Abstract
Objectives
Several studies identified a heterogeneous impact of heat on mortality in hot and cool regions during a fixed period, whereas less evidence is available for changes in risk over time due to climate change in these regions. We compared changes in risk during periods without (1996–2000) and with (2008–2012) heatwave warning forecasts in regions of South Korea with different climates.
Methods
Study areas were categorised into 3 clusters based on the spatial clustering of cooling degree days in the period 1993–2012: hottest cluster (cluster H), moderate cluster (cluster M) and cool cluster (cluster C). The risk was estimated according to increases in the daily all-cause, cardiovascular and respiratory mortality per 1°C change in daily temperature above the threshold, using a generalised additive model.
Results
The risk of all types of mortality increased in cluster H in 2008–2012, compared with 1996–2000, whereas the risks in all-combined regions and cooler clusters decreased. Temporal increases in mortality risk were larger for some vulnerable subgroups, including younger adults (<75 years), those with a lower education and blue-collar workers, in cluster H as well as all-combined regions. Different patterns of risk change among clusters might be attributable to large increases in heatwave frequency or duration during study periods and the degree of urbanisation in cluster H.
Conclusions
People living in hotter regions or with a lower socioeconomic status are at higher risk following an increasing trend of heat-related mortality risks. Continuous efforts are needed to understand factors which affect changes in heat-related mortality risks.
Keywords: EPIDEMIOLOGY, PUBLIC HEALTH, OCCUPATIONAL & INDUSTRIAL MEDICINE
Strengths and limitations of this study.
We examined the impact of heat on mortality using data which cover the whole country.
Target study regions were defined by statistically meaningful differences in climate characteristics using spatial statistics.
We compared heat-related mortality between before and after introduction of the heatwave early warning system.
We examined patterns of temporal changes in heat-related mortality risks among regions with different climate characteristics and found that risk changes are affected by regional climate.
Adjustment for air pollutants was available for limited periods but this did not affect the accuracy of risk estimation.
Introduction
An increase in environmental temperature is significantly related to daily excess mortality. Many studies have found that high temperatures are associated with all-cause mortality, as well as mortality caused by non-communicable diseases such as cardiovascular and respiratory diseases.1 The Intergovernmental Panel on Climate Change (IPCC) reported that climate change will most likely lead to further increases in air temperature and the intensity of heatwave events.2 3 This could increase the heat-related mortality risk in future. Scientists anticipate that future risks will be greater in populations identified as more vulnerable to heat-related health damage through epidemiological studies, including elderly individuals with impaired physiological ability and people with underlying chronic diseases or a low socioeconomic status.1 4 5
The heat–mortality relationship varies among populations according to climate and geographical region.6 The ‘threshold temperature’, at which the mortality risk begins to increase, is typically higher in regions where hot weather is more common in the continental USA (eg, southern latitudes in the USA).7 The threshold and risk of heat-related mortality also vary significantly even among cities within a smaller country because of differences in the intensity of summer heat; cities with hotter climates tended to have higher thresholds and lower risks, with considerably wide variance in risk noted among cities.8–13 These findings suggest that populations experiencing higher heat exposure are better able to cope with heat stress.14 15 However, studies usually focused on comparisons of the heat-related mortality risk during a short-term period among regions with different climates, except one study13 that considered temporal changes in risk over time; as a result, far less information is available about future trends in the differences in risk according to climate.
In this sense, the present study aimed to compare changes in heat-related mortality risks over time among South Korean regions with different climate characteristics in the summer. The significant impact of heat on mortality in major cities has been demonstrated in many Korean studies.16–18 One study examined temporal changes in the effect of heat over time, albeit for one city.18 This study categorised study areas across the entire country into three clusters based on the degree of heat, using cooling degree days (CDD), a concept that was adopted in a previous study to classify summer temperature in the USA.19 Temporal changes in heat-related mortality risk were assessed during periods with (2008–2012) and without (1996–2000) a national heatwave early warning system for each cluster. The Korea Meteorological Administration (KMA) has announced heatwave early forecast during summer (June to September) since 2008. Once a heatwave is forecast, a series of actions is implemented to prevent negative heat-related health outcomes including activating an emergency text message service, opening shade shelters and monitoring the occurrence of heat-related illness. Heat-related mortality risk was estimated in terms of increases in the daily all-cause, cardiovascular and respiratory mortality by change in the daily temperature. The analysis was further stratified by age group, education level and job status. South Korea has experienced rapid climate change, as evidenced by the more rapid and greater temperature increases in this country relative to global trends throughout the past two decades.20 Therefore, a comparison of patterns in risk change during these recent decades will provide insight into climate-modified changes in risk over time. We expect that the results of this study will provide basic information that will help to identify populations vulnerable to heat effect and public health policy decision-making to combat heat-related health damage.
Materials and methods
Study area
South Korea, a country in East Asia, is located at middle latitude (37° North and 127.30° East) in a temperate climate zone. South Korea has four distinctive seasons with the coolest weather in the winter (December to February) and the hottest weather in summer (June to September). Temperature is highest in July and August. All equivalent administrative units, including cities, counties and boroughs, in South Korea were considered. To analyse temporal changes in the heat–mortality relationship, we sought study periods of equal duration and with similar annual nationwide temperature trends and two subperiods were selected: 1996–2000 and 2008–2012. This was because years with relatively lower temperature ranges between 2001 and 2007 (as much as 10% lower than that in other years) could affect accurate estimation of the effect of temperature when the same threshold was applied to the study periods for an equal analytic environment.
Data
Mortality data, coded by age, sex, address, job status, educational level and cause of death (according to the International Classification of Disease, Injuries and Causes of Death, 10th version (ICD-10)), from 1996 to 2012 were collected from the Korean National Statistical Office. Total deaths, except for deaths caused by accidents (V00–Y99), were used to calculate daily all-cause mortality. Cardiovascular (I00–I99) and respiratory diseases (J00–J99) were defined as target diseases. The daily number of overall deaths, stratified by age group (<20, 20–74 and ≥75 years), was examined. The incidences of cardiovascular and respiratory disease in the <20 years group were not used for risk estimation, as the incidence was too small. Population data at the yearly midpoint were obtained from the Korean National Statistical Office. White-collar and blue-collar workers were defined on the basis of the Korea Standard Classification for Occupations used in national mortality data to identify people who were most likely outdoor workers. Among standard job classes, white-collar workers comprised people employed in management, office, scientific and service occupations. People involved in agriculture, crafts and related activities, machine manipulation, and simple manual labour were defined as blue-collar workers.
Temperature, humidity, precipitation and barometric pressure data, recorded every 3 hours, were obtained from meteorological stations affiliated with the KMA. Using these data, we calculated the daily mean and maximum temperatures, mean humidity and mean barometric pressure. To evaluate the temperature conditions during the summer, the study considered the occurrence of heatwave events.
