Abstract
Objective:
Atypical femoral fractures (AFFs) are important to diagnose early to avoid progression to complete fracture. We set out to determine the reporting accuracy of AFFs.
Methods:
We conducted a retrospective analysis of imaging performed between November 2010 and June 2013 to analyse the X-ray reporting of AFFs and to describe the key clinical considerations. Radiological reports were reviewed from the 3805 separate femoral images for search terms thought likely to identify AFFs. This identified 1558 patients. The identified radiographs were reviewed by radiologists with reference to the 2010 American Society of Bone and Mineral Research (ASBMR) criteria.
Results:
Within these 1558 patients, 16 patients met the radiological criteria for AFF according to the 2010 ASBMR task force statement of which, although all were identified as fractures, 15 were not reported as “atypical” by the original reporting author and none was formally classified as AFF by the original reporting author. Within the 1558 patients, there were an additional 17 patients labelled as having “atypical” fracture features originally, although only 1 patient met the 2010 ASBMR task force criteria for AFF. Only 13 of 16 patients had imaging of the contralateral femur, and there was a significant delay for those who were imaged (111 ± 44 days). Furthermore, two of the patients with an AFF had previous radiographs demonstrating cortical changes indicative of AFFs prior to formal diagnosis.
Conclusion:
Whilst AFFs are rare diagnoses, the compliance with published guidelines for their radiological classification is low.
Advances in knowledge:
We have raised awareness of the importance of recognizing AFFs to guide management.
INTRODUCTION
Osteoporotic fractures cost the National Health Service £1.73 billion per year. Furthermore, they are associated with significant morbidity and mortality with a fractured neck of femur carrying a 1-year mortality rate of around 30%1 and a risk of requiring nursing home care of 10–20%. The use of antiresorptive agents such as bisphosphonates and denosumab is associated with a reduction in hip fracture risk of 14%2 and 40%,3 respectively, although a recent systematic review suggests a greater risk reduction.4 In recent years, complications of the use of antiresorptive drugs have become more apparent. Whilst these drugs reduce fracture risk, there is an increasing body of data showing that they are associated with an increased risk of atypical femoral fractures (AFFs).5 However, this risk remains extremely low with one large series reporting an increase in absolute risk of 5 cases per 10,000 patient years of bisphosphonate use.6 Therefore, the risk–benefit ratio favours antiresorptive use for those at risk of osteoporotic fracture, whilst it remains important that this rare complication of antiresorptive use is recognized promptly and managed appropriately. The purpose of our work was to improve awareness of the radiological features of AFFs to allow early and appropriate imaging to guide management.
AFFs are so named because they affect the subtrochanteric or diaphyseal region, which is the strongest point of the bone. Whilst the aetiopathogenesis remains poorly understood, research in both human and animal subjects suggests that the suppression of the repair of microdamage, deregulated collagen deposition promoting brittleness and a lack of plasticity as well as hypermineralization contribute to increased fracture risk.7,8 Additionally, there is likely to be a significant biomechanical contribution to delayed healing either by micromotion at the early fracture site9 or from the hip geometry.10
The American Society of Bone and Mineral Research (ASBMR) issued their first consensus report concerning AFFs in 2010,11 which has subsequently been updated.12 The diagnostic criteria defining AFFs have changed between the two task force publications (Table 1). In 2010, to diagnose an AFF, all five major criteria must be met.11 In the more recent task force statements, four of five of the new major criteria are required with supporting evidence taken from the minor criteria.12 Despite these publications, there remains a degree of uncertainty in the reporting of AFFs. Not all patients with AFFs experience prodromal pain, and AFFs are often slow to heal13 and often bilateral.11 It is therefore crucial that patients with AFFs are managed jointly by orthopaedic surgeons and physicians with an interest in metabolic bone disease. As the term AFF now refers to a distinct subset of femoral fractures identified according to these criteria, fractures that are not AFFs but show unusual features should instead be called unusual femoral fractures to differentiate between these two femoral fracture subtypes. Radiographically, AFFs are classically located along the lateral cortex of the femoral shaft below the level of the lesser trochanter. This is an unusual location, as the weight-bearing medial cortex of the femoral neck is involved in stress fractures and the medial femoral shaft is involved in insufficiency fractures. The purpose of this study was to highlight AFFs as a distinct and separate diagnostic entity to the more common “insufficiency” and “stress” fractures of the femur, with a specific cause and different treatment implications. We also endeavour to highlight the early radiographic signs of subtle lateral cortical thickening at a typical subtrochanteric location along the lateral femoral cortex to allow early diagnosis, and the need for imaging the contralateral femur if these are detected.
