Abstract
Benign metastasising leiomyoma (BML) is a rare benign disease associated with uterine leiomyoma and history of uterine surgery. It most frequently occurs in premenopausal woman, with a pulmonary localisation, and consisting of multiple nodules. We present an uncommon case of a 69-year-old woman with a single BML of an inguinal lymph node. CT scans of thorax and abdomen excluded other metastasis localisation. The patient was cured with surgical excision of the mass. Lymph node involvement has been reported incidentally in BML literature. Lymphangitic spread can be considered a possible mechanism of BML metastasis.
Background
Benign metastasising leiomyoma (BML) is a rare condition characterised by histological benign proliferation of smooth muscle cells, metastasising with a haematological spread.1 2 It has been associated with a history of uterine leiomyoma, and many patients presenting with BML symptoms have previously undergone hysterectomy or other lower abdominal surgery.3 4 BML not only occurs predominantly in women of reproductive age but can also occur in postmenopausal. In the majority of cases, the disease consists of multiple nodules in the lungs, although other locations, such as the abdomen, soft tissue, skeletal muscles and lymph nodes, have been reported.3–6 Single case reports of metastases in skin, bone and heart have also been reported.4 7 8 Lesions are usually asymptomatic and most nodules are discovered using routine imaging. In this report, we describe an extraordinary case of a single metastasis of BML in an inguinal lymph node. We also provide a literature overview of cases of BML metastases to lymph nodes.
Case presentation
A 69-year-old woman presented with a painless subcutaneous mass in her left groin. The mass had slowly been growing over the course of 2 years. An enlarged lymph node was suspected. Her medical history consisted of an appendectomy at early age, a retroverted uterus correction at the age of 32 and uterine leiomyoma diagnosed at the age of 46, which was left untreated.
Investigations
On physical examination, a solid mass was found in the left groin, with a size of ∼20 mm×20 mm. Ultrasound-guided fine needle aspiration detected the presence of non-malignant leiomyoma, with positive desmins and actin. There was no mitotic activity and no cytonuclear atypia. To confirm the diagnosis, complete lymph node excision was performed. Histological analysis showed a lymph node with the presence of spindle-shaped cells that resembled the characteristics of those found in the fine needle aspiration (figure 1). EMA, S-100 and CD-117 staining were negative. After the diagnosis was confirmed, CT of thorax and abdomen was performed to investigate other metastases. This scan revealed no other suspected lesions.
Figure 1.
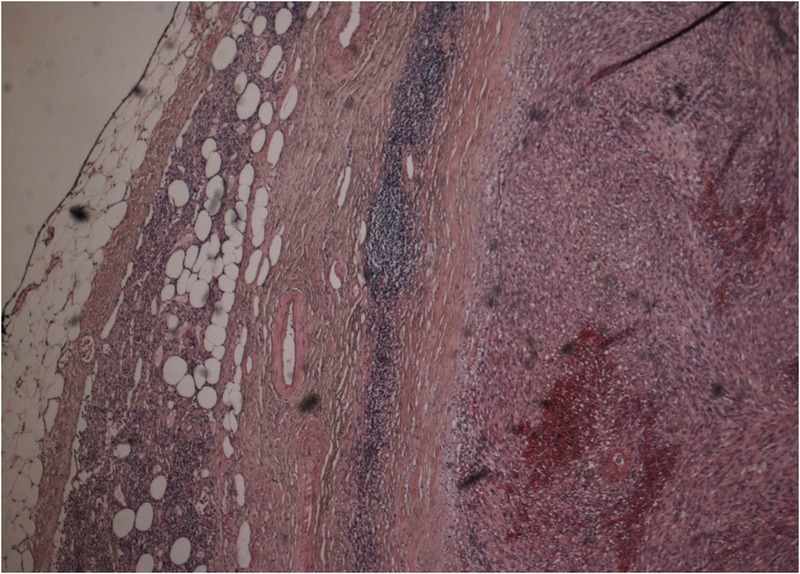
Histopathological examination. The lymph node is almost completely effaced by the lesion with just a small marginal rest of lymphoid cells. The lesion consists of non-atypical smooth muscle cells (H&E stain, ×200).
Differential diagnosis
Differential diagnosis of inguinal masses includes:
reactive lymph node,
lipoma,
malignant metastasis,
primary lymph node malignancy (eg, lymphoma),
hernia (femoral, inguinal),
femoral aneurysm,
hydrocele of the canal of Nuck.
Treatment
With the surgical excision of the lymph node, the patient's symptoms disappeared and other treatments were deferred.
