Abstract
Objective:
Despite a significant expansion in the use of cardiac MRI (CMR), there is inadequate evaluation of its incremental impact on clinical decision-making over and above other well-established modalities. We sought to determine the incremental utility of CMR in routine practice.
Methods:
629 consecutive CMR studies referred by 44 clinicians from 9 institutions were evaluated. Pre-defined algorithms were used to determine the incremental influence on diagnostic thinking, influence on clinical management and thus the overall clinical utility. Studies were also subdivided and evaluated according to the indication for CMR.
Results:
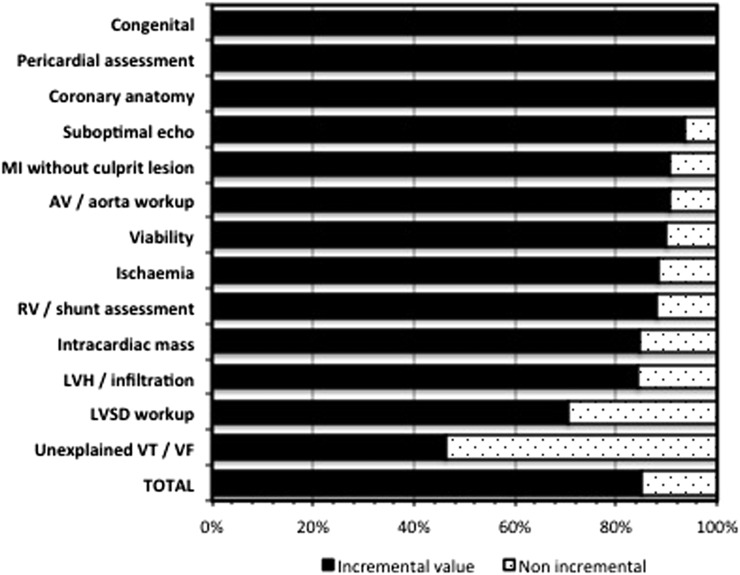
CMR provided incremental information to the clinician in 85% of cases, with incremental influence on diagnostic thinking in 85% of cases and incremental impact on management in 42% of cases. The overall incremental utility of CMR exceeded 90% in 7 out of the 13 indications, whereas in settings such as the evaluation of unexplained ventricular arrhythmia or mild left ventricular systolic dysfunction, this was <50%.
Conclusion:
CMR was frequently able to inform and influence decision-making in routine clinical practice, even with analyses that accepted only incremental clinical information and excluded a redundant duplication of imaging. Significant variations in yield were noted according to the indication for CMR. These data support a wider integration of CMR services into cardiac imaging departments.
Advances in knowledge:
These data are the first to objectively evaluate the incremental value of a UK CMR service in clinical decision-making. Such data are essential when seeking justification for a CMR service.
INTRODUCTION
Cardiac MRI (CMR) is now widely regarded as a mainstream imaging modality in contemporary clinical practice.1 Notwithstanding the widespread acceptance of this expansion in utility, there has been limited objective assessment of the incremental influence of CMR on clinical decision-making over and above other well-established modalities. Analyses of diagnostic performance are increasingly demanded by policymakers, commissioning groups and payers for healthcare, yet robust studies are virtually non-existent across all modes of cardiac imaging.2,3 A recent review of existing American College of Cardiology (ACC) and American Heart Association (AHA) guidelines for cardiac diagnostics, for example, identified that 44% of recommendations had little or no evidence base.4 The provision of a clinical CMR service incurs a significant cost and training burden, whose justification therefore requires a demonstration of incremental value of CMR in routine clinical practice. A further interrogation of the utility of CMR according to the indication for imaging would also be highly informative. We evaluated all consecutive CMR studies over an 18-month period referred to our regional CMR unit from a number of centres spanning a large geographical region of the North East England, in order to determine the incremental utility of a CMR service.
METHODS AND MATERIALS
CMR imaging and reporting
Multiparametric studies were conducted using a 1.5-T magnet (magnetom® Avanto; Siemens Medical Solutions, Erlangen, Germany) in accordance with standard protocols.5 Cine imaging was typically performed using a balanced steady-state free-precession sequence, and anatomical imaging was performed with a black-blood spin-echo sequence. Myocardial oedema was qualitatively assessed by short tau inversion recovery imaging. Regadenoson vasodilatory stress first-pass myocardial perfusion imaging was conducted using a two-dimensional balanced steady-state free-precession sequence and 0.075 mmol kg−1 bolus of gadobutrol (Gadovist, Bayer). Early and late gadolinium enhancements were assessed with a phase-sensitive inversion recovery sequence following a total contrast dose of 0.15 mmol kg−1. Three-dimensional contrast-enhanced MR angiography was acquired in complement to electrocardiogram-gated cross-sectional views for great-vessel imaging. Velocity-encoded gradient-echo imaging was used to quantify blood flow. All studies were reported by at least one Level 3 accredited clinician on a dedicated post-processing platform (CVI42®, Circle Cardiovascular Imaging Inc., Calgary, Canada).
Clinical indications for CMR
A database of all CMR studies conducted at the South Tees Hospitals NHS Foundation Trust was prospectively established. All consecutive studies over an 18-month period were grouped by the 13 most common indications for CMR (Table 1), which are closely aligned to applications outlined in expert consensus documents.6 Only the single most pertinent indication was allocated per study, excepting the few occasions where multiple separate clinical questions were posed.