Features of heatwave were measured to identify the impact of regional climate on the degree of heat. A heatwave was defined according to the criteria of the KMA which operates the heatwave early warning system; days with a daily maximum temperature >33°C for more than 2 days were defined as days with a heatwave. Heatwave duration was calculated as the number of consecutive days of heatwave. Heatwave frequency was the calculated number of occurrences of heatwaves during summer. Heatwave intensity refers to the cumulative sum of differences between the daily maximum temperature and the threshold temperature for defining heatwaves (33°C) during heatwaves.
To control for the effect of air pollutants, we obtained data for the 24-hour average concentrations of particles smaller than 10 µm (PM10) and ozone (O3) from the National Institute of Environmental Research, Republic of Korea.
Classification of heat clusters
We used CDD to classify regions into several clusters with dissimilar climate conditions in the summer. A CDD is the cumulative difference between the daily mean outdoor temperature and standard temperature (24°C) in a year, and indicates the energy needed for cooling.21 The annual CDD values of each region were calculated for the summers of 1993–2012, and regions were subsequently divided into three heat clusters based on the scores and Getis-Ord local statistics (Gi*) p values of CDD. Given the coordinates for these regions, a hotspot analysis identified spatial clusters with high or low variable values.
Gi* was calculated as
 |
1 |
where xj was the value of a variable for region j,  was an average of the variable of each region, wi,j was the spatial weight between region i, j and n were the total numbers of regions.22 S was calculated as:
was an average of the variable of each region, wi,j was the spatial weight between region i, j and n were the total numbers of regions.22 S was calculated as:
 |
2 |
A high positive Gi* value (ie, far from zero) indicated a spatial clusters with high variable values. For negative Gi*, a smaller score indicated a more intense clustering of low variable values.23 Regions with a Gi*<−1.65 and those with a Gi*>1.65 were classified as cold and hot spots, respectively, within a 90% confidence level (CI). The regions with Gi* values within those extremes were considered evenly distributed regions. The study regions were divided into cluster H (hot spots with significantly high CDD values), cluster M (regions with no significantly high or low values) and cluster C (cold spots with significantly low values; figure 1). ArcMap software V.10.2 (ESRI, Redlands, California, USA; http://www.esri.com/) was used to conduct the Hotspot analysis.
Figure 1.
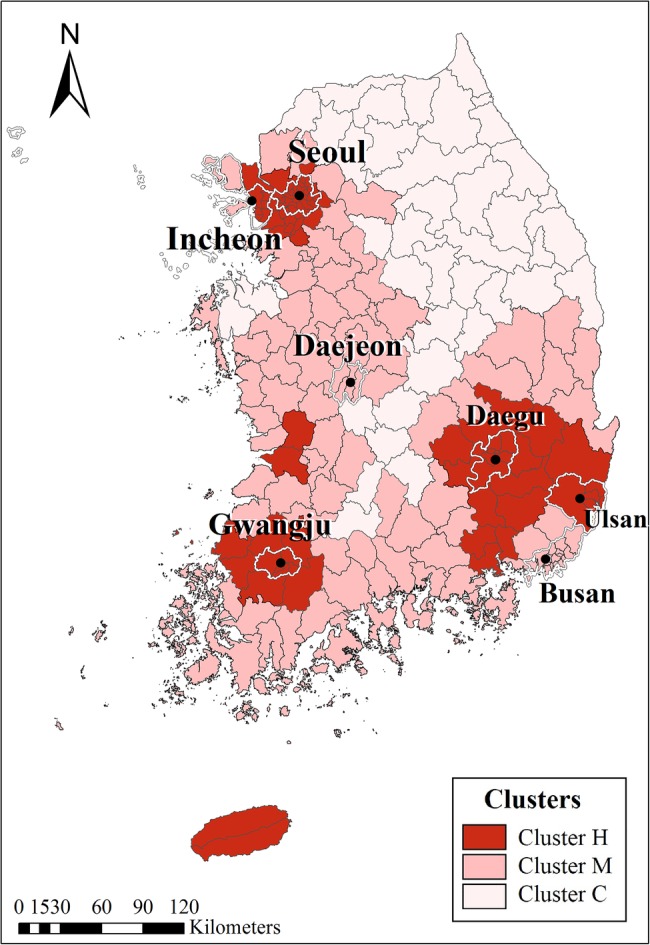
Three study clusters in South Korea. *Clusters H, M and C represent the hottest, moderate and coolest clusters, respectively. The capital and metropolitan cities are outlined in white boundaries. CDD, cooling degree days.
Descriptive statistics for meteorological indices of the clusters were estimated. The annual mean of heatwave frequency, duration and intensity was calculated for each of the study regions, which constitutes a study cluster, and the differences among the clusters were tested by Kruskal-Wallis test. The differences of annual mean of maximum temperature, mean temperature and CDD among clusters were tested by one-way analysis of variance.
Identification of a threshold using piecewise analysis
Piecewise regression analysis was used to identify the threshold temperature.24 Piecewise regression analysis identifies an inflection point in the relationship curve between the daily maximum temperature and corresponding mortality. Piecewise regression allows multiple linear models for different ranges of the independent variable. Two separate line segments were fitted for the daily maximum temperature and corresponding daily average death counts by applying a breakpoint in a model. We iteratively modelled two linear lines at multiple points through the temperature range in intervals of 0.5. The threshold was determined as the breakpoint of the best fit model based on the value of the R2 statistics. The analysis was conducted separately for all-cause, cardiovascular, and respiratory mortality and mortalities in subgroups (sex, age, education level and job status) in each heat cluster.
Estimation of the temperature–mortality relationship
GAM with a link function and a Poisson distribution was used to construct the association between daily mortality and temperature. The daily maximum temperature was used as the main independent variable. Temperatures of the current day (lag 0), previous single day (lag 1, 2 and 3) and average of 4–7 days were applied to the mode. Potential confounders, such as calendar year, month, holidays (including national holidays and weekends), humidity, pressure and concentrations of PM10 and O3 were controlled. Population was used to adjust for temporal population trends. The results are expressed as relative risks (RRs), which represent the increase in death counts with each 1°C increase in temperature above the threshold. We reported the greater estimates of temperature variables among lag days as a result.
The effect of temperature was estimated for subgroup of cause, age, sex, education level and job status. When examining age-specific risks, we compared the risk between the age groups of 20–49 and 50–74 years and the risk estimates were not particularly different between these two groups. Thus, we estimated and report temperature effect in young adults grouped into a single group (20–74 years).
