it likely that the high prevalences reported are under-representative of the actual amount of violence MSWs are experiencing. Sex work, and male sex work in particular, has historically been a profession surrounded by stigma and shame, causing hesitancy in coming forward with job-related harms. (65,66) Regulations against prostitution also make it difficult and often dangerous for MSWs to report violence against them, especially if the violence occurred in the context of sex work. (67) Even if reported, the police may not seriously investigate the offense or even deny that a sex worker, given the nature of his/her work, can be forced to have sex; (65) even more isolating, police are often the perpetrators of this violence. (68) Stigmatization and criminalization of sex work can have consequences outside of the legal system as well. Previous research has shown that fear of discrimination is an important factor that keeps sex workers from using public services, such as medical, housing, or other social services, that could potentially address experiences of violence, thus increasing the likelihood of continued violence and other negative outcomes. (69) The high amount of violence reported in the current study, taken in the context of these barriers, underscore the need for violence prevention among this vulnerable population.
While much past research with MSWs focuses on violence by clients against sex workers, it is important to note that in this context, intimate partners are actually more common sources than clients of physical, emotional and sexual violence. Same-sex intimate partnerships may face power inequalities that can lead to IPV, similar to the gender-based power inequalities that have been shown to be associated with IPV in heterosexual couples. (24) Studies have shown that IPV rates among same-sex couples are similar to those in heterosexual couples. (70) In fact, unique characteristics in same-sex couples (such as the threat of outing the victimized partner, increased isolation, and lack of civil protection (71)) often facilitate violence perpetration.
The current study is the first globally to our knowledge that examines IPV and client violence perpetration by MSWs. The previous lack of perpetration data has several important consequences. First, the health effects associated with violence perpetration, such as adverse mental health outcomes and increased sexual risk behaviors, cannot be elucidated without epidemiologic data on violence perpetration. (72) Second, it is not possible to assess and therefore address risk factors for IPV or client violence perpetration without first knowing the characteristics of the perpetrators. Thus, the detailed perpetrator data presented provides a first step towards closing this gap in the violence literature.
The association between violence, high risk sexual behaviors, and HIV found in this study is an especially important consideration for a cohort of MSWs. Our results mirror the findings of previous studies with other key groups, showing a significant association between violence victimization and high risk sexual behaviors, even after adjustment for confounding factors. (13,17,32,34,39,43,73) However, this study is the first to our knowledge that shows violence perpetration by MSWs is significantly associated with high risk sexual behavior. Further, this is the first study in which being a victim of IPV and client violence has been significantly associated with a biological outcome, HIV status, in MSWs.
Well-documented associations exist that explain how IPV and client violence can lead to increased HIV risk. The most obvious means is infection during a sexual assault; indeed, forced sex is more likely to be physically traumatic (74) and perpetrators of sexual violence are more likely to have multiple partners (54) and higher rates of STI/HIV. (29) However, sexual violence was the least prevalent type of IPV and client violence reported, either as a victim or as a perpetrator, in our cohort. Thus, not so obvious but equally important are the mechanisms that link IPV and client violence with HIV through means other than direct infection. Research on male-female relationships in several settings has found that higher levels of inequality, which often manifest through physical, emotional, and sexual violence by intimate partners, are associated with higher prevalences of STI/HIV. (21,75–77) More limited evidence has demonstrated that inequalities in male-male relationships are drivers of IPV as well. (17)
The experience of violence can have lasting effects, including outside the confines of the partnership in which the violence occurred. As an example, qualitative studies among key groups, including both FSWs (26) and MSWs, (78) have displayed that concern for physical safety makes victims more likely to acquiesce to unprotected sex. The negative effects of IPV and client violence on mental health further reduce the ability of victims to negotiate condom usage and make victims less likely to seek public health and STI testing and treatment services. (42) Past experiences of IPV and client violence have been linked with other documented drivers of HIV risk, including substance abuse, (73,78) a high number of sexual partnerships, (50) perceived helplessness, and future sexual violence. (26)
As a population with both high and stable HIV prevalence, novel preventative measures are needed for MSWs. The significant association between IPV and client violence and HIV prevalence points to violence awareness as a potential HIV prevention strategy. Encouragingly, previous work with different groups, including FSWs, has demonstrated that violence prevention interventions can contribute to dramatic reductions in violence experience. (42) Thus, there is reason to be optimistic that violence prevention strategies, such as a multilayered violence prevention intervention targeting policy makers, secondary stakeholders such as police, media and lawyers and sex workers, (42) could be effective in reducing IPV and client violence and HIV prevalence among street-based MSWs.
