Abstract
Background
Public health HIV-service providers, including Medical Case Managers (case managers) and Disease Intervention Specialists (DIS) have a key role to play in identifying and addressing clients' complex mental health needs and substance use which contribute to sexual risk behaviors, yet their understanding and its consensus with HIV-infected men who have sex with men (MSM) have not been well characterized.
Methods
Together with an AIDS Service Organization and the Connecticut State Department of Public Health in 2011–2012, we conducted a focus group of case managers (n = 14) and interviewed DIS (n = 7) and HIV-infected MSM (n = 17) in Connecticut. We used the constant comparison method, grounded theory, and a community-based participatory approach to guide analysis.
Results
We identified three themes characterizing public health HIV-service providers' and MSM's perspectives regarding factors contributing to substance use and sexual risk behaviors in the context of HIV infection: 1) While both MSM and providers described a co-occurrence of HIV, stigma, substance use, and sexual risk behaviors, only MSM identified a causal relationship between these factors; 2) MSM and providers both described varying levels of self-efficacy in readiness to decrease substance use and sexual risk behaviors among MSM; both identified the social network as the key barrier to overcome; 3) Providers described how the co-occurrence of HIV, stigma and sexual risk behaviors leads to multi-faceted client needs for which they lacked sufficient training and collaboration.
Conclusions
Provider education, skills-based training, and interventions targeting social networks may decrease sexual risk behaviors among HIV-infected MSM.
Keywords: Community-based participatory research, Men who have sex with men (MSM), Homosexuality, HIV, Qualitative research, Risk-taking
Highlights
-
•
MSM recognize that HIV diagnosis may trigger substance use and sexual risk behaviors.
-
•
HIV-service providers inconsistently prepared to facilitate behavior change among MSM
-
•
Need social network-based interventions to decrease MSM's risk behaviors
-
•
Provider training on interventions & stages of change theory to address risk behaviors warranted
1. Introduction
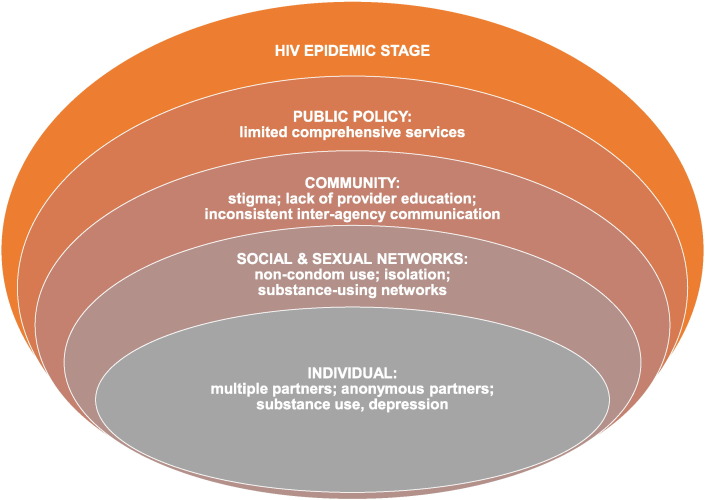
Globally, men who have sex with men (MSM) are disproportionately impacted by HIV (Baral et al., 2007, Baral et al., 2014, Beyrer et al., 2012, Centers for Disease Control and Prevention, 2008a, Centers for Disease Control and Prevention, 2010, Centers for Disease Control and Prevention, 2012) explained, in part, by sexual risk behaviors (Crepaz et al., 2009, Durham et al., 2013, Mattson et al., 2014) in the context of substance use by HIV-infected MSM (Beyrer et al., 2012, Colfax et al., 2004, Mayer et al., 2010, Morin et al., 2005, Weinhardt et al., 2004). While effective behavioral interventions to address sexual risk behaviors among HIV-infected MSM exist (Collins et al., 2010, Crepaz et al., 2014, Johnson et al., 2008), efforts to optimize their implementation are needed. Conceptual models, such as that described by Baral and colleagues (Baral et al., 2013), highlight the importance of considering multi-level factors which contribute to the HIV epidemic and may be addressed in HIV prevention efforts (Fig. 1).
Fig. 1.
Model for Factors Impacting Health and HIV Transmission among HIV-Infected MSM*.
*adapted from Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482.