Table 1.
The atypical femoral fracture (AFF) diagnostic criteria as determined by the American Society of Bone and Mineral Research (ASMBR) task force statements (2010 and 2014)
| 2010 ASMBR task force case definition of AFFs |
2014 ASMBR task force revised case definition of AFFs |
|---|---|
| 2010 Major features | 2014 Major features |
| • Located anywhere along the femur from just distal to the lesser trochanter to just proximal to the supracondylar flare |
• The fracture is associated with minimal or no trauma, as in fall from a standing height or less |
| • Associated with no trauma or minimal trauma, as in falling from a standing height or less |
• The fracture line originates at the lateral cortex and is substantially transverse in its orientation, although it may become oblique as it progresses medially across the femur |
| • Transverse or short oblique configuration | • Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex |
| • Non-comminuted | • The fracture is non-comminuted or minimally comminuted |
| • Complete fractures extend through both cortices and may be associated with a medial spike; incomplete fractures involve only the lateral cortex |
• Localized periosteal or endosteal thickening of the lateral cortex is present at the fracture site (“beaking” or “flaring”) |
| 2010 ASMBR Minor features | 2014 ASMBR Minor features |
| • Localized periosteal reaction of the lateral cortex | • Generalized increase in cortical thickness of the femoral diaphyses |
| • Generalized increase in cortical thickness of the diaphysis | • Unilateral or bilateral prodromal symptoms such as dull or aching pain in the groin or thigh |
| • Prodromal symptoms such as dull or aching pain in the groin or thigh | • Bilateral incomplete or complete femoral diaphysis fractures |
| • Bilateral fractures and symptoms | • Delayed fracture healing |
| • Delayed healing | • To satisfy the case definition of AFF, the fracture must be located along the femoral diaphysis from just distal to the less trochanter to just proximal to the supracondylar flare |
| • Comorbid conditions (e.g. vitamin D deficiency, rheumatoid arthritis, hypophosphatasia) |
|
| • Use of pharmaceutical agents (e.g. bisphosphonates, glucocorticoids, proton pump inhibitors) |
The principal aims of the present study were to examine the ability of radiologists to identify and appropriately describe AFFs, to ascertain whether those patients who were identified were referred for further appropriate management and to raise awareness of the criteria for AFFs amongst those dealing with patients with suspected femoral fractures. The secondary aim was to examine the clinical and management features of these patients to add to the growing literature about this rare consequence of antiresorptive use with a particular focus on management within the metabolic bone clinic.
METHODS AND MATERIALS
We conducted a retrospective analysis of all femoral radiographs between November 2010 and June 2013. The dates chosen include the period following the publication of the 2010 task force report and prior to the most up-to-date report.11,12 The radiological reports of the 3805 radiographs identified were analysed for the following search terms, “subtrochanteric fracture”, “shaft fracture”, ”diaphysis fracture”, “diaphyseal fracture”, “shaft of the femur”, “insufficiency fracture”, “stress fracture” with or without the terms “ femur” or ”femoral.” This identified 1558 patients. These patients' images were then reviewed by musculoskeletal radiologists (KH and SC) who were blinded to the clinical data. All radiological diagnoses of AFF were unanimous between reporting radiologists and were according to the 2010 ASBMR criteria (Table 1).11
Clinical data were extracted from the electronic patient record using in-house information technology systems. Data identified included demographics, comorbidities, drug history and the fracture management strategy employed.
