Summary
Background
Immunisation programmes have made substantial contributions to lowering the burden of disease in children, but there is a growing need to ensure that programmes are equity-oriented. We aimed to provide a detailed update about the state of between-country inequality and within-country economic-related inequality in the delivery of three doses of the combined diphtheria, tetanus toxoid, and pertussis-containing vaccine (DTP3), with a special focus on inequalities in high-priority countries.
Methods
We used data from the latest available Demographic and Health Surveys and Multiple Indicator Cluster Surveys done in 51 low-income and middle-income countries. Data for DTP3 coverage were disaggregated by wealth quintile, and inequality was calculated as difference and ratio measures based on coverage in richest (quintile 5) and poorest (quintile 1) household wealth quintiles. Excess change was calculated for 21 countries with data available at two timepoints spanning a 10 year period. Further analyses were done for six high-priority countries—ie, those with low national immunisation coverage and/or high absolute numbers of unvaccinated children. Significance was determined using 95% CIs.
Findings
National DTP3 immunisation coverage across the 51 study countries ranged from 32% in Central African Republic to 98% in Jordan. Within countries, the gap in DTP3 immunisation coverage suggested pro-rich inequality, with a difference of 20 percentage points or more between quintiles 1 and 5 for 20 of 51 countries. In Nigeria, Pakistan, Laos, Cameroon, and Central African Republic, the difference between quintiles 1 and 5 exceeded 40 percentage points. In 15 of 21 study countries, an increase over time in national coverage of DTP3 immunisation was realised alongside faster improvements in the poorest quintile than the richest. For example, in Burkina Faso, Cambodia, Gabon, Mali, and Nepal, the absolute increase in coverage was at least 2·0 percentage points per year, with faster improvement in the poorest quintile. Substantial economic-related inequality in DTP3 immunisation coverage was reported in five high-priority study countries (DR Congo, Ethiopia, Indonesia, Nigeria, and Pakistan), but not Uganda.
Interpretation
Overall, within-country inequalities in DTP3 immunisation persist, but seem to have narrowed over the past 10 years. Monitoring economic-related inequalities in immunisation coverage is warranted to reveal where gaps exist and inform appropriate approaches to reach disadvantaged populations.
Funding
None.
Introduction
Vaccines are a safe, effective, and cost-efficient health intervention that have substantially lowered the burden of disease in young children and averted many millions of deaths. The Expanded Programme on Immunization (EPI) was established by WHO in 1974, and since then the global health community has shown a serious commitment to realising the full potential of vaccines, with efforts dedicated to ensuring widespread vaccine distribution.1, 2, 3, 4 Gavi, the Vaccine Alliance—an organisation created in 2000—has been an important facilitator of improved access to more vaccines among children in poor countries.
Immunisation programmes have made strides in reaching populations at large.5 For example, in 2014, delivery of three doses of the combined diphtheria, tetanus toxoid, and pertussis-containing vaccine (DTP3) reached 86% worldwide.6 However, with about 18·7 million infants unvaccinated or undervaccinated,6 there is a growing need to ensure that disadvantaged populations are not left behind. Not only are poorer children more susceptible to infectious disease but also the tendency for geographical clustering of disadvantaged subgroups might result in an absence of herd immunity.7 In multicountry analyses, inequalities in child immunisation indicators have been reported, noting that richer subgroups within countries tend to have high coverage whereas the coverage level among poorer subgroups is variable across countries.8, 9 In some cases, disadvantaged populations have been reached successfully through equity-oriented immunisation programmes;10, 11 however, without an explicit focus on equity, disadvantaged populations generally report lower immunisation coverage,7, 12 sometimes even alongside improving national figures.13, 14
Research in context.
Evidence before this study
We searched PubMed on July 22, 2015, to identify publications in English only addressing inequalities in immunisation coverage, with the search terms “healthcare disparities”[Mesh] AND “immunization”[Mesh]. Our search yielded 97 results, dating back to 2007 (no filters were applied). We reviewed the titles and abstracts of these papers and selected ten relevant peer-reviewed publications for full-text review. We applied a snowball searching technique, drawing on the citations within these reports and other suggested similar papers, to identify further relevant studies. We also identified major global initiatives that promote immunisation and reviewed related documentation for the inclusion of equity-related considerations or reporting. These initiatives comprised: the Global Vaccine Action Plan; the Millennium Development Goals; the Decade of Vaccines; Global Immunization Vision and Strategy; and the Sustainable Development Goals. In the same manner, we reviewed publications of global organisations that report data about immunisation coverage in low-income and middle-income countries, including: WHO; Gavi, the Vaccine Alliance; UNICEF; the World Bank; Countdown to 2015; and Save the Children. We consulted with experts in the area of health inequality monitoring to identify other key academic or grey literature. The Global Vaccine Action Plan—endorsed by the 194 Member States of the World Health Assembly in 2012 and supported through the work of Gavi, the Vaccine Alliance and other organisations—promotes equitable access to vaccines for all people by the year 2020. The Plan highlights the need to promote within-country equity and requests the monitoring of coverage gaps between wealth quintiles (and other appropriate indicators). Specifically, strategic objective three in the Global Vaccine Action Plan seeks to ensure that the benefits of immunisation are extended equitably to all, with a call to build a knowledge base and capacity for enabling equitable delivery.
Added value of this study
We used the latest available household survey data gathered in 51 low-income and middle-income countries to provide an update about the global state of inequality in DTP3 immunisation coverage. Use of disaggregated data from Demographic and Health Surveys (DHS) and Multiple Indicator Cluster Surveys (MICS) enabled comparisons across countries and within countries over time. We presented the level of DTP3 immunisation coverage by wealth quintile in every country, thus extending conventional reporting of between-country inequality (ie, comparisons of national averages). Furthermore, we used data from two timepoints to quantify and compare how within-country inequality has changed over time (previous 10 years). Although many study countries had a narrowing of inequality over the past 10 years, substantial inequality persists within most study countries. We also noted variability in the state of inequality across study countries.
Implications of all the available evidence
The Sustainable Development Goals seek to reduce inequalities and ensure health and wellbeing for all, including a movement towards universal health coverage. In general, monitoring within-country inequalities in any health topic is important to ensure that the status of disadvantaged populations is not masked behind national averages; health inequality monitoring is fundamental to promoting the progressive realisation of universal health coverage. Knowledge about health inequalities helps to inform approaches to reach at-risk populations. Where warranted, inequalities should be addressed on a priority basis through equity-oriented and context-appropriate policies, programmes, and practices. Future studies can build on our results to further investigate underlying determinants of inequalities within countries.
An equity-oriented approach to increasing the reach of immunisation programmes should consider inequalities between countries and within countries and tailor programmes accordingly. The Global Vaccine Action Plan (GVAP)—endorsed by the 194 Member States of the World Health Assembly in 2012—promotes equitable access to vaccines for all people by the year 2020.2 GVAP specifies indicators that address within-country inequality, including a measure that compares the level of DTP3 coverage in the country's poorest wealth quintile with the level in the richest wealth quintile.2 National-level information has been used to identify priority countries and direct resource allocation (eg, through the work of Gavi, the Vaccine Alliance). High-priority countries—identified based on low national immunisation coverage and the absolute number of children who are unvaccinated—include DR Congo, Ethiopia, Indonesia, Nigeria, Pakistan, and Uganda.
The Sustainable Development Goals (SDGs) seek to reduce inequalities (goal 10) and ensure health and wellbeing for all (goal 3).1 Achieving universal coverage of immunisation programmes constitutes an important contribution to these goals and to the promotion of child survival and health at large. Measuring inequalities in DTP3 immunisation coverage between countries and within countries reveals where gaps exist in a routinely delivered vaccine and helps to inform appropriate approaches to reach at-risk populations. Assessing the extent to which gains in national coverage are driven by gains among poorer population subgroups is important for understanding whether within-country inequalities are reducing or widening. The objective of our study is to provide a detailed update about the state of between-country inequality and within-country economic-related inequality in childhood DTP3 immunisation in low-income and middle-income countries, with particular focus on inequalities in high-priority countries.