As they represent both community and individual-levels, understanding perspectives and experiences of HIV service providers and HIV-infected MSM regarding the role of stigma and substance use in sexual risk behaviors represent an important next step. Prior studies have identified suboptimal HIV provider practices and comfort with addressing substance use and sexual risk behaviors (Flickinger et al., 2013, Laws et al., 2011, Metsch et al., 2008, Ray et al., 2013). Few studies examines providers' perceptions of stigma and substance use's role in promoting sexual risk behaviors among HIV-infected MSM, particularly among providers well positioned to intervene: Medical Case Managers (case managers) and Disease Intervention Specialists (DIS), public health authorities who provide partner services (Centers for Disease Control and Prevention, 2008b, Rapp et al., 2014). Despite the complexity surrounding HIV, stigma, and substance use, no studies have incorporated community-based participatory research (CBPR) principles (Cashman et al., 2008, Israel et al., 1998, Minkler, 2005) to address these questions. Through CBPR, members of the community impacted by the issues of concern may be involved in all stages of the research process, including development and framing of the research questions, data collection and analysis, and dissemination. Thus, CBPR promotes development of unique and relevant research questions to the community of interest and optimizes the validity of research findings, particularly those focused on sensitive topics (Cashman et al., 2008, Horowitz et al., 2009).
Therefore, our aims were to characterize the perspectives and experiences regarding the role of stigma and substance use in sexual risk behaviors among HIV-infected MSM, case managers, and DIS, and compare and contrast findings across these groups. We also aimed to identify multi-level opportunities to address substance use and sexual risk behaviors among HIV-infected MSM to ultimately improve their health and enhance HIV prevention efforts.
2. Methods
2.1. Study overview
In 2011, we created Project C.O.A.C.H.: Counseling Others about Contacts and Exposures with HIV, a collaboration between academic researchers, an AIDS-service organization (ASO), and the Connecticut State Department of Public Health (CT DPH) (Cole et al., 2013, Edelman et al., 2013, Edelman et al., 2014). Our approach was grounded in CBPR principles, whereby members of the community affected by the topic under investigation are directly involved in all stages of the project with the goal of translating the findings into action (Agency for Healthcare Research and Quality, 2009, Cashman et al., 2008, Israel et al., 1998, Minkler, 2005). Our research team was diverse in terms of age, gender, race, occupation, sexual orientation and HIV status and included an equitable partnership, involving all partners throughout the research process. We used two qualitative methods to address our research questions: we conducted a focus group with case managers and face-to-face interviews with DIS and HIV-infected MSM (Curry et al., 2009).
2.2. Study design and sampling
To examine perspectives regarding factors contributing to sexual risk behaviors among HIV-infected MSM from multiple perspectives (Curry et al., 2009), we conducted a focus group (Morgan, 1996) with Ryan White-funded medical case managers working in New Haven, CT, a medium-sized urban center who were recruited during a regularly occurring monthly meeting. Next, we completed in-depth in-person interviews (Britten, 1995) with all CT-based DIS, excluding one who was part of the research team. We recruited a purposeful sample (Curry et al., 2009) of MSM until we reached thematic saturation using flyers and face-to-face techniques to achieve a diverse sample, including individuals receiving services from an ASO; a lesbian, gay, bisexual and transgender-focused health center; and an addiction treatment center located in three different cities (Table 1) (Curry et al., 2009). Human Investigation Committees at Yale University School of Medicine and CT State DPH approved the protocol. After receiving an information sheet outlining the study's goals, anticipated risks and benefits and alternatives to participation, all participants provided verbal informed consent and the study was HIPPA compliant. Case managers and DIS were provided a meal and MSM were reimbursed with a $25 gift card for participating.
Table 1.
Public health HIV-service provider characteristics
| Characteristic | Medical case managers, n = 14 | Disease intervention specialists, n = 7 |
|---|---|---|
| Male gender, %(n) | 28% (4) | 43% (3) |
| Age, years, mean (SD)a | 40 (12) | 49 (9) |
| Race, %(n) | ||
| White | 71% (10) | 43% (3) |
| Black | 29% (4) | 57% (4) |
| Ethnicity, %(n) | ||
| Hispanic | 21% (3) | 14% (1) |
| Education, %(n) | ||
| Bachelor's Degree and/or post-graduate Studies |
79% (11) | 71% (5) |
| Years employed in current role, mean (SD) | 5 (5) | 15 (6) |
| Location of employment, % (n) | ||
| Hospital-based clinic | 14% (2) | n/a |
| Community health center | 14% (2) | n/a |
| Community-based organization | 78% (11) | n/a |
| Average weekly case load , mean (SD) | 31 (19) | 11 (5) |
Notes: SD = standard deviation
2.3. Data collection
The focus group and interview guides were developed by those with academic expertise and with lived experience in HIV, partner notification, MSM, social services, qualitative research and CBPR. The case managers participated in a focus group, which was led by one research team member, the Executive Director (ED) of the partnering ASO (CC), with co-facilitation by a health care provider with training in HIV clinical care and health services research (EJE). We chose to use a focus group for data collection with the case managers given feasibility and with the expectation that the group dynamic would help generate unique insights about shared experiences (Curry et al., 2009). The DIS and MSM each participated in face-to-face, in-depth interviews; we chose to use in-depth interviews due privacy concerns and our goal of eliciting data on individual experiences (Curry et al., 2009). We sought to optimize data validity by matching characteristics of study participants and research team members based on, sexual orientation and HIV status. Thus, interviews of the DIS were conducted by the health care provider (EJE) and those of MSM by the ASO's ED (CC) (Adamson and Donovan, 2002, Cashman et al., 2008, Curry et al., 2009, Rhodes, 1994). Both of these individuals (EJE and CC) participated in an in-person training session on qualitative data collection prior to initiating data collection and received ongoing supervision and feedback during the data collection phase by the team's qualitative expert (MSR) (Rosenthal et al., 2009). The focus group and interviews were conducted between January 2011 and March 2012, using “grand tour” questions (i.e. open ended questions intended to stimulate discussion) followed by “probes” (i.e. prompts) (Box 1) (Edelman et al., 2014) after the interviewers introduced themselves and stated their professional roles (if not already known by the participant). These guides were piloted and refined prior to use with the study participants (Edelman et al., 2014). All participants completed a brief demographic survey. The focus group and interviews were audio-taped, professionally transcribed, reviewed for accuracy, and identifying information was removed prior to analysis (Curry et al., 2009). The focus group lasted approximately two hours, while each interview was approximately one hour in duration.
