Abstract
Introduction
Decreased plasma vitamin D (VD) levels are linked to cardiovascular damage. However, clinical trials have not demonstrated a benefit of VD supplements on left ventricular (LV) remodelling. Anterior ST-elevation acute myocardial infarction (STEMI) is the best human model to study the effect of treatments on LV remodelling. We present a proof-of-concept study that aims to investigate whether VD improves LV remodelling in patients with anterior STEMI.
Methods and analysis
The VITamin D in Acute Myocardial Infarction (VITDAMI) trial is a multicentre, randomised, double-blind, placebo-controlled trial. 144 patients with anterior STEMI will be assigned to receive calcifediol 0.266 mg capsules (Hidroferol SGC)/15 days or placebo on a 2:1 basis during 12 months. Primary objective: to evaluate the effect of calcifediol on LV remodelling defined as an increase in LV end-diastolic volume ≥10% (MRI). Secondary objectives: change in LV end-diastolic and end-systolic volumes, ejection fraction, LV mass, diastolic function, sphericity index and size of fibrotic area; endothelial function; plasma levels of aminoterminal fragment of B-type natriuretic peptide, galectin-3 and monocyte chemoattractant protein-1; levels of calcidiol (VD metabolite) and other components of mineral metabolism (fibroblast growth factor-23 (FGF-23), the soluble form of its receptor klotho, parathormone and phosphate). Differences in the effect of VD will be investigated according to the plasma levels of FGF-23 and klotho. Treatment safety and tolerability will be assessed. This is the first study to evaluate the effect of VD on cardiac remodelling in patients with STEMI.
Ethics and dissemination
This trial has been approved by the corresponding Institutional Review Board (IRB) and National Competent Authority (Agencia Española de Medicamentos y Productos Sanitarios (AEMPS)). It will be conducted in accordance with good clinical practice (International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use - Good Clinical Practice (ICH-GCP)) requirements, ethical principles of the Declaration of Helsinki and national laws. The results will be submitted to indexed medical journals and national and international meetings.
Trial registration number
NCT02548364; Pre-results.
Keywords: Vitamin D, acute myocardial infarction, calcifediol, remodeling, cardiac magnetic resonance imaging
Strengths and limitations of this study.
This study will assess the effect of vitamin D (VD) supplements on the myocardium after an acute myocardial infarction, which is probably the best model to study left ventricular remodelling.
In addition to calcidiol plasma levels, other components of mineral metabolism such as fibroblast growth factor-23 and its soluble receptor, klotho, will be taken into account.
As a limitation, this study is not powered to study if a potential benefit of VD on myocardial remodelling translates into a clinical benefit. In case of a positive result, a larger study would be necessary to further investigate this issue.
Introduction
Traditionally, changes in plasma levels of the components of mineral metabolism (vitamin D (VD), fibroblast growth factor-23 (FGF-23), parathyroid hormone (PTH) and phosphate (P)) have been associated with renal disease.1–3 When slight decreases in glomerular filtration rate appear, the excretion of P is reduced. Compensatory responses are then activated to maintain P homoeostasis, including an increase in the levels of FGF-23 and a subsequent rise in those of PTH.1 FGF-23 promotes phosphaturia and decreases levels of plasma VD, both by downregulating synthesis and by increasing degradation.1
Although high P levels are associated with an increase in cardiovascular events and mortality,2 the aforementioned adaptive mechanisms prevent an increase in serum P levels in the early stages of chronic kidney disease.1–3 However, these compensatory mechanisms themselves are also related to cardiovascular damage.4 5 Thus, high FGF-23 plasma levels are independently associated with endothelial dysfunction, arterial stiffness, atherosclerosis burden, vascular calcification, left ventricular (LV) hypertrophy, progression of renal disease, and incidence of mortality and cardiovascular events in the general population as well as in patients with coronary artery disease, even after adjusting for renal glomerular filtration.4–10 Similarly, increased PTH plasma levels are related to LV hypertrophy, hypertension and increased cardiovascular events.11–16 Finally, VD deficiency has been associated with endothelial dysfunction, inflammation, vascular smooth muscle cell proliferation, vascular calcification, activation of the renin–angiotensin system, hypertension, myocardial infarction and stroke.17–22 However, low VD plasma levels are associated with vascular damage and also play an important role in the state of the myocardium. In this regard, VD deficiency is associated with rat LV hypertrophy and systolic dysfunction, biatrial enlargement, metabolic changes, inflammation, fibrosis and apoptosis.23
Of interest, abnormalities of mineral metabolism are not restricted to patients with overt renal disease, as in more than 50% of patients with coronary artery disease we have observed a deficiency of VD. However, only 20% of them had an estimated glomerular filtration rate <60 mL/min/1.73 m2.10 Moreover, abnormalities of mineral metabolism were evident even at glomerular filtration rates >90 mL/min/1.73 m2.24 In addition, the inverse relationship between VD levels and risk of coronary heart disease has also been seen in the general population.20 25
Despite the negative association between VD deficiency and cardiovascular disease described in multiple studies,10 20 26–35 clinical trials have failed to convincingly demonstrate a benefit of VD supplements on cardiovascular (CV) health. One such study was the PRIMO trial, which showed no improvement in ventricular mass index or any other remodelling parameters by administering paricalcitol, a selective activator of VD receptors, to patients with chronic renal failure.36 However, experiments performed in vitro and in several animal models of LV pressure overload show that VD supplements attenuate LV hypertrophy, reduce cardiac fibrosis and decrease the expression of collagen, fibronectin and transforming growth factor-β, along with an improvement of the systolic and diastolic function.37–40 The negative results of the PRIMO trial may have several causes. The main cause could be that the population selected was not ideal for the purpose of linking VD supplements and ameliorated CV health. Second, hypertension leads to myocardial remodelling over the years, and it seems difficult to modify this process in only 48 weeks of therapy. Another potential reason is that FGF-23 plasma levels were not taken into account. Indeed, it has recently been observed that low levels of VD were associated with increasing mass and diameter when coexisting with high levels of FGF-23.41 In accordance with this, we have recently reported that low levels of VD were predictors of poor outcome in coronary patients with FGF-23 plasma levels that were higher than the median value of 70 RU/mL, but they were not effective predictors if FGF-23 plasma levels were below the median.10 Other authors have shown similar data for the progression of chronic kidney disease.42 These data provide support for the notion that, in addition to being an independent marker of cardiovascular risk, FGF-23 plasma levels influence the effect of low VD levels. Finally, klotho plasma levels were not taken into account. This protein is a co-receptor for FGF-23, whose extracellular portion can be released and act as an endocrine substance with multiple functions. Low levels of klotho are related to kidney damage, as well as to vascular calcification and cardiac hypertrophy and fibrosis, causing klotho to be considered an antiageing protein.43 Thus, it is possible that in people without reduced glomerular filtrate, klotho levels are normal and could interfere with the hypertrophic effect of FGF-23. The fact that VD may increase klotho levels reinforces the possibility that this compound may have a protective cardiovascular effect.
