Abstract
Background: The transgender community is one of the most marginalized sections of our society. The literature is scarce regarding the pathology and laboratory medicine challenges associated with caring for transgender patients.
Objective: To summarize the available gender-transitioning options and to discuss healthcare challenges, from a pathology/laboratory medicine perspective, in the care of transgender patients.
Method: We reviewed the current terminology and epidemiology relevant to the transgender population in preparing our analysis.
Conclusions: The main transgender healthcare challenges in pathology/laboratory medicine practice include the inflexibility of electronic medical records in documenting affirmed gender, unfamiliarity among medical and laboratory professional with the needs of and terminology related to the transgender population, lack of reference ranges for laboratory tests, unclear guidelines regarding gender classification for blood donation eligibility criteria, and paucity of experience in handling and interpreting surgical and cytologic specimens from gender-transitioning individuals. Directed efforts to overcome these shortcomings, coupled with a more welcoming posture, are essential to achieving the highest standards of care for the transgender population.
Keywords: transgender, healthcare disparities, sex reassignment procedures, clinical pathology, clinical pathology, gender identity
The transgender community is among the most underserved and underrepresented subgroups in our society.1 In this review, we focus on the common terminology regarding the epidemiology of and challenges faced by transgender people in receiving essential healthcare, from the pathology/laboratory medicine perspective.
Definitions
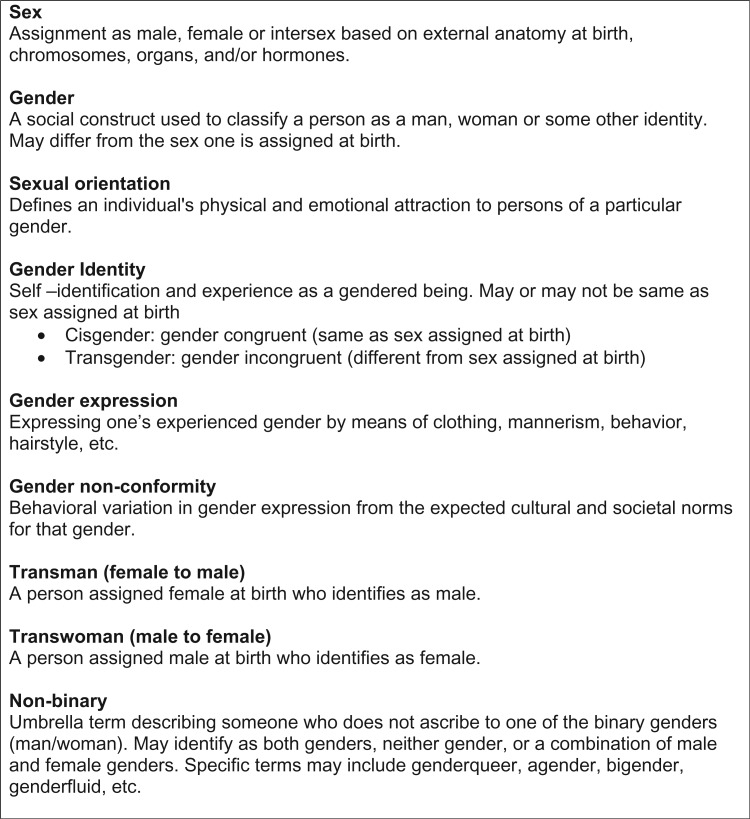
The assignment of an individual as being of the male or female sex is most often based on the phenotypic appearance of the external genitalia at birth, which is largely determined by the chromosomal type (most commonly 46,XX or 46,XY). Gender identity, however, is an individual’s perceived or experienced gender, which may or may not be the same as one’s sex assigned at birth. The concept of gender identity includes gradations of masculinity to femininity and maleness to femaleness, as well as identification of some individuals as having nonbinary gender, which means being essentially neither male nor female, or a combination of both.2 Gender nonconformity is behavioral variation in gender expression (eg, clothing, mannerisms, accessories, and hairstyles) from cultural and societal norms expected for that gender. Sexual orientation is defined as the physical and emotional attraction of an individual to same-sex people (lesbian or gay; homosexual), both same-sex and opposite-sex people (bisexual), or opposite-sex people (heterosexual).