Methods
Data source
The disaggregated data, which are available through WHO Health Equity Monitor, are the product of reanalyses of publicly available microdata from the Demographic and Health Survey (DHS) and the Multiple Indicator Cluster Survey (MICS). DHS and MICS are large-scale, nationally representative household health surveys conducted through standardised face-to-face interviews with women aged 15–49 years.15 We assumed the design and implementation quality of both DHS and MICS were sufficiently similar to permit direct comparisons between surveys, both across countries and over time.8, 16, 17
We defined DTP3 immunisation coverage as the percentage of children aged 12–23 months who had received three doses of DTP3-containing vaccine at the time of the DHS or MICS. In some countries, indicator data reflect an alternative vaccination schedule of 15–26 months or 18–29 months, which is related to the child's age when the measles vaccine is offered.
We ascertained economic status based on a household wealth index,18 which accounts for ownership of specific household items and access to specific services. We constructed country-specific indices by principal component analysis, generating quintiles ranging from quintile 1 (poorest) to quintile 5 (richest).
Country selection
We selected countries for inclusion based on data availability and survey year (reflecting the initial year of data collection, if spanning multiple calendar years). We used data from the latest available DHS or MICS (conducted between 2010 and 2013) for analysis of latest status. To analyse change over time, we obtained data from surveys done about 10 years previously (between 2000 and 2003). From available survey data, we deemed countries with the highest number of unvaccinated children and/or lowest coverage estimates to be high-priority countries for further analysis. All available survey data (from at least two household surveys) were reported for high-priority countries.
Statistical analysis
Data for DTP3 coverage were disaggregated by wealth quintile. We calculated difference and ratio measures in each of the study countries to show the latest status of inequality, based on the level of coverage in quintiles 1 and 5. Difference is an expression of absolute inequality (quintile 5–quintile 1) whereas ratio expresses relative inequality (quintile 5/quintile 1).
We applied a measure of excess change to the countries with data from a previous DHS or MICS, expressing change in economic-related inequality over time. We calculated excess change as an annual absolute value, based on comparison of the pace of change in quintiles 1 and 5. First, for each quintile 1 and 5, we calculated the annual absolute pace of change as the difference between coverage in the latest survey and coverage in the survey done about 10 years earlier, divided by the number of years between the two surveys. Then, we subtracted the annual absolute pace of change in quintile 5 from the annual absolute pace of change in quintile 1, yielding annual excess change in percentage points. A positive excess change value reflects a pro-poor change: if coverage increased in both quintiles 1 and 5, then the growth in coverage occurred faster in quintile 1 than quintile 5. A negative excess change value reflects a pro-rich change, whereby the pace of change was more favourable in quintile 5. The interpretation of excess change values for all possible underlying scenarios has been detailed elsewhere.8
We ascertained statistical significance with 95% CIs. We took into account the survey sampling design for calculating point estimates of disaggregated data and their 95% CIs. We used Taylor series method to calculate SEs of the summary measures of inequality.
Role of the funding source
The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Data for 51 low-income and middle-income countries were included in latest status analyses (appendix). Of these, 21 countries had data available from surveys done about 10 years previously, and these countries were included in analyses of change over time. Moreover, six high-priority countries were identified for further analysis: DR Congo, Ethiopia, Indonesia, Nigeria, Pakistan, and Uganda.
DTP3 immunisation coverage varied widely between and within the 51 countries (table 1). National coverage ranged from as low as 32% in Central African Republic to nearly universal coverage in Jordan (98%). A third of countries had national DTP3 coverage of 90% or higher. However, in Central African Republic, Ethiopia, Guinea, and Nigeria, at least half the child population was not covered by DTP3 immunisation.
Table 1.
Latest situation in DTP3 immunisation coverage among children aged 12–23 months in 51 low-income and middle-income countries
| National average (95% CI) | Quintile 1 (95% CI) | Quintile 2 (95% CI) | Quintile 3 (95% CI) | Quintile 4 (95% CI) | Quintile 5 (95% CI) | Difference (percentage points; 95% CI)* | Ratio (95% CI)† | |
|---|---|---|---|---|---|---|---|---|