Table 1.
Indications for cardiac MRI (CMR)
| Indication for CMR | Proportion (%) |
|---|---|
| Chest pain and raised troponin without angiographic culprit | 17.2 |
| Assessment of LVH/infiltration/abnormal ECG | 17.0 |
| Assessment of thoracic aorta/aortic valve | 17.0 |
| Assessment of LVSD | 16.9 |
| Assessment of viability | 8.6 |
| Assessment of the RV/shunts | 6.7 |
| Assessment of ischaemia | 5.6 |
| Assessment of congenital disease | 2.7 |
| Imaging after suboptimal or discrepant TTE findings | 2.5 |
| Assessment of unexplained ventricular arrhythmia | 2.1 |
| Assessment of intracardiac/paracardiac mass | 2.1 |
| Assessment for coronary artery anomaly | 1.0 |
| Assessment of pericardial disease | 0.8 |
ECG, electrocardiogram; LVH, left ventricular hypertrophy; LVSD, left ventricular systolic dysfunction; RV, right ventricular; TTE, transthoracic echocardiography.
Indications for CMR, with the relative proportion (percent) of all studies conducted for each indication.
Analysis of clinical utility
Electronic patient records pre- and post-CMR were analysed to assess the contribution of CMR. Pre-defined algorithms as detailed in the following section were used to determine the utility of the CMR study. Duplicate analyses were undertaken independently in all cases by two clinicians (AR and MJS), one being a senior clinician without any dedicated interest in CMR. Divergences in assessment were adjudicated by a third cardiologist (NM). Cases were not analysed where the clarity of clinical records was insufficient to allow unambiguous conclusion.
Algorithm for assessment of clinical utility
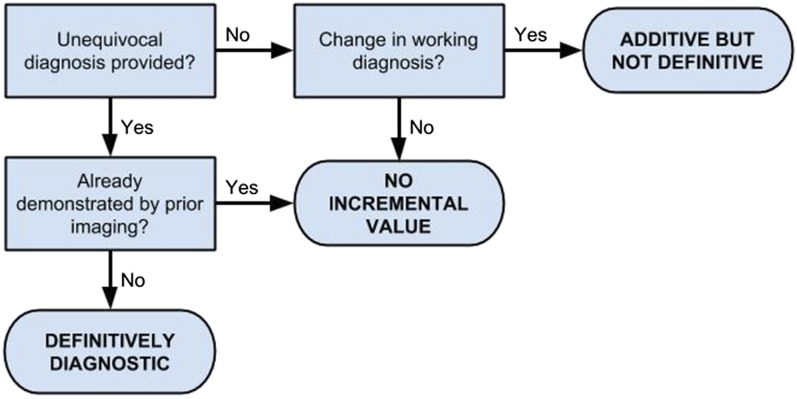
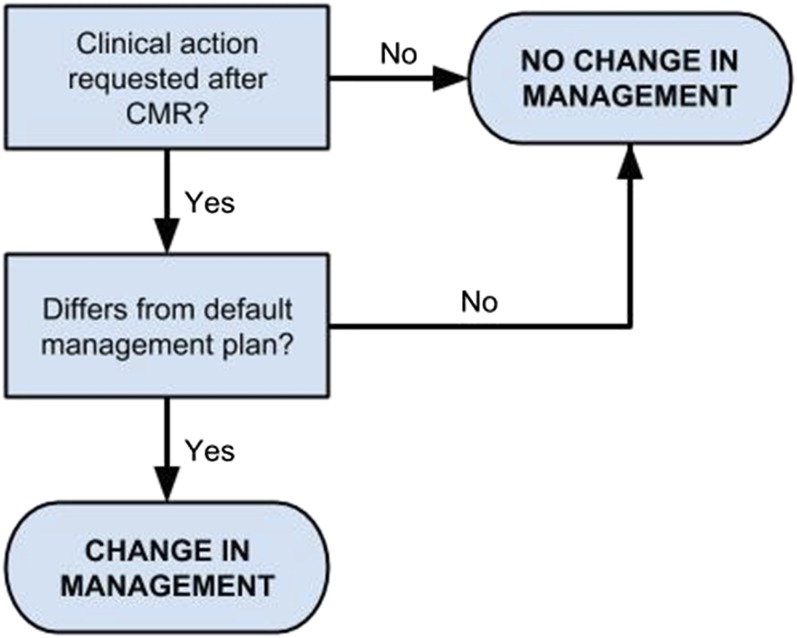
An established six-hierarchy model has previously been outlined as a framework by which the diagnostic performance of an imaging modality can be evaluated (Fryback–Thornbury model, Table 2).7 For each case, we determined outputs at Level 3 (influence of CMR on diagnostic thinking) and Level 4 (influence of CMR on further management). Pre-defined algorithms were then applied to ensure only the incremental benefit of CMR, over and above all investigations already undertaken, was captured. Thus, for influence on diagnostic thinking (Level 3 output, Figure 1), only the provision of a single conclusion not already demonstrated by prior imaging was accepted as definitive. Conversely, a mere reproduction of information already available before the CMR study or conclusions which were not accepted by the referring clinician were regarded as non-incremental even where a definitive conclusion had been provided. Where CMR was not definitively diagnostic but did alter the working diagnosis (such as an exclusion of infarction) or identified a single “most probable” diagnosis (such as hypertensive heart disease), this was labelled as additive but not definitive. For impact on management (Level 4 output, Figure 2), this required a genuine change in strategy prompted by CMR and not a mere affirmation of a pre-existing decision. Only one most pertinent change was allocated per case per indication. Finally, these data were amalgamated to determine the overall utility of CMR, this being the net influence on diagnostic thinking and management.