Box 1.
Example focus group and interview guide grand tour questions
| Providers (medical case managers and disease intervention specialists) |
|
| Clients (men who have sex with men) |
|
Alt-text: Box 1
2.4. Analysis
Our three-person multidisciplinary analysis team adhered to CBPR principles by including research team members with expertise that was both academic and lived, including the two interviewers (CC and EJE) and a health services researcher with CBPR and qualitative methods expertise (MSR) (Rosenthal et al., 2009). These three individuals, who were most directly involved with the data collection and analysis, did not have regular interaction with the study participants. Some of the participating MCMs and clients, however, were employed or received services at the ASO where CC was the ED (Cole et al., 2013). We used the constant comparative method and grounded theory, in which our code structure and subsequent themes were generated iteratively based on participants' quotes (Curry et al., 2009). To organize data and facilitate retrieval, we used qualitative analysis software (AtlasTi version 6.2, Berlin, Germany) and selected quotations from codes relating to sexual risk behaviors, as well as stigma and substance use.
2.5. Development of recommendations
Consistent with CBPR (Horowitz et al., 2009), we aimed to translate our research findings into action. We thus developed our dissemination plan and recommendations iteratively and in collaboration with various stakeholders. A summary of recommendations relevant to this analysis are presented in the results.
3. Results
All participants who consented, completed the study. For this analysis, we only included those MSM who were HIV-infected. Our analytic sample included 14 case managers, 7 DIS and 17 HIV-infected MSM (Table 2, Table 3). Case managers were predominantly white (71%), non-Hispanic (79%) women (72%), with a mean age of 40 years. DIS were mostly black (57%), non-Hispanic (86%) women (57%) with a mean age of 49 years. Case managers had been in their current role for a mean of 5 years and had average weekly case load of 31 clients; DIS, in contrast, had been in their role for a mean of 15 years and had an average weekly case load of 11 clients. The MSM were predominantly black (76%), non-Hispanic (82%) had a mean age of 46 years and had been diagnosed with HIV a median of 15 years prior to the study.
Table 2.
Client (HIV-infected MSM) Characteristics
| Characteristic | MSM, n = 17 |
|---|---|
| Male gender, % (n) | 100 (17) |
| Age, years, mean (SD) | 46 (7) |
| Race, % (n) | |
| White | 24 (4) |
| Black | 76 (13) |
| Ethnicity, % (n) | |
| Hispanic | 18 (3) |
| Education, % (n) | |
| Some high school | 24 (4) |
| High school graduate or GED | 41 (7) |
| Some college, associate's or technical degree | 18 (3) |
| College graduate | 6 (1) |
| Any post-graduate studies | 12 (2) |
| Sexual Identity, % (n) | |
| Heterosexual | 6 (1) |
| Homosexual or gay | 71 (12) |
| Bisexual | 24 (4) |
| Years diagnosed with HIV, median (range) | 15 (3–30) |
Notes: age data was missing for 4 participants; race data was missing for 1 participant; SD = standard deviation
Table 3.