GAMs are generally built for each separate subgroup of an effect modifiers (eg, sex, age) to accurately consider the population at risk, so most studies typically assessed modifying effects based on subanalyses. Similarly, two study periods in this study were compared from stratified analyses. To verify the descriptive comparison of stratified analysis, two-stage analysis was applied: year-specific GAMs followed by a metaregression analysis. We estimated the temperature–mortality relationship from year to year for each cluster allowing respective thresholds for each year from 1996 to 2012. A metaregression (mixed-effect model) was fitted for year-specific risks with year variable as a linear metaregressor to estimate trends over time. GAMs were conducted using SAS statistical software, V.9.3 (SAS Institute, Cary, North Carolina, USA; http://www.sas.com) and R ‘metafor’ package was used for the metaregression analysis.
Results
The mortality patterns and meteorological conditions in the three clusters during the periods of 1996–2000 and 2008–2012 are presented in table 1. The proportion of all-cause mortality among the elderly (age ≥75 years) increased in all clusters during the later period due to an ageing phenomenon. The population density in cluster H was prominently high (8235/km2 in 1996–2000 and 8291/km2 in 2008–2012), as this cluster included the capital and metropolitan cities within a relatively small area. Cluster C had the lowest population density (1743/km2 in 1996–2000 and 1833/km2 in 2008–2012). The numbers of all-cause and cardiovascular-related deaths in cluster H in 1996–2000 and 2008–2012 (154 373 and 170 112, respectively) were ∼1.2-fold greater than those in cluster M (134 623 and 140 549, respectively) and ∼4-fold greater than those in cluster C (37 109 and 34 812, respectively). The percentage of elderly deaths among all-cause deaths was highest in cluster C (44.2–55.4%).
Table 1.
Mortality patterns and climate conditions in clusters during the study periods
| 1996–2000 | 2008–2012 | 1996–2000 |
2008–2012 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All-combined regions |
Cluster H* | Cluster M | Cluster C | p Value | Cluster H | Cluster M | Cluster C | p Value | ||
| Population density (person/km2) | 4068 | 4054 | 8235 | 2148 | 1743 | – | 8291 | 2072 | 1833 | – |
| Number of deaths by cause (n) | ||||||||||
| All-cause | 326 105 | 345 473 | 154 373 | 134 623 | 37 109 | – | 170 112 | 140 549 | 34 812 | – |
| Cardiovascular | 85 219 | 80 512 | 39 317 | 35 948 | 9954 | – | 38 599 | 33 690 | 8223 | – |
| Respiratory | 18 155 | 26 924 | 8530 | 7427 | 2198 | – | 12 266 | 11 422 | 3236 | – |
| Number of deaths by sex (n) | ||||||||||
| Male | 176 116 | 188 067 | 82 181 | 73 358 | 20 577 | – | 92 445 | 76 463 | 19 159 | – |
| Female | 149 399 | 157 406 | 71 954 | 60 990 | 16 455 | – | 77 667 | 64 086 | 15 653 | – |
| Per cent of all-cause deaths among the elderly (≥75 years) | 40.4 | 51.4 | 38.9 | 41.1 | 44.2 | – | 49.4 | 52.8 | 55.4 | – |
| Annual mean (SD) of climate variables | – | |||||||||
| Maximum temperature (°C) | 26.9 (1.1) | 27.2 (1.1) | 27.5 (0.5) | 26.9 (1.0) | 26.5 (1.3) | 0.032 | 27.9 (0.9) | 27.2 (1.1) | 26.8 (1.2) | 0.013 |
| Mean temperature (°C) | 22.7 (1.1) | 23.1 (1.1) | 23.7 (0.9) | 22.7 (1.1) | 21.9 (0.6) | <0.0001 | 24.3 (0.8) | 23.2 (1.0) | 22.3 (0.6) | <0.0001 |
| Cooling degree days (°C)† | 87.5 (50.9) | 106.2 (55.2) | 129.0 (57.9) | 89.9 (50.0) | 57.1 (18.9) | <0.001 | 172.7 (49.1) | 105.5 (51.2) | 72.0 (22.0) | <0.0001 |
| Heatwave frequency‡ | 1.2 (0.8) | 1.0 (0.9) | 1.5 (1.0) | 1.0 (0.8) | 1.1 (0.7) | 0.264 | 2.0 (1.4) | 0.9 (0.7) | 0.8 (0.5) | 0.048 |
| Heatwave duration (days)‡ | 3.5 (2.8) | 3.6 (3.1) | 4.7 (3.8) | 3.1 (2.7) | 3.1 (1.9) | 0.377 | 6.9 (4.7) | 3.0 (2.5) | 2.8 (1.8) | 0.011 |
| Heatwave intensity (°C)‡ | 1.4 (2.2) | 2.1 (2.6) | 3.0 (3.6) | 1.1 (1.6) | 0.9 (1.0) | 0.090 | 4.4 (4.2) | 1.7 (2.1) | 1.5 (1.4) | 0.047 |
*Clusters H, M and C indicate the hottest, moderate and coolest clusters, respectively.
†Cooling degree days were defined as the difference between daily maximum temperature and base temperature (24°C), at which the use of air conditioning is required, during summer periods (June to August).
‡The number of consecutive days of heatwave (duration), number of occurrences of heatwaves (heatwave frequency) and cumulative sum of differences between the daily maximum temperature and standard point (33°C) on days with heatwaves (heatwave intensity).
The daily maximum and mean temperatures increased slightly (∼0.3–0.6°C) across all clusters (table 1). Temperature variations did not differ significantly among the clusters. The maximum temperatures were 27.5–27.9°C in cluster H, 26.9–27.2°C in cluster M and 26.5–26.8°C in cluster C. The lowest mean temperature was recorded for cluster C in 1996–2000 (21.9°C), and the highest value was recorded for cluster H in 2008–2012 (24.3°C). Meanwhile, the number of CDD in cluster H was approximately twofold greater than those in clusters M and C. The frequency, duration and intensity of heatwaves in cluster H were greater than those in clusters M and C; this difference was particularly large with respect to duration and intensity, which were approximately twofold greater in cluster H than in clusters M and C. The results illustrate that cluster H experienced more severe heat stress in summer, compared with other regions.
