Abstract
Objectives
To explore general practitioners’ (GPs’) experiences with and views on the diagnosis and management of patients with cardiorespiratory symptoms during GP out-of-hours care. We also aimed to identify ways of (diagnostic) support during these consultations.
Design
Qualitative study; face-to-face semistructured interviews.
Setting
GP out-of-hours care in the Netherlands.
Participants
15 GPs in the province of Limburg, the Netherlands.
Results
Overall, GPs find cardiorespiratory consultations challenging and difficult. Tension and uncertainty as well as defensive behaviour were the key themes that characterised GPs’ experiences. We identified several subthemes underlying the key themes: setting, potentially severe consequences, absence of a pre-existing relationship and little knowledge of the patient's background, difficulties differentiating between possible causes of symptoms, changed public opinion and patient population, and previous experiences. GPs approach cardiorespiratory consultations differently and their threshold for referring patients and performing diagnostic tests is lower. We identified differing views on the use of additional diagnostic tests at GP out-of-hours services.
Conclusions
This study sheds further light on how GPs experience cardiorespiratory consultations during out-of-hours care and how this leads to a high number of cardiorespiratory referrals. GPs relate cardiorespiratory consultation during out-of-hours care with tension and uncertainty leading to defensive behaviour, which can be translated into a different approach towards cardiorespiratory consultations and a lower threshold for referring patients and performing diagnostic tests. Opinions on the possible added value of additional diagnostics in reducing the number of referrals should be further investigated, as we identified differing views on the use of additional diagnostic tests at GP out-of-hours services.
Keywords: GENERAL MEDICINE (see Internal Medicine), PRIMARY CARE, QUALITATIVE RESEARCH
Strengths and limitations of this study.
This is the first in-depth qualitative study to explore general practitioners’ (GPs’) experiences with and views on the diagnosis and management of patients with cardiorespiratory symptoms in general during out-of-hours care.
We specifically asked GPs about symptoms and not conditions.
Out-of-hours care is differently organised across European countries and therefore some results may not be applicable to each out-of-hours care setting.
Introduction
Patients with cardiorespiratory symptoms visiting general practitioner (GP) out-of-hours services are often referred to secondary care.1 Although cardiorespiratory symptoms can be caused by serious underlying conditions, that could have severe consequences if left untreated; often, no serious underlying conditions are found and patients are discharged the same day.2 3–6
Previous research has shown that GPs find the diagnosis and management of patients with chest pain and heart failure difficult, because serious conditions are frequently masked by other conditions and symptoms are often non-specific or vague, which makes them diagnostically challenging.3–5 7 8 When investigating GPs’ perceptions, attitudes and experiences with patients with chest pain or dyspnoea in general practice, most of the existing literature focuses on GPs’ experiences with the diagnosis and management of specific cardiorespiratory conditions, for example, heart failure or specific care for patients with advanced chronic obstructive pulmonary disease.8–10 Little is known about GPs’ experiences with patients with cardiorespiratory symptoms in general and during out-of-hours care. Differences between out-of-hours care and office hours care can be expected, as previous research suggests that GPs incorporate background knowledge about the patient, discrepancies between previous and current consultation, knowledge on individual symptom presentation, the physician’s own ideas and gut feelings in the management and referral of patients in daytime practice,11–13 whereas GPs generally lack a prior relationship with patients and relevant background information during out-of-hours care.
The aim of this study was to explore GPs’ experiences with and views on the diagnosis and management of patients with cardiorespiratory symptoms during GP out-of-hours care. The secondary aim was to identify ways of (diagnostic) support during these consultations.
Methods
The Dutch GP out-of-hours system
In the Netherlands, every citizen is registered with one GP practice. GPs act as a gatekeeper to secondary care. GP out-of-hours care is organised by large-scale GP cooperatives, with generally 40–250 GPs practising at one GP out-of-hours service in one region, taking care of 100 000–500 000 citizens.14 Therefore, patients are usually unknown to the doctor on call, especially since GPs often have no to very limited access to patient records. All out-of-hours services have a telephone triage centre in which trained nurses conduct telephone triage under supervision of a GP and the services are accommodated with a specially equipped car and a driver that are available to GPs for home visits.14 Access to diagnostic tests is limited and varies between services.15 Out-of-hours services are open all evenings, nights and weekends. GP shifts are typically 6–10 hours.