Improving Case Managers and DIS Effectiveness to Address Stigma, Substance Use and Sexual Risk Behaviors
| Identified Barrier | Recommendation |
|---|---|
| Variable understanding and skills at addressing both sexual risk behaviors and substance use | Provider training on effective behavioral interventions for sexual risk reduction and substance use |
| Complex social, mental health and medical client needs | Multi-pronged and comprehensive treatment approaches |
| Unhealthy social networks | Peer- and network-based interventions to promote new social networks and interventions designed to reduce stigma and change social norms surrounding substance use within existing social networks |
| Inconsistent communication across organizations | Multi-disciplinary, cross-institutional quarterly meetings |
| Variable provider adoption of stages of change model to behavior change | Provider training to apply stages of change theory to promoting change in substance use and sexual risk behaviors |
We identified three themes characterizing public health HIV-service providers' and MSM's perspectives regarding factors contributing to sexual risk behaviors in the context of HIV infection: 1) While both MSM and providers described a co-occurrence of HIV, stigma, substance use and sexual risk behaviors, only MSM identified a causal relationship between these factors; 2) both MSM and providers described varying levels of self-efficacy in readiness to decrease substance use and sexual risk behaviors among MSM; both identified the social network as the key barrier to overcome; 3) providers described how the co-occurrence of HIV, stigma and sexual risk behaviors leads to multi-faceted client needs for which they lacked sufficient training and collaboration (Fig. 1).
3.1. Theme 1: While both MSM and providers described a co-occurrence of HIV, stigma, substance use and sexual risk behaviors, only MSM identified a causal relationship between these factors
Providers described co-existence of stigma, substance use and sexual risk behaviors, but did not identify the causal link between these factors. MSM, in contrast, described substance use as a coping strategy for managing their HIV diagnosis, self-perceived stigma, and depression; they described substance use as a way to facilitate social connectedness, through sexual risk behaviors and otherwise.
This provider reflected on the social connectedness garnered from substance use among HIV-infected individuals but did not link this to behaviors that might lead to HIV:
A lot of them [HIV-infected individuals with substance use] find, aside from the support system that they get from different agencies, they are alone. Once they make that decision [to stop their substance use], really aside from agencies that are willing to help them, they don't have those family members or friends… they figure, “If I make the change, hey, I'm alone.”
- Case Manager
On the other hand, this MSM explicitly linked his HIV diagnosis to suicidality, social isolation, and subsequent substance use:
I've always thought about [suicide]. Always thinking of a way to do it… I'm scared to do anything because I'd rather be here and try to deal with it. And my way of dealing with it is isolate myself, just stay to myself. And that's what I've meant to do after the shock of finding out I have HIV. I start[ed] isolating myself. . . I think that's when my alcohol problem and drug problem accelerated.
-MSM
Also making an argument for causation, this MSM described how his HIV diagnosis increased his need for external validation through substance use and sex:
I think that because I knew that I had AIDS, I was HIV +, I thought that maybe someone could look at me and tell, from the outside, so I had to make myself feel, like, desirable, in a flipped crazy way, and part of doing that was that I had to make sure that I was drunk before I even went out. . . Once I found out I was HIV, that made me, believe it or not, even more reckless. . . It made me even more sexually reckless and sexually irresponsible than I had ever been in my entire life.
-MSM
3.2. Theme 2: MSM and providers both described varying levels of self-efficacy in readiness to decrease substance use and sexual risk behaviors among MSM; both identified the social network as the key barrier to overcome.
For example, this provider described how, for a client who was contemplating stopping using substances, the social environment and potential social isolation were barriers:
Or the issue of wanting to do it [stop using substances], but not having the supportive network from where they're from, because they might be the first ones to step out and try to do something different. And then they'll get the discouragement of, “Well why you trying to do that? Who you trying to become? You think you're better than us now?” . . . And then that fear of failure.
-Case Manager
On the other hand, this MSM described his self-efficacy as he reported how maintenance of his recovery was dependent on avoiding his previous social network:
I only been infected with HIV for 5–4 years? 3, 4, 5 years? And I think about it sometime because I get depressed about it. . . and sometimes I want to get out there and just go start using drugs. . .but it's just being around certain people. . . So I'm trying to stay away from them.
-MSM
This provider described a self-efficacy and commitment to getting his client out of his social environment and into treatment:
I had a client it took me days to get him into help [with his substance use]. We went got his medicine – it was like 6 months since he took his medicine. See, I'm not going to give up on them. If I got to take him 60 times. . . . I try to get them away from their neighborhood. . . just to move him away from that area because it's a trigger to them. Anybody who uses drugs, it's a trigger. . .
-Case Manager
3.3. Theme 3: Providers described how the co-occurrence of HIV, stigma and sexual risk behaviors leads to multi-faceted client needs for which they lacked sufficient training and collaboration.
Providers described how by considering the multiple factors that inform a client's readiness to change sexual risk behaviors, providers may be better positioned to effect change.
This provider described how, in order to facilitate change, it is important to assess a client's comprehensive needs:
We try to remember that they might come in for one thing, but what they need is something else. We might be making referrals to … comprehensive risk counseling services, if they're high risk behavior, and they've got all kinds of issues, maybe they're suicidal, maybe not, but maybe they're so depressed, their self-esteem is really lousy…
-DIS
This provider described how a lack of training in the multi-faceted problems of clients, specifically substance use and sexual risk behaviors, may lead providers to misunderstand MSM and their sexual risk behaviors; accordingly, this provider advocated for training in substance use:
I think with the frustration that we get from a bad interview [to discuss partners], if we can understand why they're doing different things, I think it would kind of relieve us a little bit as to maybe they're just not ready. . . we can be taught in a sense to understand that it's not personal, and that this person can't stop doing drugs, that's why he has unprotected sex, or, and stuff like that. We haven't really done [any trainings regarding drug use].