Transgender is an all-inclusive term that may include all individuals whose gender identity or expression does not align with their assigned birth sex and/or those whose gender identity is outside of the binary male/female classification. Cisgender is the term for those whose gender identity or expression aligns with their assigned birth sex. Transsexual, an older term, refers to those who identify as transgender and use medical and/or surgical means to physically transition. The term transsexual is perceived by many in the community to be overly pathologizing and has been largely replaced by the term transgender.
Transgender people may be classified into 3 main categories. Transwomen are assigned the male gender at birth and affirm a feminine identity. Transmen are assigned the female gender at birth and affirm a masculine identity. People who do not identify with the binary male or female gender may identify with the term nonbinary, an all-inclusive term that includes specific genders, such as genderqueer, agender, bigender, and genderfluid. Transgender people often prefer to be addressed by a name that may be different from their legal or given name. Additionally, they may use pronouns that reflect their gender identity/expression (he/him/his for transmen and she/her/hers for transwomen). Some nonbinary people may use nonbinary pronouns (ze/zir/zirs, hir/hirs, ne/nir/nirs, they/them/their). Transgender people often have legal identity documents such as passports, driver’s licenses, and insurance cards based on their assigned sex at birth, incongruent with their affirmed gender (Figure 1).
Figure 1.
Terminology and definitions used in discussing transgenderism.
Gender incongruity and gender nonconforming behaviors by themselves do not equate to a pathologic process. The Diagnostic and Statistical Manual of Mental Disorders (DSM)–5 diagnosis of gender dysphoria describes the clinically significant distress or impairment in social, occupational, and other important areas of functioning arising out of marked incongruence between one’s experienced/expressed gender and one’s assigned gender.3 This distress must have been present for at least 6 months duration and must fulfill 2 of the additional 6 criteria listed in the DSM-5.
Evidence-based medicine offers a variety of therapeutic options for individuals seeking treatment for gender dysphoria. The number and type of interventions applied and the order in which they take place, however, may differ from person to person.4-8 Transgender people with gender dysphoria may undergo treatment with cross-sex hormones and/or gender-affirming surgeries as part of a medical transition. Transgender individuals may be treated in any combination of medical or surgical interventions to alleviate gender dysphoria to the fullest extent possible. However, for many transgender persons in the United States, exclusionary insurance policies make many surgical therapies financially infeasible.
According to the latest guidelines issued by World Professional Association for Transgender Health, Standards of Care, version 7,9 a psychosocial assessment by a qualified mental health professional is recommended to confirm the diagnosis of gender dysphoria and the individual’s capacity to give informed consent. Coexisting mental health disorders, although not a contraindication to care, must be identified and treated if present. Ongoing therapy is recommended, although it is not required. Cross-sex hormones and top surgery (bilateral mastectomy with male chest reconstruction) for transmen can be initiated after the appropriate mental health assessment is complete. It is recommended that a patient requiring bottom surgery (orchiectomy, penectomy, or vaginoplasty for transwomen; or oophorectomy, hysterectomy, metoidioplasty, or phalloplasty for transmen) have completed 1 year of hormones and living in the affirmed gender and have obtained 2 letters of recommendation from mental health professionals.