Sampling and participants
We selected a purposive sample of 38 GPs from a database of all GPs in the province of Limburg, the Netherlands. GPs were selected according to differences in age, sex and location of the GP out-of-hours service, since previous research has shown that not all GP out-of-hours services have the same diagnostic facilities, which may affect GPs' experiences.15 GPs were first invited by email and when no response followed, we contacted them by phone. Sampling continued until 15 GPs agreed to participate. We offered the participating GPs a reimbursement of €30 in vouchers.
Data collection
Two trained researchers (TB and LO) carried out 15 semistructured face-to-face interviews using a topic guide, which was developed based on existing literature. The topic guide consisted of questions on GPs’ experiences with and views on the diagnosis and management of patients with cardiorespiratory symptoms and explored the need for support and additional diagnostic tools in these consultations. We predefined cardiorespiratory as signs and symptoms that could indicate heart or lung disease. The topic guide was pilot tested in audio taped interviews with two GP trainees from our research department. During the study, we performed minor modifications to the topic guide as new insights emerged. All interviews were conducted and audio taped in GPs’ surgeries in the spring of 2015. On average, the interviews lasted 36 min with a range from 23 to 49 min. GPs were aware that the purpose of the study was to explore experiences and opinions and not to audit practice. We encouraged them to talk freely about what they considered to be important.
Prior to the interviews, participants were asked to read and sign a consent form and fill in a short questionnaire about personal and background characteristics. The interviews were equally divided among the two interviewers. One interviewer conducted the interview, while the other observed. After 13 interviews, we felt we had reached data saturation. Hereafter, we conducted two more interviews to confirm data saturation, defined as the identification of no new relevant codes in the last two interviews.
Data analysis
The interviews and analyses were conducted in parallel. TAvB and LMRO transcribed the audio taped interviews verbatim. The anonymised transcripts were used as a basis for the thematic content analysis and were read in detail by TAvB, LMRO and AMRS. The transcripts were entered into Nvivo V.9 software to assist analysis and coding. The first 10 transcripts were independently coded by both interviewers and the last five transcripts were coded by one interviewer and checked and supplemented by the other. All new codes were discussed with a third coder (AS). Disagreement among the three coders was resolved by discussion. The thematic content analysis consisted of familiarisation with the data, indexing the material, charting and interpretation to form the key themes.16 Themes were shared and debated by the team to reach a concordance of views on common themes.
Trustworthiness
Reliability of the analysis was strived for by double coding all interviews. We tried to enhance the reliability of the interpretation of the data by observing all interviews—one interviewer conducted the interview, while the other one observed—and taking notes on the interviewing process. Furthermore, peer debriefing sessions were held with the research team, to reflect on the research process as a whole and specifically on the analysis and interpretation of the data. In these sessions, we discussed the content of the interviews, coding of the interviews and the thematic content analysis, reviewed the topic guide, and assessed whether data saturation was achieved. Transferability was strived for by providing descriptive data on the study population, information on the sampling and interviewing process, and quotes from participants. Moreover, we kept a detailed record of the recruitment process and interview schedule.
Results
Characteristics of the 15 participating GPs are described in table 1. Twice as many male GPs as female GPs were interviewed; their mean age was 49 years and, on average, the GPs worked 27 out-of-hours shifts in the past 12 months.
Table 1.
GP characteristics (n=15)
| Gender, male, n | 11 |
| Age, mean (range) | 49 (37–58) |
| Years since qualifying, mean (range) | 16 (5–25) |
| Average working hours per week, mean (range) | 41 (25–65) |
| Out-of-hours shifts in the past 12 months, mean (range) | 27 (16–35) |
GP, general practitioner.
Experiences with cardiorespiratory consultation during out-of-hours care
Most GPs considered the cardiorespiratory consultation at GP out-of-hours services to be difficult. Tension and uncertainty as well as defensive behaviour were the key themes that characterised GPs’ experiences; tension and uncertainty led to a defensive decision-making style, resulting in a different approach towards these consultations and a lower threshold for referring patients and performing diagnostic tests. Although the majority of GPs expressed a desire for additional tests to reduce diagnostic uncertainty, all GPs emphasised that the patient's background and taking a thorough medical history are most important and some GPs were even very critical towards adding additional diagnostic tests. We identified several subthemes underlying the key themes (see figure 1).
Figure 1.