RESULTS
3805 femoral images were obtained. Of these, 1558 patients were identified based on the above search terms. Of these, 16 patients had AFFs according to the ASBMR 2010 criteria (Table 1). Thus, AFFs represented 1.02% of the overall burden of femoral fractures identified. There were 17 femoral fracture radiographs thought by the original reporting radiologist to show “atypical features” but were not formally labelled as AFF. The use of the descriptor “atypical” was to describe an unusual feature rather than to define an AFF. Of these, only 1 patient met the criteria for an AFF when assessed for this study and is included in the 16 patients above. On retrospective review of previous imaging, two of the patients had prior radiographic evidence of AFFs manifest as cortical changes that had not been previously identified in the radiology report.
Patients with AFFs were typically female (81%), Caucasian (63%), and were in the 8th decade (71 ± 3.9 years) (Table 2). 12.5% of fractures were bilateral. 3 of 16 patients did not have their contralateral femur imaged. For the 13 patients who did have their contralateral femur imaged, there was a delay of 111 ± 44 days.
Table 2.
The demographics and clinical features of patients identified as having atypical femoral fractures (AFFs)
| Patients with AFFs | |
|---|---|
| N | 16 |
| Age | 71 ± 3.9 years |
| Male | 3/16 |
| Ethnicity | |
| White | 10 |
| Asian | 3 |
| Black | 1 |
| Unknown | 2 |
| Site | |
| Left | 9 |
| Right | 5 |
| Bilateral | 2 |
| Prodromal pain | |
| Yes | 13 |
| No | 3 |
| Contralateral imaging | |
| Yes | 13 |
| No | 3 |
| Delay | 111 ± 44 days |
| Bisphosponate use | |
| Yes | 10 |
| No | 6 |
| Fracture fixation | 4 |
| Successful conservative | 8 |
| Failed conservative | 4 |
Data are expressed as mean ± standard error.
Of the 16 patients identified, 11 patients had been seen in the metabolic bone clinic. A significant proportion of patients experienced delayed fracture healing (9/16) as defined as no significant healing within 3 months. Anabolic agents were used in seven patients of this group of patients because of concerns with delayed healing. Of the 16 patients, only 10 patients had serum 25-hydroxyvitamin D measured, and 2 patients were vitamin D deficient (<30 nmol L−1). Additional analyses of known risk factors for AFF included pharmacotherapy with 10 of 16 patients on a bisphosphonate (duration known only in 7 patients; 5.4 ± 1.5 years), 7 of 16 patients on a proton pump inhibitor and 4 of 16 patients on oral glucocorticoids.
4 patients were managed with fixation on acute presentation and 12 patients were initially managed conservatively. Of the 12 patients managed conservatively (non-complete fractures), 4 patients required subsequent fixation. Two patients were prescribed strontium ranelate and five patients were prescribed teriparatide.
DISCUSSION
The present study was a large retrospective analysis investigating the adherence to established guidelines for the radiological classification of AFFs in a large UK hospital between the ASBMR 2010 and ASBMR 2014 task force statements. The principal focus was to look at the accuracy and reliability of the radiological classification of AFFs with a secondary aim of looking at the clinical management considerations.