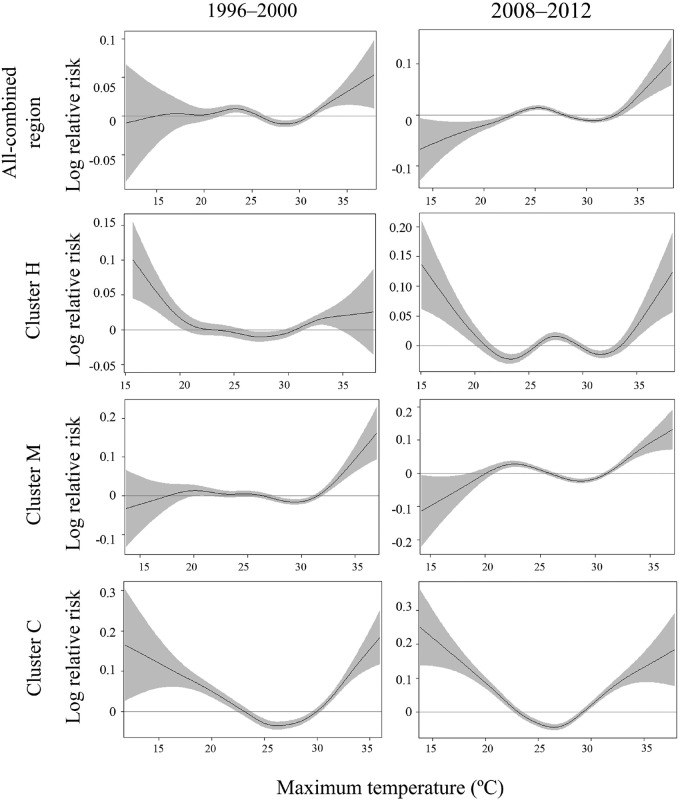
The relationship curves between maximum temperature and all-cause mortality, obtained from the GAM spline, revealed different patterns among clusters (figure 2). In clusters M and C, the slope of the curve decreased slightly in 2008–2012, compared with 1996–2000. However, the slope of cluster H was steeper in 2008–2012 than in 1996–2000. The plots for cluster H indicated the highest threshold, whereas those for cluster C indicated the lowest threshold.
Figure 2.
Curves of the relationship between all-cause mortality and maximum temperature in all-combined regions and study clusters in each study period (1996–2000 and 2008–2012). *Clusters H, M and C indicate the hottest, moderate and coolest clusters, respectively.
The thresholds for all-cause mortality, estimated by piecewise regression analysis, were 33.5°C, 32.5°C and 30.5°C for clusters H, M and C, respectively (table 2). Thresholds for other diseases were also highest in cluster H. For cardiovascular mortality, the thresholds were 33.5°C, 30.5°C and 30.5°C in clusters H, M and C, respectively. For respiratory mortality, thresholds of 31.5°C, 31.5°C and 29.5°C were identified for clusters H, M and C, respectively.
Table 2.
Relative risks in cause-specific mortality for an increase of 1°C of maximum temperature above the threshold in the study clusters during both study periods, stratified by age group
| All regions |
Cluster H* |
Cluster M |
Cluster C |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
||||||||||
| Mortality | Group | RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
||||||||
| (Threshold=33.5°C) | (Threshold=33.5°C) | (Threshold=32.5°C) | (Threshold=30.5°C) | ||||||||||||||
| All-cause | All ages | 1.05 | (1.01 to 1.08) | 1.03 | (1.01 to 1.04) | 1.07 | (1.02 to 1.12) | 1.10 | (1.06 to 1.14) | 1.04 | (1.01 to 1.07) | 1.02 | (1.01 to 1.04) | 1.03 | (1.00 to 1.06) | 1.01 | (1.00 to 1.02) |
| Age <20 years | 1.13 | (1.00 to 1.28) | 1.08 | (0.92 to 1.27) | 1.05 | (0.95 to 1.17) | 1.13 | (0.92 to .41) | 1.06 | (0.99 to 1.12) | 1.03 | (0.96 to 1.11) | 1.11 | (1.00 to 1.24) | 1.09 | (0.94 to 1.26) | |
| Age 20–74 years | 1.04 | (1.00 to 1.09) | 1.03 | (0.99 to 1.07) | 1.04 | (0.98 to 1.11) | 1.06 | (1.01 to 1.12) | 1.02 | (0.99 to 1.05) | 1.01 | (1.00 to 1.03) | 1.04 | (1.00 to 1.08) | 1.01 | (0.99 to 1.03) | |
| Age ≥75 years | 1.05 | (1.00 to 1.11) | 1.04 | (1.02 to 1.06) | 1.08 | (1.01 to 1.16) | 1.05 | (1.02 to 1.08) | 1.02 | (0.99 to 1.05) | 1.03 | (0.99 to 1.07) | 1.02 | (1.00 to 1.04) | 1.01 | (0.99 to 1.03) | |
| (Threshold=31.5°C) | (Threshold=33.5°C) | (Threshold=30.5°C) | (Threshold=30.5°C) | ||||||||||||||
| Cardiovascular | All ages | 1.02 | (0.98 to 1.05) | 1.02 | (1.00 to 1.04) | 1.05 | (0.95 to 1.15) | 1.09 | (1.01 to 1.18) | 1.07 | (1.01 to 1.14) | 1.02 | (1.00 to 1.03) | 1.03 | (0.93 to 1.13) | 1.01 | (0.99 to 1.03) |
| Age 20–74 years | 1.02 | (1.01 to 1.04) | 1.01 | (0.99 to 1.03) | 1.08 | (0.95 to 1.22) | 1.11 | (1.04 to 1.19) | 1.01 | (0.98 to 1.04) | 1.01 | (0.99 to 1.04) | 1.1 | (0.97 to 1.25) | 1.06 | (0.97 to 1.16) | |
| Age ≥75 years | 1.04 | (1.02 to 1.06) | 1.01 | (0.99 to 1.04) | 1.05 | (0.98 to 1.13) | 1.06 | (0.96 to 1.17) | 1.05 | (1.01 to 1.09) | 1.01 | (0.99 to 1.03) | 1.03 | (1.00 to 1.07) | 1.02 | (0.99 to 1.05) | |
| (Threshold=31.5°C) | (Threshold=31.5°C) | (Threshold=31.5°C) | (Threshold=29.5°C) | ||||||||||||||
| Respiratory | All ages | 1.05 | (1.02 to 1.08) | 1.02 | (1.00 to 1.04) | 1.03 | (1.01 to 1.06) | 1.05 | (1.02 to 1.07) | 1.06 | (1.01 to 1.11) | 1.02 | (0.98 to 1.06) | 1.04 | (1.00 to 1.09) | 1.03 | (0.98 to 1.09) |
| Age 20–74 years | 1.03 | (0.99 to 1.07) | 1.04 | (1.00 to 1.08) | 1.04 | (1.00 to 1.08) | 1.06 | (1.01 to 1.12) | 1.09 | (0.97 to 1.22) | 1.05 | (0.98 to 1.13) | 1.02 | (0.96 to 1.09) | 1.04 | (0.93 to 1.17) | |
| Age ≥75 years | 1.06 | (1.02 to 1.1) | 1.02 | (0.98 to 1.07) | 1.06 | (0.97 to 1.16) | 1.07 | (1.00 to 1.14) | 1.08 | (1.01 to 1.15) | 1.03 | (0.99 to 1.07) | 1.06 | (1.00 to 1.13) | 1.03 | (0.99 to 1.07) | |
Possible confounders were adjusted in the model; these included individual maximum temperature until 3 lag-days, average maximum temperature during 4–7 lag-days, humidity, pressure, daily concentrations of air pollutants (PM10 and O3), year, month, holidays and weekends.