Limitations
This study has several limitations that deserve mention. As a recent systematic review (79) pointed out, there is no standard scale to describe IPV among MSM. The most common forms of assessing IPV have been either the Conflict Tactics Scale 2 (CTS-2) (80) or binary, single item questions based on the Center for Disease Control and WHO definitions of IPV. We chose the latter, as CDC/WHO based definitions for IPV have previously been used for Latin American and other MSM in other studies (47,81–84) and because the CTS-2 has not been validated in Latin American MSM. Future studies would benefit from a validated instrument with specific information on its psychometric properties.
As a cross-sectional study, causation cannot be concluded, only associations. Also, the structure of the survey did not allow us to determine if the violence and CLAI occurred within the same partnership. However, our theoretical framework supposes that violence experience contributes to future risk-taking behaviors and is therefore not limited to the same partnership. Further, many of the published mechanisms as to how violence increases risk taking apply outside the confines of a single relationship (e.g., condom negotiation (26,78), substance abuse (73), mental health outcomes (42)). We included different recall periods for violence experience (previous six months) and CLAI (three months). A longer time frame was chosen for violence for two reasons. One, as a less frequent event than CLAI, a shorter time period might miss important violence experiences. Second, being that it occurs less frequently and is often a traumatic event for those involved, we hypothesized that distant recall would be more accurate. Regarding anal intercourse and CLAI, given that anal intercourse is a very frequent event among MSWs, a longer time period would be difficult for participants to recall with accuracy. Finally, we limited our sample to men who engaged in sex work at least once in the previous week since our study centered on men who relied on sex work as their main source of income.
Social desirability and recall bias could cause underreporting of sexual risk behaviors and violence victimization and perpetration, though MSW participants in a previous study in Lima proposed CAPI as a tool to reduce such biases. (5) We dichotomized the variables of violence and CLAI into ever versus never experienced. This dichotomization simplifies the model. However, it also increases the accuracy, as it is easier to recall if an event occurred at least once versus an exact number of times. In our bivariate and multivariable models, we did not differentiate between the three types of violence. However, we did find an association between experiencing one and more than one type of violence, both for violence victimization and perpetration. This association is intuitive and adds validity to our grouping of the three types of violence. Finally, one must be cautious when generalizing the findings for street-based sex workers, especially to non-street-based MSWs who often have different demographic, economic, and social circumstances.
A different method of analysis would have been to combine victimization and perpetration into a single model, rather than a victim model and a perpetrator model. We chose the latter because in previous studies that have used a single model, many examined victimization and perpetration in the setting of relationships, labeling them as uni or bidirectionally violent. (39,85) The purpose of the current study was not to examine relationship dynamics but rather experiences of IPV and client violence and their effects. Further, the nature of street-based sex work precludes the MSWs from having exclusive intimate relationships, thus making such an analysis of relationship dynamics impractical. Finally, given our relatively small sample size, dividing the men into four rather than two groups would greatly reduce the ability of the model to find meaningful associations.
Conclusions
With over half the MSWs in our sample reporting experience of at least one form of recent IPV and/or client violence, violence is a very real and present concern for MSWs in Peru. These findings highlight individual, interpersonal relationship and public health challenges for this vulnerable population, given that a significant association was found between violence experience, inconsistent condom use, and HIV infection. Interventions to prevent violence victimization and perpetration could be a beneficial tool in a comprehensive HIV prevention strategy, especially amongst MSWs. Our findings that describe the identities of those who committed violence against and those who were victims of violence by MSWs lay a framework for additional beneficiaries of interventions in Latin America and suggest the need for such research in regions where male sex work remains under-studied.