-DIS
This provider described how a “dually diagnosed” client, one with substance use and mental health issues, can create an especially frustrating situation when there is lack of collaboration among case managers and clinicians:
I don't know if that colleague on the other side, when they're getting ready to discharge, are they going to call me? Even though you ask, "Please call me so we can work on a plan to get him into inpatient," it doesn't always work. So when they are dually diagnosed, those are the more complicated.
-Case Manager
3.4. Actionable items for improving case managers and DIS effectiveness at addressing stigma, substance use and sexual risk behaviors
In response to the themes and ideas that emerged, we list specific recommendations for action (Table 3). These recommendations are likely to involve multi-step processes with ongoing evaluation and refinement.
4. Discussion
In this qualitative study of three key groups — MSM, case managers and DIS — we found that HIV-infected MSM perceived stigma, isolation, and substance use as critical factors contributing to sexual risk behaviors. Yet many HIV-service providers, while acknowledging the co-occurrence of these factors, did not perceive that the factors were both causal of sexual risk behaviors and a response to a HIV diagnosis. Both HIV-infected MSM and providers described varying levels of efficacy among HIV-infected MSM to change their substance use and sexual risk behaviors and viewed the MSM's social network as a barrier to achieving change. Finally, our study found that providers described the importance of training and inter-professional collaboration designed to address multi-faceted clients' needs. To our knowledge, prior studies have neither applied qualitative methods with CBPR principles to examine factors contributing to sexual risk behaviors among HIV-infected MSM nor, despite their unique position to facilitate treatment, examined the perspectives of case managers or DIS. Our findings demonstrate opportunities for addressing the needs of HIV-infected MSM across multiple levels (Fig. 1).
Our finding that sexual risk behaviors occurs in the context of complex negative psychosocial experiences is consistent with prior work (Herrick et al., 2013, Mosack et al., 2005, Stall et al., 2003, Wade Taylor et al., 2013). Our findings extend these data by demonstrating that providers inconsistently described how substance use and sexual risk behaviors may be a coping mechanism for feelings of stigma, social isolation and depression in response to living with HIV. This identified gap in understanding may serve as a place in which to begin training for providers. Further, while previous literature demonstrates that knowledge of an HIV diagnosis is associated with decreased risk behaviors (Marks et al., 2005), our study provides evidence that the initial period after diagnosis may warrant special attention.
In addition, our study demonstrates the relevance of the Stages of Change model (Prochaska et al., 1992), for addressing substance use and sexual risk behaviors. Stages of change research demonstrates that to understand where on a cycle the client is, and to understand the work it might take to get them to the next step in the cycle, relieves the provider of a sense of helplessness and facilitates movement along the curve and are likely to be more successful (Prochaska et al., 1992). Training public health HIV-service providers in Stages of Change may facilitate their work with the complicated lives of HIV-infected MSM by giving them a greater understanding of the difficulties of behavior change, which may, in turn, reduce their judgment of clients and optimize their level of engagement with challenging clients.
Importantly, providers identified existing social networks as a key barrier to behavior change. While social networks may serve as a buffer to perceived stigma and other stress related to being of a marginalized group (e.g. MSM, HIV-infected) (Wong et al., 2014), social network structures may play a key role in normalizing substance use and sexual risk behaviors (Latkin et al., 2010). Existing data demonstrating efficacy of social network-based interventions for addressing behavior change (Hoffman et al., 2013, Tobin et al., 2011), provide support for use of such interventions to target substance use and sexual risk behaviors among HIV-infected MSM (Tieu et al., 2015).
Among participating providers, we found variability in self-perceived skills for addressing substance use and sexual risk behaviors and promoting behavior change. While one provider articulated the necessity of matching their approach to the client's needs — acknowledging a key principle to promoting effective behavior change (Pearson et al., 2012) – others appeared less well prepared. A recent meta-analysis indicates that case management is effective at promoting increased linkage and retention in substance abuse treatment services, but that it does not lead to substantial improvements in substance use, physical and mental health and risk behaviors. Our findings that providers were variable in their knowledge and self-efficacy in comprehensively managing HIV-infected MSM may, in part, explain these findings (Rapp et al., 2014). Furthermore, given ongoing initiatives to expand the role of DIS to promote retention in care of HIV-infected individuals (Centers for Disease Control and Prevention, 2013), efforts to promote more comprehensive training around issues such as substance use are likely to become increasingly relevant. Our data indicate that provider trainings on complexities involved in sexual risk behaviors and how to deliver effective behavioral interventions are warranted (Johnson et al., 2008, Sullivan et al., 2011). Additional community and network-focused opportunities for addressing substance use and sexual risk behaviors among HIV-infected MSM emerged from our data (Table 3). It will be important that any provider-focused initiatives, however, consider variability in case loads, experience, training, and staff turnover given existing differences among case managers and DIS.