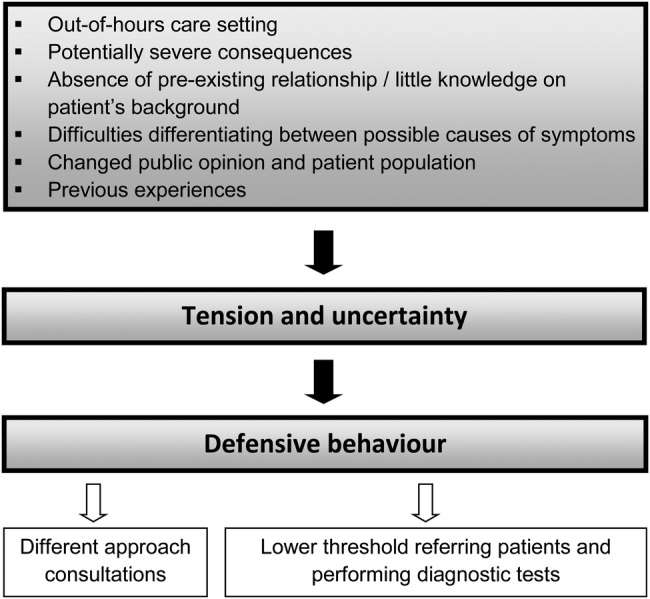
Overview of the key themes relating to cardiopulmonary consultations during out-of-hours care.
Out-of-hours care setting
GPs were more likely to be faced with patients with acute symptoms during out-of-hours care and patients were generally more worried:
‘I do get the impression that people at the out-of-hours service are clearly more worried about their symptoms than patients who come to the regular surgery with the same complaints, but I think that has to do with the whole setting, as there's a certain barrier to be overcome before you decide to see a different GP or go to the out-of-hours service.’ (GP9)
‘Well, what you see is, you see mostly patients you don't know, you see mostly urgent cases, whereas in our everyday practice, we're mostly dealing with chronic matters.’ (GP6)
This caused a sense of urgency among GPs, which prompted them to act faster and more defensively. A higher workload during out-of-hours care was identified as one of the reasons to refer more easily. One GP said:
‘(…) the speed at which things happen, the speed with which you have to make decisions. It's the pressure, of course, the waiting room full of patients. The pressure from the triage nurses, having to plan in another patient, that sort of thing. Well, that's just not very pleasant. You'd like to take all the time you need for what you're faced with, without feeling the pressure, but that's just not possible.’ (GP10)
GPs also stressed the importance of getting it right the first time as there will be no second chance, because there is little opportunity for follow-up during their shifts at the GP out-of-hours service:
‘(…) you just have to get it right at the first consultation, be on the right track. In your own practice you're more in control, you can ask the patient to return; it gives you more opportunities for a second chance.’ (GP3)
‘(…) if you want to do a reassessment, you'll have to do it within your own shift, otherwise a colleague will be dealing with the case.’ (GP9)
Potentially severe consequences
The setting makes GPs feel there is no second chance; moreover, the nature of the disease itself also urges GPs to get it right the first time. Cardiorespiratory symptoms were associated with potentially life-threatening conditions. GPs mentioned a certain apprehension of making mistakes in the diagnoses, as these conditions may have severe consequences when misdiagnosed or not treated properly. Hence, GPs acted more defensively. Two GPs said:
‘Well, because they're often more life-threatening. So you can't, if you get it completely wrong, you can't have another look the next day. I think, yeah, that makes a difference.’ (GP6)
‘(…) very rarely, but never with cardiorespiratory patients. I use different criteria then, making me more cautious. Purely because of the acute problem and the potential consequences if you get it wrong.’ (GP13)
Absence of a pre-existing relationship and little knowledge of the patient's background
Absence of a pre-existing relationship between the doctor and the patient and little to no knowledge of the patient's background were considered complicating factors. First of all, it makes it more difficult for GPs to assess a patient's current state, since the previous state is unknown to the doctor on call:
‘And if you don't know a patient, you become more cautious, and well, it makes the assessment considerably more difficult, really.’ (GP4)
The absence of a relationship of trust makes it more difficult for GPs to discuss their management with patients, since the latter are unfamiliar with the capacities of the doctor on call. Furthermore, some GPs mentioned that it is harder to justify a misdiagnosis if there is no pre-existing relationship with the patient:
‘Things can always go wrong, but such things are perceived differently at the out-of-hours service, by patients as well. They have less trust in the doctor than at my own practice. And that makes you a bit more cautious.’ (GP11)
As a result, GPs stated that the cardiorespiratory consultation takes more time during out-of-hours care:
‘And if you don't know the patient, that makes you more cautious and well it just makes the assessment that much more difficult, really, taking more time, and well you don't always have enough time.’ (GP4)
Difficulties differentiating between possible causes of symptoms
