Sir,
The posterior-most 10–20 μm of the corneal stroma has unique characteristics and provides a plane of cleavage in deep anterior lamellar keratoplasty (DALK). This has been termed the pre-Desccemets layer or Dua's layer (DL).1, 2 The initial publication on DL created some controversy. Many corneal surgeons readily related to it3, 4 and others contested its identity as a distinct layer.5 Herein, we present clear clinical evidence of the distinct nature of DL, in a patient who presented with persistent corneal edema following cataract surgery.
Case report
A 74-year-old lady presented with poor vision in the left eye (LogMar +0.52) on account of posterior sub-capsular cataract and nuclear sclerosis. She underwent an uncomplicated phacoemulsification procedure with a posterior chamber lens implant through a temporal incision. A week later, she presented with ‘hand movements' vision and a cloudy cornea, with epithelial bullae and stromal edema. The anterior chamber did not show any cells and the intraocular pressure was 14 mm of Hg. She was treated with topical dexamethasone 0.1%, 2 hourly, and chloramphenicol 0.5%, four times a day.
The corneal edema did not settle. Eleven weeks post surgery an optical coherence tomography (OCT) of the cornea revealed Descemet's membrane (DM) detachment and she was managed with air injection into the anterior chamber. Repeat OCT carried out at 4 and 8 weeks post air injection showed persistent ‘Descemet's detachment' and a well-defined patch of corneal edema (Figure 1a and b) covering most of the pupil. Her vision was ‘counting fingers'.
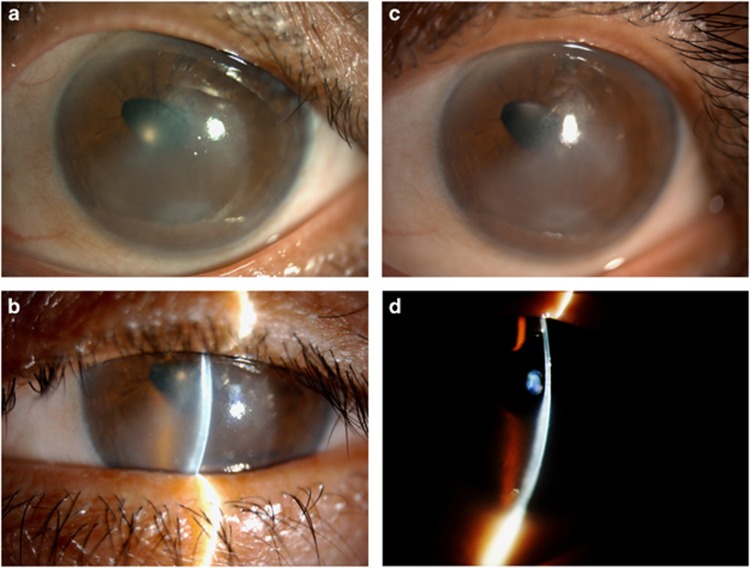
Figure 1.
Slit-lamp diffuse and slit images of left cornea: 11 weeks post cataract surgery. (a) Corneal edema affecting predominantly the infero-temporal quadrant of the left cornea and covering more than half the pupillary area. The pupil is oval shaped. (b) Slit image shows considerable thickening of the stroma. Five months post cataract surgery. (c) The corneal edema shows some improvement as more than half the pupillary area is clear. (d) The slit image does not show much improvement in the stromal thickening.
At 5 months post her original cataract surgery she presented to one of us (HSD) for a second opinion. The edema had cleared to some extent (Figure 1c and d), but pachymetry was 930±12 μm. She complained that her vision was blurry on waking in the morning and clearer by mid-morning, especially on the nasal side. OCT scans were repeated. She was offered endothelial keratoplasty, but she declined.
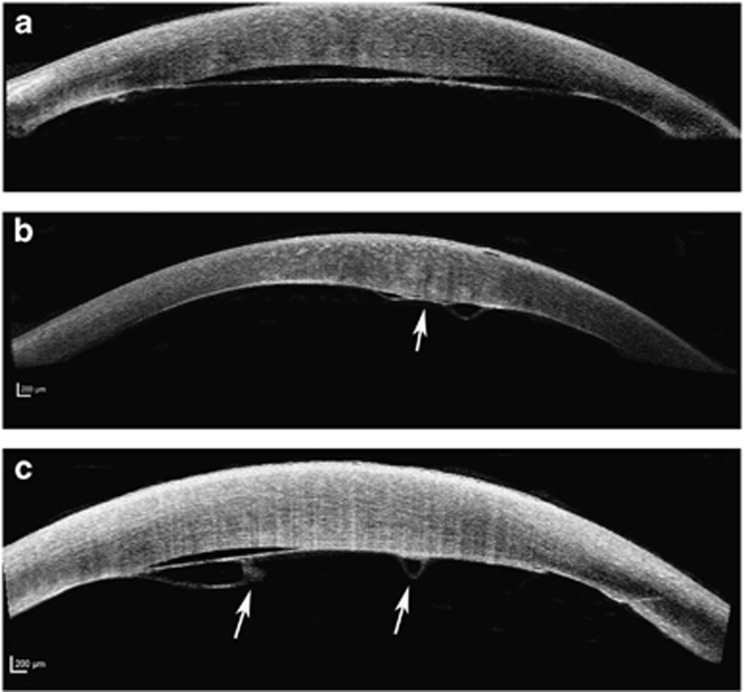
A review of all her OCT scans revealed that there was a detachment of the DM and DL, which corresponded accurately to the area of corneal edema (Figure 2a). At places two distinct lines were seen indicating separation of DM and DL (Figure 2b). In the lower third, the two hyper-reflective lines of detachment were clearly evident. The anterior line was thicker and taut, whereas the posterior line was curved with a scroll at the end. The scroll was better seen on the nasal edge of the posterior line (Figure 2c). The posterior hyper-reflective line was characteristic of a DM detachment and tear. The detached DL with detached and torn DM was seen in all scans taken before the air injection procedure and the others taken at ~4-weekly intervals thereafter. The site of DM tear corresponded to the side-port incision and was possibly related to intraoperative trauma.