Significant values (p<0.05) are indicated in bold.
*Clusters H, M and C represent the hottest, moderate and coolest clusters, respectively.
The age-specific relative mortality risks associated with a 1°C increase in temperature above the threshold for all-combined regions and each cluster are presented in table 2. The represented risks were mainly observed on lag 0 day, whereas the lag effects on lag days 1–7 were controlled. In cluster H, a pattern of increasing all-cause mortality risk was observed over time in the all ages group, whereas no increasing trends were observed in clusters M and C or all-combined regions. In cluster H, the risk for the all ages group increased from 1.07 (95% CI 1.02 to 1.12) in 1996–2000 to 1.10 (95% CI 1.06 to 1.14) in 2008–2012 for all-cause mortality. In contrast, in cluster M, the all-cause mortality risk for the all ages group decreased from 1.04 (95% CI 1.01 to 1.07) to 1.02 (95% CI 1.01 to 1.04). In cluster C, the all-cause mortality risk exhibited a decreasing trend from 1.03 (95% CI 1.00 to 1.06) to 1.01 (95% CI 1.00 to 1.02) for the all ages group. The risks of cardiovascular and respiratory mortality also exhibited an increasing pattern over time in cluster H, but decreasing patterns in clusters M and C.
For all-cause mortality in the elderly (≥75 years) in cluster H, the risk was 1.05 (95% CI 1.02 to 1.08) in 2008–2012 and 1.08 (95% CI 1.01 to 1.16) in 1996–2000, respectively (table 2). For clusters M and C, the risks in the elderly group, as well as all age groups, exhibited decreasing patterns in the later study period (2008–2012), compared with the earlier period (1996–2000). However, in younger adults (<75 years) from cluster H, an increasing trend in risk was observed from 1.04 (95% CI 0.98 to 1.11) to 1.06 (95% CI 1.01 to 1.12).
The impacts of temperature on all-cause mortality in subpopulations classified according to sex, job status and education level were also evaluated (table 3). Although during one period men had a higher risk than women, this pattern reversed in the other period; accordingly, there was no significant risk pattern according to sex. The risks for male and female exhibited an increasing pattern in cluster H, but not in clusters M and C. The risks for those with no education were higher in 2008–2012 relative to 1996–2000 in the all-combined regions (1.04 vs 1.02) and in cluster H (1.04 vs 1.02), whereas those in cluster M or C hardly changed. Significantly greater risks for blue-collar workers were observed in 2008–2012, compared with 1996–2000 in the all-combined regions (RR=1.06, 95% CI 1.04 to 1.07), cluster H (RR=1.05, 95% CI 1.02 to 1.08) and cluster M (RR=1.05, 95% CI 1.03 to 1.08).
Table 3.
All-cause mortality risk from heat according to sex, educational level and job status
| All regions |
Cluster H† |
Cluster M |
Cluster C |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
1996–2000 |
2008–2012 |
||||||||||
| Variable* | Group | RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
RR (95% CI) |
||||||||
| (Threshold=33.5°C) | (Threshold=33.5°C) | (Threshold=32.5°C) | (Threshold=30.5°C) | ||||||||||||||
| Sex | Male | 1.01 | (0.96 to 1.05) | 1.05 | (1.03 to 1.07) | 1.06 | (0.99 to 1.13) | 1.10 | (1.04 to 1.16) | 1.05 | (1.00 to 1.1) | 1.02 | (1.00 to 1.04) | 1.01 | (0.99 to 1.03) | 1.01 | (0.99 to 1.03) |
| Female | 1.02 | (0.98 to 1.08) | 1.07 | (1.04 to 1.09) | 1.07 | (1.00 to 1.15) | 1.09 | (1.03 to 1.15) | 1.03 | (0.97 to 1.09) | 1.03 | (0.99 to 1.08) | 1.02 | (1.00 to 1.04) | 1.02 | (0.98 to 1.06) | |
| (Threshold=29.5°C) | (Threshold=29.5°C) | (Threshold=30.5°C) | (Threshold=29.5°C) | ||||||||||||||
| Education level | None | 1.02 | (1.01 to 1.03) | 1.04 | (1.03 to 1.05) | 1.02 | (1.01 to 1.04) | 1.04 | (1.03 to 1.06) | 1.04 | (1.02 to 1.06) | 1.04 | (1.01 to 1.06) | 1.01 | (0.99 to 1.04) | 1.02 | (0.99 to 1.05) |
| Elementary | 0.99 | (0.99 to 1.00) | 1.01 | (1.01 to 1.02) | 1.01 | (1.00 to 1.01) | 1.01 | (1.00 to 1.03) | 1.01 | (0.99 to 1.03) | 1.01 | (1.00 to 1.03) | 1.02 | (1.00 to 1.04) | 1.01 | (0.99 to 1.03) | |
| ≥6th grade | 0.99 | (0.98 to 1.00) | 1.01 | (1.00 to 1.02) | 1.02 | (1.01 to 1.02) | 1.01 | (0.99 to 1.03) | 1.01 | (0.99 to 1.02) | 1.01 | (1.00 to 1.02) | 1.05 | (0.99 to 1.11) | 1.01 | (0.95 to 1.07) | |
| (Threshold=30.5°C) | (Threshold=30.5°C) | (Threshold=30.5°C) | (Threshold=29.5°C) | ||||||||||||||
| Job status‡ | White-collar | 1.01 | (0.99 to 1.03) | 1.01 | (0.99 to 1.02) | 1.03 | (1.00 to 1.05) | 1.02 | (0.99 to 1.04) | 1.05 | (1.00 to 1.12) | 1.03 | (1.00 to 1.06) | 1.04 | (0.99 to 1.1) | 1.01 | (0.97 to 1.06) |
| Blue-collar | 1.01 | (0.99 to 1.02) | 1.06 | (1.04 to 1.07) | 1.02 | (0.99 to 1.04) | 1.05 | (1.02 to 1.08) | 1.01 | (0.99 to 1.02) | 1.05 | (1.03 to 1.08) | 1.02 | (1.01 to 1.04) | 1.02 | (1.00 to 1.04) | |
Significant values (p<0.05) are indicated in bold.
*Possible confounders were adjusted in the model; these included individual maximum temperature until 3 lag-days, average maximum temperature during 4–7 lag-days, humidity, pressure, daily concentrations of air pollutants (PM10 and O3), year, month, holidays and weekends.
†Clusters H, M and C represent the hottest, moderate and coolest clusters, respectively.
‡White-collar jobs include management, office, scientific and service occupations. Blue-collar jobs include agricultural, manufacturing or manual work.
PM10, particles smaller than 10 µm.