The tension and uncertainty experienced by GPs can partially be explained by the difficulty in differentiating between possible causes of the symptoms. The strongly divergent and sometimes vague symptoms of patients complicate the identification of serious pathology:
‘If people present with vague symptoms, like being a bit dyspneic, vague chest pains, for instance. And then they cough a little. That's enough to start wondering what might this be.’ (GP11)
Furthermore, GPs struggle with diagnostic uncertainties. Most of them, for instance, found it difficult to interpret ECGs:
‘I'm glad in a way that our protocol says that the cardiologist must also look at it. As I think that the correct interpretation of an ECG is actually too difficult for a GP, in the case of acute or potentially acute problems. I wouldn't consider myself fully qualified to do that without some back-up of a specialist.’ (GP5)
Moreover, the absence of a typical clinical presentation, normal physical examination and a normal ECG does not exclude severe underlying pathology:
‘I can listen to a heart, but that says nothing at all. You can even have an ECG made; that doesn't say it all either. (…) Or how ill a patient is; I've had patients walking in calmly and saying to me: well, I have such and such, and I thought Oh well I might as well see a doctor. And he turned out to have an acute myocardial infarction.’ (GP4)
Most GPs stated that they find it harder to diagnose and manage patients with cardiac symptoms compared to pulmonary symptoms, with the exception of a pulmonary embolism:
‘Of course we haven't talked about pulmonary embolism yet, but that remains very difficult to diagnose. It can take all sorts of forms, and patients may or may not be very ill.’ (GP4)
‘Yeah, that's (…) a problem that's sometimes disguised. You hear nothing, you see nothing on the ECG, except occasionally a strained atrium or ventricle. No, I really think that's a difficult one.’ (GP1)
Changed public opinion and patient population
According to the GPs, the public opinion and the expectations of patients have changed over time. This has had an effect on the tension and uncertainty experienced by GPs. Four GPs stated that, unlike in the past, society seems to accept medical errors or mistakes to a lesser extent. The fear of a complaint or reprimand by the Disciplinary Board was an important incentive to act more cautiously:
‘Everyone makes mistakes of course. But society is now such that people no longer accept errors in medical care, nor in other areas. And, well, that's made me a lot more cautious.’ (GP4)
This is accompanied by an ever more demanding patient, who expects GPs to perform additional tests. As a consequence, GPs stated to refer patients more easily and to attach great importance to justifying management decisions, in particular to patients or the Disciplinary Board. GPs also encountered a change in patient population over the past decade. In particular, they mentioned an increased medical complexity:
‘What I've noticed in recent years at the out-of-hours service is increased comorbidity, so people with a range of pathologies, the really chronic patient with all kinds of problems, the geriatric patient with all kinds of problems, with contra-indications for certain medications, certain therapies, with interactions. And that can also make it more difficult, making you think: what do I need to do for this patient? What would be good for them and what would not be good?’ (GP7)
Previous experiences
Some GPs mentioned a form of misdiagnosis or mistake when taking care of a patient with chest symptoms in the past. They explained that this has influenced subsequent decisions, making them more defensive than before:
‘(…) Ten years ago I got a reprimand from the Disciplinary Board as I was said to have missed a cardiac infarction. (…) For the first years after that I did feel more insecure. You notice that you tend to adopt a very defensive attitude as a GP.’ (GP3)
‘Because I ‘burnt my fingers’ a few times (…) got it wrong (…) as a doctor you gradually learn from your mistakes.’ (GP6)
Also, experiences of colleagues caused some GPs to become more defensive:
‘(…) I've also noticed and heard, you hear from colleagues from time to time, how things can develop differently from your on-the-spot assessment. That's made me more cautious.’ (GP11)
This was strengthened by the notion that possible consequences of a misdiagnosis can be serious, especially with potential cardiac pathology.