Epidemiology
Inconsistency in diagnostic classifications and difficulties in identification have led to wide variations in the estimated prevalence of transgender populations across the world. Many studies have made estimates by using the easily accounted numbers of the subgroup accessing treatment at specialized European gender-reassignment clinics. One such study from The Amsterdam Gender Dysphoria Clinic, which has collected data on the Dutch transgender population for more than 4 decades, has estimated the prevalence to be roughly 1 in 10,000 assigned males and 1 in 30,000 assigned females.10 In a more recent review, which is the largest meta-analysis to date of the prevalence of transgenderism (as defined by the International Statistical Classification of Diseases and Related Health Problems, 10th revision [ICD-10]),11 Arcelus et al reported a prevalence of approximately 1 in 20,000 individuals in the overall population; 1 in 15,000 for transwomen; and 1 in 40,000 for transmen.12
A clear increase in the prevalence of transgender individuals is noted consistently across all the studies we examined that were performed in the past 50 years. However, because most studies depended on a clinical database that defined the population based on previous genital surgery or severe dysphoria, these numbers are likely an underestimate of the true prevalence. A significant majority of this population group may not attend such clinics for fear of discrimination, because of financial limitations, or because they do not require the specific procedures offered. A recent United States study that more broadly defined individuals who identify as transgender reported an overall prevalence of 1 in 200 individuals.13 Overall, the paucity of demographic data pertaining to gender identity makes it difficult to estimate the true prevalence with any certainty.
Stigma Related to Transgenderism
Despite the ever-increasing visibility of transgender individuals in the media in the United States, the transgender population remains one of the most underserved subgroups in this country. The rates of unemployment, clinical depression, anxiety disorders, interpersonal violence, family rejection, workplace discrimination, physical abuse, mental abuse, suicide risk, substance abuse, and serious illnesses such as human immunodeficiency virus (HIV) are amongst the highest of any group.14 Although many review articles have dealt with these issues, we approach transgender healthcare from the pathology/laboratory medicine perspective in this article.
Healthcare Obstacles and Challenges
There are multiple impediments to optimal healthcare for the transgender population. Societal intolerance and stigmatization, combined with discriminatory practices in healthcare settings, have resulted in decreased access to adequate healthcare.15 Greater media attention has increased public awareness of transgender issues, but the lived experience of many transgender individuals is still filled with hardship. Healthcare providers may lack sensitivity to transgender issues, such as the need to ask about preferred names and pronouns. Electronic medical records (EMRs) and laboratory information systems (LISs) often do not allow for gender designations beyond assigned sex, thus resulting in misgendering of transgender patients.
Additional problems arise for patients who have legally changed their sex designation to match their affirmed gender. For example, many EMRs structure procedure orders to the patient’s recorded sex, thus making it difficult to order a prostate ultrasound on a transwoman or to create a pregnancy encounter for a transman. The EMR working group convened by a World Professional Association for Transgender Health (WPATH) executive committee in 2011 recommended that the demographic variables of an EMR should include preferred name, assigned sex at birth, gender identity, and pronoun preference.16 These practices remain uncommon in the United States, although the situation may improve as the U. S. Department of Health and Human Services has mandated that all EMRs must collect data on gender identity, to meet the requirements outlined in Stage 3 of the Meaningful Use incentive program.17 Additional practical issues in the healthcare setting include the limited availability of unisex restrooms in outpatient settings and challenges associated with shared rooms in inpatient units.
Also, in the United States, healthcare for transgender and gender-nonconforming people is limited by a lack of health insurance or other means to pay for the medical care used to treat gender dysphoria. The passage of the Affordable Care Act (ACA) in the United States (2010), which redefines sex to include gender identity and strictly prohibits “sex-based discrimination” in the healthcare domain, has been beneficial to the health of the transgender community. The ACA clearly mandates that service providers and agencies provide access to essential preventative procedures and treatments (eg, mammograms for transwomen and Papanicolaou [Pap] tests for transmen) if deemed necessary by a medical provider. However, in most cases, the implementation of this law currently falls short of mandating coverage for gender-transition services, including cross-sex hormones and gender-affirming surgeries.
Next, we describe the 2 most commonly practiced gender-affirming interventions. These options highlight the role of the field of pathology department in promoting the highest standards of care for the transgender community.