Table 2.
Hierarchical model of diagnostic performance
| Level 1 | Technical quality of images |
| Level 2 | Diagnostic accuracy of modality |
| Level 3 | Influence on diagnostic thinking |
| Level 4 | Therapeutic efficacy |
| Level 5 | Patient outcome efficacy |
| Level 6 | Societal efficacy |
Figure 1.
Algorithm for evaluation of influence on diagnostic thinking. Decision-making flow chart by which patient records were interrogated to determine the incremental influence on diagnostic thinking of the CMR study. CMR, cardiac MRI.
Figure 2.
Algorithm for evaluation of influence on management. Decision-making flow chart by which patient records were interrogated to determine the incremental influence on management of the CMR study. CMR, cardiac MRI.
RESULTS
Clinical indications for CMR
629 studies were conducted over the evaluated period, with requests arising from 44 clinicians across 9 referring institutions. The majority were undertaken as work-up for chest pain and troponin rise without angiographic culprit (17.2%), the further assessment of left ventricular hypertrophy or infiltration (17.0%), assessment of the aorta and aortic valve (17.0%) and work-up for left ventricular systolic dysfunction (LVSD) of uncertain aetiology (16.9%) (Table 1). Only 2% of CMR studies were uninterpretable, and no major complications occurred as a direct result of any CMR study. Patient records were sufficient to fully ascertain the incremental value of imaging in 97% of cases. Discrepancies between the two investigators arose in 1.9% of assessments.
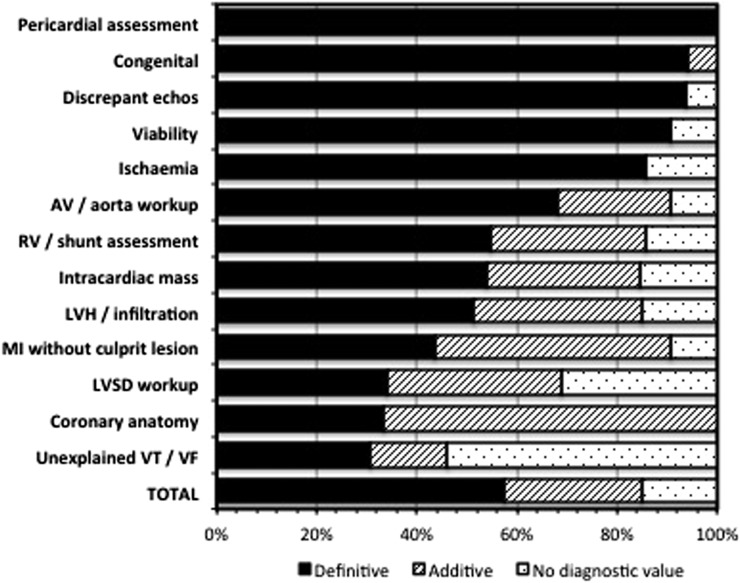
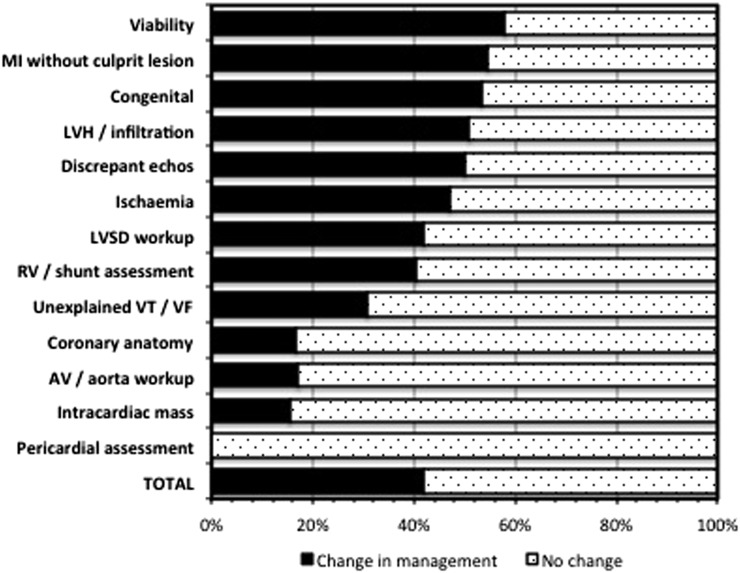
Diagnostic performance of all CMR studies
Across all analysed studies, 57.6% studies were definitively diagnostic, with a further 27.3% studies being of additive diagnostic value (Figure 3). 42% studies prompted a clear change in management (Figure 4, Table 3). Overall, only 15% of studies were of no incremental value towards either diagnosis or management (Figure 5).
Figure 3.