| Armenia | 95·0% (90·4–97·4) | 88·3% (68·0–96·4) | 99·1% (93·4–99·9) | 94·2% (81·3–98·4) | 96·1% (86·0–99·0) | 96·9% (89·3–99·2) | 8·6 (−5·0 to 22·3) | 1·10 (0·94–1·28) |
| Bangladesh | 93·4% (91·5–95·0) | 90·3% (85·9–93·5) | 90·1% (84·9–93·6) | 93·2% (89·3–95·8) | 96·3% (93·1–98·0) | 97·8% (94·9–99·1) | 7·5 (3·3 to 11·7) | 1·08 (1·03–1·13) |
| Belize | 71·4% (66·5–75·8) | 71·7% (62·4–79·5) | 71·3% (61·2–79·7) | 70·3% (56·7–81·0) | 75·0% (61·5–85·0) | 68·9% (56·1–79·3) | −2·8 (−17·4 to 11·7) | 0·96 (0·78–1·18) |
| Benin | 73·9% (71·4–76·3) | 59·0% (53·4–64·5) | 67·9% (63·0–72·4) | 76·5% (72·1–80·5) | 80·2% (76·0–83·8) | 85·6% (80·4–89·7) | 26·6 (19·4 to 33·8) | 1·45 (1·30–1·62) |
| Bosnia and Herzegovina | 92·2% (89·4–94·3) | 91·4% (84·0–95·6) | 90·4% (82·7–94·9) | 91·7% (83·7–96·0) | 93·4% (86·2–96·9) | 93·8% (87·1–97·1) | 2·3 (−4·9 to 9·6) | 1·03 (0·95–1·11) |
| Burkina Faso | 89·5% (87·6–91·2) | 83·4% (78·7–87·2) | 87·9% (84·1–90·8) | 91·6% (88·9–93·7) | 92·5% (89·5–94·7) | 92·9% (87·8–95·9) | 9·5 (3·7 to 15·2) | 1·11 (1·04–1·19) |
| Burundi | 95·7% (94·3–96·8) | 94·4% (90·9–96·6) | 96·1% (92·7–98·0) | 96·9% (92·0–98·8) | 96·9% (93·9–98·5) | 94·2% (90·8–96·4) | −0·2 (−4·1 to 3·7) | 1·00 (0·96–1·04) |
| Cambodia | 84·8% (82·3–87·0) | 73·5% (67·8–78·4) | 82·9% (77·2–87·4) | 88·6% (83·8–92·1) | 90·7% (85·6–94·2) | 92·6% (88·4–95·3) | 19·1 (12·8 to 25·4) | 1·26 (1·16–1·37) |
| Cameroon | 68·8% (65·2–72·2) | 44·6% (37·3–52·1) | 66·3% (59·4–72·7) | 74·0% (68·0–79·3) | 77·9% (73·1–82·0) | 87·6% (83·5–90·8) | 43·0 (34·7 to 51·2) | 1·96 (1·65–2·33) |
| Central African Republic | 32·1% (28·5–36·0) | 17·8% (13·9–22·6) | 21·0% (17·0–25·7) | 28·0% (23·4–33·0) | 45·2% (38·6–52·0) | 59·6% (50·9–67·7) | 41·7 (32·2 to 51·3) | 3·34 (2·52–4·43) |
| Colombia | 90·5% (89·2–91·7) | 84·9% (81·8–87·6) | 92·0% (89·3–94·1) | 93·4% (90·7–95·3) | 91·8% (88·1–94·5) | 92·5% (87·6–95·5) | 7·6 (2·8 to 12·3) | 1·09 (1·03–1·15) |
| Comoros | 73·1% (67·9–77·7) | 57·5% (46·8–67·6) | 66·3% (55·5–75·6) | 80·5% (72·2–86·8) | 82·5% (71·4–89·9) | 83·5% (72·8–90·5) | 26·0 (12·3 to 39·7) | 1·45 (1·18–1·79) |
| Congo | 69·1% (64·9–73·1) | 54·6% (49·7–59·4) | 61·9% (52·4–70·7) | 73·4% (64·6–80·7) | 81·1% (72·5–87·4) | 81·6% (72·9–88·0) | 27·0 (18·1 to 36·0) | 1·50 (1·32–1·70) |
| Costa Rica | 94·2% (88·1–97·3) | 89·3% (69·2–96·9) | 97·0% (90·2–99·1) | 95·2% (80·4–99·0) | 95·5% (77·7–99·2) | 97·2% (86·9–99·4) | 7·8 (−5·5 to 21·1) | 1·09 (0·94–1·26) |
| Côte d'Ivoire | 63·8% (59·4–68·0) | 52·1% (44·3–59·8) | 60·4% (53·1–67·3) | 58·1% (49·7–66·1) | 73·9% (66·2–80·4) | 80·7% (72·4–86·9) | 28·6 (17·9 to 39·2) | 1·55 (1·30–1·84) |
| DR Congo | 60·6% (56·9–64·2) | 48·1% (42·1–54·2) | 51·0% (45·4–56·6) | 56·5% (50·5–62·3) | 69·8% (63·6–75·4) | 83·0% (77·2–87·5) | 34·9 (26·9 to 42·8) | 1·72 (1·50–1·98) |
| Ethiopia | 37·0% (33·0–41·3) | 26·0% (20·0–33·2) | 29·4% (23·0–36·7) | 31·4% (24·1–39·8) | 42·8% (35·2–50·8) | 63·6% (54·5–71·8) | 37·5 (26·6 to 48·5) | 2·44 (1·83–3·26) |
| Gabon | 72·9% (68·5–76·8) | 62·2% (55·6–68·3) | 78·1% (70·8–84·0) | 67·7% (57·1–76·7) | 88·1% (78·7–93·6) | 71·8% (55·1–84·1) | 9·7 (−6·4 to 25·7) | 1·16 (0·92–1·45) |
| Ghana | 92·9% (90·8–94·6) | 93·0% (88·5–95·8) | 93·2% (88·6–96·0) | 90·1% (83·7–94·2) | 94·0% (87·3–97·3) | 94·4% (87·0–97·7) | 1·4 (−4·6 to 7·5) | 1·02 (0·95–1·08) |
| Guinea | 50·0% (45·5–54·5) | 32·4% (26·1–39·3) | 53·2% (43·4–62·8) | 51·6% (43·6–59·6) | 54·5% (47·0–61·8) | 63·0% (54·0–71·3) | 30·7 (19·7 to 41·6) | 1·95 (1·52–2·49) |
| Haiti | 62·8% (58·8–66·6) | 54·7% (45·5–63·6) | 63·3% (55·5–70·4) | 67·0% (59·8–73·4) | 62·9% (54·7–70·5) | 67·9% (57·3–77·0) | 13·2 (−0·2 to 26·7) | 1·24 (1·00–1·55) |
| Honduras | 95·6% (94·4–96·6) | 96·4% (94·3–97·7) | 94·9% (91·7–96·9) | 93·7% (90·3–95·9) | 95·7% (91·9–97·7) | 98·1% (94·8–99·3) | 1·7 (−0·9 to 4·3) | 1·02 (0·99–1·04) |
| Indonesia | 72·2% (69·8–74·5) | 52·5% (47·8–57·2) | 69·1% (64·1–73·7) | 75·0% (70·0–79·3) | 81·0% (76·1–85·2) | 85·1% (80·8–88·6) | 32·6 (26·5 to 38·7) | 1·62 (1·47–1·79) |
| Iraq | 70·1% (68·3–71·9) | 55·2% (51·7–58·6) | 67·8% (64·3–71·1) | 72·6% (68·9–76·0) | 79·6% (76·1–82·8) | 82·3% (77·6–86·1) | 27·1 (21·6 to 32·6) | 1·49 (1·38–1·62) |
| Jordan | 98·4% (97·6–99·0) | 96·2% (93·3–97·9) | 99·1% (98·1–99·6) | 99·2% (97·9–99·7) | 99·3% (98·3–99·7) | 99·1% (94·4–99·9) | 2·8 (0·1 to 5·6) | 1·03 (1·00–1·06) |
| Kazakhstan | 96·8% (95·1–97·9) | 97·1% (93·3–98·8) | 98·9% (95·6–99·7) | 97·0% (92·7–98·8) | 94·4% (89·2–97·2) | 95·2% (90·3–97·7) | −2·0 (−6·2 to 2·3) | 0·98 (0·94–1·02) |
| Kyrgyzstan | 87·4% (84·0–90·2) | 94·3% (89·3–97·0) | 95·4% (90·1–97·9) | 90·8% (84·2–94·8) | 82·1% (74·5–87·8) | 75·0% (64·9–83·0) | −19·3 (−29·1 to −9·5) | 0·80 (0·70–0·90) |
| Laos | 55·5% (52·1–58·8) | 36·8% (31·3–42·6) | 46·6% (40·7–52·6) | 59·4% (53·7–64·9) | 67·6% (61·2–73·4) | 81·4% (75·2–86·3) | 44·6 (36·7 to 52·6) | 2·21 (1·87–2·62) |
| Liberia | 71·5% (67·4–75·3) | 58·0% (51·2–64·5) | 72·1% (66·1–77·3) | 73·6% (65·1–80·6) | 78·3% (68·6–85·6) | 79·4% (69·3–86·8) | 21·4 (10·4 to 32·4) | 1·37 (1·17–1·60) |
| Macedonia | 95·2% (90·7–97·5) | 92·7% (79·1–97·7) | 98·9% (92·7–99·8) | 96·2% (86·2–99·1) | 93·7% (73·2–98·8) | 94·0% (78·8–98·5) | 1·2 (−10·3 to 12·7) | 1·01 (0·90–1·15) |