In summary, there is substantial evidence demonstrating the negative effects of VD deficiency on the cardiovascular system, including the development of LV hypertrophy. Despite the negative results of VD supplements in previous clinical trials, the convincing evidence obtained in animal models in which it is shown that VD may protect the heart supports the need for a new clinical trial designed to take into account the most recent discoveries in the field. The VITamin D in Acute Myocardial Infarction (VITDAMI) trial has been designed as a proof-of-concept study to test the effect of VD supplements in patients with anterior ST-elevation myocardial infarction (STEMI). The reason is that a great part of the remodelling process following a large STEMI may be concentrated in the months following the acute event, making these patients probably the best human model for studying therapeutic interventions on ventricular remodelling. Moreover, when STEMI affects the anterior wall of the LV, it tends to be larger than in other locations, and remodelling is thus especially intensive in these cases. In this regard, in the METOCARD trial comparing early versus delayed β-blockade in patients with anterior STEMI,44 45 the control group showed an increase of 11.5% in mean LV end-diastolic volume and a decrease of 22.8% in mean LV mass at 6 months, along with a minimal increase of 2.2% in the ejection fraction. In addition, we will see if this effect occurs only in those patients with FGF-23 above the median or in all the study participants. Similarly, we will assess possible differences in the effect of VD in patients with klotho plasma levels above and below the median. Based on the ideas developed above, it is possible that benefits could be present only in patients with elevated levels of FGF-23, in those with klotho levels below the median or in both situations.
Methods
Study aim
To compare the effect of 1-year treatment with calcifediol 0.266 mg (equivalent to 15 960 units) soft gelatin capsules versus placebo on LV remodelling in patients with anterior STEMI.
Primary hypothesis
The oral administration of one calcifediol 0.266 mg soft gelatin capsule every 15 days to patients with anterior STEMI will reduce the presence of LV remodelling assessed by cardiac MRI, defined as an increase in LV end-diastolic volume of ≥10%, at 1 year as compared with the baseline assessment.
Secondary hypotheses
- Patients receiving calcifediol will show, as compared with those receiving placebo:
- Less increase in end-diastolic and end-systolic volumes;
- More increase in ejection fraction;
- Less decrease in diastolic sphericity index, defined as the ratio of long-axis to short-axis dimension of the LV cavity at end diastole;46
- Less increase in the area of fibrosis;
- Better diastolic function;
- Better endothelial function;
- A significant reduction in plasma levels of one or more of these biomarkers: N-terminal brain natriuretic peptide (NT-proBNP) and galectin-3, as related to heart failure and adverse prognosis; and monocyte chemoattractant protein-1 (MCP-1), related to inflammation and acute ischaemic events;47
- Higher plasma levels of calcidiol (25OH VD) and/or klotho, and lower levels of FGF-23 and/or PTH.
The results of the previous hypotheses will be more evident or even restricted to those patients with FGF-23>median and/or klotho<median plasma levels.
Since it is possible that calcidiol plasma levels are heterogeneous, patients will be also divided into three groups according to the tertiles of calcidiol plasma levels at 6 months to study if the hypotheses described in item 1 hold for patients in the highest versus lowest tertiles.
All analyses will be carried out comparing patients who received calcifediol and placebo as specified in the protocol, including those patients in whom calcifediol was stopped due to high plasma levels. On the other hand, patients giving up the study medication due to other reasons will be excluded from the analysis. The reason is that this is just a proof-of-concept study, where we try to demonstrate for the first time in human beings that taking VD supplements to reach normal calcidiol levels may decrease LV remodelling after a STEMI. On the other hand, we do not intend to show that anterior STEMI must be treated with VD, as a large clinical trial demonstrating reduction of clinical events would be necessary for this purpose.
Trial population
Patients between 40 and 85 years of age admitted at the hospital due to an anterior STEMI, who have received primary angioplasty, are ready to be discharged and who accept to participate and sign the informed consent are eligible for randomisation. STEMI is defined by suggestive symptoms, such as chest discomfort irradiated to the arms or jaw, or just compatible symptoms as sweating, nausea, vomiting or ill-defined malaise lasting more than 20 min, in association with persistent ECG ST elevation and subsequent release of biomarkers of myocardial necrosis with a standard curve.48 Diagnostic anterior ST elevation in absence of LV hypertrophy or left bundle-branch block is defined according to current guidelines as new ST elevation at the J point in at least two contiguous leads of ≥2 mm in V1–V6 in men, ≥1.5 mm in V2–V3 in women and/or ≥1 mm in the remaining anterior leads will be accepted.49 Exclusion criteria are listed in box 1. Recruitment will be competitive.
Box 1. Exclusion criteria.