Discussion
A few studies have analysed changes in heat-related mortality over time;25–33 however, those studies were often conducted in a single region and gave little consideration to differences in patterns of risk change based on climate. To the best of our knowledge, this is the first study to examine temporal changes in the temperature–mortality risk relationship in geographical regions of South Korea with climatic differences. Apparent threshold differences were identified among clusters classified by climate; the hottest cluster showed a consistently higher threshold for all types of mortality, compared with the cooler clusters. Similarly, previous studies in China,34 the USA,7 35 European cities8 11 36 37 and South Korea17 compared the temperature–mortality relationship among cities located in various geographic regions and found a higher threshold temperature in cities with hotter climates.
We found an interesting result of a difference in patterns of temporal changes in risk among clusters, and this finding might require confirmation in further studies. An increasing pattern of heat-related mortality was observed in the hottest cluster (cluster H), whereas the risk remained unchanged or decreased slightly in cooler clusters (cluster M or C). The results of metaregression analyses of year-specific temperature-related risks supported the findings from stratified analyses in the main results; the increasing trend in RRs of all-cause mortality for all ages and 20–74 age groups over year in cluster H were statistically significant (see online supplementary figure S1). The decreased risks in the elderly (≥75 years) or 20–74 years age group in cluster M and in cluster C showed weak statistical power. This result was similar to that of a recent study conducted in the USA, which showed that regions with cooler climates exhibited a steeper temporal decline in temperature-related mortality, whereas regions with hotter climates exhibited a slight reduction.38 A recent study examined changes in mortality risk associated with high temperature in six Korean cities and found weak evidence for increases in risks.39 In our study, the changes in the risks over time for all-combined regions similarly demonstrated little evidence of risk changes. However, we added new information of different risk changing patterns among regions by considering clusters with different climate. Increases in the average temperature led to higher increases in heatwave variables (frequency, duration and intensity) over a 17-year period in cluster H relative to the other clusters (table 1), which may explain the increased heat effect in cluster H. Our results suggest that future climate changes could induce considerably more extreme heatwave events and temperature-related mortalities within populations living in hotter regions. Moderate and cool regions could be also at higher risks in the future because of their lower threshold compared with hotter regions, although increased risks were not found in this study.
Yearly Relative Risks in the elderly (Left) and the young adults (Right) in each cluster: (a) Cluster H, (b) Cluster M, (c) Cluster C.
bmjopen-2016-011786supp_figure.pdf (202.4KB, pdf)
There are six metropolitan cities in South Korea, and they are under the direct and intensive control of the central government. The developmental level of these cities is exceedingly higher than that in other cities, as these metropolitan cities have been developed as special zones. We identified that more urbanised regions, including the capital (Seoul) and three metropolitan cities (Gwangju, Daegu and Busan), comprised the hottest cluster (cluster H). The rate of increase in usage of air conditioning, an important factor of risk reduction,18 38 40 did not differ significantly among clusters during the study periods, despite differences in urbanisation and socioeconomic status. Urbanised areas have an increased capacity for thermal retention because of the heavy building density. This causes an ‘urban heat island effect’, which refers to higher ambient temperatures in urban areas relative to surrounding regions.41 This ‘urban heat island effect’ most likely causes urbanised areas to suffer from a higher frequency of heatwaves, compared with other regions, eventually leading to a stronger heat–mortality relationship.42 43 In addition, according to a governmental report published by the Rural Development Administration, the increase in temperature over the past 30 years was higher in urban areas than in rural areas because of the lower amount of green space and higher building density in the former.44 As a result, the increased heat effect observed in cluster H agrees with the projection that urbanised regions might be much more vulnerable to damage from temperature-related mortality caused by future climate changes.42
CDD is a major index used to explain energy demand in the energy and power fields.45 Several studies have used CDD to approximate differences in climate and explain geographical variances in the effect of heat on heat-related health consequences.46–48 To the best of our knowledge, this is the first study to evaluate the impact of temperature on mortality in South Korea using CDD. The adoption of CDD for categorising regions with different heat conditions appears useful for a country-level study, rather than using typical categorisation methods based on air mass type, as a small country is generally classified under a single category (eg, hot and humid). Compared with other commonly used thermal indices (eg, mean or maximum temperature), CDD may also more effectively represent geographical differences in the degree of heat because those other indices reveal relatively narrow variances among regions. Using multiple clusters based on CDD, we could identify variations in temporal changes in the temperature–mortality relationship even within a small country.
Preventive measures such as heatwave early warning forecasts have been implemented to prevent temperature-related mortality in developed countries worldwide. Several studies have reported the effectiveness of early heat health warning forecasts or surveillance systems for reducing heat-related mortality by comparing the risks between time periods with and without these preventive measures.26 27 30 31 33 The KMA initiated a national heatwave early warning system in 2008. Maximum temperature and the national threshold are used to identify heatwave. Heatwave is defined as days with a daily maximum temperature exceeding 33°C for more than 2 days. A heatwave forecast announces regions where heatwave is predicted. Once a heatwave is predicted or observed, the local government's heatwave department immediately receives a warning text from the KMA, after which officials implement actions targeted towards the elderly (>65 years old) and disabled people who live alone; they open shade shelters and dispatch health volunteers to the targeted people. These measures might be unequally effective with respect to region, age, socioeconomic status and job status. There might be a positive effect of heatwave plan targeted plan since common risk reduction was observed in elderly populations over time in all clusters by the stratified analyses. However, the trend of increased risks in the hottest cluster suggests a need for a modified heatwave plan for groups considered highly vulnerable to heat exposure, specifically younger people, those with less education attainment or those holding blue-collar jobs. Younger people and those with less education are more likely to be exposed to high heat during the summer because of relatively frequent outdoor activity9 and a low socioeconomic status, respectively. Blue-collar workers are more vulnerable than other workers to heat-related risk49 because many blue-collar jobs comprise outdoor occupations such as agricultural or manual labour, where workers are exposed to high temperatures during working hours.50 51 Efforts to develop particularly customised preventive measures, both for the elderly and younger adults, as well as those with a low socioeconomic status and outdoor labourers are highly recommended.
This study has several limitations. First, the study period (17 years) might be short to predict in the far future trends in the impact of high temperatures following global warming. Nevertheless, the increasing trend in temperatures due to climate change was higher in South Korea than the average global temperature increase in the 20th century as reported by the IPCC Fourth Report, and these changes in temperature have accelerated during the most recent two decades.20 Therefore, we expect that our study results will sufficiently reflect variations in the effects of heat on mortality over time to some degree.
Second, the risks calculated in 2008–2012 were only adjusted for PM10 and O3 concentrations, as the daily mean PM10 and O3 data were only available for a limited period (2003–2012). Several studies showed that air pollutants were potential confounders of the temperature–mortality relationship,1 52–54 whereas others reported no significant confounding effect.13 In this study, the adjusted risks for mortality hardly changed or decreased only slightly when compared with the unadjusted estimates.