Incremental influence on diagnostic thinking (Level 3 output). Frequency (percent) by which CMR incrementally influenced diagnostic thinking, with further subdivision according to individual indication. Diagnostic influence could be categorized as (i) definitively diagnostic; (ii) additive but not definitive; or (iii) no incremental diagnostic value. AV, aortic value; CMR, cardiac MRI; LVSD, left ventricular systolic dysfunction; LVH, left ventricular hypertrophy; RV, right ventricle; VF, ventricular fibrillation; VT, ventricular tachycardia.
Figure 4.
Incremental influence on management (Level 4 output). Frequency (percent) by which CMR incrementally influenced management, with further subdivision according to individual indications. Influence on management was a binary outcome (impact vs no impact). AV, aortic value; CMR, cardiac MRI; LVSD, left ventricular systolic dysfunction; LVH, left ventricular hypertrophy; RV, right ventricle; VF, ventricular fibrillation; VT, ventricular tachycardia.
Table 3.
Impact on management of cardiac MRI (CMR)
| Impact on management | Frequency (%) |
|---|---|
| Change in medication (antiplatelets) | 7.8 |
| Change in medication (anticoagulation) | 0.8 |
| Change in medication (other) | 3.2 |
| Revascularization/intervention/surgery scheduled | 3.8 |
| Revascularization/intervention/surgery no longer indicated | 4.0 |
| Choice of revascularization/intervention/surgery altered | 1.6 |
| Cardiac catheterization scheduled | 1.3 |
| Cardiac catheterization no longer indicated | 2.5 |
| Surveillance initiated/admitted | 2.7 |
| Surveillance terminated/discharged | 4.6 |
| CRT/ICD scheduled | 1.6 |
| CRT/ICD no longer indicated | 1.0 |
| Choice of device altered | 0.3 |
| HCM prognostic assessment scheduled | 3.2 |
| Genetic/familial screening scheduled | 1.3 |
| Endomyocardial biopsy scheduled | 0.3 |
| Endomyocardial biopsy no longer indicated | 0.3 |
| Other | 1.0 |
CRT, cardiac resynchronization therapy; HCM, hypertrophic cardiomyopathy; ICD, implantable cardioverter defibrillator.
Categorization and frequency (percent) of impact on clinical management across all CMR studies conducted during the study period.
Figure 5.
Overall incremental utility. Frequency (percent) by which incremental and clinically useful information was provided by the CMR study, defined as the presence or absence of any incremental influence on either diagnostic thinking or clinical management. AV, aortic value; CMR, cardiac MRI; LVSD, left ventricular systolic dysfunction; LVH, left ventricular hypertrophy; RV, right ventricle; VF, ventricular fibrillation; VT, ventricular tachycardia.
Chest pain and troponin rise without angiographic culprit
New definitive diagnoses were revealed in 44% of cases. Additional diagnostic information was provided in a further 47% of cases, typically the exclusion of infarction. The principle conclusions included focal infarction, myocarditis, Takotsubo cardiomyopathy, hypertrophic cardiomyopathy or no clear diagnosis. Management was altered in 55% of cases, with discontinuation of antiplatelet therapy being the commonest change. Overall, 9% of studies were of no incremental utility towards either diagnosis or management. Separately, we also observed a reduced detection of myocarditis in delayed studies (14% in those studies conducted >14 days after the index event vs 38% in those studies conducted <14 days after the index event; p < 0.02).
Assessment of left ventricular hypertrophy, infiltration or abnormal electrocardiogram
CMR allowed the referring clinician to make a definitive diagnosis in 51% of cases. Conditions most frequently encountered were primarily hypertrophic cardiomyopathy or the revision of an erroneous label of hypertrophy by echocardiography. Less frequently encountered diagnoses were athletic heart, hypertensive heart disease, non-compaction cardiomyopathy, Anderson–Fabry cardiomyopathy, cardiac sarcoidosis and cardiac amyloid. Management was altered in 51% of cases, primarily the new initiation of further prognostic work-up and genetic/familial screening or a discharge from follow-up that was no longer deemed necessary. Overall, 16% of studies were of no incremental utility towards either diagnosis or management.
Assessment of the aorta/aortic valve
CMR provided new definitive information in 68% of studies. Referring clinicians typically sought a more comprehensive evaluation of the entire thoracic aorta and/or of aortic valve morphology. Management was altered in 17% of cases, predominantly decisions between ongoing surveillance vs surgical management. Overall, 10% of studies were of no incremental clinical utility towards either diagnosis or management.
Assessment of left ventricular systolic dysfunction
Only 34% of studies resulted in a definitive diagnosis. Conclusions included dilated cardiomyopathies (12.2%), myocarditis (8.5%), infarction (5.6%), non-compaction cardiomyopathy (3.8%), hypertensive heart disease (3.8%), cardiac sarcoidosis (2.8%), severely regurgitant valve disease (1.9%) and arrhythmogenic left ventricular cardiomyopathy (0.9%). Of note, the incremental diagnostic yield was very poor where LVSD was only mild on preceding echocardiography. Management was altered in 42% of all cases, with a wide spectrum of decisions regarding cardiac catheterization, revascularization, change of medication and reclassification of indication for cardiac resynchronization therapy/implantable cardioverter defibrillator. Overall, 30% of studies were of no incremental utility towards either diagnosis or management.