Outcome and follow-up
The patient has not returned with recurrence or formation of BML in other locations postoperatively. We advised her to return to clinics if symptoms recurred or new masses were noticed. No further routine follow-up was advised.
Discussion
BML usually occurs in premenopausal women with a history of uterine leiomyoma and lower abdominal surgery, and mainly consists of multiple nodules affecting the lungs. To the best of our knowledge, our case is the first case of BML in an inguinal lymph node. Only a few cases describe single metastasis, and the occurrence of BML in postmenopausal women is rare.9
We conducted a MEDLINE literature search, covering the period from 1960 up to 2016 for lymph node metastasis of BML. In table 1, articles describing cases of lymph node BML are presented.10–19
Table 1.
Review of cases with lymph node benign metastasising leiomyoma
| Author | Year | Age | Localisation | Amount | Treatment | Other localisation |
|---|---|---|---|---|---|---|
| Andreeva et al10 | 2012 | 54 | Retroperitoneal | – | – | |
| Yoon et al11 | 2011 | 34 | Retroperitoneal | Multiple | Hysterectomy, resection and aromatase inhibitor | Lung |
| Tori et al12 | 2008 | 47 | Retroperitoneal | Multiple | GnRH agonist | Skeletal muscle (biceps) |
| Obana et al13 | 1996 | 39 | Retroperitoneal | Multiple | – | |
| Barter et al14 | 1987 | 46 | Retroperitoneal | Multiple | Resection+chemotherapy+radiation treatment | |
| Horie et al15 | 1984 | 50 | Retroperitoneal | Single | Hysterectomy+resection | LPD |
| Rigaud and Bogomoletz16 | 1983 | 57 | Retroperitoneal | Multiple | Hysterectomy+hormonal ablation+resection | |
| Hsu et al17 | 1981 | 40 | Retroperitoneal | Multiple | Hysterectomy+resection | LPD |
| Deppe et al18 | 1980 | 32 | Retroperitoneal | Multiple | Hysterectomy+resection | |
| Abell and Littler19 | 1975 | 27 | Retroperitoneal | Multiple | Hysterectomy+resection |
LPD, leiomyoma peritonealis disseminata.
Lymph node involvement is reported retroperitoneal. Only one case report found a single lymph node at presentation.15 In the cases reporting lymph node involvement, BML was found in lungs, skeletal muscles, chest and abdomen. Leiomyoma peritonealis disseminata has also been identified to coexist with lymph node manifestation.15 17
The pathogenesis of BML is still largely unknown. Previous reports have described a mainly haematological spread of metastasis.2 However, our case, as well as several previous case reports, demonstrate the involvement of the lymphatic system in the disease.10–19 In several cases, there was no evidence of haematological spread, as most metastases were only present in lymph nodes. Therefore, lymphangitic spread could be a plausible explanation of metastasis. Clinical implications, including prognosis and specific treatment, require further investigation. CT should be performed to exclude other nodules in thorax and abdomen, since BML mostly occurs with multiple nodules.6 Other localisations, such as lymph nodes, should be investigated with clinical suspicion of tumour metastasis.
There is no standard treatment for BML. Possible treatment strategies include expectative follow-up, surgical resection, hormonal ablation (oophorectomy) and hormonal medication (GnRH agonist, aromatase inhibitors, selective oestrogen receptor modulators and progesterone).1 2 Because of hormonal association, postmenopausal patients with BML should be treated with either expectative follow-up or primary surgical resection.20
We present the first case of a single BML located in a lymph node in the groin. Lymph node localisation has previously been described to be located mainly retroperitoneal. This case and previous case reports of lymph node BML, without other metastases localisations, indicate the possibility of the lymphangitic spread of the disease.
Learning points.
Single benign metastasising leiomyoma is extremely rare.
Benign metastasising leiomyoma can occur in inguinal lymph nodes.
Lymphangetic spread is a possible route of metastasis.