Supplementary Material
Acknowledgments
The authors would like to acknowledge and thank all of the study participants and staff without whom this analysis would not have been possible. PEG would also like to acknowledge and thank Drs. Jesse Clark, Jordan Lake, Eddy Segura and Kelika Konda for their guidance and support throughout the research process. The pilot skills building intervention was supported by two grants from the National Institute of Health (K01TW009206, R21MH098982). PEG was supported by the University of California, Los Angeles South American Program in HIV Prevention Research (SAPHIR, NIH R25 MH 087222). The funding sources played no role in study design, data collection, analysis, and interpretation, writing of the manuscript or the decision to submit the paper for publication.
References
- 1.ANÁLISIS DE LA SITUACIÓN EPIDEMIOLÓGICA DEL VIH/SIDA EN EL PERÚ, 2013. Minist Salud Direccion Gen Epidemiol . 2013 Nov [Google Scholar]
- 2.Ugarte Ubillúz O, Arce Rodríguez M, et al. Informe nacional sobre los progresos realizados en la aplicación del UNGASS. Período: enero 2008-diciembre 2009. [cited 2014 Dec 5];Perú. 2010 Available from: http://www.bvcooperacion.pe/biblioteca/handle/123456789/6409.
- 3.García PJ, Bayer A, Cárcamo CP. The Changing face of HIV in Latin America and the Caribbean. Curr HIV/AIDS Rep. 2014 Jun 1;11(2):146–57. doi: 10.1007/s11904-014-0204-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministerio de Salud (MINSA) Perú. Lima, Peru: MINSA, ONUSIDA; 2012. Apr, Programa Conjunto de las Naciones Unidas sobre el VIH/SIDA (ONUSIDA). Informe Nacional sobre los Progresos Realizados en el País. Periodo enero 2011 - diciembre 2012. [Google Scholar]
- 5.Bayer AM, Garvich M, Díaz DA, Sánchez H, García PJ, Coates TJ. “Just getting by”: a cross-sectional study of male sex workers as a key population for HIV/STIs among men who have sex with men in Peru. Sex Transm Infect . 2014 Jan 3; doi: 10.1136/sextrans-2013-051265. doi:sextrans – 2013–051265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beyrer C, Baral SD, van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, et al. Global epidemiology of HIV infection in men who have sex with men. The Lancet. 2012 Aug 3;380(9839):367–77. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minichiello V, Mariño R, Browne J, Jamieson M, Peterson K, Reuter B, et al. A profile of the clients of male sex workers in three Australian cities. Aust N Z J Public Health. 1999 Oct 1;23(5):511–8. doi: 10.1111/j.1467-842x.1999.tb01308.x. [DOI] [PubMed] [Google Scholar]
- 8.Baral SD, Friedman MR, Geibel S, Rebe K, Bozhinov B, Diouf D, et al. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. [cited 2014 Sep 10];The Lancet [Internet] 2014 doi: 10.1016/S0140-6736(14)60801-1. Available from: http://www.sciencedirect.com/science/article/pii/S0140673614608011. [DOI] [PMC free article] [PubMed]
- 9.Baral S, Kizub D, Masenior NF, Peryskina A, Stachowiak J, Stibich M, et al. Male sex workers in Moscow, Russia: a pilot study of demographics, substance use patterns, and prevalence of HIV-1 and sexually transmitted infections. AIDS Care. 2009 Dec 2;22(1):112–8. doi: 10.1080/09540120903012551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bayer AM, Garvich M, Díaz DA, Sánchez H, García PJ, Coates TJ. When Sex Work Becomes Your Everything The Complex Linkages Between Economy and Affection Among Male Sex Workers in Peru. Am J Mens Health. 2014 Sep 1;8(5):373–86. doi: 10.1177/1557988313514769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark J, Salvatierra J, Segura E, Salazar X, Konda K, Perez-Brumer A, et al. Moderno Love: Sexual Role-Based Identities and HIV/STI Prevention Among Men Who Have Sex with Men in Lima, Peru. AIDS Behav. 