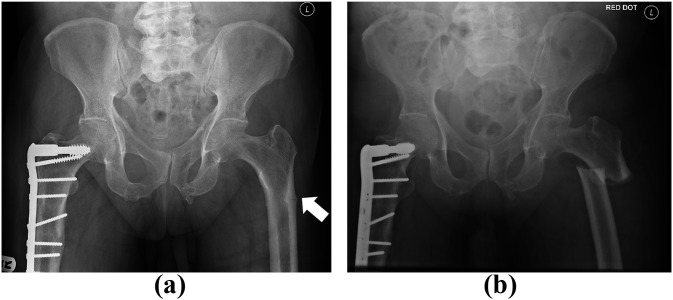
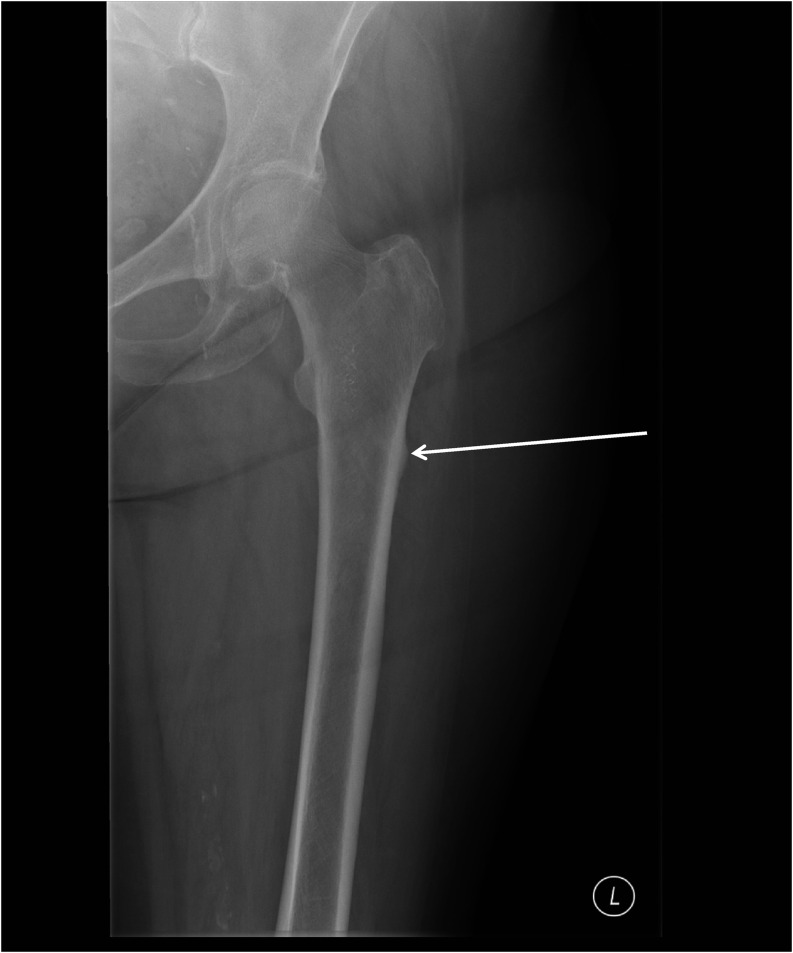
AFFs made up 1.02% of the femoral fractures identified (16/1558), which is marginally lower than that of previous studies.14,15 The University Hospitals Birmingham is a major trauma centre which may dilute the relative proportion of AFFs. Of the 16 patients identified by the radiological search, none had been labelled as AFFs by the original reporting radiologist reflecting the limited awareness of the condition and the diagnostic criteria. It is important to acknowledge that all were reported as fractures, although on retrospective review, two patients with a prodrome of pain and cortical reaction were not recognized on earlier films. This led to a delay in diagnosis and management. The importance of early recognition is highlighted in Figure 1. These radiographs are taken from the same patient 3 months apart. In Figure 1a the horizontal fracture line is clearly visible in the lateral cortex and within 3 months the fracture is complete (Figure 1b). We have endeavoured to highlight some of the key radiological findings in reporting plain radiographs (Figures 1–5) of AFFs. Of the original reports, 17 fractures were labelled as atypical in nature but only 1 fracture met the formal criteria for AFF. The use of the word “atypical” here was a qualitative comment made by the reporting radiologist that the fracture had unusual features, rather than a misdiagnosis of AFF; this might be more appropriately termed unusual. Three patients did not have the contralateral femur imaged. For the 13 of 16 patients who did have the contralateral femur imaged, there was a considerable delay (111 ± 44 days). This is of significant concern as 12.5% were bilateral and in spite of patients attending a specialist clinic, one did not have the contralateral femur imaged.
Figure 1.
A plain radiograph showing lateral cortical thickening with a radiolucent line (a; arrow) prior to completion of the fracture and (b) 3 months later in the same patient. L, left.