Ischaemia and/or viability
CMR definitively demonstrated or excluded perfusion defects in 86% of ischaemia studies. In most cases, coronary artery disease had already been demonstrated invasively, with only 20% of studies conducted as initial work-up of chest pain. Management was influenced subsequently in 47% of cases. Assessments of viability were definitively fulfilled in 91% of cases and influenced subsequent management in 58% of cases. Overall, 12% of studies for ischaemia and 10% of studies of viability were of no incremental utility towards either diagnosis or management.
Assessment of the right heart
CMR was requested predominantly for suspected abnormalities of right ventricular structure or function (88%), pulmonary valve or artery evaluation (10%) or the further assessment of a shunt (2%). Definitive diagnoses [or a major modified task force criterion in the case of arrhythmogenic right ventricular cardiomyopathy (ARVC)]8 were provided in 55% of studies, and additive diagnostic information (or minor task force criteria in the case of ARVC) in a further 31% of studies. Management was influenced in 40% of cases, predominantly decisions to initiate or terminate further clinical surveillance, and further genetic/familial assessment in a smaller proportion. Overall, 12% of studies were of no incremental utility towards either diagnosis or management.
Congenital conditions
A definitive assessment was provided in 94% of cases. Studies were requested primarily for the follow-up of repaired congenital disease with residual anatomical, valvular or functional abnormalities. Management was altered in 53% of cases, primarily referral for intervention. All studies were of incremental influence towards either diagnosis or management.
Suboptimal or discrepant echocardiogram
Definitive structural and functional assessment was provided by CMR and accepted by the referring clinician in 94% of instances where echocardiographic images were suboptimal or discrepant. 19% of cases had atrial fibrillation at the time of the study, but uninterpretable studies in 6% of cases were all due to significant ventricular ectopy. Management was altered in 50% of cases, typically decisions with regards to cardiac resynchronization therapy/implantable cardioverter defibrillator. Overall, 6% of studies were of no incremental utility towards either diagnosis or management.
Assessment of ventricular arrhythmia of uncertain origin
Assessments under this indication were typically those where work-up had not already revealed substrate for arrhythmia. Pre-CMR suspicion for ARVC is evaluated separately under assessment of the right ventricle. Definitive substrate for arrhythmia was demonstrated in 31% of cases. Management was altered in 31% of cases. Overall, 54% of studies had no incremental value towards either diagnosis or management.
Intracardiac/paracardiac masses
CMR definitively identified the nature of a cardiac mass in 54% of cases. Conclusions included a demonstration rather of normal anatomy/anatomical variant (46%), a distinction as to whether the mass was likely to be benign or malignant (38%) or the presence or absence of thrombus (15%). All patients had undergone transthoracic echocardiography prior to CMR; diagnostic efficacy of CMR was present only where echocardiographic characterization was incomplete. Changes in management prompted purely by CMR in 15% of cases were all related to anticoagulation, whereas no decisions regarding surgical intervention were altered purely by CMR. Overall, 15% of studies had no incremental utility towards either diagnosis or management.
Coronary artery assessment
One study evaluated coronary artery aneurysm and thrombus in a patient with Behcet's disease, and one was requested as part of the evaluation of coronary artery disease in parallel with vasodilatory perfusion CMR in a patient reporting a prior anaphylactic response to iodine-based contrast. All other studies were conducted to detect or further assess anomalous coronary artery anatomy. 33% of studies were incrementally definitive, and 17% of studies altered management. Overall, all studies were of incremental utility towards either diagnosis or management.
Assessment of the pericardium
Most studies were requested to determine whether a diagnosis of constrictive pericarditis was supported, excepting one demonstrating congenital absence of the pericardium. All studies provided a definitive diagnosis, and thus all studies were of incremental value. Management was not influenced in any of the cases during the study period however.
DISCUSSION
This study examines the clinical yield of a consecutive series of 629 multiparametric CMR studies, conducted at a medium-sized tertiary centre with a throughput that is representative of many other UK CMR departments.9 Within a real-world setting, CMR incrementally influenced diagnostic thinking in 85% of cases and clinical management in 42% of cases. These figures compare favourably with those few studies in this domain of other imaging modalities such as a 26% change in management with a routine use of fractional flow reserve as an adjunct to coronary angiography, or 35.6% of selected individuals undergoing contrast echocardiography.10,11 Crucially, we were able to capture a wide range of referral habits (44 clinicians across 9 institutions) and with pre-defined algorithms that returned highly reproducible and objective data sets. Such data will thus be highly relevant to units seeking justification for CMR services and are novel with respect to the typical throughput of a UK centre.
Hierarchical assessment of clinical utility
The quantification of clinical utility of a diagnostic imaging modality is challenging. In this study, we used a hierarchical model (Fryback–Thornbury model) that has been widely adopted in the systematic evaluation of imaging efficacy (Table 2).7,12 A hierarchical categorization of diagnostic outputs as such is increasingly advocated in technology assessment in view of its organizing concepts and for pointing out important gaps in our current understanding.2 Outputs of CMR at Level 1 (technical quality of the image) and Level 2 (sensitivity, specificity, negative-predictive and positive-predictive values) were not addressed by our data set as a number of such studies are already present in the literature. There are however few studies of outputs at Level 3 (influence on diagnostic thinking) and Level 4 (influence on management), and as such, our data fill an important knowledge gap in the clinical utility of CMR.