Our study has limitations. Participants were recruited from three metropolitan areas within a single state. That we employed rigorous qualitative methods using CBPR-principles improves the likelihood that these findings may apply to other medium-sized metropolitan areas (Cashman et al., 2008). The majority of MSM in our sample had been living with HIV for a median of 15 years and were engaged in services, which may not reflect perspectives of individuals newly diagnosed or not in care. Lastly, we did not routinely document field notes or review transcripts or a summary of these findings with study participants (i.e. participant confirmation) from this analysis as it was not feasible. We were otherwise consistent with the consolidated criteria for reporting qualitative research (COREQ) guidelines and believe that the multi-disciplinary nature of our research team optimizes the validity of our reported findings (Edelman et al., 2014).
4.1. Conclusions
Perspectives among HIV-infected MSM, case managers and DIS on the causal relationships leading to HIV-risk behaviors differ, yet there is recognition of a need to meet multi-faceted needs through increased training and collaboration. Strategies to optimize how case managers and DIS understand and intervene upon stigma, substance use and sexual risk behaviors among HIV-infected MSM has potential to help prevent ongoing HIV transmission.
Disclosures
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Yale Center for Clinical Investigation, the Department of Veterans Affairs, the Connecticut State Department of Public Health, or the National Institute on Drug Abuse. An earlier version of this work was presented as an oral abstract at the 38th National Annual Association for Medical Education and Research in Substance Abuse, November 6th, 2014, San Francisco, CA.
Conflicts of interest
The authors have no conflicts of interest to disclose.
Acknowledgements
Sources of support: This work was generously supported by the Yale Center for Clinical Investigation, Yale School of Medicine (UL1 TR000142). Dr. Edelman was supported by the Robert Wood Johnson Clinical Scholars Foundation, the United States Department of Veteran Affairs and the Yale-Drug Abuse, Addiction, and HIV Research Scholars Program (K12DA033312-01A1) during the conduct of this work. The funders of this work had no role in the study design, collection analysis or interpretation of data or the decision to submit this report for publication.
References
- Adamson J., Donovan J.L. Research in black and white. Qual. Health Res. 2002;12:816–825. doi: 10.1177/10432302012006008. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality . Rockville; MD: 2009. AHRQ Activities Using Community-Based Participatory Research to Address Healthcare Disparities. [Google Scholar]
- Baral S., Sifakis F., Cleghorn F., Beyrer C. Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med. 2007;4 doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S., Logie C.H., Grosso A., Wirtz A.L., Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S.D., Grosso A., Holland C., Papworth E. The epidemiology of HIV among men who have sex with men in countries with generalized HIV epidemics. Curr. Opin. HIV AIDS. 2014;9:156–167. doi: 10.1097/COH.0000000000000037. [DOI] [PubMed] [Google Scholar]
- Beyrer C., Baral S.D., van Griensven F. Global epidemiology of HIV infection in men who have sex with men. Lancet. 2012;380:367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britten N. Qualitative interviews in medical research. BMJ. 1995;311:251–253. doi: 10.1136/bmj.311.6999.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cashman S.B., Adeky S., Allen A.J., 3rd The power and the promise: working with communities to analyze data, interpret findings, and get to outcomes. Am. J. Public Health. 2008;98:1407–1417. doi: 10.2105/AJPH.2007.113571. (AJPH.2007.113571 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention HIV prevalence estimates–United States, 2006. MMWR Morb. Mortal. Wkly Rep. 2008;57:1073–1076. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Recommendations for partner services programs for HIV infection, syphilis, gonorrhea, and chlamydial infection. MMWR Recomm. Rep. 2008;57:1–83. (quiz CE81-84) [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Prevalence and awareness of HIV infection among men who have sex with men — 21 cities, United States, 2008. MMWR Morb. Mortal. Wkly Rep. 2010;59:1201–1207. (mm5937a2 [pii]) [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2012. Estimated HIV incidence in the United States, 2007–2010. Atlanta, Georgia. [Google Scholar]
- Centers for Disease Control and Prevention STD/HIV Disease Intervention Services Training Centers (DISTC): funding opportunity announcement. 2013. http://www.cdc.gov/std/foa/distc/default.htm (accessed on June 12 2014 >)