2013 May 1;17(4):1313–28. doi: 10.1007/s10461-012-0210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verre MC, Peinado J, Segura ER, Clark J, Gonzales P, Benites C, et al. Socialization Patterns and Their Associations with Unprotected Anal Intercourse, HIV, and Syphilis Among High-Risk Men Who Have Sex with Men and Transgender Women in Peru. AIDS Behav. 2014 May;1:1–10. doi: 10.1007/s10461-014-0787-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koblin BA, Torian L, Xu G, Guilin V, Makki H, MacKellar D, et al. Violence and HIV-related risk among young men who have sex with men. AIDS Care. 2006 Nov 1;18(8):961–7. doi: 10.1080/09540120500467182. [DOI] [PubMed] [Google Scholar]
- 14.Lloyd S, Operario D. HIV Risk among Men Who Have Sex With Men Who Have Experienced Childhood Sexual Abuse: Systematic Review and Meta-Analysis. AIDS Educ Prev. 2012 Jun;24(3):228–41. doi: 10.1521/aeap.2012.24.3.228. [DOI] [PubMed] [Google Scholar]
- 15.Heintz AJ, Melendez RM. Intimate Partner Violence and HIV/STD Risk Among Lesbian, Gay, Bisexual, and Transgender Individuals. J Interpers Violence. 2006 Feb 1;21(2):193–208. doi: 10.1177/0886260505282104. [DOI] [PubMed] [Google Scholar]
- 16.Bedoya CA, Mimiaga MJ, Beauchamp G, Donnell D, Mayer KH, Safren SA. Predictors of HIV Transmission Risk Behavior and Seroconversion Among Latino Men Who have Sex with Men in Project EXPLORE. AIDS Behav. 2012 Apr 1;16(3):608–17. doi: 10.1007/s10461-011-9911-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunkle KL, Decker MR. Gender-Based Violence and HIV: Reviewing the Evidence for Links and Causal Pathways in the General Population and High-risk Groups. Am J Reprod Immunol. 2013 Feb 2;69:20–6. doi: 10.1111/aji.12039. [DOI] [PubMed] [Google Scholar]
- 18.Decker MR, Wirtz AL, Baral SD, Peryshkina A, Mogilnyi V, Weber RA, et al. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex Transm Infect. 2012 Jun 1;88(4):278–83. doi: 10.1136/sextrans-2011-050171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kouyoumdjian FG, Calzavara LM, Bondy SJ, O'Campo P, Serwadda D, Nalugoda F, et al. Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS May 15 2013. 2013;27(8):1331–8. doi: 10.1097/QAD.0b013e32835fd851. [DOI] [PubMed] [Google Scholar]
- 20.Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Contr Saf Promot. 2008 Dec;15(4):221–31. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maman S, Campbell J, Sweat MD, Gielen AC. The intersections of HIV and violence: directions for future research and interventions. Soc Sci Med. 2000 Feb;50(4):459–78. doi: 10.1016/s0277-9536(99)00270-1. [DOI] [PubMed] [Google Scholar]
- 22.Phillips DY, Walsh B, Bullion JW, Reid PV, Bacon K, Okoro N. The intersection of intimate partner violence and HIV in U.S. women: a review. J Assoc Nurses AIDS Care JANAC. 2014 Feb;25(1 Suppl):S36–49. doi: 10.1016/j.jana.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 23.WHO. Definition and typology of violence [Internet] [cited 2014 Sep 17];WHO. Available from: http://www.who.int/violenceprevention/approach/definition/en/