Incremental clinical utility
An overarching requirement of our pre-defined algorithms was that only the incremental value of CMR, over and above other preceding investigations. This was a vital consideration in order to ensure value was not erroneously attributed to CMR studies that merely replicated the findings of preceding imaging. Virtually, all patients underwent transthoracic echocardiography prior to consideration of CMR, as well as other investigations deemed appropriate for their presentation such as coronary angiography, stress echo/single photon emission CT, transoesophageal echocardiography, CT angiography, electrophysiology studies and genetic testing. These findings thus reflect the true yield of CMR in day-to-day practice rather than a redundant repetition of investigation. Objective data of this nature are warranted to justify the burgeoning healthcare expenditure incurred during the assessment of cardiovascular disease,13 yet there are currently few data in this domain. One that has examined this issue is the large multicentre EuroCMR registry.1,14 The results of EuroCMR may not be readily applicable to current UK practice however. In the German pilot data, 35.9% of cases did not have a transthoracic echo prior to CMR, and in 23.1% of cases CMR was the first imaging modality conducted. The authors do however emphasize the potential benefit of adopting CMR as a single and initial imaging modality in certain settings where this might obviate the need for multiple investigations.
Validity of analyses
A non-systematic assessment of clinical utility may have been vulnerable to subjectivity. Several measures were thus taken to eliminate bias and to ensure an objective data set. All consecutive cases within a fixed period were systematically reviewed via electronic patient records. Strict pre-defined algorithms were used, and every case was also subject to duplicate analysis by a senior clinician without any dedicated interest in CMR. That this was a robust, objective and reproducible algorithm is demonstrated by concordance rates between the two analysing clinicians exceeding 98%. To further prevent empirical analyses, patient records without sufficient clarity were not analysed. In fact, 97% of records proved to be adequate, most likely owing to a predominantly outpatient origin of referrals where dictated communication regarding diagnosis and management plan was typically very comprehensive.
Clinical utility in individual indications
A high yield (typically exceeding 90%) was demonstrated in indications such as in congenital heart disease, assessment of the pericardium, detection of coronary anomaly or assessment of the right heart. These data do provide objective support for the use of CMR in these settings that are already strongly advocated by expert consensus,15 but as such will not alter current practice. We observed important and/or conflicting considerations or much lower yields in other indications however, and these now merit further scrutiny.
The utility of CMR in the evaluation of chest pain with biomarkers of myocardial injury but without angiographic culprit is unique. Incremental value was frequently demonstrated despite being preceded in every case by both coronary angiography and echocardiography. The presence or absence of subendocardial late gadolinium enhancement was particularly important in guiding decision-making with regards to continued antiplatelet therapy. Clinicians varied in their response to those scans showing an absence of any late gadolinium enhancement however, reflecting a lack of high quality evidence as to how this finding should influence management. We also noted an important influence of time delay to CMR study, with a significantly poorer diagnostic yield in studies conducted more than 2 weeks after presentation. Routine and early access to a CMR service for this indication should therefore be encouraged.
The further evaluation of LVSD is a frequent indication for CMR across UK and European centres.1,9 Influence on diagnostic thinking was relatively modest however, with a definitive diagnosis over and above other mainstream diagnostic modalities provided in only one-third of studies, and overall incremental yield in two-third of studies. One other study has recently reviewed the impact of CMR in 150 consecutive patients with LVSD in addition to standard investigations,16 with a similar overall “significant clinical impact” of 65%. A particularly low incremental utility was observed in our data set for mild LVSD, and a routine use of CMR in this subgroup may thus not currently be appropriate.
CMR evaluation of cardiac masses prompted only a low incremental impact on management. Closer scrutiny demonstrated an important dichotomy according to subindication however, with high incremental impact on decisions relating to suspected thrombus vs low incremental impact in relation to all other masses. Although CMR arguably conferred to the requesting physician a greater confidence in the diagnosis that is not captured by our algorithm, the subsequent management nonetheless continued to match the preceding decisions based purely on echocardiography except in the case of thrombus. An incremental role of CMR in the management of a mass of uncertain aetiology may thus be limited outside of cases where thrombus is suspected or where echocardiographic windows have been suboptimal.
A high clinical utility of stress perfusion CMR of 84% was demonstrated. A number of modalities for the detection of ischaemia are already well established in contemporary UK practice however,17 and whether CMR should be preferred to other modalities remains unclear. Although large clinical trials have now demonstrated superior diagnostic accuracy of perfusion CMR over single photon emission CT,18,19 other major considerations such as cost-effectiveness and impact on outcomes remain unresolved. Two comprehensive economic analyses of CMR in the diagnosis of ischaemic heart disease have reached opposing conclusions regarding cost-efficacy against competing imaging modalities.20,21 It is noteworthy however that CMR in our data set was requested predominantly to guide revascularization in known multivessel or complex disease, with relatively few studies conducted for the primary evaluation of chest pain. Those economic analyses may therefore not be applicable to contemporary CMR case mixes of ischaemia studies.