| Malawi | 93·2% (91·8–94·4) | 91·4% (88·7–93·6) | 93·7% (91·4–95·4) | 92·2% (88·4–94·8) | 94·8% (92·0–96·7) | 94·3% (90·9–96·5) | 2·9 (−0·7 to 6·5) | 1·03 (0·99–1·07) |
| Mali | 63·7% (60·3–66·9) | 48·6% (41·0–56·2) | 58·4% (52·4–64·2) | 61·4% (55·2–67·3) | 72·6% (67·4–77·3) | 77·6% (72·6–81·8) | 29·0 (20·1 to 37·9) | 1·60 (1·35–1·89) |
| Mongolia | 92·7% (90·4–94·5) | 91·2% (86·9–94·1) | 92·5% (87·5–95·6) | 92·7% (86·6–96·1) | 91·6% (84·1–95·7) | 96·1% (90·6–98·5) | 4·9 (0·0 to 9·9) | 1·05 (1·00–1·11) |
| Mozambique | 76·9% (73·8–79·8) | 65·4% (58·2–71·9) | 70·8% (65·4–75·6) | 81·0% (75·8–85·3) | 86·0% (81·5–89·5) | 87·5% (83·5–90·7) | 22·2 (14·4 to 29·9) | 1·34 (1·20–1·50) |
| Nepal | 91·8% (88·5–94·3) | 88·1% (81·7–92·5) | 89·7% (81·6–94·5) | 90·5% (82·4–95·0) | 96·7% (91·8–98·8) | 98·4% (94·9–99·5) | 10·3 (4·7 to 15·9) | 1·12 (1·05–1·19) |
| Niger | 68·5% (64·9–71·9) | 53·3% (46·7–59·7) | 65·0% (57·6–71·7) | 68·2% (61·8–74·0) | 70·5% (63·0–77·0) | 84·4% (80·2–87·8) | 31·1 (23·5 to 38·6) | 1·58 (1·39–1·80) |
| Nigeria | 38·5% (35·5–41·6) | 7·4% (5·6–9·6) | 18·9% (15·9–22·3) | 40·1% (36·0–44·3) | 60·1% (55·5–64·5) | 79·6% (76·1–82·7) | 72·3 (68·4 to 76·1) | 10·82 (8·21–14·25) |
| Pakistan | 65·3% (60·5–69·8) | 29·9% (21·6–39·7) | 67·5% (60·1–74·2) | 69·2% (61·7–75·9) | 78·9% (73·5–83·4) | 88·0% (83·6–91·3) | 58·1 (48·2 to 68·0) | 2·95 (2·17–4·01) |
| Peru | 83·7% (81·4–85·8) | 83·4% (79·4–86·8) | 82·5% (77·9–86·3) | 85·1% (79·7–89·2) | 80·3% (73·5–85·7) | 88·6% (80·2–93·7) | 5·1 (−2·4 to 12·6) | 1·06 (0·97–1·16) |
| Philippines | 86·2% (84·1–88·1) | 78·5% (73·7–82·7) | 83·7% (78·9–87·6) | 89·1% (84·7–92·3) | 91·6% (87·1–94·7) | 93·0% (87·8–96·1) | 14·5 (8·5 to 20·5) | 1·18 (1·10–1·27) |
| Rwanda | 96·9% (95·8–97·8) | 96·1% (93·3–97·8) | 95·7% (92·7–97·4) | 97·1% (94·3–98·5) | 97·9% (95·5–99·0) | 98·7% (96·8–99·5) | 2·6 (0·1 to 5·0) | 1·03 (1·00–1·05) |
| Senegal | 88·8% (86·2–90·9) | 80·2% (73·3–85·6) | 88·0% (83·4–91·4) | 93·1% (88·5–95·9) | 91·2% (84·3–95·2) | 94·6% (87·2–97·8) | 14·4 (6·6 to 22·2) | 1·18 (1·08–1·29) |
| Sierra Leone | 78·5% (75·4–81·2) | 79·4% (74·0–84·0) | 77·6% (71·7–82·5) | 79·7% (74·7–83·9) | 81·6% (76·2–86·0) | 72·3% (64·0–79·4) | −7·1 (−16·3 to 2·1) | 0·91 (0·80–1·03) |
| Suriname | 55·4% (50·0–60·7) | 64·0% (56·5–70·9) | 50·7% (40·1–61·3) | 56·3% (45·4–66·5) | 51·0% (38·5–63·4) | 45·9% (31·8–60·6) | −18·1 (−34·6 to −1·7) | 0·72 (0·51–0·99) |
| Swaziland | 90·6% (87·4–93·1) | 89·7% (82·2–94·3) | 91·7% (82·6–96·2) | 94·0% (87·0–97·3) | 92·1% (83·6–96·4) | 83·6% (73·3–90·4) | −6·1 (−16·4 to 4·2) | 0·93 (0·83–1·05) |
| Tajikistan | 93·2% (90·8–95·0) | 92·9% (84·2–97·0) | 95·6% (91·3–97·8) | 93·3% (88·7–96·2) | 91·9% (85·7–95·6) | 91·6% (86·8–94·7) | −1·3 (−8·4 to 5·8) | 0·99 (0·91–1·06) |
| Tanzania | 88·0% (84·9–90·6) | 84·1% (77·4–89·0) | 84·1% (77·4–89·0) | 87·3% (81·9–91·2) | 91·3% (84·4–95·3) | 96·9% (93·2–98·6) | 12·9 (6·6 to 19·1) | 1·15 (1·07–1·24) |
| Togo | 72·4% (68·4–76·0) | 62·8% (54·9–70·1) | 75·2% (67·8–81·3) | 70·6% (61·6–78·2) | 73·8% (64·3–81·5) | 84·4% (74·8–90·8) | 21·6 (10·6 to 32·6) | 1·34 (1·15–1·57) |
| Uganda | 72·2% (68·8–75·4) | 74·5% (67·6–80·4) | 72·6% (65·7–78·5) | 67·2% (60·2–73·4) | 71·3% (62·9–78·5) | 74·8% (67·1–81·3) | 0·3 (−9·3 to 9·9) | 1·00 (0·88–1·14) |
| Vietnam | 73·9% (69·8–77·7) | 59·3% (49·3–68·6) | 71·7% (61·1–80·3) | 74·1% (64·2–82·1) | 78·1% (68·8–85·1) | 85·5% (78·1–90·8) | 26·2 (14·6 to 37·9) | 1·44 (1·20–1·73) |
| Zimbabwe | 73·6% (69·3–77·4) | 67·4% (59·1–74·7) | 71·2% (62·5–78·6) | 71·2% (62·9–78·4) | 78·8% (72·0–84·3) | 80·9% (73·5–86·7) | 13·5 (3·3 to 23·8) | 1·20 (1·04–1·38) |
| Median | 76·9% | 73·5% | 77·6% | 80·5% | 82·1% | 85·6% | 12·9 | 1·16 |
Data taken from DHS and MICS 2010–13. DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine. MICS=Multiple Indicator Cluster Survey.
Calculated by subtracting the level of coverage in quintile 1 from the level of coverage in quintile 5.
Calculated by dividing the level of coverage in quintile 5 by the level of coverage in quintile 1.
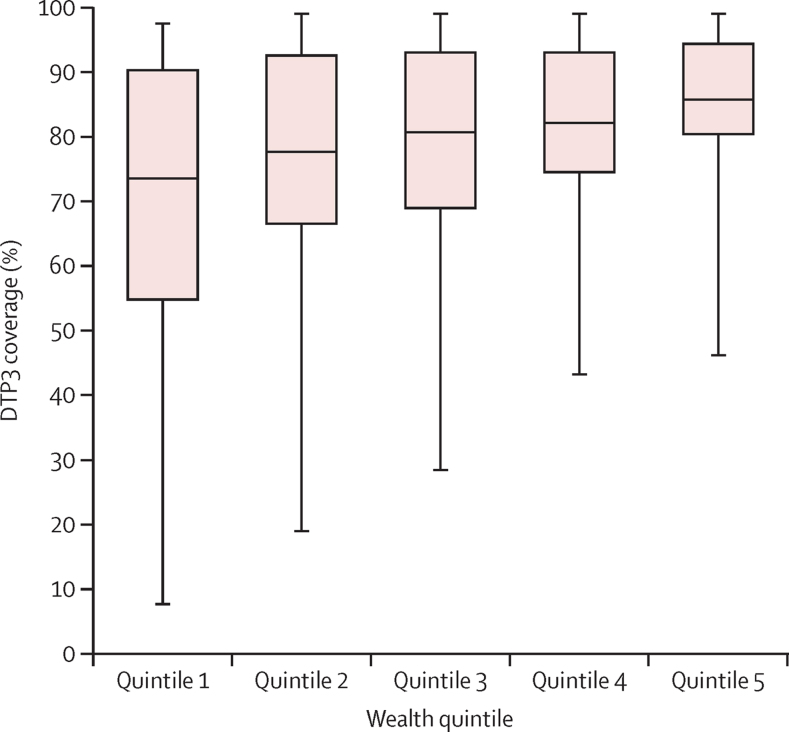
Overall, DTP3 immunisation coverage tended to be lowest in children from poorer households, and increased with rising economic status, indicating pro-rich inequality. Median DTP3 coverage was 74% among children in quintile 1 compared with 86% in quintile 5 (figure 1). On the whole, study countries reported a wider range of coverage values in quintile 1 than quintile 5.
Figure 1.
Latest situation of DTP3 coverage among children aged 12–23 months in 51 low-income and middle-income countries, by economic status
Data taken from DHS and MICS 2010–13. Box and whisker plots show the distribution of DTP3 coverage within wealth quintiles of 51 low-income and middle-income countries. Whiskers represent maximum and minimum values; the centre line denotes the median value; and the shaded box indicates the IQR (middle 50% of country estimates). DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine. MICS=Multiple Indicator Cluster Survey.