- 24.Finneran C, Stephenson R. Intimate Partner Violence Among Men Who Have Sex With Men A Systematic Review. Trauma Violence Abuse. 2013 Apr 1;14(2):168–85. doi: 10.1177/1524838012470034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shannon K, Kerr T, Strathdee SA, Shoveller J, Montaner JS, Tyndall MW. Prevalence and structural correlates of gender based violence among a prospective cohort of female sex workers. BMJ. 2009 Aug 22;339(7718):442–5. doi: 10.1136/bmj.b2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Panchanadeswaran S, Johnson SC, Sivaram S, Srikrishnan AK, Latkin C, Bentley ME, et al. Intimate partner violence is as important as client violence in increasing street-based female sex workers' vulnerability to HIV in India. Int J Drug Policy. 2008 Apr;19(2):106–12. doi: 10.1016/j.drugpo.2007.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Argento E, Muldoon KA, Duff P, Simo A, Deering KN, Shannon K. High Prevalence and Partner Correlates of Physical and Sexual Violence by Intimate Partners among Street and Off-Street Sex Workers. PLoS ONE. 2014 Jul;9(7):1–7. doi: 10.1371/journal.pone.0102129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pando MA, Coloccini RS, Reynaga E, Fermepin MR, Vaulet LG, Kochel TJ, et al. Violence as a Barrier for HIV Prevention among Female Sex Workers in Argentina. PLoS ONE. 2013 Jan;8(1):1–7. doi: 10.1371/journal.pone.0054147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dunkle KL, Jewkes RK, Murdock DW, Sikweyiya Y, Morrell R. Prevalence of Consensual Male–Male Sex and Sexual Violence, and Associations with HIV in South Africa: A Population-Based Cross-Sectional Study. PLoS Med. 2013 Jun;10(6):1–11. doi: 10.1371/journal.pmed.1001472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ramachandran S, Yonas MA, Silvestre AJ, Burke JG. Intimate partner violence among HIV-positive persons in an urban clinic. AIDS Care. 2010;22(12):1536–43. doi: 10.1080/09540121.2010.482199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Belza MJ, Llácer A, Mora R, Morales M, Castilla J, de la Fuente L. Sociodemographic characteristics and HIV risk behaviour patterns of male sex workers in Madrid, Spain. AIDS Care. 2001 Oct 1;13(5):677–82. doi: 10.1080/09540120120063296. [DOI] [PubMed] [Google Scholar]
- 32.Dunkle KL, Wong FY, Nehl EJ, Lin L, He N, Huang JM, et al. Male-on-Male Intimate Partner Violence and Sexual Risk Behaviors Among Money Boys and Other Men Who Have Sex With Men in Shanghai, China. Sex Transm Dis May 2013. 2013;40(5):362–5. doi: 10.1097/OLQ.0b013e318283d2af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cohan D, Lutnick A, Davidson P, Cloniger C, Herlyn A, Breyer J, et al. Sex worker health: San Francisco style. Sex Transm Infect. 2006 Oct;82(5):418–22. doi: 10.1136/sti.2006.020628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coker AL. Does Physical Intimate Partner Violence Affect Sexual Health? A Systematic Review. Trauma Violence Abuse. 2007 Apr 1;8(2):149–77. doi: 10.1177/1524838007301162. [DOI] [PubMed] [Google Scholar]
- 35.Campbell JC. Health consequences of intimate partner violence. The Lancet. 2002 Apr 13;359(9314):1331–6. doi: 10.1016/S0140-6736(02)08336-8. [DOI] [PubMed] [Google Scholar]
- 36.Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002 Oct 5;360(9339):1083. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- 37.Teitelman AM, Ratcliffe SJ, Dichter ME, Sullivan CM. Recent and Past Intimate Partner Abuse and HIV Risk Among Young Women. J Obstet Gynecol Neonatal Nurs. 2008 Mar 1;37(2):219–27. doi: 10.1111/j.1552-6909.2008.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mittal M, Senn TE, Carey MP. Mediators of the Relation Between Partner Violence and Sexual Risk Behavior Among Women Attending a Sexually Transmitted Disease Clinic. Sex Transm Dis June 2011. 2011;38(6):510–5. doi: 10.1097/OLQ.0b013e318207f59b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PMD. Intimate Partner Violence and Sexually Transmitted Infections Among Young Adult Women. Sex Transm Dis May 2012. 2012;39(5):366–71. doi: 10.1097/OLQ.0b013e3182478fa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gielen AC, Ghandour RM, Burke JG, Mahoney P, McDonnell KA, O'Campo P. HIV/AIDS and intimate partner violence intersecting women's health issues in the united states. Trauma Violence Abuse. 2007;8(2):178–98. doi: 10.1177/1524838007301476. [DOI] [PubMed] [Google Scholar]