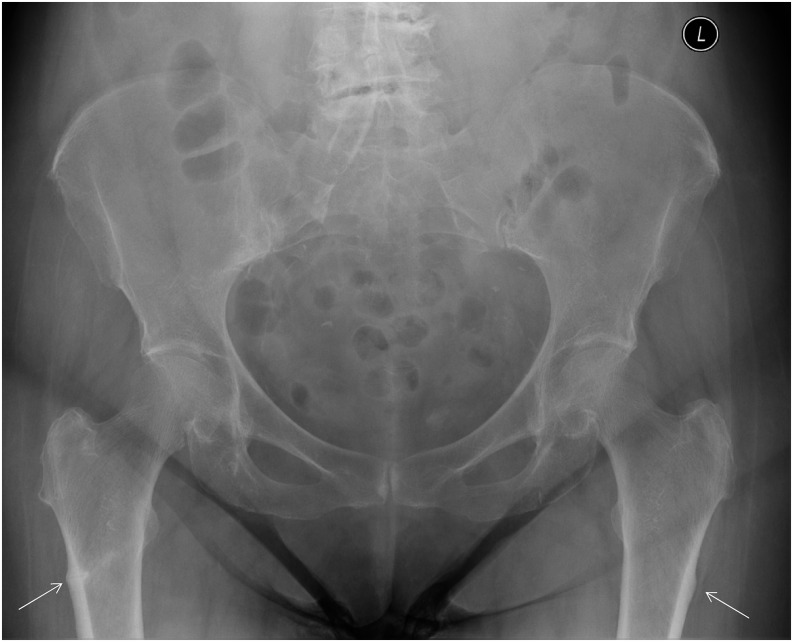
Figure 5.
Typical location of atypical fractures along the lateral subtrochanteric femoral diaphysis (arrows). L, left.
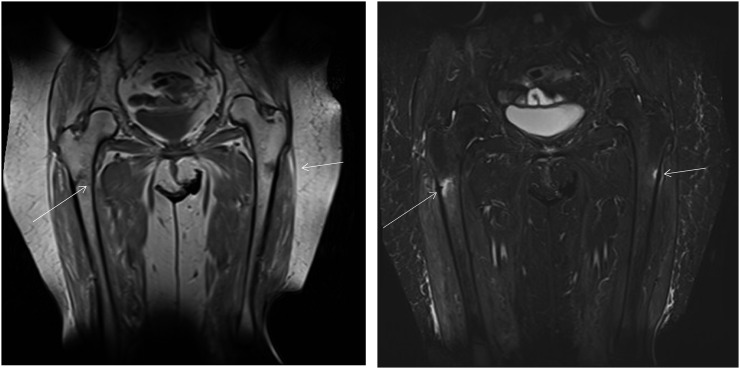
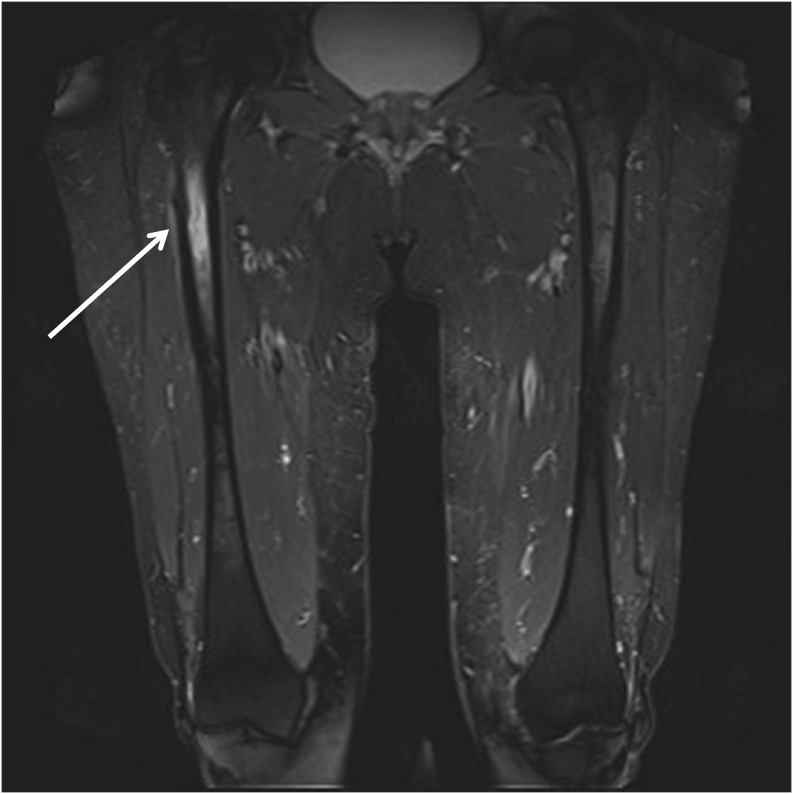
Incomplete AFFs may be easy to overlook on plain film radiography.16,17 There are many differential diagnoses, including insufficiency fractures and pseudofractures (Looser's Zones).16,18 In addition, AFFs may appear particularly aggressive on plain film radiographs, suggestive of pathological fracture.18–20 Familiarity with the typical appearance of AFFs should enable diagnosis,19 however utilizing other imaging modalities such as CT, MRI or bone scintigraphy in addition to plain film radiography may help when there is diagnostic uncertainty (Figures 6–9). In particular, MRI demonstrates marrow and endosteal oedema (Figure 6) prior to the radiographic changes of AFF17,19,20 and would therefore be useful for early detection in the absence of plain film changes and is the most accurate modality for distinguishing stress fractures from pathological fractures.18
Figure 6.