Hormonal and Surgical Options for Transgender Individuals
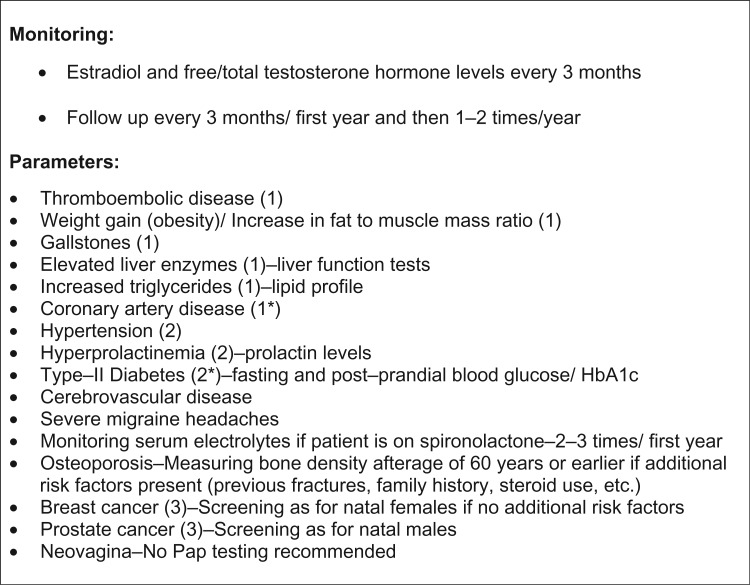
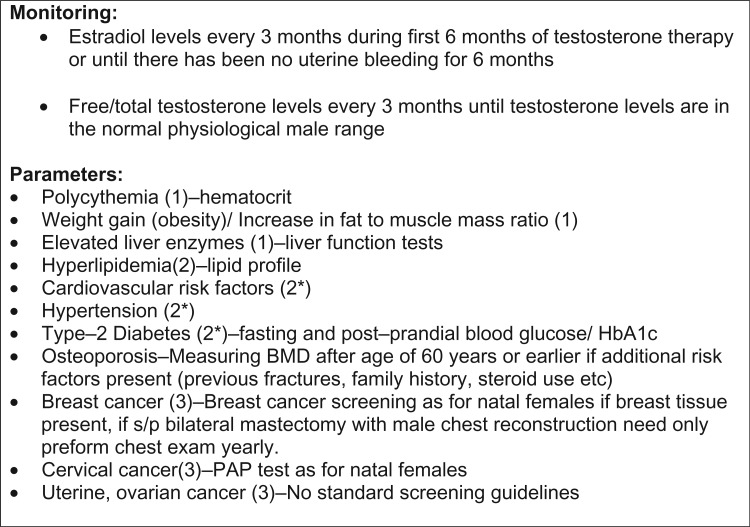
For many transgender people, cross-sex hormone therapy is the mainstay of treatment for their gender dysphoria. Feminizing medications used in transwomen include 17β-estradiol administered by mouth, transdermally, or intramuscularly. Also, spironolactone is often used as an androgen antagonist. Masculinizing medications for transmen include testosterone administered transdermally or via injection (subcutaneous or intramuscular).18 The Endocrine Society recommends starting with minimum doses of cross-sex hormones to maintain normal physiological ranges for the desired sex. Like any other intervention, hormonal therapy has its own risks and requires regular clinical and laboratory monitoring. The Endocrine Society Clinical Guidelines published in 2009 recommend that individuals who undergo cross-sex hormonal therapy be followed up every 3 months for the first year and once or twice a year thereafter to evaluate the appropriateness of physical changes, hormonal levels, and adverse factors.19 Cardiovascular risk factor surveillance is recommended in all patients undergoing hormonal therapy; specific recommendations are made for transwomen and transmen based on differences in hormonal therapy (Figure 2 and Figure 3).
Figure 2.
Monitoring Guidelines and Parameters for Transwomen.19 (1) Indicates likely increased risk with * or without additional risk factors; (2) indicates possible increased risk with * or without additional risk factors; (3) indicates no increased risk.