The relatively low yield of CMR in our data set for the investigation of ventricular arrhythmia of unclear origin might initially suggest a limited role in this setting (outside of the detection of ARVC, which was dealt with under a separate indication). Of note, White et al22 observed a substantially greater incremental yield of CMR in the assessment of ventricular arrhythmia. In contrast to our data set, CMR was requested in all patients in the relevant study arm rather than only at the clinician's discretion, with a substantial proportion of the yield derived from a reclassification of diagnosis. Put together, this may suggest that the management of those cases with an ostensibly secure diagnosis may still benefit from further scrutiny by CMR, whereas an absence of structural substrate for arrhythmia on initial diagnostic work-up is often not resolved by further advanced imaging.
Limitations
The limitations of data from a single-centre CMR service must be acknowledged. This is greatly offset however by the large number of referring clinicians across multiple centres, which will therefore have captured an appropriately wide spectrum of referral habits. Although we demonstrated influences of CMR on clinical management, subsequent influences of CMR on patient outcomes could not be evaluated in this retrospective uncontrolled data set. This may be a particular limitation where a change in management (albeit using other imaging modalities) has not necessarily been proven to improve outcomes; for example, viability assessment for the purpose of myocardial revascularization. An objective assessment of the clinical utility of an imaging modality unquestionably remains vital in day-to-day practice however,2 and the novel data in this study thus fill an important knowledge gap with respect to the merits of a UK CMR service.
Our primary focus was an evaluation of the incremental utility of a CMR service, for which a real-world data set is highly desirable. However, our secondary focus on the utility according to individual indication is subject to referral bias, with studies representing consecutive referrals rather than all consecutive presentations. As such, our secondary conclusions regarding the utility of CMR according to indication must be interpreted with caution. It is noteworthy however that, with the exception of unexplained ventricular arrhythmia, an agreement with the existing evidence base was typically noted.16,23,24 Finally, the small numbers in certain categories such as pericardial or coronary anomaly evaluation limits a wider extrapolation in these particular indications.
CONCLUSION
In a medium-sized centre that is likely to be representative of other UK CMR services, we observed a high overall incremental clinical utility of CMR over and above other well-established investigations. A more routine and early imaging appears reasonable in individuals with biomarker-positive chest pain without angiographic culprit and in the evaluation of suspected left ventricular thrombus, whereas a more selective approach may be appropriate in individuals with only mild LVSD, unexplained ventricular arrhythmia or cardiac masses that are already well characterized on other imaging.
Contributor Information
Adil Rajwani, Email: adil.rajwani@nhs.net.
Michael J Stewart, Email: Michael.Stewart@stees.nhs.uk.
James D Richardson, Email: JDR@doctors.org.uk.
Nicholas M Child, Email: n.child@nhs.net.
Neil Maredia, Email: neilmaredia@me.com.
REFERENCES
- 1.Bruder O, Wagner A, Lombardi M, Schwitter J, van Rossum A, Pilz G, et al. European cardiovascular magnetic resonance (EuroCMR) registry–multi national results from 57 centers in 15 countries. J Cardiovasc Magn Reson 2013; 15: 9. doi: 10.1186/1532-429X-15-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mark DB, Anderson JL, Brinker JA, Brophy JA, Casey DE, Jr, Cross RR, et al. ACC/AHA/ASE/ASNC/HRS/IAC/Mended Hearts/NASCI/RSNA/SAIP/SCAI/SCCT/SCMR/SNMMI 2014 health policy statement on use of noninvasive cardiovascular imaging: a report of the American College of Cardiology Clinical Quality Committee. J Am Coll Cardiol 2014; 63: 698–721. doi: 10.1016/j.jacc.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 3.Carr JJ, Hendel RC, White RD, Patel MR, Wolk MJ, Bettmann MA, et al. 2013 appropriate utilization of cardiovascular imaging: a methodology for the development of joint criteria for the appropriate utilization of cardiovascular imaging by the American College of Cardiology Foundation and American College of Radiology. J Am Coll Cardiol 2013; 61: 2199–206. doi: 10.1016/j.jacc.2013.02.010 [DOI] [PubMed] [Google Scholar]
- 4.Tricoci P, Allen JM, Kramer JM, Califf RM, Smith SC, Jr. Scientific evidence underlying the ACC/AHA clinical practice guidelines. JAMA 2009; 301: 831–41. doi: 10.1001/jama.2009.205 [DOI] [PubMed] [Google Scholar]