Influence of defensive behaviour on the decision-making process
The defensive behaviour of GPs influences the decision-making process in several ways. GPs have a different approach towards these consultations. They rely less on their gut feelings and try to take only objective symptoms into account:
‘At my own practice I can afford to trust my intuition more. If I see the same patient at the out-of-hours service I may have the same intuition, but I'd tend not to take it into account unless I can objectify it.’ (GP3)
Furthermore, their threshold for referring patients and performing diagnostic tests is lower. For example, GPs use ECG more often during out-of-hours care.
‘(…) In any case I'm a bit more defensive than usually at the out-of-hours service. That's got to do with the factors I just mentioned. Not knowing the patients well and of course not wanting to make mistakes and wanting…at least, that's what I call more defensive. That you perform diagnostic tests more easily and perhaps refer sooner, yes.’ (GP2)
Some GPs stated that the relatively large number of patients sent back home after referral to secondary care is inherent to the organisation of the out-of-hours care and the possibly severe underlying pathology in patients with cardiorespiratory symptoms.
Possible improvements in support during cardiorespiratory consultation
GPs expressed a desire for more time available for cardiorespiratory consultations, immediate consultation of a cardiologist to aid them in the interpretation of an ECG and improving the availability as well as the quality of patients’ medical records. Furthermore, GPs requested improvements of the current triage system, which sometimes leads to higher urgency categories than necessary:
‘The triage nurses have to assess the urgency, and they very often classify it too high. I can understand that, as they're facing the same problem as we: when in doubt, refer to a higher tier. But that greatly increases the workload, especially with this group of patients. So you often see clusters of high-urgency cases for cardiorespiratory problems, which makes matters more difficult for us too.’ (GP7)
GPs were divided when asked whether or not they wanted more additional diagnostics available. GPs in favour of diagnostic tests expressed a desire for additional diagnostics as these could aid in reassuring the patient and help to motivate management decisions to patients and their relatives. Additional diagnostics could help GPs to rule out acute pathology, allowing them to send patients back home safely. One GP explained his wish for the use of d-dimers and troponin as follows:
‘Because when they're negative, that excludes a lot of options. So I can safely leave someone at home and safely discuss follow-up management.’ (GP9)
As a result, they would be less likely to refer a patient. Moreover, additional diagnostic facilities could help reduce the GPs’ tension and uncertainty. One GP even suggested that it could help to improve the quality of GP out-of-hours care in general:
‘Yeah, that would make me very happy. I'm really looking forward to that. So I think we can take further major quality-improvement steps in primary care in that respect.’ (GP6)
However, some GPs did not see any added value of additional diagnostic tests. According to them, some tests should be preserved for secondary care only because GPs lack the knowledge and skills to safely use and interpret this kind of diagnostics:
‘What I want to have while on duty at the out-of-hours service is my stethoscope, as I really know how that works, I know what I'm supposed to hear and not to hear. And I very much prefer to leave it to the cardiologist to interpret the patient's troponin.’ (GP3)
GPs were concerned that the availability of additional diagnostics would oblige them to use them. Some GPs were apprehensive of overdiagnosis: the use of diagnostics without a proper indication. Furthermore, they had doubts about the validity and reliability of these additional diagnostic tests. Two GPs said:
‘(…) What I find is that once patients know it exists, they start to ask for it. So it also involves, like, how am I going to prevent having to do it too often, as you're going to, you have to do it based on a proper indication, I think.’ (GP14)
‘(…) Well, actually, before you start using a test it must have been thoroughly evaluated, and the test must also be reliable.’ (GP15)
Discussion
Summary
Most GPs consider the cardiorespiratory consultation during out-of-hours care to be difficult. They relate it with tension and uncertainty leading to defensive behaviour during GP out-of-hours care. GPs have a different approach towards cardiorespiratory consultations at the out-of-hours service compared to their own practice and their threshold for referring patients and performing diagnostic tests is lower. We identified differing views on the use of additional diagnostic tests at GP out-of-hours services.
Strengths and limitations
As far as we know, this is the first in-depth qualitative study to explore GPs’ experiences with and views on the diagnosis and management of patients with cardiorespiratory symptoms in general during out-of-hours care. We specifically chose to ask GPs about symptoms and not conditions, as typical patients present with symptoms and making an accurate diagnosis within a 10 min consultation is part of the complexity of general practice. We aimed to achieve an in-depth data analysis, as both interviewers were trained; one interviewer observed while the other one conducted the interview; both interviewers who analysed the data were already familiar with the data and all transcripts were double coded. All face-to-face interviews were conducted in the GPs’ surgeries, as we assumed GPs felt more comfortable and secure in their daily environment. Given that this kind of research is prone to socially desirable answers, we emphasised that we were interested in the GPs’ own experiences and opinions and that we were not auditing practice or assessing knowledge.