Figure 3.
Monitoring guidelines and parameters for transmen.19 (1) Indicates likely increased risk with * or without additional risk factors; (2) indicates possible increased risk with * or without additional risk factors; (3) indicates no increased risk
Gender-affirming surgical options for transwomen include nongenital surgeries such as breast augmentation, liposuction, facial feminization surgery, lipofilling, voice feminization surgery, thyroid cartilage reduction, and gluteal augmentation. Genital feminizing surgeries include bilateral orchiectomy, penectomy, and options for remodeling the genital tract via clitoroplasty, vaginoplasty, and/or vulvoplasty.
Similarly, transmen may opt to undergo bilateral total or partial mastectomy, chest contouring, liposuction, lipofilling, liposurgery, and/or pectoral implants. Genital masculinizing surgeries include metoidioplasty (lengthening and straightening of the testosterone-enlarged clitoris to create a neophallus), phalloplasty, urethral lengthening and scrotal reconstruction with insertion of testicular prostheses with or without hysterectomy, and or bilateral salpingo-oophorectomy (removal of the fallopian tubes and ovaries).
Health Maintenance for Transwomen
Transwomen treated with estrogen without other risk factors for breast cancer should follow the standard breast screening guidelines for cisgender women. Prostate cancer is rare in transwomen who have undergone gonadectomy secondary to decreased exogenous testosterone. However, even if a transwoman undergoes gender-affirming surgery, including penectomy, orchiectomy, and vaginoplasty, the prostate will most likely be left intact. Current consensus guidelines recommend that all transwomen follow the same screening guidelines for prostate cancer that are recommended for cisgender males.19
Health Maintenance for Transmen
The American College of Obstetricians and Gynecologists (ACOG) recommends that transmen with a cervix follow the same screening guidelines as cisgender females. Age appropriate mammography screening for breast cancer should also be continued unless mastectomy has occurred. For patients using testosterone therapy with an intact uterus, there may be an increased risk of endometrial cancer and ovarian cancer.20 Three cases of ovarian cancer have been reported in transmen.21 Due to a largely unknown risk of these malignant neoplasms coupled with potential delay in diagnosis due to reasons discussed previously herein, the aforementioned surgeries may be considered in these patients, especially in those older than 40 years or who have unexplained vaginal bleeding. Currently, transmen who retain their uterus and ovaries are followed up in a similar fashion to cisgender females, due to an absence of formal screening guidelines.
Blood Donor Eligibility and Transgender Individuals
Issues associated with eligibility for blood donation arise for transgender individuals. For example, the risk assessment of potential blood donors includes questions on whether males have had sex with other males and whether females have had sex with males who have had sex with other males.22 For decades, “yes” responses to these questions have resulted in an indefinite deferral for blood donation. More recently, the U. S. Food and Drug Administration (FDA) has changed recommendation from indefinite deferral to 12-month deferral, provided that no other reasons for indefinite deferral are present.23 This change in the recommendation raises the question of how to answer these questions for transmen or transwomen who have had sex with males, before or after gender transition. A discussion of various scenarios is documented in the summary of the November 2012 meeting of the American Association of Blood Banks (AABB) FDA Liaison Committee.24 The most recent FDA guidance on this issue is as follows: “The FDA’s recommendation to blood establishments is that in the context of the donor history questionnaire, male or female gender should be self-identified and self-reported for the purpose of blood donation.”23
In addition to the sexual history–based questions, donor centers may also have additional eligibility criteria based on gender. For instance, the American Red Cross has weight and height criteria that differ by gender for donors younger than 18 years and for double red blood cell donors.25 In general, the eligibility criteria for transgender individuals who wish to donate blood needs further study and more clarity.
The Pathology and Laboratory Medicine Perspective
With the transgender population gaining cultural visibility, guidelines and recommendations for screening and treatment are expected to become more elaborate and comprehensive. However, certain basic issues need to be addressed before we can envision the goal of promoting the highest standards of transgender healthcare. To begin, formal training of physicians, nurses, and laboratory staff at all levels would be a major step toward achieving optimal healthcare delivery to this patient subgroup.