- 5.Kramer CM, Barkhausen J, Flamm SD, Kim RJ, Nagel E; Society for Cardiovascular Magnetic Resonance Board of Trustees Task Force on Standardized Protocols. Standardized cardiovascular magnetic resonance imaging (CMR) protocols, society for cardiovascular magnetic resonance: board of trustees task force on standardized protocols. J Cardiovasc Magn Reson 2008; 10: 35. doi: 10.1186/1532-429X-10-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American College of Cardiology Foundation Task Force on Expert Consensus Documents; Hundley WG, Bluemke DA, Finn JP, Flamm SD, Fogel MA, Friedrich MG, et al. ACCF/ACR/AHA/NASCI/SCMR 2010 expert consensus document on cardiovascular magnetic resonance: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. J Am Coll Cardiol 2010; 55: 2614–62. doi: 10.1016/j.jacc.2009.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 8.Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J 2010; 31: 806–14. doi: 10.1093/eurheartj/ehq025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antony R, Daghem M, McCann GP, Daghem S, Moon J, Pennell DJ, et al. Cardiovascular magnetic resonance activity in the United Kingdom: a survey on behalf of the British Society of Cardiovascular Magnetic Resonance. J Cardiovasc Magn Reson 2011; 13: 57. doi: 10.1186/1532-429X-13-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curzen N, Rana O, Nicholas Z, Golledge P, Zaman A, Oldroyd K, et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain?: the RIPCORD study. Circ Cardiovasc Interv 2014; 7: 248–55. doi: 10.1161/CIRCINTERVENTIONS.113.000978 [DOI] [PubMed] [Google Scholar]
- 11.Kurt M, Shaikh KA, Peterson L, Kurrelmeyer KM, Shah G, Nagueh SF, et al. Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol 2009; 53: 802–10. doi: 10.1016/j.jacc.2009.01.005 [DOI] [PubMed] [Google Scholar]
- 12.Gazelle GS, Kessler L, Lee DW, McGinn T, Menzin J, Neumann PJ, et al. ; Working Group on Comparative Effectiveness Research for Imaging. A framework for assessing the value of diagnostic imaging in the era of comparative effectiveness research. Radiology 2011; 261: 692–8. doi: 10.1148/radiol.11110155 [DOI] [PubMed] [Google Scholar]
- 13.Shaw LJ, Marwick TH, Zoghbi WA, Hundley WG, Kramer CM, Achenbach S, et al. Why all the focus on cardiac imaging? JACC Cardiovasc Imaging 2010; 3: 789–94. doi: 10.1016/j.jcmg.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 14.Bruder O, Schneider S, Nothnagel D, Dill T, Hombach V, Schulz-Menger J, et al. EuroCMR (European Cardiovascular Magnetic Resonance) registry: results of the German pilot phase. J Am Coll Cardiol 2009; 54: 1457–66. doi: 10.1016/j.jacc.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 15.Pennell DJ, Sechtem UP, Higgins CB, Manning WJ, Pohost GM, Rademakers FE, et al. ; Society for Cardiovascular Magnetic Resonance; Working Group on Cardiovascular Magnetic Resonance of the European Society of Cardiology. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. Eur Heart J 2004; 25: 1940–65. doi: 10.1016/j.ehj.2004.06.040 [DOI] [PubMed] [Google Scholar]
- 16.Abbasi SA, Ertel A, Shah RV, Dandekar V, Chung J, Bhat G, et al. Impact of cardiovascular magnetic resonance on management and clinical decision-making in heart failure patients. J Cardiovasc Magn Reson 2013; 15: 89. doi: 10.1186/1532-429X-15-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute for Health and Clinical Excellence (NICE). Chest pain of recent onset: assessment and diagnosis [CG 95]. NICE; 2010. Manchester, UK: [Updated August 2013, cited October 2015.] Available from: http://www.nice.org.uk/guidance/CG95. [Google Scholar]
- 18.Greenwood JP, Maredia N, Younger JF, Brown JM, Nixon J, Everett CC, et al. Cardiovascular magnetic resonance and single-photon emission computed tomography for diagnosis of coronary heart disease (CE-MARC): a prospective trial. Lancet 2012; 379: 453–60. doi: 10.1016/S0140-6736(11)61335-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwitter J, Wacker CM, Wilke N, Al-Saadi N, Sauer E, Huettle K, et al. ; MR-IMPACT Investigators. MR-IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion-cardiac magnetic resonance vs. single-photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J 2013; 34: 775–81. doi: 10.1093/eurheartj/ehs022 [DOI] [PubMed] [Google Scholar]
- 20.The relative cost-effectiveness of five non-invasive cardiac imaging technologies for diagnosing coronary artery disease in Ontario. Ontario: Toronto Health Economics and Technology Assessment Collaborative; 2010. Available from: http://old_theta.phm.utoronto.ca/papers/theta_report_007.pdf. [Google Scholar]
- 21.Walker S, Girardin F, McKenna C, Ball SG, Nixon J, Plein S, et al. Cost-effectiveness of cardiovascular magnetic resonance in the diagnosis of coronary heart disease: an economic evaluation using data from the CE-MARC study. Heart 2013; 99: 873–81. doi: 10.1136/heartjnl-2013-303624 [DOI] [PubMed] [Google Scholar]
- 22.White JA, Fine NM, Gula L, Yee R, Skanes A, Klein G, et al. Utility of cardiovascular magnetic resonance in identifying substrate for malignant ventricular arrhythmias. Circ Cardiovasc Imaging 2012; 5: 12–20. doi: 10.1161/CIRCIMAGING.111.966085 [DOI] [PubMed] [Google Scholar]
- 23.Mahmoudi M, Harden S, Abid N, Peebles C, Nicholas Z, Jones T, et al. Troponin-positive chest pain with unobstructed coronary arteries: definitive differential diagnosis using cardiac MRI. Br J Radiol 2012; 85: e461–6. doi: 10.1259/bjr/90663866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McConnell MV, Ganz P, Selwyn AP, Li W, Edelman RR, Manning WJ. Identification of anomalous coronary arteries and their anatomic course by magnetic resonance coronary angiography. Circulation 1995; 92: 3158–62. doi: 10.1161/01.CIR.92.11.3158 [DOI] [PubMed] [Google Scholar]