Figure 2.
Optical coherence tomography (OCT) of the cornea (Spectralis, Heidelberg Engineering, Heidelberg, Germany). (a) OCT scan in a plane corresponding to the upper third of the area of edema. A clear thick line of detachment is seen along the posterior (Descemets membrane and endothelium) aspect of the corena. The detached layer is not torn. (b) OCT scan in a plane corresponding to the mid-third of the area of edema. The posterior hyper-reflective line with folds into the anterior chamber corresponds to the detachment of Descemets membrane, which in the middle (arrow) is attached to the Dua's layer (DL) that itself is separating from the posterior stroma. (c) OCT scan in a plane corresponding to the lower third of the area of edema. A posterior-curved hyper-reflective line with a central-scrolled edge, corresponding to detachment of the Descements membrane is clearly visible. Anterior to this is the distinct taut image of the detached DL. Arrows point to the two central ends of the torn Descemets membrane.
Comment
This is the first demonstration of DL in clinical pathology of the posterior cornea. Dua et al1 had postulated that DL could have a role in acute hydrops of keratoconus. Subsequently, Yahia Chérif et al4 showed that suturing the DL without DM resulted in rapid resolution of the hydrops and presented this as evidence of the existence of DL. The plane between DL and deep stroma can be accessed surgically, and two surgical procedures namely DALK-triple and pre-Descemets endothelial keratoplasty have been designed around DL.6
DL is made of five to eight compact thin lamellae of type 1 collagen, has an abundance of type 6 (long spacing) collagen, is devoid or sparsely populated with keratocytes, is impervious to air, is populated by trabecular cells at the peripheral 350 μm and continues as the collagen core of the trabecular meshwork.1, 7 Recently, Lewis et al8 demonstrated an extensive network of elastin fibers in the cornea that are concentrated in the pre-Descemets layer and as an annulus at the limbus. The case reported herein adds to the body of evidence illustrating the unique nature of DL, and the increasing recognition of its role in corneal pathology and lamellar surgery.
Acknowledgments
This work was supported by Elizabeth C King Trust, USA.
The authors declare no conflict of interest.
References
- Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre Descemet's layer (Dua's layer). Ophthalmology 2013; 120: 1778–1785. [DOI] [PubMed] [Google Scholar]
- Dua HS, Mastropasqua L, Faraj L, Nubile M, Elalfy MS, Lanzini M et al. Big bubble deep anterior lamellar keratoplasty: the collagen layer in the wall of the big bubble is. unique. Acta Ophthalmol 2015; 93: 427–430. [DOI] [PubMed] [Google Scholar]
- Goweida MB. Intraoperative review of different bubble types formed during pneumodissection (big-bubble) deep anteriorlamellar keratoplasty. Cornea 2015; 34: 621–624. [DOI] [PubMed] [Google Scholar]
- Yahia Chérif H, Gueudry J, Afriat M, Delcampe A, Attal P, Gross H et al. Efficacy and safety of pre-Descemet's membrane sutures for the management of acute corneal hydrops in keratoconus. Br J Ophthalmol 2015; 99: 773–777. [DOI] [PubMed] [Google Scholar]
- Schlötzer-Schrehardt U, Bachmann BO, Tourtas T, Torricelli AA, Singh A, González S et al. Ultrastructure of the posterior corneal stroma. Ophthalmology 2015; 122: 693–699. [DOI] [PubMed] [Google Scholar]
- Dua HS, Faraj L, Said DG. Dua's layer: discovery, characteristics, clinical applications, controversy and potential relevance to glaucoma. Expert Rev Ophthalmol 2015; 10: 1–17. [Google Scholar]
- Dua HS, Faraj LA, Branch MJ, Yeung AM, Elalfy MS, Said DG et al. The collagen matrix of the human trabecular meshwork is an extension of the novel pre-Descemet's layer (Dua's layer). Br J Ophthalmol 2014; 98: 691–697. [DOI] [PubMed] [Google Scholar]
- Lewis PN, White TL, Young RD, Bell JS, Winlove CP, Meek KM. Three-dimensional arrangement of elastic fibers in the human corneal stroma. Exp Eye Res 2015; 146: 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]