Death or complications compromising patient survival (ie, cardiogenic shock) during the index event;
No primary angioplasty;
Impossibility to perform the desirable revascularisation (Severe stenoses (angiographic severity >70% or borderline with a positive intracoronary adenosine test) are allowed only in secondary vessels considered either not relevant by the investigator because of the small vessel diameter or distal lesion, or technically unfeasible due to vessel calcification or tortuosity);
Indication of cardiac transplant;
Surgical coronary revascularisation during the index event;
Revascularisation pending at the moment of discharge;
Complications that extend the patient’s stay at the hospital for more than 7 days;
Absence of akinetic area in the anterior wall of the left ventricle;
Previous myocardial infarction;
Valve prosthesis;
Aortic stenosis with mean gradient >25 mm Hg (Doppler) and stenosis of any other valve;
Moderate-to-severe valve regurgitation;
Cardiomyopathy (dilated, hypertrophic or restrictive);
Severe left ventricle hypertrophy (wall thickness ≥17 mm in men and ≥16 mm in women);
Conditions limiting survival;
Inflammatory or immune disease;
Estimated glomerular filtration rate <40 mL/min/1.73 m2;
Intolerance to vitamin D supplements;
Indication or patient's decision to take vitamin D or calcium;
-
Therapy with drugs that can interfere with absorption, distribution, metabolism or excretion of Vitamin D:
Antiepileptic (phenytoin, phenobarbital, primidone, other enzymatic inducers);
Cholestyramine, colestipol, orlistat;
Penicillins;
Laxatives as paraffin and mineral oil;
Digitalis;
Magnesium salts;
Verapamil;
Steroids;
Disorders that can interfere with the pharmacokinetics or pharmacodynamics of vitamin D: hepatic insufficiency, inflammatory bowel disease, sarcoidosis, tuberculosis or other granulomatous disorders;
Plasma calcium levels >10.5 mg/dL, history of hypercalciuria or calcium litiasis;
Contraindications for MRI: claustrophobic, pacemaker, defibrillators, resynchronisation devices or high probability that they need them during the study (among them, patients with an ejection fraction <30% at discharge);
Impossibility to follow the patients;
Difficult compliance of the therapy as estimated by the investigator;
Patient rejects to participate and/or does not sign the informed consent;
Pregnancy or lactation period;
Patients participating in another clinical trial.
Trial design
The VITDAMI trial is a randomised, multicentre, double-blind, placebo-controlled trial.
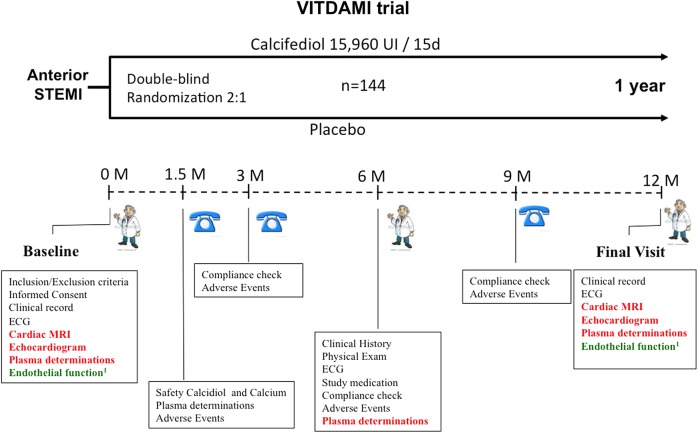
The protocol (V.2.1, 1 July 2015) has been approved by the corresponding Institutional Review Board (IRB) and the Spanish Drug Agency (AEMPS). One-hundred and forty-four patients with anterior STEMI will be included at cardiology departments of the participating sites in Spain that have been chosen because they have the equipment and programmes needed to care for patients with STEMI, along with the facility for cardiac MRI. After signing the informed consent, they will undergo cardiac examination by MRI and ECG, blood extraction for plasma storage, ECG and non-invasive endothelial function test (only in patients admitted to Fundación Jiménez Díaz; figure 1) as soon as possible and no later than 7 days after admission. Immediately after completing these tests, patients will be randomly assigned to receive on a 2:1, double-blind basis an oral dose of 0.266 mg of calcifediol or placebo every 15 days (±1 day) during 1 year. In addition to study treatment, patients will be managed according to standard clinical practice based on European guidelines for STEMI.48 Given that heterogeneity in calcidiol plasma levels may exist due to different baseline levels, a 2:1 instead of 1:1 randomisation has been chosen in order to allow comparing the outcomes across different ranges of calcidiol levels.
Figure 1.
Flow chart of the VITDAMI trial. (1) Only at Fundación Jiménez Díaz. STEMI, ST-elevation myocardial infarction; VITDAMI, VITamin D in Acute Myocardial Infarction.
Forty-five days after inclusion, blood will be extracted to perform a safety determination of calcidiol and calcium plasma levels, to adjust the dose of study medication according to the results. By phone contact, dose adjustment will be communicated to the patient and the appearance of potential adverse effects will be evaluated. At months 3 and 9, adverse effects will be checked by phone call. At month 6, patients will be seen by the investigator to rule out adverse effects and to collect empty blisters to confirm compliance with study medication, performing also a new blood extraction for study plasma determinations. At this time, they will be provided study medication for the last 6 months of the study. Finally, in month 12, procedures performed at inclusion will be repeated, and the study drug will be discontinued. One month after the last dose, a follow-up visit will be performed by phone contact to register any possible adverse events, and the study will be finished. Table 1 summarises the visit schedule.
Table 1.
Visit schedule
| V0 | V1 | V2 | V2 | V4 | V5 | V6 | |
|---|---|---|---|---|---|---|---|
| 0 m | 1.5 m | 3 m | 6 m | 9 m | 12 m | 13 m | |
| Inclusion/exclusion criteria | X | ||||||
| Informed consent | X | ||||||
| Clinical history | X | X | X | X | X | ||
| Concomitant medication | X | X | X | ||||
| Physical exam | X | X | X | ||||
| Heart rate and blood pressure | X | X | X | ||||
| Haemogram and biochemistry | X | X | X | ||||
| Chest roentgenogram | X | X | |||||
| ECG | X | X | X | ||||
| Calcidiol and calcium determination | X | ||||||
| Biological samples | X | X | X | ||||
| Cardiac MRI | X | X | |||||
| Echocardiogram | X | X | |||||
| Endothelial function* | X | X | |||||
| Dispense study medication/collect empty blisters | X | X | X | ||||
| Compliance check | X | X | X | X | X | ||
| Adverse events | X | X | X | X | X | X |
,.
*Only in Fundación Jiménez Díaz (FJD).
Patient recruitment started in November 2015 and the trial is expected to conclude in December 2017.
Randomisation and blinding
Patients will be randomly assigned to receive one calcifediol 0.266 mg soft gelatin capsule (Hidroferol SGC), or one soft capsule, containing placebo, every 15 days. Allocation ratio will be 2:1 and the randomisation scheme will be computer-generated by the statistician at the coordinating centre and block-balanced. Closed envelopes with the randomisation sequence will be prepared and distributed to the participating centres. Randomisation will be performed by the study investigators. Treatment allocation will be blind for patients and the research team. Unblinding will be allowed in case a patient suffers a serious adverse event if the attending medical team considers it necessary to preserve the patient's health.
