Abstract
Purpose
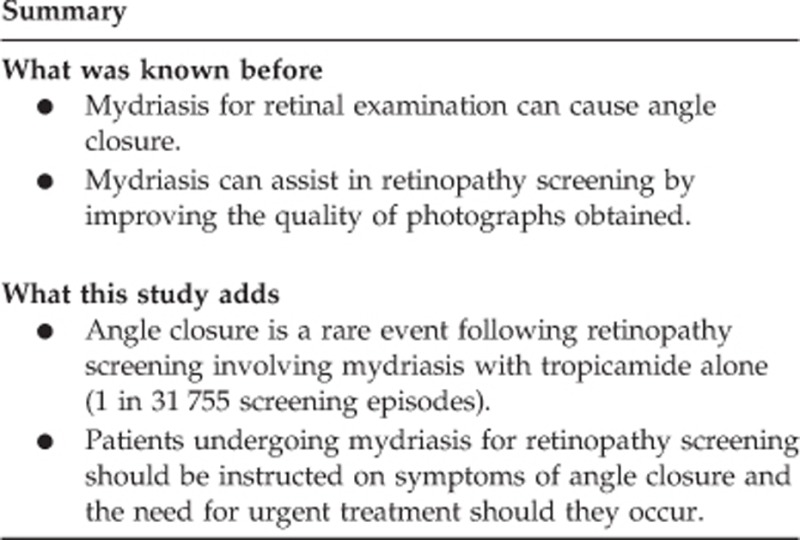
To ascertain the risk of angle closure glaucoma associated with mydriasis in the Northern Ireland Diabetic Retinopathy Screening Programme.
Methods
A retrospective case note review was carried out, cross referencing hospital records with those of the screening programme, to identify episodes of angle closure glaucoma, which occurred within 14 days of a retinopathy screening episode involving pharmacological mydriasis.
Results
Three cases of angle closure following mydriasis for screening were identified. The incidence of angle closure within the screening programme was calculated to be 1 in 31 755 patients dilated or 0.75 patients per year.
Conclusion
Angle closure is a rare complication of mydriasis used in photographic screening for diabetic retinopathy. We advocate the provision of clear instructions to patients in screening programmes on when and how to access emergency ophthalmic care following dilation to prevent loss of vision in this rare event.
Introduction
The Northern Ireland Diabetic Retinopathy Screening Programme (NIDRSP) provides a regional screening service to those with diabetes mellitus, estimated to be 60 000, with the aim of identifying sight-threatening diabetic retinopathy using the fundal photography. Fundus photographs are captured at screening clinics at local healthcare facilities and are graded at a central screening office with reports returned to each patient's general practitioner with advice on action recommended, if any.
Mydriasis is known to improve the sensitivity of fundal photographs.1, 2 In the NIDRSP, mydriasis is achieved by the instillation of tropicamide 1% drops into the eyes of the following groups of patients: those over 50 years of age at the time of screening and those under 50 in whom the quality of images obtained without mydriasis is inadequate (~25% of those under 50 years of age screened). Patients may refuse to have drops instilled, and if this is the case, photography is attempted without mydriasis. Angle closure glaucoma is a rare side effect of diagnostic mydriasis, with the risk estimated as 0.3–0.03%.3, 4
The purpose of this study was to ascertain the risk of angle closure associated with mydriasis in the NIDRSP.
Materials and methods
The care of acute ophthalmic emergencies in Northern Ireland is co-ordinated in the ophthalmology departments of the Royal Victoria Hospital, Belfast and Altnagelvin Area Hospital, Londonderry.
We aimed to identify all presentations of acute angle closure from January 2007 to December 2010. We used clinical coding to identify all diagnoses of angle closure, and all peripheral iridotomy procedures carried out within the two healthcare facilities during this time period. We then cross-referenced patient details with NIDRSP records, identifying cases where the diagnosis or procedure occurred within 14 days of a screening episode in which a mydriatic agent was used. Case notes were then reviewed with the appropriate Institutional Board review.
Results
We identified three cases of angle closure occurring within 14 days of mydriasis for retinopathy screening. We present the cases below.