MRI of the same patient identified in Figure 5, showing bone marrow oedema (arrows) suggesting these are acute.
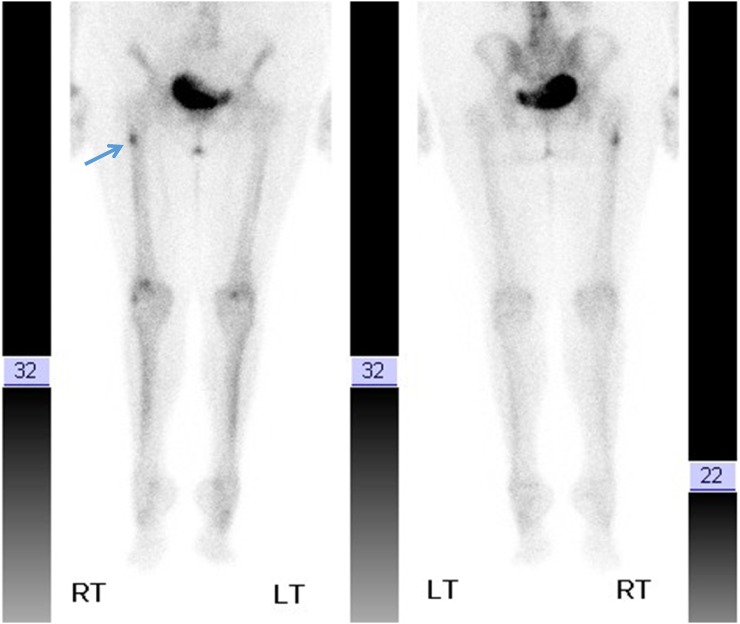
Figure 9.
A bone scan demonstrating uptake along the lateral cortex of the right femur (arrow) on the same patient. This study was performed prior to the MRI (Figure 7), when a question of metastasis was raised. LT, left; RT, right.
Figure 8.
A CT performed on the same day, following the MRI shown in Figure 7 confirms an atypical femoral fracture (arrows). A, anterior view; L, lateral view.
AFFs are located in the subtrochanteric femur. Radiographic appearances are typically lateral cortical thickening (Figures 2 and 3). In some patients, a linear radiolucent line (Figures 1 and 4) may be visible in the area of cortical thickening, a finding associated with greater likelihood of surgical intervention.21 MRI helps in guiding further management by identifying bone marrow oedema (Figures 6 and 7) related to cortical thickening indicating an incomplete fracture requiring active treatment, in contrast to cortical thickening without bone marrow oedema on MRI which would indicate an old healed incomplete fracture.21
Figure 2.
Early plain radiographic appearance of subtle cortical thickening (arrow). L, left.
Figure 3.
A plain radiograph demonstrating lateral cortical thickening and a periosteal reaction. R, right.
Figure 4.
Atypical femoral fracture with a lucency at the site of cortical thickening (arrow), which makes these more likely to need surgical fixation.
Figure 7.