- Cole C.A., Edelman E.J., Boshnack N., Jenkins H., Richardson W., Rosenthal M.S. Time, dual roles, and departments of public health: lessons learned in CBPR by an AIDS service organization. Prog. Community Health Partnersh. 2013;7:323–330. doi: 10.1353/cpr.2013.0034. (S1557055X13300126 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colfax G., Vittinghoff E., Husnik M.J. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am. J. Epidemiol. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Collins C.B., Jr., Hearn K.D., Whittier D.N., Freeman A., Stallworth J.D., Phields M. Implementing packaged HIV-prevention interventions for HIV-positive individuals: considerations for clinic-based and community-based interventions. Public Health Rep. 2010;125(Suppl. 1):55–63. doi: 10.1177/00333549101250S108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N., Marks G., Liau A. Prevalence of unprotected anal intercourse among HIV-diagnosed MSM in the United States: a meta-analysis. AIDS. 2009;23:1617–1629. doi: 10.1097/QAD.0b013e32832effae. [DOI] [PubMed] [Google Scholar]
- Crepaz N., Tungol-Ashmon M.V., Higa D.H. A systematic review of interventions for reducing HIV risk behaviors among people living with HIV in the United States, 1988–2012. AIDS. 2014;28:633–656. doi: 10.1097/QAD.0000000000000108. (00002030-201403130-00002 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry L.A., Nembhard I.M., Bradley E.H. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- Durham M.D., Buchacz K., Richardson J. Sexual risk behavior and viremia among men who have sex with men in the HIV Outpatient Study, United States, 2007–2010. J. Acquir. Immune Defic. Syndr. 2013;63:372–378. doi: 10.1097/QAI.0b013e31828c20d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman E.J., Cole C.A., Boshnack N., Jenkins H., Richardson W., Rosenthal M.S. Promoting HIV testing among partners of HIV-positive clients. 2013. http://www.ces4health.info/find-products/view-product.aspx?code=C6NX2HTH (accessed on 3/14/2013 2013 >)
- Edelman E.J., Cole C.A., Richardson W., Boshnack N., Jenkins H., Rosenthal M.S. Opportunities for improving partner notification for HIV: results from a community-based participatory research study. AIDS Behav. 2014;18:1888–1897. doi: 10.1007/s10461-013-0692-9. [DOI] [PubMed] [Google Scholar]
- Flickinger T.E., Berry S., Korthuis P.T. Counseling to reduce high-risk sexual behavior in HIV care: a multi-center, direct observation study. AIDS Patient Care STDs. 2013;27:416–424. doi: 10.1089/apc.2012.0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick A.L., Lim S.H., Plankey M.W. Adversity and syndemic production among men participating in the multicenter AIDS cohort study: a life-course approach. Am. J. Public Health. 2013;103:79–85. doi: 10.2105/AJPH.2012.300810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman I.F., Latkin C.A., Kukhareva P.V. A peer-educator network HIV prevention intervention among injection drug users: results of a randomized controlled trial in St. Petersburg, Russia. AIDS Behav. 2013;17:2510–2520. doi: 10.1007/s10461-013-0563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz C.R., Robinson M., Seifer S. Community-based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009;119:2633–2642. doi: 10.1161/CIRCULATIONAHA.107.729863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel B.A., Schulz A.J., Parker E.A., Becker A.B. Review of community-based research: assessing partnership approaches to improve public health. Annu. Rev. Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- Johnson W.D., Diaz R.M., Flanders W.D. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst. Rev. 2008 doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- Latkin C.A., Kuramoto S.J., Davey-Rothwell M.A., Tobin K.E. Social norms, social networks, and HIV risk behavior among injection drug users. AIDS Behav. 2010;14:1159–1168. doi: 10.1007/s10461-009-9576-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laws M.B., Bradshaw Y.S., Safren S.A. Discussion of sexual risk behavior in HIV care is infrequent and appears ineffectual: a mixed methods study. AIDS Behav. 2011;15:812–822. doi: 10.1007/s10461-010-9844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks G., Crepaz N., Senterfitt J.W., Janssen R.S. Meta-analysis of high-risk sexual behavior in persons aware and unaware they are infected with HIV in the United States: implications for HIV prevention programs. J. Acquir. Immune Defic. Syndr. 2005;39:446–453. doi: 10.1097/01.qai.0000151079.33935.79. [DOI] [PubMed] [Google Scholar]