Case report 1
The patient presented to Eye Casualty 4 days following dilation for diabetic retinopathy screening with symptoms of angle closure and unilateral reduced visual acuity. Best-corrected visual acuity was OD 6/60, OS 6/12, and the intraocular pressure measured was 30 mm Hg OD and 12 mm Hg OS. Anterior chambers were noted to be shallow. Bilateral laser peripheral iridotomies were performed. At most recent review, 15 months after presentation, the patient remained phakic with patent peripheral iridotomies and normal intraocular pressures. Visual acuity was OD 6/12, OS 6/12.
Case report 2
The patient presented to Eye Casualty the day following dilation for diabetic retinopathy screening with symptoms of angle closure and unilateral reduced visual acuity. Best-corrected visual acuity was OD 6/9, OS 6/36, and the intraocular pressure measured was 20 mm Hg OD and 52 mm Hg OS. Peripheral iridotomies were performed, relieving the angle closure, and the visual acuity had recovered the next day to OD 6/9, OS 6/9. Three months later, the patient underwent uneventful left cataract surgery with intraocular lens. The axial length was recorded as 22.65 mm with an optical anterior chamber depth of 2.15 mm. The patient declined right cataract surgery. At most recent review, 27 months after presentation, the visual acuity measured OD 6/9 and OS 6/9; there was moderate cupping of the left optic disc.
Case report 3
The patient presented to Eye Casualty the day following dilation for diabetic retinopathy screening with bilaterally reduced visual acuity (OD 6/24, OS 6/60), and the intraocular pressures initially measured was 52 mm Hg OD and 60 mm Hg OS. Bilateral laser iridotomies were performed and the intraocular pressures normalised to 14 mm Hg OU. At most recent review, 22 months hence, the visual acuity was 6/9 OU and the patient remained phakic bilaterally. Of note, the patient had refused dilating drops on all occasions following the episode of angle closure.
We have identified three cases of angle closure in 4 years associated with mydriasis for diabetic retinopathy screening by the NIDRSP. During that time, there were 95 265 screening episodes where dilating drops were used. The risk of angle closure was 1 in 31 755 patients dilated. The annual incidence of angle closure was 0.75 cases per year.
Discussion
Angle closure is a rare complication of mydriasis used in photographic screening for diabetic retinopathy. Two of the patients detailed here presented within 24 h of the screening episode, and all presented based on their symptoms. None have suffered severe visual loss as a result of the episode of angle closure. We advocate the provision of clear instructions to patients in screening programmes on when and how to access emergency ophthalmic care in order to prevent severe visual loss from this rare event.
The starting point for this study was the observation that we had noted more than one patient presenting with acute angle closure following dilation for community photographic diabetic retinopathy screening. We were keen to ascertain the scale of any problem, and we are pleased to report that angle closure is a rare complication of pharmacological dilation for diabetic retinopathy screening. As we are working in a geographically well-defined comprehensive healthcare system, we are confident that our search strategy has identified all cases of acute angle closure precipitated by retinopathy screening, and that it is unlikely that patients would have sought care elsewhere. It is possible that a patient may have been travelling outside of Northern Ireland in the period following their screening and sought emergency treatment elsewhere, but as a resident of Northern Ireland would usually return to our service for ongoing NHS care, and we would hope these patients would be picked up by our search strategy unless there was a delay in referral back to us. It is possible that our search strategy may have missed a sub-acute presentation (more than 14 days following the screening episode) but we did not seek to identify these due to the increased difficulty of attributing causation with the passage of time. We are also pleased to report that the visual outcomes were satisfactory, possibly due to the prompt presentations and timely treatments, thereby ensuring that minimal harm was done by the screening process in line with World Health Organisation standards.5 Murgatroyd et al6 have shown that mydriasis with tropicamide improves the screening process by reducing the number of ungradable photographs from 26 to 5% in retinopathy screening.