In 20 countries, pro-rich inequality was substantial, with a gap in DTP3 immunisation coverage of 20 percentage points or more between quintiles 1 and 5 (table 1). In Nigeria, Pakistan, Laos, Cameroon, and Central African Republic, the level of absolute inequality was very high, with a difference exceeding 40 percentage points. Several countries (Nigeria, Central African Republic, Pakistan, Ethiopia, and Laos) indicated high relative inequality, with DTP3 immunisation coverage at least twice as high in quintile 5 than in quintile 1. Kyrgyzstan and Suriname showed pro-poor inequality whereby, in absolute terms, coverage was significantly higher in quintile 1 than in quintile 5. In 18 countries, the absolute difference in DTP3 immunisation coverage between richest and poorest quintiles did not reach significance.
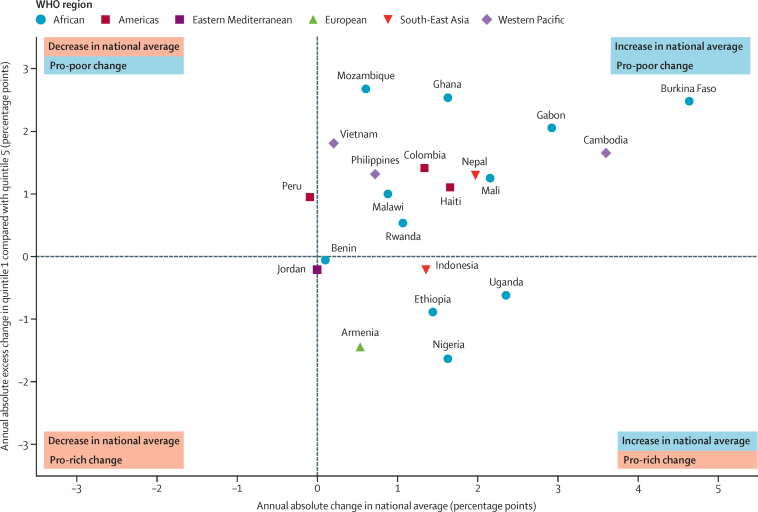
In 15 of 21 countries, national DTP3 immunisation coverage rose significantly over time, and a further two countries had growth of borderline significance. In Burkina Faso, Cambodia, Gabon, Uganda, Mali, and Nepal, the absolute increase in coverage was at least 2·0 percentage points per year (table 2). In most countries, an escalation in national coverage was achieved alongside faster improvement in quintile 1 compared with quintile 5 (figure 2). Pro-poor excess change was significant in 11 countries. In Mozambique, Ghana, Burkina Faso, and Gabon, the DTP3 coverage increase in the poorest quintile outpaced that in the richest quintile by at least 2·0 percentage points per year (table 2). Nigeria was the only study country with a significant pro-rich excess change, with the improvement in quintile 5 exceeding that in quintile 1.
Table 2.
Change over time in DTP3 immunisation coverage among children aged 12–23 months in 21 low-income and middle-income countries
|
National average |
Quintile 1 |
Quintile 5 |
Absolute annual excess change (percentage points) (95% CI)† | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Coverage in year 1 (95% CI) | Coverage in year 2 (95% CI) | Absolute annual change (percentage points) (95% CI)* | Coverage in year 1 (95% CI) | Coverage in year 2 (95% CI) | Absolute annual change (percentage points) (95% CI)* | Coverage in year 1 (95% CI) | Coverage in year 2 (95% CI) | Absolute annual change (percentage points) (95% CI)* | ||
| Armenia | 89·7% (85·4 to 92·8) | 95·0% (90·4 to 97·4) | 0·5 (0·0 to 1·0) | 89·3% (80·9 to 94·2) | 88·3% (68·0 to 96·4) | −0·1 (−1·6 to 1·4) | 83·5% (69·6 to 91·8) | 96·9% (89·3 to 99·2) | 1·3 (0·2 to 2·5) | −1·4 (−3·3 to 0·4) |
| Benin | 72·9% (69·0 to 76·5) | 73·9% (71·4 to 76·3) | 0·1 (−0·3 to 0·6) | 63·5% (55·7 to 70·6) | 59·0% (53·4 to 64·5) | −0·4 (−1·4 to 0·5) | 89·5% (82·4 to 93·9) | 85·6% (80·4 to 89·7) | −0·4 (−1·1 to 0·3) | −0·1 (−1·2 to 1·1) |
| Burkina Faso | 57·1% (52·3 to 61·7) | 89·5% (87·6 to 91·2) | 4·6 (3·9 to 5·4) | 45·7% (38·6 to 53·0) | 83·4% (78·7 to 87·2) | 5·4 (4·2 to 6·6) | 72·5% (65·7 to 78·4) | 92·9% (87·8 to 95·9) | 2·9 (1·8 to 4·0) | 2·5 (0·9 to 4·1) |
| Cambodia | 48·8% (44·8 to 52·8) | 84·8% (82·3 to 87·0) | 3·6 (3·1 to 4·1) | 39·0% (32·5 to 45·8) | 73·5% (67·8 to 78·4) | 3·4 (2·6 to 4·3) | 74·7% (65·3 to 82·3) | 92·6% (88·4 to 95·3) | 1·8 (0·9 to 2·7) | 1·7 (0·4 to 2·9) |
| Colombia | 77·2% (73·8 to 80·2) | 90·5% (89·2 to 91·7) | 1·3 (1·0 to 1·7) | 64·2% (56·9 to 70·8) | 84·9% (81·8 to 87·6) | 2·1 (1·3 to 2·8) | 86·0% (79·0 to 90·9) | 92·5% (87·6 to 95·5) | 0·7 (0·0 to 1·4) | 1·4 (0·4 to 2·5) |
| Ethiopia | 21·1% (18·2 to 24·5) | 37·0% (33·0 to 41·3) | 1·4 (1·0 to 1·9) | 15·3% (11·4 to 20·2) | 26·0% (20·0 to 33·2) | 1·0 (0·3 to 1·7) | 43·1% (33·5 to 53·1) | 63·6% (54·5 to 71·8) | 1·9 (0·7 to 3·1) | −0·9 (−2·3 to 0·5) |
| Gabon | 37·7% (33·6 to 42·0) | 72·9% (68·5 to 76·8) | 2·9 (2·4 to 3·4) | 18·9% (14·5 to 24·4) | 62·2% (55·6 to 68·3) | 3·6 (2·9 to 4·3) | 53·2% (42·1 to 64·1) | 71·8% (55·1 to 84·1) | 1·6 (0·0 to 3·1) | 2·1 (0·4 to 3·7) |
| Ghana | 79·8% (76·0 to 83·1) | 92·9% (90·8 to 94·6) | 1·6 (1·1 to 2·1) | 65·7% (56·6 to 73·7) | 93·0% (88·5 to 95·8) | 3·4 (2·2 to 4·6) | 87·4% (78·9 to 92·8) | 94·4% (87·0 to 97·7) | 0·9 (−0·2 to 1·9) | 2·5 (1·0 to 4·1) |
| Haiti | 42·9% (36·9 to 49·1) | 62·8% (58·8 to 66·6) | 1·7 (1·1 to 2·3) | 31·1% (23·5 to 39·8) | 54·7% (45·5 to 63·6) | 2·0 (0·9 to 3·0) | 57·6% (35·1 to 77·3) | 67·9% (57·3 to 77·0) | 0·9 (−1·2 to 2·9) | 1·1 (−1·2 to 3·4) |
| Indonesia | 58·6% (55·0 to 62·1) | 72·2% (69·8 to 74·5) | 1·4 (0·9 to 1·8) | 41·9% (35·9 to 48·1) | 52·5% (47·8 to 57·2) | 1·1 (0·3 to 1·8) | 72·3% (64·1 to 79·2) | 85·1% (80·8 to 88·6) | 1·3 (0·4 to 2·1) | −0·2 (−1·4 to 0·9) |
| Jordan | 98·3% (97·2 to 98·9) | 98·4% (97·6 to 99·0) | 0·0 (−0·1 to 0·1) | 98·3% (96·7 to 99·2) | 96·2% (93·3 to 97·9) | −0·2 (−0·5 to 0·0) | 99·5% (96·7 to 99·9) | 99·1% (94·4 to 99·9) | 0·0 (−0·2 to 0·1) | −0·2 (−0·5 to 0·1) |
| Malawi | 84·3% (81·9 to 86·5) | 93·2% (91·8 to 94·4) | 0·9 (0·6 to 1·1) | 77·8% (72·7 to 82·2) | 91·4% (88·7 to 93·6) | 1·4 (0·8 to 1·9) | 90·6% (86·7 to 93·5) | 94·3% (90·9 to 96·5) | 0·4 (−0·1 to 0·8) | 1·0 (0·3 to 1·7) |
| Mali | 39·9% (35·8 to 44·1) | 63·7% (60·3 to 66·9) | 2·2 (1·7 to 2·7) | 28·1% (22·1 to 34·9) | 48·6% (41·0 to 56·2) | 1·9 (1·0 to 2·8) | 70·8% (63·7 to 77·0) | 77·6% (72·6 to 81·8) | 0·6 (−0·1 to 1·4) | 1·3 (0·1 to 2·4) |
| Mozambique | 72·1% (68·3 to 75·6) | 76·9% (73·8 to 79·8) | 0·6 (0·0 to 1·2) | 52·6% (45·7 to 59·4) | 65·4% (58·2 to 71·9) | 1·6 (0·4 to 2·8) | 96·0% (90·4 to 98·4) | 87·5% (83·5 to 90·7) | −1·1 (−1·7 to −0·4) | 2·7 (1·3 to 4·0) |
| Nepal | 72·1% (66·8 to 76·9) | 91·8% (88·5 to 94·3) | 2·0 (1·4 to 2·5) | 62·1% (53·0 to 70·3) | 88·1% (81·7 to 92·5) | 2·6 (1·6 to 3·6) | 85·4% (77·4 to 90·9) | 98·4% (94·9 to 99·5) | 1·3 (0·6 to 2·0) | 1·3 (0·1 to 2·5) |