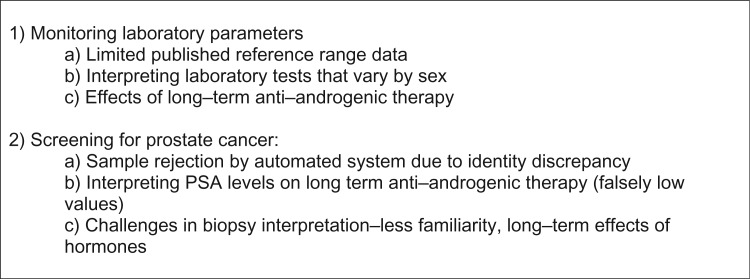
The lack of a standardized definition of “normal” laboratory values is the major challenge faced by laboratory staff in reporting clinical laboratory or surgical pathology results for the transgender patient population. The interpretation of laboratory data in transgender patients is especially complicated for laboratory tests that have sex-specific reference ranges, such as tests of liver enzyme, creatinine, and hematocrit levels. There is a scarcity of scientific studies on this topic, which makes it difficult for healthcare providers to decide what reference range is “normal” for each patient.
In the largest retrospective study to date of laboratory values in the transgender population, the results of multiple laboratory tests did not fit into the standard male or female reference ranges.26 The data reported by those researchers suggest the urgent need to empirically determine new reference ranges for transgender patients. There is likely heterogeneity in these values even within the transgender population because many laboratory parameters would be affected by hormonal and surgical therapy in ways currently not fully understood. A striking example is that of prostate-specific antigen (PSA) levels, a test used in screening for prostate cancer, which is falsely decreased with long-term antiandrogenic therapy and therefore is likely not a reliable tumor marker in transwomen.27
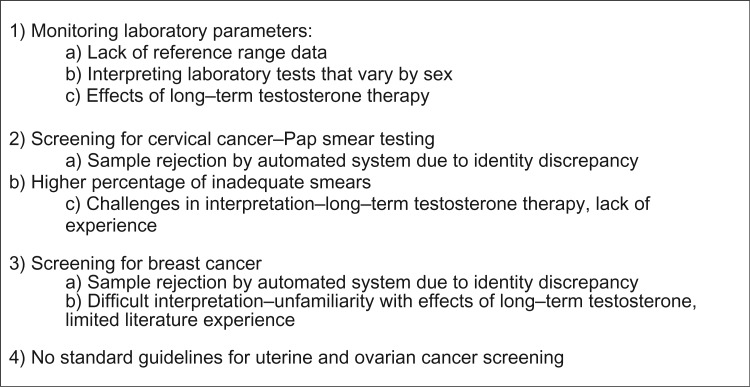
In the realm of anatomic pathology, assessment of Pap smears, prostate biopsies, and breast biopsies from transgender individuals is challenging and prone to misinterpretation. Exogenous hormonal therapy is a key factor that impacts interpretation of these specimens. Even pathology laboratories associated with large medical centers only encounter a small volume of specimens from transgender individuals. In a recent study performed at Fenway Health Center, a large community health care and research facility dedicated to caring for the lesbian, gay, bisexual, and transgender (LGBT) population in the greater Boston, Massachusetts area, the prevalence of Pap smears with inadequate material was found to be 8.3 times higher among transmen compared with other patients. The high unsatisfactory specimen prevalence among transmen was attributed to a combination of physical changes induced by testosterone therapy and possible provider/patient discomfort with the exam.28 The pathology challenges for transwomen and transmen are summarized in Figure 4 and Figure 5, respectively.
Figure 4.
Pathology challenges in transwomen.
Figure 5.
Pathology challenges in transmen.