According to the worst greenhouse gas emission scenario, it is expected that the annual average temperatures will increase by up to 5.3°C and that the annual extreme heatwave duration will increase by 6.1 days in South Korea in the late 21st century, compared with the late 1990s.20 These changes will be much greater in lowland areas with higher temperatures.20 Along with this projection, populations living in hotter regions or with exposure to high levels of heat due to socioeconomic status might be at a higher risk of heat-related health damage resulting from climate change. It is imperative to improve preparedness for health damage resulting from heat stress at the national and regional levels.29 Continuous efforts should also be implemented to assess long-term trends in heat-related risks with regard to public health and identify the factors related to changes in this risk in order to develop appropriate climate change adaptation plans.
Footnotes
Contributors: SH contributed to building the study concept and design, conducting the paper review and the entire statistical analysis, writing documents and corresponding to peer reviewers. BYK gave advice on statistical analysis. JK collected and managed the data. KHJ participated in the paper review. The proofreading of the first draft is attributed to discussing process with SH, SL and EL.
Funding: The researchers of this study express thanks to the Korea Center for Disease Control and Prevention (CDC), with research programme no. 2013E2100102 and no. 2013E2100202. Also, this work was funded by the Korea Meteorological Administration Research and Development Program under (Grant KMIPA 2015-2130).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Basu R. High ambient temperature and mortality: a review of epidemiologic studies from 2001 to 2008. Environ Health 2009;8:40 10.1186/1476-069X-8-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basu R, Samet JM. An exposure assessment study of ambient heat exposure in an elderly population in Baltimore, Maryland. Environ Health Perspect 2002;110:1219–24. 10.1289/ehp.021101219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalkstein LS, Greene JS. An evaluation of climate/mortality relationships in large US cities and the possible impacts of a climate change. Environ Health Perspect 1997;105:84 10.1289/ehp.9710584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol 2003;157:1074–82. 10.1093/aje/kwg096 [DOI] [PubMed] [Google Scholar]
- 5.Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med 2009;51:33–7. 10.1097/JOM.0b013e318193e12e [DOI] [PubMed] [Google Scholar]
- 6.Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med 2008;35:429–35. 10.1016/j.amepre.2008.08.021 [DOI] [PubMed] [Google Scholar]
- 7.Curriero FC, Heiner KS, Samet JM et al. . Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol 2002;155:80–7. 10.1093/aje/155.1.80 [DOI] [PubMed] [Google Scholar]
- 8.Iñiguez C, Ballester F, Ferrandiz J et al. . Relation between temperature and mortality in thirteen Spanish cities. Int J Environ Res Public Health 2010;7:3196–210. 10.3390/ijerph7083196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu W, Xiao Y, Li G et al. . Temperature–mortality relationship in four subtropical Chinese cities: a time-series study using a distributed lag non-linear model. Sci Total Environ 2013;449:355–62. 10.1016/j.scitotenv.2013.01.090 [DOI] [PubMed] [Google Scholar]
- 10.Li Y, Cheng Y, Cui G et al. . Association between high temperature and mortality in metropolitan areas of four cities in various climatic zones in China: a time-series study. Environ Health 2014;13:65 10.1186/1476-069X-13-65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong BG, Chalabi Z, Fenn B et al. . Association of mortality with high temperatures in a temperate climate: England and Wales. J Epidemiol Community Health 2010;65:340–5. 10.1136/jech.2009.093161 [DOI] [PubMed] [Google Scholar]
- 12.Michelozzi P, De Sario M, Accetta G et al. . Temperature and summer mortality: geographical and temporal variations in four Italian cities. J Epidemiol Community Health 2006;60:417–23. 10.1136/jech.2005.040857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morabito M, Crisci A, Moriondo M et al. . Air temperature-related human health outcomes: current impact and estimations of future risks in Central Italy. Sci Total Environ 2012;441:28–40. 10.1016/j.scitotenv.2012.09.056 [DOI] [PubMed] [Google Scholar]
- 14.Chung J-Y, Honda Y, Hong Y-C et al. . Ambient temperature and mortality: an international study in four capital cities of East Asia. Sci Total Environ 2009;408:390–6. 10.1016/j.scitotenv.2009.09.009 [DOI] [PubMed] [Google Scholar]
- 15.Lim Y-H, Park AK, Kim H. Modifiers of diurnal temperature range and mortality association in six Korean cities. Int J Biometeorol 2012;56:33–42. 10.1007/s00484-010-0395-0 [DOI] [PubMed] [Google Scholar]
- 16.Son JY, Lee JT, Anderson GB et al. . Bulnerability to temperature-related mortality in Seoul, Korea. Environ Res Lett 2011;6:034027 10.1088/1748-9326/6/3/034027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ha J, Shin Y, Kim H. Distributed lag effects in the relationship between temperature and mortality in three major cites in South Korea. Sci Total Environ 2011;409:3274–80. 10.1016/j.scitotenv.2011.05.034 [DOI] [PubMed] [Google Scholar]
- 18.Ha J, Kim H. Changes in the association between summer temperature and mortality in Seoul, South Korea. Int J Biometeorol 2013;57:535–44. 10.1007/s00484-012-0580-4 [DOI] [PubMed] [Google Scholar]
- 19.Zanobetti A, O'Neill MS, Gronlund CJ et al. . Summer temperature variability and long-term survival among elderly people with chronic disease. Proc Natl Acad Sci USA 2012;109:6608–13. 10.1073/pnas.1113070109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Korea Meteorological Administration. Korea Climate Change Evaluation Report Seoul: Climate Policy Division, 2014. [Google Scholar]
- 21.Christenson M, Manz H, Gyalistras D. Climate warming impact on degree-days and building energy demand in Switzerland. Energy Conversion Manage 2006;47:671–86. 10.1016/j.enconman.2005.06.009 [DOI] [Google Scholar]
- 22.Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geographical Anal 1995;27:286–306. 10.1111/j.1538-4632.1995.tb00912.x [DOI] [Google Scholar]
- 23.ESRI online help library. (http://help.arcgis.com/EN/ARCGISDESKTOP/10.0/HELP/index.html#/How_Hot_Spot_Analysis_Getis_Ord_Gi_works/005p00000011000000/) (accessed 7 Dec 2015).