No information is gathered on lens status by the NIDRSP, therefore we are unable to comment on the risk in phakic patients alone. Although accepting that the theoretical risk in pseudophakes is nil, we feel that an overall estimate of risk in the population of patients with diabetes is useful to those planning screening programmes, or indeed to non-specialists considering dilatation with tropicamide without being aware of the significance of a history of cataract surgery. We were also unable to ascertain the number of individuals screened (as opposed to the number of screening episodes) from the data obtained, though a crude estimation could be made through our knowledge of the approximate screening interval (15 months). We agree that the incidence per patient would be useful, but also feel that the incidence per screening episode is a valid measure, particularly where we have no information on other relevant events potentially affecting risk within the time period, for example, cataract surgery.
The risk of angle closure ascertained here is less than reported in other publications. The population-based Rotterdam Study3 reported an incidence of angle closure of 3 in 10 000 following diagnostic mydriasis with tropicamide 0.5% and phenylephrine 2.5% (with miosis induced by thymoxamine 0.5% subsequently). The Baltimore Eye Survey4 dilated 4870 subjects with no episodes of angle closure. This study excluded and examined separately those deemed to have potentially occludable angles. They ascertained an overall risk of dilating a potentially occludable angle, after accurate screening for such patients, to be <1 in 333. A systematic review of published research 1933–1999 found no cases of angle closure precipitated by the use of tropicamide drops alone and reported them to be safe.7 Our study suggests that angle closure can be induced by the use of tropicamide alone.
There are several reported methods of screening for those at risk of angle closure on mydriasis. These include ascertainment of a history of glaucoma along with a shallow anterior chamber on pentorch examination,4 and slit lamp assessment including the VanHerick test.8 The papers describing these tests also report their lack of sensitivity and specificity. They also require training and a level of expertise. Our community screening programme is carried out by trained photographers, and it is not practical to perform such screening tests before dilation in this scenario. Thus far we have relied on informing patients of the symptoms of angle closure and asking them to present promptly in the rare event that they should develop such symptoms. This study vindicates such an approach.
This case series improves our ability to inform patients of the low risk of angle closure within our service. It has been agreed there will be ongoing surveillance of angle closure glaucoma cases associated with a screening episode to provide further information.
The authors declare no conflict of interest.
Footnotes
This study was presented at UKEGS, Manchester, December 2011/Irish College of Ophthalmology Conference, Cavan, May 2011 (poster)/Royal College of Ophthalmologists, May 2011 (poster).
References
- Klein R, Klein BEK, Neider MW, Hubbard LD, Meuer SM, Brothers RJ et al. Diabetic retinopathy as detected using ophthalmoscopy, a non-mydriatic fundus camera and a standard fundus camera. Ophthalmology 1985; 92: 485–491. [DOI] [PubMed] [Google Scholar]
- Pugh JA, Wiley R, Tuley MR, Velez R, van Heuven WAJ, Jacobson J et al. Diabetic retinopathy screening: the non-mydriatic camera (NMRC) performs better mydriatically. Diabetes 1990; 39: 170A. [Google Scholar]
- Wolfs RC, Grobbee DE, Hofman A, de Jong PT. Risk of acute angle-closure glaucoma after diagnostic mydriasis in non-selected subjects: the Rotterdam study. Invest Ophthalmol Vis Sci 1997; 38: 2683–2687. [PubMed] [Google Scholar]
- Patel KH, Javitt JC, Tielsch JM, Street DAKatz J, Quigley HA et al. Incidence of angle-closure after pharmacologic mydriasis. Am J Ophthalmol 1995; 120: 709–717. [DOI] [PubMed] [Google Scholar]
- Wilson JMG, Jungner G. Principles and practice of screening for disease. WHO Chronicle 1968; 22(11): 473. [Google Scholar]
- Murgatroyd H, Ellingford A, Cox A, Binnie M, Ellis JD, MacEwen CJ et al. Effect of mydriasis and different field strategies on digital image screening of diabetic eye disease. Br J Ophthalmol 2004; 88: 920–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit RJ, Taylor R. Mydriasis and glaucoma: exploding the myth. A systematic review. Diabet Med 2000; 17: 693–699. [DOI] [PubMed] [Google Scholar]
- Terry JE. Mydriatic angle-closure glaucoma – mechanism, evaluation and reversal. J Am Optom Assoc 1977; 48: 159–168. [PubMed] [Google Scholar]