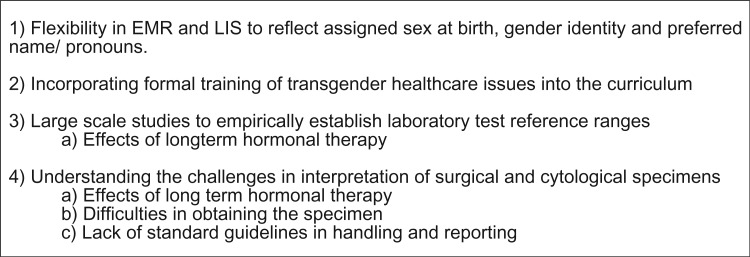
To conclude, despite increasing awareness and decreasing stigmatization of the transgender population, many barriers must be overcome before we can fulfill our long-term goal of achieving the highest standards of care for members of this diverse societal subgroup (Figure 6). EMRs and LISs should allow for designation of assigned sex at birth, gender identity, and preferred name and pronouns. This change will especially aid pathology staff members, such as those in phlebotomy and transfusion medicine, who interface directly with patients. Healthcare facilities should incorporate formal training in transgender health issues and provide inclusive structural facilities, such as unisex restrooms. In laboratory medicine, studies are needed to establish reference ranges for laboratory tests for transwomen and transmen. The results of such studies will likely reveal heterogeneity within the transgender population. In anatomic pathology, personnel should be aware of the complexities in handling and interpreting specimens and biopsies from transgender patients. Ultimately, fulfillment of these goals will allow transgender patients to maximize their overall health, psychological well-being, and self-actualization.
Figure 6.
Future challenges in providing appropriate medical care to transgender patients.
Acknowledgments
We thank Paula Dayton, BA (DeGowin Blood Center, University of Iowa), for her advice on blood donor eligibility issues with the transgender population.
Glossary
Abbreviations
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- ICD
International Statistical Classification of Diseases and Related Health Problems, 10th revision
- HIV
human immunodeficiency virus
- EMRs
electronic medical records
- LISs
laboratory information systems
- WPATH
World Professional Association for Transgender Health
- ACA
Affordable Care Act
- Pap
Papanicolaou
- ACOG
American College of Obstetricians and Gynecologists
- FDA
Food and Drug Administration
- AABB
American Association of Blood Banks
- PSA
prostate-specific antigen
- LGBT
lesbian, gay, bisexual, and transgender
- BMD
bone-mineral density
References
- 1.Institute of Medicine. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington (DC: ): National Institutes of Health; 2011. [PubMed] [Google Scholar]
- 2.Fausto-Sterling A. Sexing the Body. 1st ed New York, NY: Basic Books; 2000. [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington (DC: ): American Psychiatric Publishing; 2013. [Google Scholar]
- 4.Bockting WO, Knudson G, Goldberg JM. Counseling and mental health care for transgender adults and loved ones. Int J Transgend. 2006;9(3-4):35-82. [Google Scholar]
- 5.Bolin A. Transcending and transgendering: male-to-female transsexuals, dichotomy and diversity In Herdt G, editor. Third Sex, Third Gender: Beyond Sexual Dimorphism in Culture and History. New York, NY: Zone Books; 1994. [Google Scholar]
- 6.Rachlin K. Factors which influence individual’s decisions when considering female-to-male genital reconstructive surgery. Int J Transgend . 1999;3(3):1. [Google Scholar]
- 7.Rachlin K, Green J, Lombardi E. Utilization of health care among female-to-male transgender individuals in the United States. J Homosex. 2008;54(3):243-258. [DOI] [PubMed] [Google Scholar]
- 8.Rachlin K, Hansbury G, Pardo ST. Hysterectomy and oophorectomy experiences of female-to-male transgender individuals. Int J Transgend. 2010;12(3):155-166. [Google Scholar]
- 9.Coleman E, Bockting W, Botzer M, et al. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2012;13(4):165-232. [Google Scholar]