| Nigeria | 22·2% (17·8 to 27·3) | 38·5% (35·5 to 41·6) | 1·6 (1·1 to 2·2) | 7·1% (4·0 to 12·1) | 7·4% (5·6 to 9·6) | 0·0 (−0·4 to 0·5) | 63·0% (52·8 to 72·2) | 79·6% (76·1 to 82·7) | 1·7 (0·6 to 2·7) | −1·6 (−2·8 to −0·5) |
| Peru | 84·8% (82·9 to 86·5) | 83·7% (81·4 to 85·8) | −0·1 (−0·3 to 0·1) | 76·4% (72·4 to 79·9) | 83·4% (79·4 to 86·8) | 0·6 (0·2 to 1·0) | 93·0% (87·6 to 96·1) | 88·6% (80·2 to 93·7) | −0·4 (−1·0 to 0·3) | 1·0 (0·2 to 1·7) |
| Philippines | 79·0% (76·5 to 81·4) | 86·2% (84·1 to 88·1) | 0·7 (0·4 to 1·0) | 64·3% (58·8 to 69·4) | 78·5% (73·7 to 82·7) | 1·4 (0·7 to 2·1) | 92·0% (86·1 to 95·6) | 93·0% (87·8 to 96·1) | 0·1 (−0·5 to 0·7) | 1·3 (0·4 to 2·2) |
| Rwanda | 86·2% (83·7 to 88·4) | 96·9% (95·8 to 97·8) | 1·1 (0·8 to 1·3) | 81·1% (74·3 to 86·5) | 96·1% (93·3 to 97·8) | 1·5 (0·9 to 2·1) | 89·0% (84·3 to 92·4) | 98·7% (96·8 to 99·5) | 1·0 (0·6 to 1·4) | 0·5 (−0·2 to 1·3) |
| Uganda | 46·2% (42·1 to 50·4) | 72·2% (68·8 to 75·4) | 2·4 (1·9 to 2·8) | 47·5% (38·3 to 56·9) | 74·5% (67·6 to 80·4) | 2·5 (1·4 to 3·5) | 40·9% (34·4 to 47·8) | 74·8% (67·1 to 81·3) | 3·1 (2·2 to 4·0) | −0·6 (−2·0 to 0·7) |
| Vietnam | 72·4% (66·0 to 77·9) | 73·9% (69·8 to 77·7) | 0·2 (−0·7 to 1·1) | 52·8% (41·7 to 63·6) | 59·3% (49·3 to 68·6) | 0·8 (−1·0 to 2·7) | 93·5% (87·0 to 96·9) | 85·5% (78·1 to 90·8) | −1·0 (−2·0 to 0·0) | 1·8 (−0·3 to 3·9) |
| Median | 72·1% | 83·7% | 1·4 | 52·8% | 74·5% | 1·5 | 85·4% | 88·6% | 0·9 | 1·1 |
Data taken from DHS and MICS 2000–03 and 2010–13. DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine. MICS=Multiple Indicator Cluster Survey.
Calculated by subtracting coverage in year 1 from coverage in year 2, and dividing by the number of intervening years.
Calculated by subtracting the annual absolute change in quintile 5 from the annual absolute change in quintile 1.
Figure 2.
Change over time in national average of DTP3 coverage among children aged 12–23 months, and in quintile 1 compared with quintile 5, in 21 low-income and middle-income countries
Data taken from DHS and MICS 2000–03 and 2010–13. Every country is represented by a shape, which corresponds to its WHO region. For every study country, the annual absolute change in national average was calculated by subtracting the national coverage in survey year 1 (2000–03) from coverage in survey year 2 (2010–13) and dividing by the number of intervening years. The annual absolute excess change was calculated by subtracting the annual absolute change in quintile 5 from the annual absolute change in quintile 1. Red and blue boxes portray undesirable and desirable scenarios, respectively. DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine. MICS=Multiple Indicator Cluster Survey.
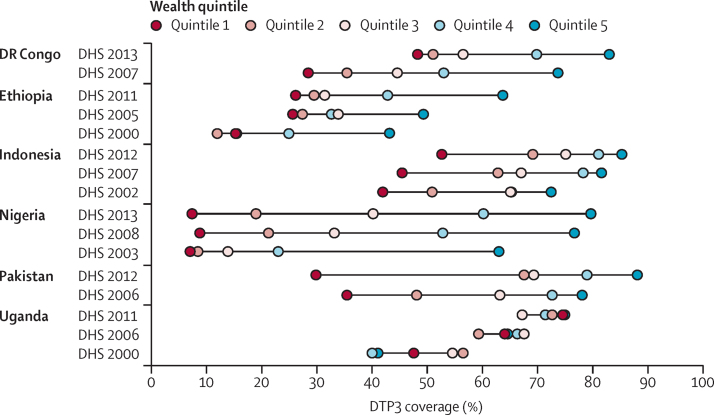
Substantial economic-related inequality in DTP3 immunisation coverage was noted in all high-priority countries, except Uganda (figure 3). In DR Congo, an increase in coverage between DHS 2007 and DHS 2013 was seen in all quintiles, with remarkable growth in poorer quintiles. Although inequality narrowed in DHS 2013, the gap in coverage was still large (about 35 percentage points). In Ethiopia, economic-related inequality persisted between DHS 2000 and DHS 2011, despite overall gains in DTP3 coverage in all quintiles. In DHS 2005, large improvements were noted in poorer quintiles alongside some improvement in richer quintiles, whereas substantial gains in richer quintiles were evident in DHS 2011, and poorer quintiles showed no improvement. In Indonesia, DHS 2012 indicated a significant pro-rich absolute difference in DTP3 immunisation coverage (32·6 percentage points, 95% CI 26·5–38·7). Although national coverage grew over the period 2002–12, improvements were achieved at a similar pace in quintiles 1 and 5 and, thus, the gap between these quintiles persisted. Faster improvements, however, were noted in intermediate quintiles (notably, quintile 2). In Nigeria, DHS 2003 showed a large gap in coverage between quintile 5 and all other quintiles—eg, the difference between quintiles 5 and 4 was 40 percentage points, and the difference between quintiles 5 and 1 was 56 percentage points. DHS 2008 and DHS 2013 indicated faster improvements in quintiles 3, 4, and 5 than in quintiles 1 and 2; as a result, inequality between quintiles 5 and 4 halved (to 20 percentage points in DHS 2013), but inequality between quintiles 5 and 1 increased (to 72 percentage points in DHS 2013). The level of coverage in quintile 1 remained under 10% at all timepoints. In Pakistan, substantial inequality was reported in immunisation coverage in DHS 2006, with a difference of more than 40 percentage points between quintiles 1 and 5. In DHS 2012, all but the poorest quintile had improved coverage, with a notable increase of 20 percentage points in quintile 2. Coverage in quintile 1 decreased, resulting in a widening gap between quintile 1 and the rest of the population; the coverage gap between quintiles 1 and 2 grew by three times between DHS 2006 (12·6 percentage points) and DHS 2012 (37·6 percentage points). Finally, in Uganda, economic-related inequality presented an uncommon pattern; the richest 40% (quintiles 4 and 5) had the lowest DTP3 coverage in 2000, and the poorest (quintile 1) had intermediate coverage. The overall situation improved over time, although we still do not see the usual increasing pattern of coverage from poorest to richest. In any case, wealth-related inequality in Uganda has decreased over time. In DHS 2011, DTP3 coverage was around 75% in both quintile 1 and quintile 5.