Atypical femoral fracture picked up incidentally in a patient with thigh pain, with a previous history of breast cancer. A coronal short tau inversion recovery MRI shows cortical thickening and bone marrow as well as periosteal oedema (arrow), suggesting a fracture rather than metastasis. The location of this finding suggested an atypical fracture.
In contrast to bisphosphonate-related atypical fractures, Looser's zones in osteomalacia occur along the medial femoral cortex with relatively lesser cortical thickening. The latter are typically located at additional sites like the femoral neck, pubic rami, ribs and scapula.
Stress fractures of the femur occur mostly in athletes, those undergoing military training and the elderly. These more usually involve the subcapital femoral neck and start from the weight-bearing medial cortex.22
In our series, 4 of 16 patients with AFF proceeded to surgical fixation following diagnosis; 4 patients who were initially managed conservatively subsequently required surgery. This conversion to operative management follows that seen in previous studies.23
The use of anabolic agents was limited with two patients prescribed strontium ranelate and five patients prescribed teriparatide. Much of the data in non-healing AFFs are from retrospective small case series24 with some emergent prospective data demonstrating improved healing with teriparatide in non-healing AFFs.25
The key finding of the present work is that radiologists are not yet aware of AFFs as a distinct diagnosis and that failure to report these may result in delay of imaging of the contralateral side, recognition of the prodromal cortical reaction and referral to specialist services. With increased awareness of AFFs and other complications, patients are now advised to take bisphosphonates for shorter duration (perhaps 5 years initially), and it is hoped that this will limit the number of AFFs whilst providing protection against more typical osteoporotic fractures. It is crucial that therapy remains under review to prevent osteoporotic fractures which remain far more common than AFFs.
Acknowledgments
ACKNOWLEDGMENTS
Thanks to the radiology department at Queen Elizabeth Hospital Birmingham for provision of the imaging.
Contributor Information
Katrina Harborne, Email: Kficarotta@doctors.org.uk.
Jonathan M Hazlehurst, Email: jonathan.hazlehurst@gmail.com.
Hari Shanmugaratnam, Email: hari.shanmugaratnam@gmail.com.
Samuel Pearson, Email: sampearson1@nhs.net.
Alison Doyle, Email: Alison.Doyle@uhb.nhs.uk.
Neil J Gittoes, Email: Neil.Gittoes@uhb.nhs.uk.
Surabhi Choudhary, Email: surabhi.choudhary@uhb.nhs.uk.
Rachel K Crowley, Email: R.Crowley@st-vincents.ie.
REFERENCES
- 1.Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study. BMJ 2003; 327: 771–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, et al. Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 1998; 280: 2077–82. doi: 10.1001/jama.280.24.2077 [DOI] [PubMed] [Google Scholar]
- 3.Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. ; FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 2009; 361: 756–65. doi: 10.1056/NEJMoa0809493 [DOI] [PubMed] [Google Scholar]
- 4.Crandall CJ, Newberry SJ, Diamant A, Lim YW, Gellad WF, Booth MJ, et al. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med 2014; 161: 711–23. doi: 10.7326/M14-0317 [DOI] [PubMed] [Google Scholar]
- 5.Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res 2013; 28: 1729–37. doi: 10.1002/jbmr.1893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schilcher J, Michaëlsson K, Aspenberg P. Bisphosphonate use and atypical fractures of the femoral shaft. N Engl J Med 2011; 364: 1728–37. doi: 10.1056/NEJMoa1010650 [DOI] [PubMed] [Google Scholar]
- 7.Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 2005; 90: 1294–301. doi: 10.1210/jc.2004-0952 [DOI] [PubMed] [Google Scholar]