- 41.Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010 Jul 3;376(9734):41–8. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- 42.Beattie TS, Bhattacharjee P, Ramesh BM, Gurnani V, Anthony J, Isac S, et al. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010 Aug 11;10(1):476. doi: 10.1186/1471-2458-10-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Swain SN, Saggurti N, Battala M, Verma RK, Jain AK. Experience of violence and adverse reproductive health outcomes, HIV risks among mobile female sex workers in India. BMC Public Health. 2011 May 20;11(1):357. doi: 10.1186/1471-2458-11-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ulibarri MD, Strathdee SA, Lozada R, Magis-Rodriguez C, Amaro H, O'Campo P, et al. Intimate partner violence among female sex workers in two Mexico–U.S. Border cities: Partner characteristics and HIV risk behaviors as correlates of abuse. Psychol Trauma Theory Res Pract Policy. 2010 Dec;2(4):318–25. doi: 10.1037/a0017500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of Co-Occurring Psychosocial Health Problems and Increased Vulnerability to HIV/AIDS Among Urban Men Who Have Sex With Men. Am J Public Health. 2003 Jun;93(6):939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Braitstein P, Asselin JJ, Schilder A, Miller M-L, Laliberté N, Schechter MT, et al. Sexual violence among two populations of men at high risk of HIV infection. AIDS Care. 2006 Oct 1;18(7):681–9. doi: 10.1080/13548500500294385. [DOI] [PubMed] [Google Scholar]
- 47.Feldman MB, Díaz RM, Ream GL, El-Bassel N. Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men. J LGBT Health Res. 2007;3(2):9–19. doi: 10.1300/J463v03n02_02. [DOI] [PubMed] [Google Scholar]
- 48.Tran A, Lin L, Nehl EJ, Talley CL, Dunkle KL, Wong FY. Prevalence of Substance Use and Intimate Partner Violence in a Sample of A/PI MSM. J Interpers Violence. 2014 Jul 1;29(11):2054–67. doi: 10.1177/0886260513516006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geibel S, Luchters S, King'ola N, Esu-Williams E, Rinyiru A, Tun W. Factors Associated With Self-Reported Unprotected Anal Sex Among Male Sex Workers in Mombasa, Kenya. Sex Transm Dis August 2008. 2008;35(8):746–52. doi: 10.1097/OLQ.0b013e318170589d. [DOI] [PubMed] [Google Scholar]
- 50.Shaw SY, Lorway RR, Deering KN, Avery L, Mohan HL, Bhattacharjee P, et al. Factors Associated with Sexual Violence against Men Who Have Sex with Men and Transgendered Individuals in Karnataka, India. PLoS ONE. 2012 Mar;7(3):1–8. doi: 10.1371/journal.pone.0031705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Biello KB, Colby D, Closson E, Mimiaga MJ. The Syndemic Condition of Psychosocial Problems and HIV Risk Among Male Sex Workers in Ho Chi Minh City, Vietnam. AIDS Behav. 2014 Jul 1;18(7):1264–71. doi: 10.1007/s10461-013-0632-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Raj A, Santana MC, La Marche A, Amaro H, Cranston K, Silverman JG. Perpetration of intimate partner violence associated with sexual risk behaviors among young adult men. Am J Public Health. 2006;96(10):1873–8. doi: 10.2105/AJPH.2005.081554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jewkes R, Dunkle K, Koss MP, Levin JB, Nduna M, Jama N, et al. Rape perpetration by young, rural South African men: Prevalence, patterns and risk factors. Soc Sci Med. 2006 Dec;63(11):2949–61. doi: 10.1016/j.socscimed.