- Mattson C.L., Freedman M., Fagan J.L. Sexual risk behaviour and viral suppression among HIV-infected adults receiving medical care in the United States. AIDS. 2014;28:1203–1211. doi: 10.1097/QAD.0000000000000273. (00002030-201405150-00013 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer K.H., O'Cleirigh C., Skeer M. Which HIV-infected men who have sex with men in care are engaging in risky sex and acquiring sexually transmitted infections: findings from a Boston community health centre. Sex. Transm. Infect. 2010;86:66–70. doi: 10.1136/sti.2009.036608. (sti.2009.036608 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metsch L.R., Pereyra M., Colfax G. HIV-positive patients' discussion of alcohol use with their HIV primary care providers. Drug Alcohol Depend. 2008;95:37–44. doi: 10.1016/j.drugalcdep.2007.12.006. [DOI] [PubMed] [Google Scholar]
- Minkler M. Community-based research partnerships: challenges and opportunities. J. Urban Health. 2005;82 doi: 10.1093/jurban/jti034. (ii3-12. jti034 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D.L. Focus Groups. Annu. Rev. Sociol. 1996;22:129–152. [Google Scholar]
- Morin S.F., Steward W.T., Charlebois E.D. Predicting HIV transmission risk among HIV-infected men who have sex with men: findings from the healthy living project. J. Acquir. Immune Defic. Syndr. 2005;40:226–235. doi: 10.1097/01.qai.0000166375.16222.eb. (00126334-200510010-00016 [pii]) [DOI] [PubMed] [Google Scholar]
- Mosack K.E., Abbott M., Singer M., Weeks M.R., Rohena L. If I didn't have HIV, I'd be dead now: illness narratives of drug users living with HIV/AIDS. Qual. Health Res. 2005;15 doi: 10.1177/1049732304271749. (586-605. 15/5/586 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson F.S., Prendergast M.L., Podus D., Vazan P., Greenwell L., Hamilton Z. Meta-analyses of seven of the National Institute on Drug Abuse's principles of drug addiction treatment. J. Subst. Abus. Treat. 2012;43:1–11. doi: 10.1016/j.jsat.2011.10.005. (S0740-5472(11)00208-X [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J.O., DiClemente C.C., Norcross J.C. In search of how people change. Applications to addictive behaviors. Am. Psychol. 1992;47:1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Rapp R.C., Van Den Noortgate W., Broekaert E., Vanderplasschen W. The efficacy of case management with persons who have substance abuse problems: A three-level meta-analysis of outcomes. J. Consult. Clin. Psychol. 2014 doi: 10.1037/a0036750. (2014-16730-001 [pii]) [DOI] [PubMed] [Google Scholar]
- Ray M.K., Beach M.C., Nicolaidis C., Choi D., Saha S., Korthuis P.T. Patient and provider comfort discussing substance use. Fam. Med. 2013;45:109–117. [PMC free article] [PubMed] [Google Scholar]
- Rhodes P.J. Race-of-Interviewer Effects - a Brief Comment. Sociology. 1994;28:547–558. [Google Scholar]
- Rosenthal M.S., Lucas G.I., Tinney B. Teaching community-based participatory research principles to physicians enrolled in a health services research fellowship. Acad. Med. 2009;84:478–484. doi: 10.1097/ACM.0b013e31819a89e8. (00001888-200904000-00022 [pii]) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R., Mills T.C., Williamson J. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am. J. Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan L.E., Tetrault J.M., Braithwaite R.S., Turner B.J., Fiellin D.A. A Meta-analysis of the Efficacy of Nonphysician Brief Interventions for Unhealthy Alcohol Use: Implications for the Patient-Centered Medical Home. Am. J. Addict. 2011;20:343–356. doi: 10.1111/j.1521-0391.2011.00143.x. [DOI] [PubMed] [Google Scholar]
- Tieu H.V., Liu T.Y., Hussen S. Sexual Networks and HIV Risk among Black Men Who Have Sex with Men in 6 U.S. Cities. PLoS One. 2015;10 doi: 10.1371/journal.pone.0134085. (Hptn) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin K.E., Kuramoto S.J., Davey-Rothwell M.A., Latkin C.A. The STEP into Action study: a peer-based, personal risk network-focused HIV prevention intervention with injection drug users in Baltimore, Maryland. Addiction. 2011;106:366–375. doi: 10.1111/j.1360-0443.2010.03146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade Taylor S., O'Cleirigh C., Mayer K.H., Safren S.A. HIV-infected men who have sex with men who engage in very high levels of transmission risk behaviors: establishing a context for novel prevention interventions. Psychol. Health Med. 2013;18:576–587. doi: 10.1080/13548506.2012.756537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhardt L.S., Kelly J.A., Brondino M.J. HIV transmission risk behavior among men and women living with HIV in 4 cities in the United States. J. Acquir. Immune Defic. Syndr. 2004;36:1057–1066. doi: 10.1097/00126334-200408150-00009. (00126334-200408150-00009 [pii]) [DOI] [PubMed] [Google Scholar]
- Wong C.F., Schrager S.M., Holloway I.W., Meyer I.H., Kipke M.D. Minority stress experiences and psychological well-being: the impact of support from and connection to social networks within the Los Angeles House and Ball communities. Prev. Sci.: Off. J.Soc. Prev. Res. 2014;15:44–55. doi: 10.1007/s11121-012-0348-4. [DOI] [PMC free article] [PubMed] [Google Scholar]