- 8.Ettinger B, Burr DB, Ritchie RO. Proposed pathogenesis for atypical femoral fractures: lessons from materials research. Bone 2013; 55: 495–500. doi: 10.1016/j.bone.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 9.Schilcher J, Sandberg O, Isaksson H, Aspenberg P. Histology of 8 atypical femoral fractures: remodeling but no healing. Acta Orthop 2014; 85: 280–6. doi: 10.3109/17453674.2014.916488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taormina DP, Marcano AI, Karia R, Egol KA, Tejwani NC. Symptomatic atypical femoral fractures are related to underlying hip geometry. Bone 2014; 63: 1–6. doi: 10.1016/j.bone.2014.02.006 [DOI] [PubMed] [Google Scholar]
- 11.Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, et al. ; American Society for Bone and Mineral Research. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2010; 25: 2267–94. doi: 10.1002/jbmr.253 [DOI] [PubMed] [Google Scholar]
- 12.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014; 29: 1–23. doi: 10.1002/jbmr.1998 [DOI] [PubMed] [Google Scholar]
- 13.Egol KA, Park JH, Rosenberg ZS, Peck V, Tejwani NC. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res 2014; 472: 2728–34. doi: 10.1007/s11999-013-2963-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thompson RN, Phillips JR, McCauley SH, Elliott JR, Moran CG. Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surg Br 2012; 94: 385–90. doi: 10.1302/0301-620X.94B3.27999 [DOI] [PubMed] [Google Scholar]
- 15.Schilcher J, Koeppen V, Aspenberg P, Michaëlsson K. Risk of atypical femoral fracture during and after bisphosphonate use. N Engl J Med 2014; 371: 974–6. doi: 10.1056/NEJMc1403799 [DOI] [PubMed] [Google Scholar]
- 16.Porrino JA, Jr, Kohl CA, Taljanovic M, Rogers LF. Diagnosis of proximal femoral insufficiency fractures in patients receiving bisphosphonate therapy. AJR Am J Roentgenol 2010; 194: 1061–4. doi: 10.2214/AJR.09.3383 [DOI] [PubMed] [Google Scholar]
- 17.Moeinoddini SA, Parikh RJ, Moore SR, Moore DJ. Sequential bilateral femoral fractures. BMJ 2012; 345: e7361. doi: 10.1136/bmj.e7361 [DOI] [PubMed] [Google Scholar]
- 18.Fayad LM, Kawamoto S, Kamel IR, Bluemke DA, Eng J, Frassica FJ, et al. Distinction of long bone stress fractures from pathologic fractures on cross-sectional imaging: how successful are we? AJR Am J Roentgenol 2005; 185: 915–24. doi: 10.2214/AJR.04.0950 [DOI] [PubMed] [Google Scholar]
- 19.Chan SS, Rosenberg ZS, Chan K, Capeci C. Subtrochanteric femoral fractures in patients receiving long-term alendronate therapy: imaging features. AJR Am J Roentgenol 2010; 194: 1581–6. doi: 10.2214/AJR.09.3588 [DOI] [PubMed] [Google Scholar]
- 20.Fayad LM, Kamel IR, Kawamoto S, Bluemke DA, Frassica FJ, Fishman EK. Distinguishing stress fractures from pathologic fractures: a multimodality approach. Skeletal Radiol 2005; 34: 245–59. doi: 10.1007/s00256-004-0872-9 [DOI] [PubMed] [Google Scholar]
- 21.Saleh A, Hegde VV, Potty AG, Schneider R, Cornell CN, Lane JM. Management strategy for symptomatic bisphosphonate-associated incomplete atypical femoral fractures. HSS J 2012; 8: 103–10. doi: 10.1007/s11420-012-9275-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khadabadi NA, Patil KS. Simultaneous bilateral femoral neck stress fracture in a young stone mason. Case Rep Orthop 2015; 2015: 306246. doi: 10.1155/2015/306246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res 2011; 469: 2028–34. doi: 10.1007/s11999-011-1828-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carvalho NN, Voss LA, Almeida MO, Salgado CL, Bandeira F. Atypical femoral fractures during prolonged use of bisphosphonates: short-term responses to strontium ranelate and teriparatide. J Clin Endocrinol Metab 2011; 96: 2675–80. doi: 10.1210/jc.2011-0593 [DOI] [PubMed] [Google Scholar]
- 25.Miyakoshi N, Aizawa T, Sasaki S, Ando S, Maekawa S, Aonuma H, et al. Healing of bisphosphonate-associated atypical femoral fractures in patients with osteoporosis: a comparison between treatment with and without teriparatide. J Bone Miner Metab 2015; 33: 553–9. doi: 10.1007/s00774-014-0617-3 [DOI] [PubMed] [Google Scholar]