Figure 3.
Change over time in DTP3 coverage among children aged 12–23 months in six high-priority countries, by economic status
Data taken from DHS 2000–13. For each country, disaggregated data are presented for wealth quintiles by coloured dots; the horizontal lines indicate the difference between the most extreme quintile values. DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine.
Discussion
In our study of household health surveys, inequality in DTP3 immunisation coverage was noted both between and within countries. The extent of within-country inequality varied by country: most countries (but not all) showed substantial pro-rich inequality. In most countries, improved national coverage over the past 10 years was driven by accelerated improvements in poorer quintiles. The criterion of the GVAP indicator relates to within-country inequality—ie, that DTP3 coverage in quintile 1 is not more than 20 percentage points below coverage in quintile 5. This indicator was not met by 20 of 51 study countries. Moreover, five of six high-priority countries had a DTP3 immunisation coverage gap of greater than 20 percentage points between the poorest and richest quintiles.
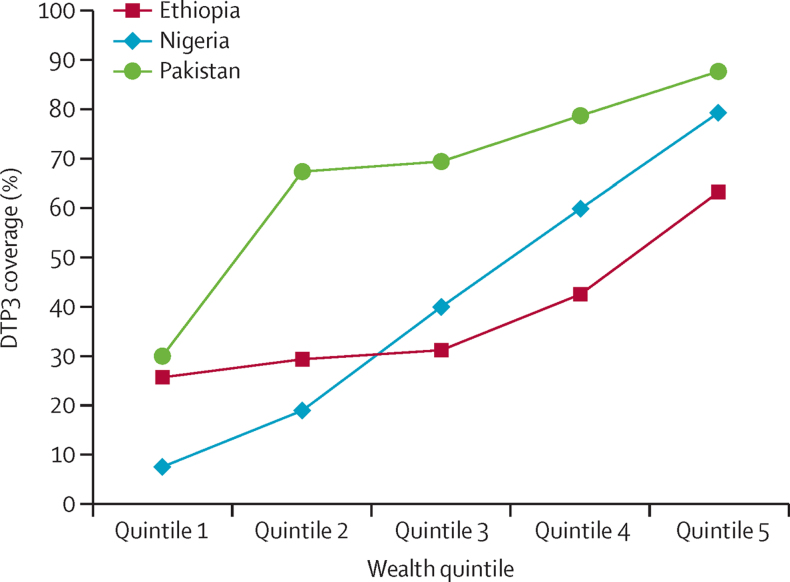
Disaggregating data by wealth quintile allows for closer examination of underlying shapes of within-country inequality, which helps to indicate equity-oriented approaches to expand coverage.19 For instance, a marginal exclusion pattern, as seen in Pakistan, generally shows a need for interventions targeted to the most disadvantaged subgroup (figure 4). The mass deprivation pattern in Ethiopia suggests a need for a population-wide approach that improves coverage in all subgroups. The queuing pattern, as reported in Nigeria, prompts an approach that combines population-wide and targeted interventions.
Figure 4.
Latest situation of DTP3 coverage among children aged 12–23 months in three high-priority countries, by economic status
Data taken from DHS 2011–13. DHS=Demographic and Health Survey. DTP3=three doses of the combined diphtheria, tetanus toxoid, and pertussis vaccine.
Analyses of change over time showed different patterns of national improvement in DTP3 immunisation coverage across countries. The SDGs call for movement towards universal coverage of health services,1 which should be realised in an equity-oriented manner: overall gains accompanied by accelerated improvements in disadvantaged populations.20 Programmes that promote expansion of health services should have an equity focus. Use of disaggregated data to track changes over time can show whether a country is achieving progressive realisation of universal coverage.21 Ghana and Nigeria, for instance, both reported national absolute annual change of 1 · 6 percentage points. Although Ghana reported a reduction of inequality (faster improvement in the poorest quintile than the richest), Nigeria reported a widening of inequality (faster improvement in the richest quintile than the poorest). Thus, in the case of DTP3 immunisation, data from Ghana indicated an equity-oriented progression towards universal coverage.
DTP3 coverage is an appropriate indicator to show a country's capacity to identify and deliver three doses of vaccine to the same child at appropriate times through routine systems.5 When successful, routine immunisation programmes offer a sustainable approach to delivering vaccines, because long-term delivery of vaccines can be integrated into the regular activities of national health systems.22 By contrast with routine programmes, immunisation campaigns can be delivered to provide immediate and widespread reach and, in doing so, have contributed to making progress towards eradicating some diseases or to increase coverage in specific acute situations (eg, conflicts, natural disasters, or outbreaks). However, campaigns are delivered outside of the routine system and might lack the resources to ensure sustainability, and recognition is growing of the benefits of transitioning back to routine immunisation. In some situations, supplementing routine immunisation with periodic intensification and outreach could be appropriate.22
Planning of vaccination campaigns should be informed by evidence on the distribution of coverage gaps, with dedicated efforts made to ensure that those people missed by routine systems are reached. Following WHO and UNICEF recommendations, the Reaching Every District (RED) and Reaching Every Community (REC) strategies have been implemented successfully in many countries, with the objective of addressing common obstacles to increase immunisation coverage in areas with low coverage. This approach outlines five operational components, with one focusing on re-establishment of regular outreach services. For outreach activities, health-facility staff leave their facility to deliver vaccine to those districts or communities. This approach is especially valuable for communities with difficult access.23
With the exception of Uganda, the high-priority countries highlighted in our study had high levels of economic-related inequality in DTP3 immunisation coverage, with poorer quintiles lagging behind the rest of the population. In general, economic-related inequality is typically reflected in patterns of geographical inequality and can be exacerbated in situations of insecurity or political instability within countries. Nigeria had especially amplified levels of inequality, which could be attributable partly to the country's federal system of governance (granting a high degree of autonomy to states in the delivery of health care, and resulting in variable levels of coverage). A country-tailored approach, based on replicating successes of high-performing states, is being piloted in Nigeria to address discrepancies between states.22 In Ethiopia, challenges in reaching remote areas have been addressed by introducing routine outreach programmes. In addition to fixed posts, this approach includes outreach services, which are anticipated to better reach communities that move seasonally.22 In DR Congo, infrastructure development is needed to overcome logistical challenges of distributing vaccines throughout the country.22 In Pakistan, overall strengthening of health systems is needed to deliver vaccines routinely to a growing number of children.22 Moving forward, assessments of equity-oriented efforts to improve coverage should be done, and successful interventions reported and taken to scale.