A limitation of this study is that three interviews were not observed by the second interviewer, though we found no major differences between the results of these interviews and the other interviews. Moreover, we did not return transcripts to participants for comments and participants did not provide feedback on the findings. Some results may not be applicable to each out-of-hours care setting in Europe, as out-of-hours care is differently organised across European countries. Furthermore, we only included GPs from one province in the South of the Netherlands. This may have influenced the results, because this province has one of the highest mortality rates from cardiovascular pathologies in the Netherlands and GPs have relatively more access to diagnostic tests in this region.15 17 Nonetheless, we interviewed several GPs working at an out-of-hours service where hardly any diagnostic tests were available. Although female GPs were under-represented in our research population, we did not identify any major differences in responses of female GPs compared to our main results.
Comparison with existing literature
In accordance with the literature on care during office hours, we found that GPs experience cardiorespiratory consultations as difficult. While some of the underlying reasons for this perceived challenge are the same as for cardiorespiratory consultations during office hours,3–5 7 8 we found supplemental reasons for why these consultations are notoriously difficult during out-of-hours care. For example, the absence of a pre-existing relationship with the patient and little to no knowledge of the patient's background are of major influence on the cardiorespiratory consultation during out-of-hours care, as it makes it more difficult to assess the patient's current state. It seems logical that a lack of this knowledge complicates the consultation during out-of-hours care, as previous research focusing on care during office hours found that background information and discrepancies between previous and current consultation were important factors in chest pain consultations.12 13 Information on the patient's background as well as taking a thorough medical history were considered the most important aspects of the consultation in our study. This is in line with previous research on GPs’ diagnostic approach of patients with chest pain during out-of-hours care.18 However, the GPs in our study stated that they attach less value to their gut feelings and more to objective signs during out-of-hours care, which is in contradiction with previous research that found that GPs’ gut feelings and personal ideas are important in the decision-making process for patients with chest pain during office hours.11 12 This contradiction could again be explained by the difference in setting.
We found that tension and uncertainty play an important role in the cardiorespiratory consultation during GP out-of-hours care, which leads to a lower threshold for referring patients to secondary care. A study that explored variations in GPs’ out-of-hours referrals in general found similar reasons for being more cautious during out-of-hours care, such as GPs’ anxiety about the consequences of the decision not to refer.19 We gained new insight into GPs’ views on patients with pulmonary symptoms. Most GPs experience such patients as less difficult than those with cardiac symptoms, with the exception of a pulmonary embolism.
Implications for research and practice
This study sheds further light on why referrals for cardiorespiratory symptoms are relatively high during out-of-hours care. Additional diagnostics may be of added value in reducing the number of referrals. However, since we identified differing views on the use of such additional diagnostic tests, further research is necessary to gain a better understanding of GPs’ motives to either use or refuse new diagnostic tests. The insights into the cardiorespiratory decision-making process of GPs working at out-of-hours services may aid the development of strategies to reduce the number of referrals and could aid in improving mutual understanding between primary and secondary care physicians.
Acknowledgments
The authors thank all GPs who participated in the interviews.
Footnotes
Contributors: AMRS, TAvB, LMRO and JWLC created the interview script and TAvB and LMRO performed the interviews. AMRS, TAvB and LMRO performed the initial data analyses and AMRS, TAvB, LMRO and JWLC discussed and analysed the results and made adjustments to the interview script. AMRS, TAvB and LMRO drafted the first manuscript. All authors contributed to the decisions about the study design, how to present the data, organise and edit the final manuscript.
Funding: This work was supported by a Veni-grant, assigned to JWLC (91614078), of the Netherlands Organisation for Health Research and Development (ZonMw).
Competing interests: None declared.