- 10.van Kesteren PJ, Gooren LJ, Megens JA. An epidemiological and demographic study of transsexuals in The Netherlands. Arch Sex Behav. 1996;25(6):589-600. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th revision, 4th edn Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 12.Arcelus J, Bouman WP, Van Den Noortgate W, Claes L, Witcomb G, Fernandez-Aranda F. Systematic review and meta-analysis of prevalence studies in transsexualism. Eur Psychiatry. 2015;30(6):807-815. [DOI] [PubMed] [Google Scholar]
- 13.Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: results from a household probability sample of adults. Am J Public Health. 2012;102(1):118-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roberts TK, Fantz CR. Barriers to quality health care for the transgender population. Clin Biochem. 2014;47(10-11):983-987. [DOI] [PubMed] [Google Scholar]
- 15.Grant JM, Mottet LA, Tanis J, Herman JL, Harrison J, Keisling M. National Transgender Discrimination Survey Report on Health and Health Care. Washington, DC: National Center for Transgender Equality and the National Gay and Lesbian Task Force; 2010. [Google Scholar]
- 16.Deutsch MB, Green J, Keatley J, Mayer G, Hastings J, Hall AM, World Professional Association for Transgender Health EMR Working Group. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc. 2013;20(4):700-703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Federal Register. 2015. Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications. https://www.federalregister.gov/articles/2015/10/16/2015-25597/2015-edition-health-information-technology-health-it-certification-criteria-2015-edition-base. Accessed April 25, 2016. [PubMed]
- 18.Olson J, Schrager SM, Clark LF, Dunlap SL, Belzer M. Subcutaneous testosterone: an effective delivery mechanism for masculinizing young transgender men. LGBT Health. 2014;1(3):165-167. [DOI] [PubMed] [Google Scholar]
- 19.Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, et al. Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132-3154. [DOI] [PubMed] [Google Scholar]
- 20.Moore E, Wisniewski A, Dobs A. Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects. J Clin Endocrinol Metab. 2003;88(8):3467-3473. [DOI] [PubMed] [Google Scholar]
- 21.Dizon DS, Tejada-Berges T, Koelliker S, Steinhoff M, Granai CO. Ovarian cancer associated with testosterone supplementation in a female-to-male transsexual patient. Gynecol Obstet Invest. 2006;62(4):226-228. [DOI] [PubMed] [Google Scholar]
- 22.American Association of Blood Banks. Donor history questionnaires. http://www.aabb.org/tm/questionnaires/Pages/default.aspx. Accessed March 13, 2016.
- 23.Food and Drug Administration. Revised recommendations for reducing the risk of human immunodeficiency virus transmission by blood and blood products—questions and answers. http://www.fda.gov/BiologicsBloodVaccines/BloodBloodProducts/QuestionsaboutBlood/ucm108186.htm. Updated January 12, 2015. Accessed March 13, 2016.
- 24.American Association of Blood Banks. FDA Liaison Meeting—January 11, 2012. http://www.aabb.org/advocacy/government/fdaliaison/bloodcomponents/Pages/flm110112.aspx. Accessed March 13, 2016.
- 25.American Red Cross. Eligibility requirements. http://www.redcrossblood.org/donating-blood/eligibility-requirements. Accessed March 13, 2016.
- 26.Roberts TK, Kraft CS, French D, Ji W, Wu AH, Tangpricha V, Fantz CR. Interpreting laboratory results in transgender patients on hormone therapy. Am J Med. 2014;127(2):159-162. [DOI] [PubMed] [Google Scholar]
- 27.Epstein JI. PSA and PAP as immunohistochemical markers in prostate cancer. Urol Clin North Am. 1993;20(4):757-770. [PubMed] [Google Scholar]
- 28.Peitzmeier SM, Reisner SL, Harigopal P, Potter J. Female-to-male patients have high prevalence of unsatisfactory Paps compared to non-transgender females: implications for cervical cancer screening. J Gen Intern Med. 2014;29(5):778-784. [DOI] [PMC free article] [PubMed] [Google Scholar]