Strong health information systems are fundamental to monitoring inequalities in immunisation coverage and across all health topics. Household health surveys such as DHS and MICS provide harmonised, disaggregated immunisation data that are appropriate for between-country and within-country inequality monitoring. Household health surveys should be done according to a regular schedule and be expanded to countries where they are not currently done. According to GVAP recommendations, household surveys should be undertaken at least every 5 years in priority countries. In addition to survey data, information from administrative activities (eg, immunisation records kept by health facilities), censuses, and vital registration systems might be useful inputs for inequality monitoring. Whenever possible, data sources should contain small area identifiers (eg, postal codes) so that health data can be linked with—and disaggregated by—data about dimensions of inequality. For example, an analysis of inequality in DTP3 coverage in Bogota, Colombia, linked district-level data about socioeconomic and living conditions (gathered through national surveys) with facility data from immunisation registries.24 Future research at the country level is warranted to elucidate how to strengthen and develop health information systems effectively within national contexts. In our study we used 95% CIs to account for survey sampling error and assess statistical significance; however, from a public health perspective, significance might not indicate a situation that warrants remedial action. For instance, Jordan and Rwanda had significant—but, practically, very low—levels of absolute inequality (<3 percentage points between quintiles 1 and 5).
Pairwise difference and ratio inequality measures, which compare data in quintiles 1 and 5, do not take into account all data and can limit interpretability of results. In our study, we chose to present such measures for the sake of simplicity. To avoid possible limitations, we did compare conclusions arising from these measures with more complex inequality measures that take into account the full data (slope index of inequality for absolute inequality and concentration index for relative inequality) to ensure that they were similar. For reference, disaggregated data for all quintiles of all study countries are available in table 1. Similarly, the excess change measure, which expresses change in inequality over time, has an inherent limitation because it does not take into account changes in quintiles 2, 3, and 4. Figure 3 shows the change over time across these intermediate quintiles in the six high-priority study countries.
To interpret excess change, we must take into account the baseline level of coverage. In countries with elevated baseline levels of inequality, disadvantaged subgroups generally have low levels of coverage and, therefore, more room for improvement. In Gabon, for instance, less than 19% of children in quintile 1 of the baseline survey received vaccines versus 53% of children in quintile 5, indicating much room for improvement in terms of equity and overall coverage. By contrast, Jordan had nearly complete levels of DTP3 coverage across all wealth quintiles in both surveys, effectively achieving near-universal levels of coverage.
The estimates we report are based on disaggregated data from household health surveys. This information might differ from reported coverage data from national authorities, which are based typically on administrative reporting systems or official WHO and UNICEF estimates and are derived through triangulation of survey and facility data.
In conclusion, many study countries achieved a narrowing of economic-related inequality in DTP3 coverage over the past 10 years; however, substantial inequality persists within most countries and should be addressed on a priority basis through equity-oriented and context-appropriate policies, programmes, and practices. The regular monitoring of within-country inequalities in immunisation should have an important role in informing efforts to increase coverage in an equity-oriented manner, aiming for those with the greatest need to accrue the most substantial gains.
Acknowledgments
Acknowledgments
The views expressed in this Article are those of the authors and do not necessarily represent the views or policies of WHO.
Contributors
ARH had the idea for the paper. NB wrote the first draft of the report, with input from ARH. AJDB, AS, and ARH did the statistical analysis and prepared the figures and tables. AS, AJDB, TB, MG-D, PMH, and KS revised the report and provided edits and comments. All authors have read and approved the final version.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.United Nations Open working group proposal for Sustainable Development Goals. 2015. https://sustainabledevelopment.un.org/sdgsproposal.html (accessed Sept 7, 2015).
- 2.WHO . Global vaccine action plan: monitoring, evaluation & accountability 2011–2020. World Health Organization; Geneva: 2012. [Google Scholar]
- 3.UN . The Millennium Development Goals report 2015. United Nations; New York: 2015. [Google Scholar]
- 4.WHO. UNICEF . Global Immunization Vision and Strategy 2006–2015. World Health Organization; Geneva: 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brearley L, Eggers R, Steinglass R, Vandelaer J. Applying an equity lens in the Decade of Vaccines. Vaccine. 2013;31(suppl 2):B103–B107. doi: 10.1016/j.vaccine.2012.11.088. [DOI] [PubMed] [Google Scholar]
- 6.WHO Global vaccine action plan: monitoring, evaluation & accountability: secretariat annual report 2014. 2015. http://www.who.int/immunization/global_vaccine_action_plan/gvap_secretariat_report_2014.pdf (accessed July 21, 2016).
- 7.Clouston S, Kidman R, Palermo T. Social inequalities in vaccination uptake among children aged 0–59 months living in Madagascar: an analysis of Demographic and Health Survey data from 2008 to 2009. Vaccine. 2014;32:3533–3539. doi: 10.1016/j.vaccine.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 8.WHO . State of inequality: reproductive, maternal, newborn and child health. World Health Organization; Geneva: 2015. [Google Scholar]
- 9.Barros AJD, Ronsmans C, Axelson H. Equity in maternal, newborn, and child health interventions in Countdown to 2015: a retrospective review of survey data from 54 countries. Lancet. 2012;379:1225–1233. doi: 10.1016/S0140-6736(12)60113-5. [DOI] [PubMed] [Google Scholar]
- 10.Barata RB, Ribeiro MC, de Moraes JC, Flannery B. Socioeconomic inequalities and vaccination coverage: results of an immunisation coverage survey in 27 Brazilian capitals, 2007–2008. J Epidemiol Community Health. 2012;66:934–941. doi: 10.1136/jech-2011-200341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker AT, Smith PJ, Kolasa M. Reduction of racial/ethnic disparities in vaccination coverage, 1995–2011. MMWR Suppl. 2014;63:7–12. [PubMed] [Google Scholar]
- 12.Doherty E, Walsh B, O'Neill C. Decomposing socioeconomic inequality in child vaccination: results from Ireland. Vaccine. 2014;32:3438–3444. doi: 10.1016/j.vaccine.2014.03.084. [DOI] [PubMed] [Google Scholar]
- 13.Chan SS, Grundy J, Duncan R, Thor R, Bilous JB. From reaching every district to reaching every community: analysis and response to the challenge of equity in immunization in Cambodia. Health Policy Plan. 2013;28:526–535. doi: 10.1093/heapol/czs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delamonica E, Minujin A, Gulaid J. Monitoring equity in immunization coverage. Bull World Health Organ. 2005;83:384–391. [PMC free article] [PubMed] [Google Scholar]
- 15.UNICEF Statistics and monitoring: Multiple Indicator Cluster Survey (MICS) 2013. http://www.unicef.org/statistics/index_24302.html (accessed Sept 7, 2015).
- 16.Requejo J, Victora C, Bryce J. Data resource profile: countdown to 2015: maternal, newborn and child survival. Int J Epidemiol. 2014;43:586–596. doi: 10.1093/ije/dyu034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hancioglu A, Arnold F. Measuring coverage in MNCH: tracking progress in health for women and children using DHS and MICS household surveys. PLoS Med. 2013;10:e1001391. doi: 10.1371/journal.pmed.1001391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.USAID The DHS Program: wealth index. 2014. http://dhsprogram.com/topics/wealth-index/Index.cfm (accessed Sept 7, 2015).
- 19.WHO . Handbook on health inequality monitoring: with a special focus on low- and middle-income countries. World Health Organization; Geneva: 2013. [Google Scholar]
- 20.WHO. The World Bank . Tracking universal health coverage: first global monitoring report. World Health Organization; Geneva: 2015. [Google Scholar]
- 21.Hosseinpoor AR, Bergen N, Koller T. Equity-oriented monitoring in the context of universal health coverage. PLoS Med. 2014;11:e1001727. doi: 10.1371/journal.pmed.1001727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gavi, the Vaccine Alliance . Gavi, the Vaccine Alliance progress report 2013. Gavi, the Vaccine Alliance; Geneva: 2014. [Google Scholar]
- 23.Vandelaer J, Bilous J, Nshimirimana D. Reaching Every District (RED) approach: a way to improve immunization performance. Bull World Health Organ. 2008;86:A–B. doi: 10.2471/BLT.07.042127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mosquera PA, Hernandez J, Vega R. The impact of primary healthcare in reducing inequalities in child health outcomes, Bogota–Colombia: an ecological analysis. Int J Equity Health. 2012;11:66. doi: 10.1186/1475-9276-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.