Study medication
Hidroferol SGC will be used for this trial. This is a new formulation containing 0.266 mg of calcifediol (15 960 UI of VD) that improves bioavailability (22%) with respect to the liquid calcifediol immediate release oral formulation, due to its Self-Emulsifying Drug Delivery Systems (SEDDS) pharmaceutical technology.
Calcifediol and placebo capsules will be provided and labelled by FAES FARMA S.A. Laboratories to ensure the blindness of the study. Pharmacy departments at each centre will receive the study medication, and will keep a registry of the medication received, dispensed and stored. The medication will be stored in appropriate conditions and kept locked under restricted access. Any non-used study medication and all the empty packages will be stored until the end of the study and adequately destroyed locally afterwards.
Adherence to study medication will be evaluated by direct questions to the patient in each visit on how many doses he/she has omitted. In addition, this information will be checked with pharmacy registries to calculate the final adherence percentage.
Safety issues
At 1.5 months, a safety assessment of plasma calcidiol and calcium levels will be performed—after the intake of the first three doses—as by this time calcidiol is expected to reach its peak concentration. The study therapy will be adjusted following these rules:
Calcidiol >70 ng/mL or calcium >10.5 mg/dL: therapy will be stopped and the patient will continue to be followed.
Calcidiol 30–70 ng/mL and calcium ≤10.5 mg/dL: the dose of the study drug will be reduced to one capsule every month as a maintenance dose.
Calcidiol <30 ng/mL and calcium ≤10.5 mg/dL: the dose of the study drug will be kept at one capsule every 15 days.
Of interest, no baseline calcidiol measurement is performed, as this is deemed unnecessary due to different reasons. (1) In a previous study from our group on 704 patients with coronary artery disease,10 24 maximal calcidiol levels were 51 ng/mL, far from the upper normal limit of 70 ng/mL. (2) The dose chosen is well below the tolerable upper intake level of 4000 IU/day.50 51 (3) In the large VITAL clinical trial, in primary prevention, a dose of 2000 IU/day VD is being used for 5 years without assessing basal levels and performing only one safety determination of calcidiol levels in a small subgroup of patients.52
Criteria for study withdrawal
Patients may voluntarily leave the study at any time without giving any reason and with no consequences for their subsequent care. They will also be withdrawn from the study at investigator criteria for the following reasons: new myocardial infarction during treatment period (as it may influence LV remodelling), lost to follow-up, loss of the capacity to consent, safety concerns (ie, unexpected serious adverse events), failure to fulfil eligibility criteria and failure to collaborate or to comply with study procedures. Irrespective of the reason for withdrawal, efforts will be made by the investigator's team to perform the end of study visit and to register in the clinical records and case report form (CRF) as much information as possible until the ending of patient participation.
Trial procedures
Cardiac MRI
Comprehensive cardiac MRI will be carried out to study cardiac function, LV mass, myocardial oedema and myocardial fibrosis/necrosis. Scans will be performed with 1.5 T equipments at each participating centre. For assessment of global and segmental left and right ventricular function, and LV mass, balanced steady-state free precession with sensitivity encoding the fast parallel imaging technique (True FISP) sequence will be used for cine imaging. Images will be obtained at short axis (8 mm slices from the apex to the base of the left ventricle), four-chamber, two-chamber and three-chamber. Myocardial oedema will be assessed matching the slice position of the cine images, using a T2-weighted triple IR turbo spin echo (STIR) sequence. For study of fibrosis/myocardial necrosis, a gadolinium-based contrast agent will be intravenously administered. Delayed enhancement imaging to assess necrotic myocardium will be performed using IR Turbo-FLASH (3D-IR-GRE, 2D-IR-GRE and PSIR sequences).
The necrotic/fibrotic area is defined as an area with delayed gadolinium uptake (high-intensity STIR signals) and myocardium at risk as an area with oedema. Salvaged myocardium is assessed as the difference between myocardium at risk and the necrotic area. Myocardium at risk, the necrotic size and the salvaged myocardium will be expressed as percentage of the total LV mass. In addition, the necrotic area will be also expressed in grams. All the results will be given in absolute numbers and normalised by body surface area. LV end-diastolic and end-systolic volumes, as well as the ejection fraction and the LV sphericity index (maximal long axis/short axis of LV cavity at end diastole), will be assessed.46 Finally, microvascular obstruction, a parameter related to cardiac remodelling,53 will be assessed at the initial MRI exploration. MRI studies will be analysed blinded to treatment allocation at a central core laboratory located at the Centro Nacional de Investigaciones Cardiovasculares Carlos III with the QMass system (V.7.6). Fifteen per cent of the MRI studies will be randomly chosen to perform interobserver and intraobserver variability.
Doppler-ECG
This technique will be performed and interpreted at the centre where the patient is included. Apical four-chamber and two-chamber views as well as long-axis and short-axis parasternal views will be used. Bidimensional and M-mode echocardiography will be used to analyse diastolic and systolic diameters of the LV, septal and posterior wall thickness, ejection fraction (Simpson method), segmental contractility using a 17-segment model and registering areas of akinesia, dyskinesia and hypokinesia. Diastolic function will be assessed by analysing the deceleration time (ms), peak E and A waves (cm/s), E/A ratio, and the isovolumetric relaxation time (ms) by pulsed Doppler, and E′ (cm/s) and A′ (cm/s) waves by tissue Doppler imaging.
Endothelial function test
The ENDOPAT technology will be used, measuring changes of finger arterial pulsatile volume (reactive hyperaemia plethysmographic biosensors). This test will be carried out in the subgroup of patients at the Fundación Jiménez Díaz. Given that this group will have a small sample size, subgroup analysis will not be performed and only comparisons between both groups of therapy will be carried out.