Footnotes
Contributors: This case report was designed by KGL and RET-M, The manuscript was written by KGL, RET-M and HWRS. The pathological images and pathological sections of the manuscript were provided and written by JALH.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tietze L, Günther K, Hörbe A et al. . Benign metastasizing leiomyoma: a cytogenetically balanced but clonal disease. Hum Pathol 2000;31:126–8. 10.1016/S0046-8177(00)80210-5 [DOI] [PubMed] [Google Scholar]
- 2.Patton KT, Cheng L, Papavero V et al. . Benign metastasizing leiomyoma: clonality, telomere length and clinicopathologic analysis. Mod Pathol 2006;19:130–40. 10.1038/modpathol.3800504 [DOI] [PubMed] [Google Scholar]
- 3.Awonuga AO, Shavell VI, Imudia AN et al. . Pathogenesis of benign metastasizing leiomyoma: a review. Obstet Gynecol Surv 2010;65:189–95. 10.1097/OGX.0b013e3181d60f93 [DOI] [PubMed] [Google Scholar]
- 4.Kayser K, Zink S, Schneider T et al. . Benign metastasizing leiomyoma of the uterus: documentation of clinical, immunohistochemical and lectin-histochemical data of ten cases. Virchows Arch 2000;437:284–92. 10.1007/s004280000207 [DOI] [PubMed] [Google Scholar]
- 5.Alessi G, Lemmerling M, Vereecken L et al. . Benign metastasizing leiomyoma to skull base and spine: a report of two cases. Clin Neurol Neurosurg 2003;105:170–4. 10.1016/S0303-8467(03)00002-7 [DOI] [PubMed] [Google Scholar]
- 6.Jo JH, Lee JH, Kim DC et al. . A case of benign metastasizing leiomyoma with multiple metastasis to the soft tissue, skeletal muscle, lung and breast. Korean J Intern Med 2006;21:199–201. 10.3904/kjim.2006.21.3.199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang LX, Lv FZ, Ma X et al. . Multifocal osteolytic lesions within lumbar spine in a middle-aged Chinese woman: a benign metastasizing leiomyoma? Spine 2012;37:E259–63. 10.1097/BRS.0b013e31822e9578 [DOI] [PubMed] [Google Scholar]
- 8.Galvin SD, Wademan B, Chu J et al. . Benign metastasizing leiomyoma: a rare metastatic lesion in the right ventricle. Ann Thorac Surg 2010;89:279–81. 10.1016/j.athoracsur.2009.06.050 [DOI] [PubMed] [Google Scholar]
- 9.Funakoshi Y, Sawabata N, Takeda S et al. . Pulmonary benign metastasizing leiomyoma from the uterus in a postmenopausal woman: report of a case. Surg Today 2004;34:55–7. 10.1007/s00595-003-2627-y [DOI] [PubMed] [Google Scholar]
- 10.Andreeva I, Danilova NV, Shikeeva AA et al. . Benign metastatic leiomyoma of the corpus uteri. Arkh Patol 2012;74:39–43. [PubMed] [Google Scholar]
- 11.Yoon G, Kim TJ, Sung CO et al. . Benign metastasizing leiomyoma with multiple lymph node metastasis: a case report. Cancer Res Treat 2011;43:131–3. 10.4143/crt.2011.43.2.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tori M, Akamatsu H, Mizutani S et al. . Multiple benign metastasizing leiomyomas in the pelvic lymph nodes and biceps muscle: report of a case. Surg Today 2008;38:432–5. 10.1007/s00595-007-3609-2 [DOI] [PubMed] [Google Scholar]
- 13.Obana Y, Yamazumi T, Kuroda T et al. . A case of leiomyomatosis in pelvic lymph nodes. Rinsho Byori 1996;44:595–8. [PubMed] [Google Scholar]
- 14.Barter JF, Szpak C, Creasman WT. Uterine leiomyomas with retroperitoneal lymph node involvement. South Med J 1987;80:1320–2. 10.1097/00007611-198710000-00030 [DOI] [PubMed] [Google Scholar]
- 15.Horie A, Ishii N, Matsumoto M et al. . Leiomyomatosis in the pelvic lymph node and peritoneum. Acta Pathol Jpn 1984;34:813–19. [DOI] [PubMed] [Google Scholar]
- 16.Rigaud C, Bogomoletz WV. Leiomyomatosis in pelvic lymph node. Arch Pathol Lab Med 1983;107:153–4. [PubMed] [Google Scholar]
- 17.Hsu YK, Rosenshein NB, Parmley TH et al. . Leiomyomatosis in pelvic lymph nodes. Obstet Gynecol 1981;57:91S–3S. [PubMed] [Google Scholar]
- 18.Deppe G, Clachko M, Deligdisch L et al. . Uterine fibroleimoyomata with aortic lymph node metastases. Int J Gynaecol Obstet 1980;18:1–3. [DOI] [PubMed] [Google Scholar]
- 19.Abell MR, Littler ER. Benign metastasizing uterine leiomyoma. Multiple lymph nodal metastases. Cancer 1975;36:2206–13. 10.1002/cncr.2820360938 [DOI] [PubMed] [Google Scholar]
- 20.Goto T, Maeshima A, Akanabe K et al. . Benign metastasizing leiomyoma of the lung. Ann Thorac Cardiovasc Surg 2012;18:121–4. 10.5761/atcs.cr.11.01688 [DOI] [PubMed] [Google Scholar]