Ethics approval: Ethics approval for this study was obtained from the Medical Ethics Committee of Maastricht University in the Netherlands (METC 15-4-099) and all participants provided written consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Moll van Charante EP, van Steenwijk-Opdam PC, Bindels PJ. Out-of-hours demand for GP care and emergency services: patients’ choices and referrals by general practitioners and ambulance services. BMC Fam Pract 2007;8:46 10.1186/1471-2296-8-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruins Slot MH, Rutten FH, van der Heijden GJ et al. . Diagnostic value of a heart-type fatty acid-binding protein (H-FABP) bedside test in suspected acute coronary syndrome in primary care. Int J Cardiol 2013;168:1485–9. 10.1016/j.ijcard.2012.12.050 [DOI] [PubMed] [Google Scholar]
- 3.McConaghy JR, Oza RS. Outpatient diagnosis of acute chest pain in adults. Am Fam Physician 2013;87:177–82. [PubMed] [Google Scholar]
- 4.Willemsen RT, Kietselaer BL, Kusters R et al. . [Diagnostic tools for acute coronary syndrome (ACS): a challenge for general practitioners and cardiologists]. Ned Tijdschr Geneeskd 2014;158:A8078. [PubMed] [Google Scholar]
- 5.Body R, Carley S, Wibberley C et al. . The value of symptoms and signs in the emergent diagnosis of acute coronary syndromes. Resuscitation 2010;81:281–6. 10.1016/j.resuscitation.2009.11.014 [DOI] [PubMed] [Google Scholar]
- 6.Nilsson S, Scheike M, Engblom D et al. . Chest pain and ischaemic heart disease in primary care. Br J Gen Pract 2003;53:378–82. [PMC free article] [PubMed] [Google Scholar]
- 7.Phillips SM, Marton RL, Tofler GH. Barriers to diagnosing and managing heart failure in primary care. Med J Aust 2004;181:78–81. [DOI] [PubMed] [Google Scholar]
- 8.Fuat A, Hungin AP, Murphy JJ. Barriers to accurate diagnosis and effective management of heart failure in primary care: qualitative study. BMJ 2003;326:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khunti K, Hearnshaw H, Baker R et al. . Heart failure in primary care: qualitative study of current management and perceived obstacles to evidence-based diagnosis and management by general practitioners. Eur J Heart Fail 2002;4:771–7. 10.1016/S1388-9842(02)00119-8 [DOI] [PubMed] [Google Scholar]
- 10.Young J, Donahue M, Farquhar M et al. . Using opioids to treat dyspnea in advanced COPD: attitudes and experiences of family physicians and respiratory therapists. Can Fam Physician 2012;58:e401–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Stolper E, van Bokhoven M, Houben P et al. . The diagnostic role of gut feelings in general practice. A focus group study of the concept and its determinants. BMC Fam Pract 2009;10:17 10.1186/1471-2296-10-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruyninckx R, Van den Bruel A, Hannes K et al. . GPs’ reasons for referral of patients with chest pain: a qualitative study. BMC Fam Pract 2009;10:55 10.1186/1471-2296-10-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hani MA, Keller H, Vandenesch J et al. . Different from what the textbooks say: how GPs diagnose coronary heart disease. Fam Pract 2007;24:622–7. 10.1093/fampra/cmm053 [DOI] [PubMed] [Google Scholar]
- 14.Giesen P, Smits M, Huibers L et al. . Quality of after-hours primary care in the Netherlands: a narrative review. Ann Intern Med 2011;155:108–13. 10.7326/0003-4819-155-2-201107190-00006 [DOI] [PubMed] [Google Scholar]
- 15.Schols AM, Stevens F, Zeijen C et al. . [Diagnostic tests in GP out-of-hours services in the Netherlands]. Ned Tijdschr Geneeskd 2015;159:A9022. [PubMed] [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 17.Plat AW, te Wierik MJ, Kroon AA et al. . Regional differences in cardiovascular risk factor profile cannot fully explain differences in cardiovascular morbidity in the Netherlands: a comparison of two urban areas. Neth J Med 2005;63:309–15. [PubMed] [Google Scholar]
- 18.Burman RA, Zakariassen E, Hunskaar S. Chest pain out-of-hours—an interview study of primary care physicians’ diagnostic approach, tolerance of risk and attitudes to hospital admission. BMC Fam Pract 2014;15:207 10.1186/s12875-014-0207-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calnan M, Payne S, Kemple T et al. . A qualitative study exploring variations in GPs’ out-of-hours referrals to hospital. Br J Gen Pract 2007;57:706–13. [PMC free article] [PubMed] [Google Scholar]