Blood extractions and assessments
At blood withdrawal, 26 mL will be obtained, from which 18 mL will be placed in EDTA tubes and 8 mL in tubes without EDTA. Blood will undergo centrifugation for 10 min at 2.500 G and the obtained plasma will be stored in 2 mL cryovials at −80°C. Half of these samples will be stored at Instituto de Investigación Sanitaria Fundación Jiménez Díaz (IIS-FJD) and the other half at Móstoles University Hospital to limit the probabilities of damaging the samples in case of failure of the freezer. Nevertheless, both freezers have a CO2 release system and telephonic alarm in cases of malfunction of the system. The study of mineral metabolism will be performed at the laboratory of renal function at Gómez-Ulla Hospital, and the remaining determinations will be carried out at the laboratories of biochemistry and vascular pathology at Fundación Jiménez Díaz. Calcidiol levels will be quantified using chemiluminescent immunoassay with LIAISON XLanalyser (total VD Assay DiaSorin, Saluggia, Italy). FGF-23 will be assessed by an ELISA that recognises epitopes in the terminal portion carboxyl terminus of FGF-23 (Human FGF-23, C-Term, Immutopics, San Clemente, California, USA), klotho will be studied by ELISA (soluble α-klotho ELISA, IBL International, Hamburg, Germany), intact PTH by an automated chemiluminescent method of second generation (2010 platform Elecsys, Roche Diagnostics, Mannheim, Germany) and P will be assessed by enzymatic method (Integra 400 analyser, Roche Diagnostics, Mannheim, Germany). NT-proBNP levels will be determined by immunoassay (VITROS, Orthoclinical Diagnostics, USA), high-sensitivity C reactive proteins by immunoturbidimetric latex and determinations of lipids, glucose and creatinine will be carried out by standard methods (ADVIA 2400 Chemistry System, Siemens, Germany). Plasma levels of MCP-1 and galectin-3 will be determined in duplicate using commercially available ELISA kits (BMS279/2, Bender MedSystems, Burlingame, California; and DCP00, R&D Systems, Minneapolis, Minnesota). Albumin and calcium will be assessed by standard methods (ADVIA 2400 Chemistry System, Siemens, Germany).
Finally, if the patient consents, the remaining plasma samples will be stored in a registered collection (Instituto de Salud Carlos III, C.0003386) for future determinations of plasma levels of other molecules that may be potentially related to the other variables assessed, such as mineral metabolism or LV remodelling.
Trial outcomes
Main outcome: Proportion of patients who develop LV remodelling defined as an increase of ≥10% in the end-diastolic volume measured by cardiac MRI at the end of the study as compared with the baseline assessment.
Secondary outcomes
Per cent change in LV end-diastolic volume;
Per cent change in LV end-systolic volume;
Per cent change in ejection fraction;
Per cent change in sphericity index;
Per cent change in size of the necrotic/fibrotic area, defined as delayed gadolinium uptake (high-intensity STIR signals);
Per cent change in LV mass;
Per cent change in endothelial function;
Per cent change in diastolic function as assessed by flow and tissue Doppler;
Adverse events rate and description;
Compliance rate;
Incidence of heart failure, death or any acute coronary syndrome (STEMI or non-ST-elevation acute coronary syndrome);
- Levels of the following biomarkers in plasma will be measured at 6 and 12 months:
- NT-proBNP, galectin-3, MCP-1 and high sensitive-C reactive protein;
- Calcidiol, FGF-23, PTH, P and klotho.
In addition to comparing the changes in the final versus the baseline assessment of all the mentioned variables, we will also compare the results obtained in the final visit between both treatment groups.
Also, assessment of main and secondary outcomes will be performed in the following subgroup of patients:
FGF-23 plasma levels above and below the median;
Klotho plasma levels above and below the median;
Estimated glomerular filtration rate above and below 60 mL/min/1.73 m2;
Different tertiles of calcidiol plasma levels. Also, prespecified cut-off levels will be set 10, 15 and 20 ng/mL plasma levels;
Different degrees of microvascular obstruction at baseline MRI;
With/without thrombectomy at primary angioplasty;
In patients who achieve TIMI III flow at primary angioplasty.
Statistical considerations
Sample size
As there are no published data on the effect of VD on LV remodelling in patients with STEMI, a formal sample size calculation based on the expected effect for the primary end point has not been performed. From this point of view, the trial can be considered exploratory for the primary outcome. First, we defined as remodelling an increase in 10% of LV end-diastolic volume, given that according to previous studies this value is above the observed intraobserver and interobserver variability for this parameter in cardiac MRI.54 Then the probability that a variation higher than 10% in the final study as compared with the baseline is due to observational variability is very low. Then we reviewed data from the METOCARD study,44 comparing early versus delayed β-blockade in a similar population, and observed that 52% of patients from the group of conventional β-blockade developed this outcome at 6 months. Given that we expect this number to be higher at 1 year, we believe that a reduction of 24% in the number of patients is a reasonable target if VD really has a positive effect. With these numbers, we estimate that 120 patients are needed to have a power of 80% (1−β=0.8) using a two-sided test with a level of significance α=0.05, assuming that the LV end-diastolic volume measured by MRI is normally distributed.
To have 120 cases suitable for analysis, we have estimated that it is necessary to include a total of 144 patients. With this sample size, considering that mortality in the first year after a STEMI may be up to 5%,55 and taking into account that we have observed 2.6% of incidence of recurrent non-fatal myocardial infarctions during this period in our patients (unpublished data), we will have 11 patients not completing the trial, leaving 133 patients. In addition, we estimate that up to 10% of these patients could give up the study for other reasons, then leading 120 patients for analysis.
Endothelial function will be assessed only in one centre. However, information regarding endothelial function is available from one previous study by Tarcin et al.56 The authors describe that flow-mediated vasodilation increases significantly from 7.0±3.2% to 10.4±3.3% after treatment with VD. Assuming that similar differences will be observed in our study, 33 participants would be enough to have a power of 80% with a two-sided level of significance α=0.05.
Statistical analysis
Analyses of treatment effect will be performed as per protocol. No interim analyses will be performed, given the short duration and the limited sample used in this proof-of-concept study. A descriptive analysis of baseline characteristics of patients included in both groups will be performed, to ensure that they are comparable. Qualitative variables will be described as absolute numbers and percentages. Quantitative variables with normal distribution (tested by the Kolmogorov-Smirnov test) will be reported as mean (SD), and those that do not follow a normal distribution will be described as median (IQR).
To compare quantitative variables between the VD and the placebo groups, Student's t-test will be used in case data are normally distributed. In case distribution is not normal, the Mann-Whitney test will be performed. For the comparison of baseline versus end of treatment values, the paired t-test will be used for normally distributed data and the Wilcoxon test will be carried out if normal distribution cannot be demonstrated. For qualitative variables, χ2 test will be performed.