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 54.Decker MRS, Seage GRIS, Hemenway D, Raj A, Saggurti N, Balaiah D, et al. Intimate Partner Violence Functions as Both a Risk Marker and Risk Factor for Women's HIV Infection: Findings From Indian Husband-Wife Dyads. J Acquir Immune Defic Syndr August 2009. 2009;51(5):593–600. doi: 10.1097/QAI.0b013e3181a255d6. [Miscellaneous Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Raj A, Reed E, Welles SL, Santana MC, Silverman JG. Intimate Partner Violence Perpetration, Risky Sexual Behavior, and STI/HIV Diagnosis Among Heterosexual African American Men. Am J Mens Health. 2008 Sep 1;2(3):291–5. doi: 10.1177/1557988308320269. [DOI] [PubMed] [Google Scholar]
- 56.Fiestas F, Rojas R, Gushiken A, Gozzer E. ?' Quién es la víctima y quién el agresor en la violencia física entre parejas? Estudio epidemiológico en siete ciudades del Perú. Rev Peru Med Exp Salud Pública. 2012;29(1):44–52. [PubMed] [Google Scholar]
- 57.Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, et al. A Systematic Review of the Correlates of Violence Against Sex Workers. Am J Public Health. 2014 Mar 13;104(5):e42–54. doi: 10.2105/AJPH.2014.301909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bayer A, Diaz D. Enumeration of Venue-Based Male and Transwomen Sex Workers in Peru Using PLACE and Capture-Recapture. Oral Presentation presented at: 2014 STD Presentation Conference; 2014 Jun; Atlanta, GA. [Google Scholar]
- 59.Saitz R, Lepore MF, Sullivan LM, Amaro H, Samet JH. Alcohol abuse and dependence in latinos living in the united states: Validation of the cage (4m) questions. Arch Intern Med. 1999 Apr 12;159(7):718–24. doi: 10.1001/archinte.159.7.718. [DOI] [PubMed] [Google Scholar]
- 60.Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Soc Sci Med. 1997 May;44(9):1303–12. doi: 10.1016/s0277-9536(96)00258-4. [DOI] [PubMed] [Google Scholar]
- 61.Mylonakis E, Paliou M, Lally M, Flanigan TP, Rich JD. Laboratory testing for infection with the human immunodeficiency virus: established and novel approaches. Am J Med. 2000 Nov;109(7):568–76. doi: 10.1016/s0002-9343(00)00583-0. [DOI] [PubMed] [Google Scholar]
- 62.Thompson ML, Myers JE, Kriebel D. Prevalence odds ratio or prevalence ratio in the analysis of cross sectional data: what is to be done? Occup Environ Med. 1998;55(4):272–7. doi: 10.1136/oem.55.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cuzick J. A wilcoxon-type test for trend. Stat Med. 1985 Oct 1;4(4):543–7. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 64.Nemoto T, Operario D, Keatley J, Han L, Soma T. HIV Risk Behaviors Among Male-to-Female Transgender Persons of Color in San Francisco. Am J Public Health. 2004 Jul;94(7):1193–119. doi: 10.2105/ajph.94.7.1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Decker MR, Crago A-L, Chu SKH, Sherman SG, Seshu MS, Buthelezi K, et al. Human rights violations against sex workers: burden and effect on HIV. [cited 2014 Sep 22];The Lancet [Internet] doi: 10.1016/S0140-6736(14)60800-X. Available from: http://www.sciencedirect.com/science/article/pii/S014067361460800X. [DOI] [PMC free article] [PubMed]
- 66.Scott J, Minichiello V, Mariño R, Harvey GP, Jamieson M, Browne J. Understanding the New Context of the Male Sex Work Industry. J Interpers Violence. 2005 Mar 1;20(3):320–42. doi: 10.1177/0886260504270334. [DOI] [PubMed] [Google Scholar]
- 67.Aggleton P, Parker R. Men who Sell Sex: Global Perspectives [Internet] [cited 2015 Feb 6];Routledge. 2014 Available from: https://books.google.com/books?hl=en&lr=&id=11dWBQAAQBAJ&oi=fnd&pg=PT30&dq=Men+Who+Sell+Sex+Global+Perspectives&ots=_WF0CZtE-t&sig=w4JK0wBsS-e47_MrxM4BvBziVGE.