- 24.Lee S, Lee E, Park MS et al. . Short-term effect of temperature on daily emergency visits for acute myocardial infarction with threshold temperatures. PLoS ONE 2014;9:e94070 10.1371/journal.pone.0094070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weisskopf MG, Anderson HA, Foldy S et al. . Heat wave morbidity and mortality, Milwaukee, Wis, 1999 vs 1995: an improved response? Am J Public Health 2002;92:830–3. 10.2105/AJPH.92.5.830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fouillet A, Rey G, Wagner V et al. . Has the impact of heat waves on mortality changed in France since the European heat wave of summer 2003? A study of the 2006 heat wave. Int J Epidemiol 2008;37:309–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kyselý J, Kříž B. Decreased impacts of the 2003 heat waves on mortality in the Czech Republic: an improved response? Int J Biometeorol 2008;52:733–45. 10.1007/s00484-008-0166-3 [DOI] [PubMed] [Google Scholar]
- 28.Nitschke M, Tucker GR, Hansen AL et al. . Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis. Environ Health 2011;10:42 10.1186/1476-069X-10-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kyselý J, Plavcová E. Declining impacts of hot spells on mortality in the Czech Republic, 1986–2009: adaptation to climate change? Climatic Change 2012;113:437–53. 10.1007/s10584-011-0358-4 [DOI] [Google Scholar]
- 30.Morabito M, Profili F, Crisci A et al. . Heat-related mortality in the Florentine area (Italy) before and after the exceptional 2003 heat wave in Europe: an improved public health response? Int J Biometeorol 2012;56:801–10. 10.1007/s00484-011-0481-y [DOI] [PubMed] [Google Scholar]
- 31.Schifano P, Leone M, De Sario M et al. . Changes in the effects of heat on mortality among the elderly from 1998–2010: results from a multicenter time series study in Italy. Environ Health 2012;11:58 10.1186/1476-069X-11-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Culqui DR, Diaz J, Simón F et al. . Evaluation of the plan for surveillance and controlling of the effects of heat waves in Madrid. Int J Biometeorol 2014;58:1799–802. 10.1007/s00484-013-0731-2 [DOI] [PubMed] [Google Scholar]
- 33.Petkova EP, Gasparrini A, Kinney PL. Heat and mortality in New York City since the beginning of the 20th century. Epidemiology 2014;25:554–60. 10.1097/EDE.0000000000000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Lan L, Wang Y et al. . Extremely cold and hot temperatures increase the risk of diabetes mortality in metropolitan areas of two Chinese cities. Environ Res 2014;134:91–7. 10.1016/j.envres.2014.06.022 [DOI] [PubMed] [Google Scholar]
- 35.Hartz DA, Brazel AJ, Golden JS. A comparative climate analysis of heat-related emergency 911 dispatches: Chicago, Illinois and Phoenix, Arizona USA 2003 to 2006. Int J Biometeorol 2013;57:669–78. 10.1007/s00484-012-0593-z [DOI] [PubMed] [Google Scholar]
- 36.Baccini M, Biggeri A, Accetta G et al. . Heat effects on mortality in 15 European cities. Epidemiology 2008;19:711–19. 10.1097/EDE.0b013e318176bfcd [DOI] [PubMed] [Google Scholar]
- 37.Keatinge W, Donaldson G, Cordioli E et al. . Heat related mortality in warm and cold regions of Europe: observational study. BMJ 2000;321:670–3. 10.1136/bmj.321.7262.670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bobb JF, Peng RD, Bell ML et al. . Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect 2014;122:811–16. 10.1289/ehp.1307392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gasparrini A, Guo Y, Hashizume M et al. . Temporal variation in heat-mortality associations: a multicountry study. Environ Health Perspect 2015;123:1200–7. 10.1289/ehp.1409070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nordio F, Zanobetti A, Colicino E et al. . Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ Int 2015;81:80–6. 10.1016/j.envint.2015.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Basu R, Samet JM. Relation between elevated ambient temperature and mortality: a review of the epidemiologic evidence. Epidemiol Rev 2002;24:190–202. 10.1093/epirev/mxf007 [DOI] [PubMed] [Google Scholar]
- 42.Hajat S, Kosatky T. Heat-related mortality: a review and exploration of heterogeneity. J Epidemiol Community Health 2010;64:753–60. 10.1136/jech.2009.087999 [DOI] [PubMed] [Google Scholar]
- 43.Tan J, Zheng Y, Tang X et al. . The urban heat island and its impact on heat waves and human health in Shanghai. Int J Biometeorol 2010;54:75–84. 10.1007/s00484-009-0256-x [DOI] [PubMed] [Google Scholar]
- 44.Rural Development Administraion National Institute of Agricultural Sciences. What is the economic value of agriculture in the era of Climate Change? (Published in Korean). (http://radar.ndsl.kr/radDetail.do?cn=DT200800442) (accessed 7 Dec 2015)
- 45.OrtizBeviá M, Sánchez-López G, Alvarez-Garcìa F et al. . Evolution of heating and cooling degree-days in Spain: trends and interannual variability. Global Planetary Change 2012;92:236–47. 10.1016/j.gloplacha.2012.05.023 [DOI] [Google Scholar]
- 46.McDonald R, McDonald J, Bida J et al. . Subarachnoid hemorrhage incidence in the United States does not vary with season or temperature. AJNR Am J Neuroradiol 2012;33:1663–8. 10.3174/ajnr.A3059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramlow JM, Kuller LH. Effects of the summer heat wave of 1988 on daily mortality in Allegheny County, PA. Public Health Rep 1990;105:283–9. [PMC free article] [PubMed] [Google Scholar]
- 48.Alexander P. Association of monthly frequencies of diverse diseases in the calls to the public emergency service of the city of Buenos Aires during 1999–2004 with meteorological variables and seasons. Int J Biometeorol 2013;57:83–90. 10.1007/s00484-012-0536-8 [DOI] [PubMed] [Google Scholar]
- 49.Yang J, Ou C-Q, Ding Y et al. . Daily temperature and mortality: a study of distributed lag non-linear effect and effect modification in Guangzhou. Environ Health 2012;11:63 10.1186/1476-069X-11-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kravchenko J, Abernethy AP, Fawzy M et al. . Minimization of heatwave morbidity and mortality. Am J Prev Med 2013;44:274–82. 10.1016/j.amepre.2012.11.015 [DOI] [PubMed] [Google Scholar]
- 51.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet 2006;367:859–69. 10.1016/S0140-6736(06)68079-3 [DOI] [PubMed] [Google Scholar]
- 52.Basu R, Feng W-Y, Ostro BD. Characterizing temperature and mortality in nine California counties. Epidemiology 2008;19:138–45. 10.1097/EDE.0b013e31815c1da7 [DOI] [PubMed] [Google Scholar]
- 53.O'Neill MS, Hajat S, Zanobetti A et al. . Impact of control for air pollution and respiratory epidemics on the estimated associations of temperature and daily mortality. Int J Biometeorol 2005;50:121–9. 10.1007/s00484-005-0269-z [DOI] [PubMed] [Google Scholar]
- 54.Ren C, Williams GM, Morawska L et al. . Ozone modifies associations between temperature and cardiovascular mortality: analysis of the NMMAPS data. Occup Environ Med 2008;65:255–60. 10.1136/oem.2007.033878 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Yearly Relative Risks in the elderly (Left) and the young adults (Right) in each cluster: (a) Cluster H, (b) Cluster M, (c) Cluster C.
bmjopen-2016-011786supp_figure.pdf (202.4KB, pdf)