Also, differences in the same parameters will be assessed among the groups defined by plasma calcidiol tertiles. For quantitative data, one-way analysis of variance (ANOVA) followed by post hoc tests will be used in cases of normal distribution. The Kruskal-Wallis test followed by Mann-Whitney tests will be performed if the distribution is not normal. Qualitative analyses will be performed by χ2 test.
Interobserver variability will be assessed by the estimation of intraclass correlation coefficients. Analyses will be considered significant when ‘p’<0.05 (two-tailed). Analyses will be performed with the SPSS V.19.0 statistical package.
Ethics and dissemination
Any relevant amendments to the protocol will be adequately submitted for evaluation to the corresponding institutions and properly communicated to relevant parties after approval. Patient confidentiality will be warranted according to Spanish data protection laws. In the CRF and any other of the trial documents, patients will be identified by a numeric code and will not contain any personal information that could allow identification.
We have contracted liability insurance to cover the patients from potential adverse consequences secondary to their participation in the trial.
All patients must sign an informed consent form before participating and keep a copy for their records. Investigators are responsible for obtaining written informed consent from each individual participating in this study after adequate explanation of the aims, methods, objectives and potential hazards of the study. It should be made clear that refusal to participate or withdrawal from the trial at any stage will have no consequences on the patient’s subsequent care. A specific section to consent for the storage of biological samples is included in the informed consent form. Clinical Trial Pharmacovigilance and Monitoring will be performed by the Spanish Clinical Research Network (SCReN) every 6 months, reviewing CRF and confirming that they only include data registered at the patient’s hospital clinical records. The results of the study will be submitted to indexed medical journals and presented at national and international meetings. The trial is registered in ClinicalTrials.gov (NCT02548364) and the EU Clinical Trials Register (EudraCT 2014-004512-11).
Conclusions
The VITDAMI trial is the first exploratory trial to evaluate the effect of VD treatment on myocardial remodelling in patients with anterior STEMI and preserved renal function. Furthermore, it will be the first study to analyse the influence of other components of mineral metabolism, such as FGF-23 and klotho levels, on the effect of VD. The results, expected by December 2017, will most likely contribute to our understanding of the complex role of VD and other components of mineral metabolism in cardiovascular diseases. If the trial is successful, a large-scale study should be performed to see if the improvement in cardiac remodelling translates into clinical benefits.
Acknowledgments
The authors are indebted to Oliver Shaw (IIS-Fundación Jiménez Díaz, Madrid, Spain) for his assistance in editing this work.
Footnotes
Contributors: JT, EG-P and JE conceived the study. All authors participated in the development of the protocol. JT, IG-H and LL-J raised the manuscript. All other authors revised the manuscript for relevant scientific content. All authors approved the final version of the manuscript.
Funding: The VITDAMI trial is an investigator initiated study, sponsored by the Instituto de Investigación Sanitaria Fundación Jiménez Díaz (IIS-FJD). Funding has been obtained from Fondo de Investigaciones Sanitarias (PI14/01567; http://www.isciii.es/) and Spanish Society of Cardiology (http://secardiologia.es/). In addition, the study medication has been provided freely by the pharmaceutical Company FAES FARMA S.A. (Leioa, Vizcaya, Spain; http://faesfarma.com/). This company was the only funder who collaborated in study design (IG-H).
Competing interests: JE has been a lecturer for Abbott Spain.
Patient consent: Obtained.
Ethics approval: This trial has been already approved by the corresponding Institutional Review Boards and the National Competent Authority (Agencia Española de Medicamentos y Productos Sanitarios; AEMPS). Regional Ethics Committee of the Community of Madrid.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: In addition to the paper and the protocol, the informed consent documents and case report forms are available on request.
References
- 1.Wolf M. Forging forward with 10 burning questions on FGF23 in kidney disease. J Am Soc Nephrol 2010;21:1427–35. 10.1681/ASN.2009121293 [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez-Parra E, Tuñón J, Egido J et al. . Phosphate: a stealthier killer than previously thought? Cardiovasc Pathol 2012;21:372–81. 10.1016/j.carpath.2012.02.008 [DOI] [PubMed] [Google Scholar]
- 3.Larsson T, Nisbeth U, Ljunggren O et al. . Circulating concentration of FGF-23 increases as renal function declines in patients with chronic kidney disease, but does not change in response to variation in phosphate intake in healthy volunteers. Kidney Int 2003;64:2272–9. 10.1046/j.1523-1755.2003.00328.x [DOI] [PubMed] [Google Scholar]
- 4.Faul C, Amaral AP, Oskouei B et al. . FGF23 induces left ventricular hypertrophy. J Clin Invest 2011;121:4393–408. 10.1172/JCI46122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker BD, Schurgers LJ, Brandenburg VM et al. . The associations of fibroblast growth factor 23 and uncarboxylated matrix Gla protein with mortality in coronary artery disease: the Heart and Soul Study. Ann Intern Med 2010;152:640–8. 10.7326/0003-4819-152-10-201005180-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mirza MA, Larsson A, Lind L et al. . Circulating fibroblast growth factor-23 is associated with vascular dysfunction in the community. Atherosclerosis 2009;205:385–90. 10.1016/j.atherosclerosis.2009.01.001 [DOI] [PubMed] [Google Scholar]