- 68.Shannon K, Csete J. VIolence, condom negotiation, and hiv/sti risk among sex workers. JAMA. 2010 Aug 4;304(5):573–4. doi: 10.1001/jama.2010.1090. [DOI] [PubMed] [Google Scholar]
- 69.Scorgie F, Vasey K, Harper E, Richter M, Nare P, Maseko S, et al. Human rights abuses and collective resilience among sex workers in four African countries: a qualitative study. Glob Health. 2013;9(1):33. doi: 10.1186/1744-8603-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bryant AS, Demian Relationship characteristics of American gay and lesbian couples: Findings from a national survey. J Gay Lesbian Soc Serv. 1994;1(2):101–17. [Google Scholar]
- 71.Rohrbaugh JB. Domestic violence in same-gender relationships. Fam Court Rev. 2006;44(2):287–99. [Google Scholar]
- 72.Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. 2002 Nov;23(4):260–8. doi: 10.1016/s0749-3797(02)00514-7. [DOI] [PubMed] [Google Scholar]
- 73.El-Bassel N, Witte SS, Wada T, Gilbert L, Wallace J. Correlates of Partner Violence Among Female Street-Based Sex Workers: Substance Abuse, History of Childhood Abuse, and HIV Risks. AIDS Patient Care STDs. 2001 Jan 1;15(1):41–51. doi: 10.1089/108729101460092. [DOI] [PubMed] [Google Scholar]
- 74.McLean I, Roberts SA, White C, Paul S. Female genital injuries resulting from consensual and non-consensual vaginal intercourse. Forensic Sci Int. 2011 Jan 30;204(1–3):27–33. doi: 10.1016/j.forsciint.2010.04.049. [DOI] [PubMed] [Google Scholar]
- 75.Zierler S, Krieger N. Reframing women's risk: social inequalities and HIV infection. Annu Rev Public Health. 1997;18(1):401–36. doi: 10.1146/annurev.publhealth.18.1.401. [DOI] [PubMed] [Google Scholar]
- 76.Garcia-Moreno C, Watts C. Violence against women: its importance for HIV/AIDS. AIDS Lond Engl. 1999;14:S253–65. [PubMed] [Google Scholar]
- 77.Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. The Lancet. 2004 May 1;363(9419):1415–21. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- 78.Niccolai LM, King EJ, Eritsyan KU, Safiullina L, Rusakova MM. “In different situations, in different ways”: male sex work in St. Petersburg, Russia. Cult Health Sex. 2013 Mar 7;15(4):480–93. doi: 10.1080/13691058.2013.766931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stephenson R, Finneran C. The IPV-GBM scale: a new scale to measure intimate partner violence among gay and bisexual men. [cited 2015 Nov 14];2013 doi: 10.1371/journal.pone.0062592. Available from: http://dx.plos.org/10.1371/journal.pone.0062592. [DOI] [PMC free article] [PubMed]
- 80.Straus MA, Hamby SL, BONEY-McCOY SUE, Sugarman DB. The Revised Conflict Tactics Scales (CTS2) Development and Preliminary Psychometric Data. J Fam Issues. 1996 May 1;17(3):283–316. [Google Scholar]
- 81.Ghanem A, Little SJ, Drumright L, Liu L, Morris S, Garfein RS. High-risk behaviors associated with injection drug use among recently HIV-infected men who have sex with men in San Diego, CA. AIDS Behav. 2011;15(7):1561–9. doi: 10.1007/s10461-011-9970-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bimbi DS, Palmadessa NA, Parsons JT. Substance use and domestic violence among urban gays, lesbians and bisexuals. J LGBT Health Res. 2008;3(2):1–7. doi: 10.1300/J463v03n02_01. [DOI] [PubMed] [Google Scholar]
- 83.Friedman MS, Marshal MP, Stall R, Cheong J, Wright ER. Gay-related development, early abuse and adult health outcomes among gay males. AIDS Behav. 2008;12(6):891–902. doi: 10.1007/s10461-007-9319-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rhodes SD, McCoy TP, Wilkin AM, Wolfson M. Behavioral risk disparities in a random sample of self-identifying gay and non-gay male university students. J Homosex. 2009;56(8):1083–100. doi: 10.1080/00918360903275500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hess KL, Javanbakht M, Brown JM, Weiss RE, Hsu P, Gorbach PM. Intimate Partner Violence and Anal Intercourse In Young Adult Heterosexual Relationships. Perspect Sex Reprod Health. 2013 Mar 1;45(1):6–12. doi: 10.1363/4500613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.