- 7.Mirza MA, Hansen T, Johansson L et al. . Relationship between circulating FGF23 and total body atherosclerosis in the community. Nephrol Dial Transplant 2009;24:3125–31. 10.1093/ndt/gfp205 [DOI] [PubMed] [Google Scholar]
- 8.Masai H, Joki N, Sugi K et al. . A preliminary study of the potential role of FGF-23 in coronary calcification in patients with suspected coronary artery disease. Atherosclerosis 2013;226:228–33. 10.1016/j.atherosclerosis.2012.10.045 [DOI] [PubMed] [Google Scholar]
- 9.Ärnlöv J, Carlsson AC, Sundström J et al. . Higher fibroblast growth factor-23 increases the risk of all-cause and cardiovascular mortality in the community. Kidney Int 2013;83:160–6. 10.1038/ki.2012.327 [DOI] [PubMed] [Google Scholar]
- 10.Tuñón J, Cristóbal C, Tarín N et al. . Coexistence of low vitamin D and high fibroblast growth factor-23 plasma levels predicts an adverse outcome in patients with coronary artery disease. PLoS ONE 2014;9:e95402 10.1371/journal.pone.0095402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kestenbaum B, Katz R, de Boer I et al. . Vitamin D, parathyroid hormone, and cardiovascular events among older adults. J Am Coll Cardiol 2011;58:1433–41. 10.1016/j.jacc.2011.03.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor EN, Curhan GC, Forman JP. Parathyroid hormone and the risk of incident hypertension. J Hypertens 2008;26:1390–4. 10.1097/HJH.0b013e3282ffb43b [DOI] [PubMed] [Google Scholar]
- 13.Anderson JL, Vanwoerkom RC, Horne BD et al. . Parathyroid hormone, vitamin D, renal dysfunction, and cardiovascular disease: dependent or independent risk factors? Am Heart J 2011;162:331–9. 10.1016/j.ahj.2011.05.005 [DOI] [PubMed] [Google Scholar]
- 14.Saleh FN, Schirmer H, Sundsfjord J et al. . Parathyroid hormone and left ventricular hypertrophy. Eur Heart J 2003;24:2054–60. 10.1016/j.ehj.2003.09.010 [DOI] [PubMed] [Google Scholar]
- 15.Aceña A, Pello AM, Carda R et al. . Parathormone levels are independently associated with the presence of left ventricular hypertrophy in patients with coronary artery disease. J Nutr Health Aging 2016;20:659–64. 10.1007/s12603-015-0649-y [DOI] [PubMed] [Google Scholar]
- 16.Hagström E, Hellman P, Larsson TE et al. . Plasma parathyroid hormone and the risk of cardiovascular mortality in the community. Circulation 2009;119:2765–71. 10.1161/CIRCULATIONAHA.108.808733 [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-Parra E, Rojas-Rivera J, Tuñón J et al. . VD receptor activation and cardiovascular disease. Nephrol Dial Transplant 2012;27(Suppl 4):iv17–21. 10.1093/ndt/gfs534 [DOI] [PubMed] [Google Scholar]
- 18.Watson KE, Abrolat ML, Malone LL et al. . Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation 1997;96:1755–60. 10.1161/01.CIR.96.6.1755 [DOI] [PubMed] [Google Scholar]
- 19.Syal SK, Kapoor A, Bhatia E et al. . Vitamin D deficiency, coronary artery disease, and endothelial dysfunction: observations from a coronary angiographic study in Indian patients. J Invasive Cardiol 2012;24:385–9. [PubMed] [Google Scholar]
- 20.Scragg R, Jackson R, Holdaway IM et al. . Myocardial infarction is inversely associated with plasma 25-hydroxyvitamin D3 levels: a community-based study. Int J Epidemiol 1990;19:559–63. 10.1093/ije/19.3.559 [DOI] [PubMed] [Google Scholar]
- 21.Lavie CJ, Lee JH, Milani RV. Vitamin D and cardiovascular disease will it live up to its hype? J Am Coll Cardiol 2011;58:1547–56. 10.1016/j.jacc.2011.07.008 [DOI] [PubMed] [Google Scholar]
- 22.de Borst MH, Vervloet MG, ter Wee PM et al. . Cross talk between the renin-angiotensin-aldosterone system and VD-FGF-23-klotho in chronic kidney disease. J Am Soc Nephrol 2011;22:1603–9. 10.1681/ASN.2010121251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Assalin HB, Rafacho BP, dos Santos PP et al. . Impact of the length of vitamin D deficiency on cardiac remodeling. Circ Heart Fail 2013;6:809–16. 10.1161/CIRCHEARTFAILURE.112.000298 [DOI] [PubMed] [Google Scholar]
- 24.González-Parra E, Aceña A, Lorenzo O et al. . Important abnormalities of bone mineral metabolism are present in patients with coronary artery disease with a mild decrease of the estimated glomerular filtration rate. J Bone Min Metab 2105. [Epub ahead of print 23 Aug 2015]. [DOI] [PubMed] [Google Scholar]
- 25.Karakas M, Thorand B, Zierer A et al. . Low levels of serum 25-hydroxyvitamin D are associated with increased risk of myocardial infarction, especially in women: results from the MONICA/KORA Augsburg case-cohort study. J Clin Endocrinol Metab 2013;98:272–80. 10.1210/jc.2012-2368 [DOI] [PubMed] [Google Scholar]
- 26.Joergensen C, Gall MA, Schmedes A et al. . Vitamin D levels and mortality in type 2 diabetes. Diabetes Care 2010;33:2238–43. 10.2337/dc10-0582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melamed ML, Muntner P, Michos ED et al. . Serum 25-hydroxyvitamin D levels and the prevalence of peripheral arterial disease: results from NHANES 2001 to 2004. Arterioscler Thromb Vasc Biol 2008;28:1179–85. 10.1161/ATVBAHA.108.165886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang TJ, Pencina MJ, Booth SL et al. . Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008;117:503–11. 10.1161/CIRCULATIONAHA.107.706127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giovannucci E, Liu Y, Hollis BW et al. . 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med 2008;168:1174–80. 10.1001/archinte.168.11.1174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dobnig H, Pilz S, Scharnagl H et al. . Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxy VD levels with all-cause and cardiovascular mortality. Arch Intern Med 2008;168:1340–9. 10.1001/archinte.168.12.1340 [DOI] [PubMed] [Google Scholar]
- 31.Pilz S, Dobnig H, Nijpels G et al. . Vitamin D and mortality in older men and women. Clin Endocrinol (Oxf) 2009;71:666–72. 10.1111/j.1365-2265.2009.03548.x [DOI] [PubMed] [Google Scholar]
- 32.Poole KE, Loveridge N, Barker PJ et al. . Reduced Vitamin D in acute stroke. Stroke 2006;37:243–5. 10.1161/01.STR.0000195184.24297.c1 [DOI] [PubMed] [Google Scholar]
- 33.Wang L, Song Y, Manson JE et al. . Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: a meta-analysis of prospective studies. Circ Cardiovasc Qual Outcomes 2012;5:819–29. 10.1161/CIRCOUTCOMES.112.967604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grandi NC, Breitling LP, Brenner H. Vitamin D and cardiovascular disease: systematic review and meta-analysis of prospective studies. Prev Med 2010;51:228–33. 10.1016/j.ypmed.2010.06.013 [DOI] [PubMed] [Google Scholar]
- 35.Brøndum-Jacobsen P, Benn M, Jensen GB et al. . 25-hydroxyvitamin d levels and risk of ischemic heart disease, myocardial infarction, and early death: population-based study and meta-analyses of 18 and 17 studies. Arterioscler Thromb Vasc Biol 2012;32:2794–802. 10.1161/ATVBAHA.112.248039 [DOI] [PubMed] [Google Scholar]
- 36.Thadhani R, Appelbaum E, Pritchett Y et al. . Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. JAMA 2012;307:674–84. 10.1001/jama.2012.120 [DOI] [PubMed] [Google Scholar]
- 37.Wu J, Garami M, Cheng T et al. . 1,25(OH)2 VD3, and retinoic acid antagonize endothelin-stimulated hypertrophy of neonatal rat cardiac myocytes. J Clin Invest 1996;97:1577–88. 10.1172/JCI118582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bodyak N, Ayus JC, Achinger S et al. . Activated vitamin D attenuates left ventricular abnormalities induced by dietary sodium in Dahl salt-sensitive animals. Proc Natl Acad Sci USA 2007;104:16810–15. 10.1073/pnas.0611202104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meems LM, Cannon MV, Mahmud H et al. . The vitamin D receptor activator paricalcitol prevents fibrosis and diastolic dysfunction in a murine model of pressure overload. J Steroid Biochem Mol Biol 2012;132:282–9. 10.1016/j.jsbmb.2012.06.004 [DOI] [PubMed] [Google Scholar]
- 40.Koleganova N, Piecha G, Ritz E et al. . Calcitriol ameliorates capillary deficit and fibrosis of the heart in subtotally nephrectomized rats. Nephrol Dial Transplant 2009;24:778–87. 10.1093/ndt/gfn549 [DOI] [PubMed] [Google Scholar]
- 41.Ky B, Shults J, Keane MG et al. . CRIC Study Investigators. FGF23 modifies the relationship between vitamin D and cardiac remodeling. Circ Heart Fail 2013;6:817–24. 10.1161/CIRCHEARTFAILURE.112.000105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakano C, Hamano T, Fujii N et al. . Combined use of vitamin D status and FGF23 for risk stratification of renal outcome. Clin J Am Soc Nephrol 2012;7:810–19. 10.2215/CJN.08680811 [DOI] [PubMed] [Google Scholar]
- 43.Hu MC, Kuro-o M, Moe OW. Renal and extrarenal actions of klotho. Semin Nephrol 2013;33:118–29. 10.1016/j.semnephrol.2012.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pizarro G, Fernández-Friera L, Fuster V et al. . Long-term benefit of early pre-reperfusion metoprolol administration in patients with acute myocardial infarction: results from the METOCARD-CNIC trial (Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction). J Am Coll Cardiol 2014;63:2356–62. 10.1016/j.jacc.2014.03.014 [DOI] [PubMed] [Google Scholar]
- 45.Ibáñez B, Macaya C, Sánchez-Brunete V et al. . Effect of early metoprolol on infarct size in ST-segment-elevation myocardial infarction patients undergoing primary percutaneous coronary intervention: the Effect of Metoprolol in Cardioprotection During an Acute Myocardial Infarction (METOCARD-CNIC) trial. Circulation 2013;128:1495–503. 10.1161/CIRCULATIONAHA.113.003653 [DOI] [PubMed] [Google Scholar]
- 46.van Dalen BM, Kauer F, Vletter WB et al. . Influence of cardiac shape on left ventricular twist. J Appl Physiol 2010;108:146–51. 10.1152/japplphysiol.00419.2009 [DOI] [PubMed] [Google Scholar]
- 47.Tuñón J, Blanco-Colio L, Cristóbal C et al. . Usefulness of a combination of monocyte chemoattractant protein-1, galectin-3, and N-terminal probrain natriuretic peptide to predict cardiovascular events in patients with coronary artery disease. Am J Cardiol 2014;113:434–40. 10.1016/j.amjcard.2013.10.012 [DOI] [PubMed] [Google Scholar]
- 48.Thygesen K, Alpert JS, Jaffe AS et al. . Third universal definition of myocardial infarction. Circulation 2012;126:2020–35. 10.1161/CIR.0b013e31826e1058 [DOI] [PubMed] [Google Scholar]
- 49.Steg PG, James SK, Atar D et al. , Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–619. 10.1093/eurheartj/ehs215 [DOI] [PubMed] [Google Scholar]
- 50.Ross AC, Manson JE, Abrams SA et al. . The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of medicine: what clinicians need to know. J Clin Endocrinol Metab 2011;96:53–8. 10.1210/jc.2010-2704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hathcock JN, Shao A, Vieth R et al. . Risk assessment for vitamin D. Am J Clin Nutr 2007;85:6–18. [DOI] [PubMed] [Google Scholar]
- 52.Manson JE, Bassuk SS, Lee IM et al. . The VITamin D and OmegA-3 TriaL (VITAL): rationale and design of a large randomized controlled trial of vitamin D and marine omega-3 fatty acid supplements for the primary prevention of cancer and cardiovascular disease. Contemp Clin Trials 2012;33:159–71. 10.1016/j.cct.2011.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Romero J, Lupercio F, Díaz JC et al. . Microvascular obstruction detected by cardiac MRI after AMI for the prediction of LV remodeling and MACE: a meta-analysis of prospective trials. Int J Cardiol 2015;202:344–8. 10.1016/j.ijcard.2015.08.197 [DOI] [PubMed] [Google Scholar]
- 54.Luijnenburg SE, Robbers-Visser D, Moelker A et al. . Intra-observer and interobserver variability of biventricular function, volumes and mass in patients with congenital heart disease measured by CMR imaging. Int J Cardiovasc Imaging 2010;26:57–64. 10.1007/s10554-009-9501-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.López-Sendón JL, González-Juanatey JR, Pinto F et al. . Quality markers in cardiology: measures of outcomes and clinical practice-a perspective of the Spanish Society of Cardiology and of Thoracic and Cardiovascular Surgery. Eur Heart J 2016;37:12–23. 10.1093/eurheartj/ehv527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tarcin O, Yavuz DG, Ozben B et al. . Effect of vitamin D deficiency and replacement on endothelial function in asymptomatic subjects. J Clin Endocrinol Metab 2009;94:4023–30. 10.1210/jc.2008-1212 [DOI] [PubMed] [Google Scholar]